Abstract
Objective
Signs and symptoms of ischemia but no obstructive coronary artery disease (CAD) is often a diagnostic dilemma in women. The use of stress cardiac magnetic resonance imaging (CMRI) for advanced diagnostic assessment in these patients is a non-ionizing radiation option, but the diagnostic utility in this population is unknown. We examined the diagnostic role of stress CMRI in our patient population of these women.
Methods
We analyzed 113 consecutive female patients from 2/2006–11/2007 who had prior cardiac evaluations for signs and symptoms of ischemia but no obstructive CAD who underwent stress CMRI, which included anatomic, functional, adenosine stress perfusion and delayed enhancement imaging.
Results
The population demographics of 113 women included a mean age of 55±12.2 years with an average body mass index (BMI) of 25 ± 4.5. Overall, 43% had hypertension, 4% had diabetes and 3% were smokers. Overall, 80/113 (70%) demonstrated abnormal stress CMRI results. The majority of patients demonstrated findings consistent with subendocardial perfusion abnormalities suggestive of coronary microvascular dysfunction (CMD). Of note, 3 patients (4%) were diagnosed with congenital coronary anomalies or cardiomyopathy not detected in prior cardiac evaluations.
Conclusion
Among women with signs and symptoms of ischemia but no obstructive CAD, stress CMRI is frequently abnormal and is valuable in diagnosis of CMD. Stress CMRI appears useful for advanced diagnostic assessment in these diagnostically challenged patients.
Keywords: Myocardial ischemia, coronary microvascular dysfunction, cardiac magnetic resonance imaging
Introduction
Signs and symptoms of ischemia but no obstructive coronary artery disease (CAD) is often a diagnostic dilemma in women. Compared to men, women have a lower burden of obstructive CAD but relatively high rates of adverse cardiac events and near term mortality, related to coronary microvascular dysfunction (CMD) (1). Both stress testing with single photon emission computed tomography (SPECT) and echocardiography, optimized for segmental abnormalities related to epicardial CAD, are routinely used diagnostically, however, may be less sensitive and specific for detecting ischemia in women without obstructive CAD (2). Diagnosis is important for both prognostic and therapeutic reason.
Detection of perfusion abnormality consistent with myocardial ischemia is an important diagnostic finding with prognostic and therapeutic implications. Routine imaging with SPECT and echo does not specifically evaluate the subendocardium and may fail to detect CMD. Technological developments over the past decade allow for comprehensive cardiac magnetic resonance imaging (CMRI) which includes myocardial perfusion, function and anatomical assessment. Stress CMRI is a noninvasive method for evaluating myocardial perfusion that may offer an additional diagnostic value for differentiation of symptomatic patients with and without ischemia(3). The absence of ionizing radiation furthers its appeal as an imaging modality in women who have the double burden of radiation exposure to both lungs and breasts. We report our findings from women with signs and symptoms of ischemia but no obstructive CAD who underwent stress CMRI, to better understand the utility for diagnosis..
Methods
We analyzed 113 women with signs and symptoms of ischemia but no obstructive CAD who underwent stress CMRI for further evaluation between February 2006–November 2007. Institutional Review Board approval was obtained for the study. All subjects gave written informed consent prior to study participation.
CMRI
All stress CMRI studies were performed at Cedars-Sinai Medical Center with a 1.5 Tesla magnet (Siemens Sonata, Erlangen, Germany) with ECG-gating and a phased array coil using a highly standardized protocol with 0.05mmol/kg gadolinium first-pass perfusion three slice stress, followed by rest first pass perfusion. All patients tolerated pharmacologic stress using Adenosine at 140 μg/kg−1/min−1 infused for two minutes prior to and continued during first pass perfusion image acquisition. Cine imaging was performed in left ventricular short axis slices from above the base to the apex in addition to left ventricular long axis and outflow tract views. Delayed enhancement imaging in matched image positions was performed for exclusion of myocardial infarction.
The percentage of myocardial perfusion abnormality was defined semi-quantitatively by two experienced readers (DB, LT) who were blinded to the clinical status of the patient. Studies were analyzed using visual semi-quantitative 5-point, 16-segment AHA scoring system: 0- normal, 1- mildly reduced/equivocal, 2-moderately reduced 3-severely reduced, 4-absent perfusion. Scores in the basal-mid and distal-short axis slices were summed to obtain a summed rest score (SRS) and a summed stress score (SSS). A summed difference score (SDS) was obtained from the difference of the SRS and SSS. The percentage of abnormal myocardium was estimated by the summed stress scores divided by 64 and then multiplying by 100 (4, 5) We defined left ventricular non-compaction as prominent left ventricular trabeculae and deep intertrabecular recesses with ratio of tracbeculated to normal myocardium >2
Invasive Coronary Flow Reserve Determination
All women underwent clinically-indicated invasive coronary reactivity testing (CRT). During the CRT we evaluated coronary micro- and macro-vascular endothelial and non-endothelial dependent function were evaluated as previously published(6).
Statistical Analysis
Wilcoxon signed rank test was performed on the data. Categorical variables were compared using a Fischer’s exact test. All statistical analyses were performed using SAS 9.1 (SAS Institute Inc., Cary, NC, USA).
Results
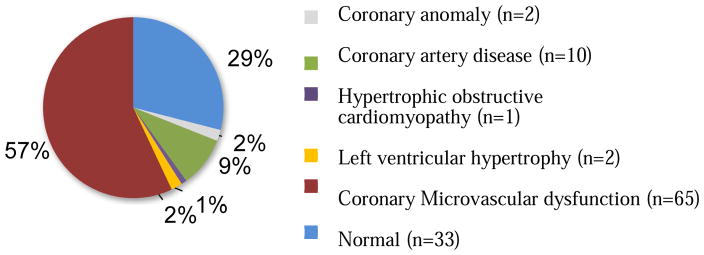
The clinical characteristics profile is a cohort of 113 women (55 ± 12 years) with cardiovascular risk factors (Table 1). The stress CMRI diagnostic findings are depicted in Figure 1. The majority of patients demonstrated stress-induced subendocardial perfusion abnormalities of variable severity, suggestive of CMD. Overall, 65/113 (57 %) were diagnosed with CMD on the basis of subendocardial perfusion abnormalities consistent with myocardial ischemia on stress CMRI ( Figure 1). Of note, 3 patients (4%) were diagnosed with congenital coronary anomalies or cardiomyopathy (left ventricular non-compaction) that had not been detected in prior cardiac evaluations.
Table 1.
| Demographics (n=113) | |
|---|---|
| Age (years ± SD) | 55 ± 12 |
| Hypertensive | 43% |
| BMI (mean ± SD) | 25 ±5 |
| Diabetics | 4% |
| Current Smokers | 3% |
Figure 1. CMRI Findings.
Stress CMRI findings in 113 patients with signs and symptoms of ischemia in cardiac workup and no prior diagnosis.
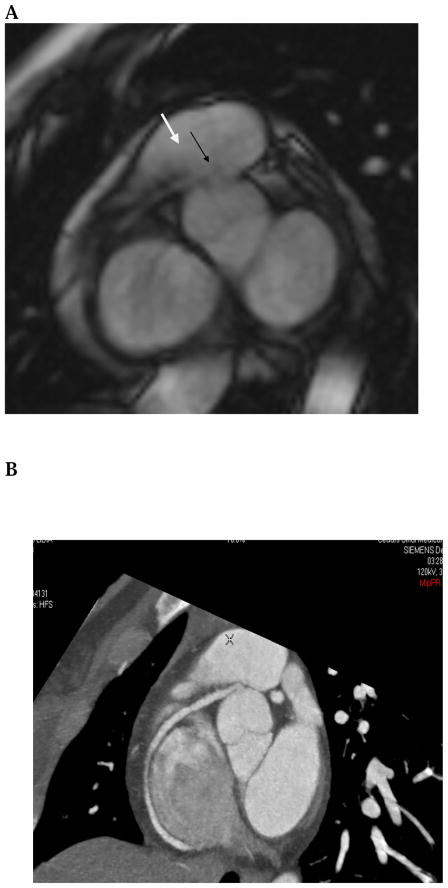
One of the patients was found to have an anomalous right coronary artery, as shown in Figure 2 A–B. The CMI perfusion study demonstrated a mid-ventricular hypoperfusion defect in the papillary muscles, lateral wall and septum. Detection of the anomalous right coronary artery was identified (Figure 2A) and subsequently confirmed with coronary computed tomography angiography (CCTA) (Figure 2B). The patient was then taken to cardiac catheterization and subsequently to coronary artery bypass surgery.
Figure 2. Case Example 1.
A. Stress CMRI cine imaging in the basal short axis suggested presence of anomalous origin of the right coronary artery from the left coronary sinus with course between the aortic root and the right ventricular outflow tract (black arrow). B. This congenital abnormality was subsequently confirmed by coronary computed tomography angiography (CCTA).
Discussion
This study demonstrates that stress CMRI is useful for advanced diagnostic assessment in patients who present with signs and symptoms of ischemia and no obstructive CAD. Overall, 80/113 (71%) of these patients demonstrated abnormal stress CMRI results. In particular, 3 patients (4%) were diagnosed with important structural abnormalities that had not been detected in prior cardiac evaluations.
Improvement in imaging
There are several challenges related to women with evidence of ischemia but no obstructive CAD. Women often present with atypical symptomatology which can be dismissed as “non-cardiac”. Women more commonly have subendocardial ischemia compared to men which can be missed on traditional stress testing. In addition, due to the decreased prevalence of obstructive CAD in women compared to men, exercise stress testing has a lower sensitivity and specificity for the detection of coronary disease in women(1). Because of these differences, traditional treadmill stress testing may not be the ideal first line “rule out” test in women with chest pain. Clinicians have a wide range of non-invasive diagnostic modalities for detecting ischemia including stress echocardiography, SPECT, positron emission tomography (PET), CCTA and stress CMRI. However, the accuracy and limitations of conventional stress testing in women remains an area of significant interest and the best modality for non-invasive testing is yet to be determined(7). Our study outlines some of the advantages of more detailed testing such as stress CMRI, which was able to show significant perfusion abnormalities as well as congenital anomalies that would have been missed with conventional stress testing.
Advanced cardiac imaging with stress CMRI offers promise for patients with persistent chest pain. Jahnke et al. suggests that a normal stress CMRI predicts very low adverse cardiac events (0.8%) over the next 3 years, whereas in a univariate analysis, abnormalities in perfusion and wall motion were highly predictive of future cardiac events (hazard ratio, 12.51; 95% CI, 3.64–43.03; and hazard ratio, 5.42; 95% CI, 2.18–13.50; P<0.001 respectively) (8) . Coelho-Filho et al. further validate CMRI’s strong prognostic value when evaluating a cohort of 405 patients (168 women, mean age 58 ±14 years)(9). They found that women with evidence of ischemia on CMRI demonstrated a strong association with major adverse cardiac events (MACE) compared to women without evidence of ischemia. This study further showed that subendocardial ischemia on stress CMRI also had a strong correlation with abnormal CRT. In addition, Negative myocardial ischemia on stress CMRI in women was associated with a very low annual MACE rate (0.3%), which was not statistically significant when compared to the male cohort.
While our study was based on women in the outpatient setting, stress CMRI has also been reported to have significant advantages in the inpatient setting and emergency department (ED). Miller et al. demonstrated that stress CMRI potentially be a cost-effective tool for the assessment of chest pain in the ED’s observation unit (OU) with no statistical difference in major cardiac events.(10) They randomized 109 ED patients with intermediate risk acute chest pain to OU care, cardiac markers and CMRI compared to standard inpatient care. First-year cardiac-related costs were significantly lower for the patients receiving OU-CMRI care versus inpatient care (geometric mean= $3,101 vs. $ 4,742 including the index visit [p= 0.004] and $29 vs. $152 following discharge [p=0.012])(10). Those patients with negative perfusion imaging could avoid hospital admission and ultimately decrease readmission rates and medical costs. Our findings support the utilization of stress CMRI for those institutions that are capable of supplying the personnel and equipment to perform and interpret testing.
Limitations
This is an observational and retrospective study was conducted solely on women in a tertiary care center, and may not be generalizable to community women or men. We used adenosine as stress agent and results may be different with regadenosine. We did not compare stress CMRI with CMRI without stress.
Conclusion
Among women with signs and symptoms of ischemia but no obstructive CAD, stress CMRI is frequently abnormal. Stress CMRI can uniquely evaluate myocardial ischemia, assess for function and identify anatomical abnormalities. Our data support the utilization of CMRI for advanced diagnostic assessment in patients with signs and symptoms of ischemia but no obstructive CAD.
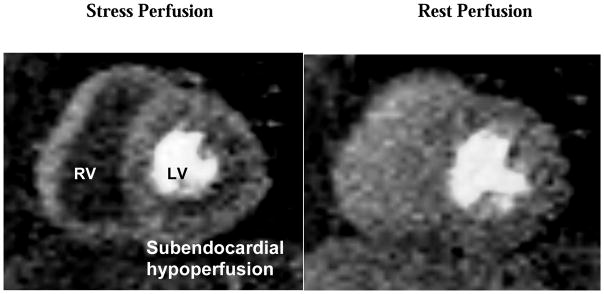
Figure 3. Case Example 2.
Stress CMR testing demonstrating a near circumferential subendocardial reversible perfusion abnormality with normal rest first pass perfusion
Highlights.
Signs and symptoms of ischemia but no obstructive coronary artery disease (CAD) is often a diagnostic dilemma in women. The use of stress cardiac magnetic resonance imaging (CMRI) for advanced diagnostic assessment in these patients is a non-ionizing radiation option, but the diagnostic utility in this population is unknown. We examined the diagnostic role of stress CMRI in our patient population of these women.
We analyzed 113 consecutive female patients from 2/2006–11/2007 who had prior cardiac evaluations for signs and symptoms of ischemia but no obstructive CAD who underwent stress CMRI, which included anatomic, functional, adenosine stress perfusion and delayed enhancement imaging.
The majority of patients demonstrated findings consistent with subendocardial perfusion abnormalities suggestive of coronary microvascular dysfunction (CMD). Of note, 3 patients (4%) were diagnosed with congenital coronary anomalies or cardiomyopathy not detected in prior cardiac evaluations.
Among women with signs and symptoms of ischemia but no obstructive CAD, stress CMRI is frequently abnormal and is valuable in diagnosis of CMD. Stress CMRI appears useful for advanced diagnostic assessment in these diagnostically challenged patients.
Acknowledgments
This work was supported by the National Institute on Aging, GCRC grant MO1-RR00425 from the National Center for Research Resources and grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, The Women’s Guild of Cedars-Sinai Medical Center, Los Angeles, CA, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, and QMED, Inc., Laurence Harbor, NJ, the Edythe L. Broad Women’s Heart Research Fellowship, Cedars-Sinai Medical Center, Los Angeles, California, and the Barbra Streisand Women’s Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Shaw LJ, Bugiardini R, Merz CNB. Women and Ischemic Heart Disease Evolving Knowledge. Journal of the American College of Cardiology. 2009;54(17):1561–75. doi: 10.1016/j.jacc.2009.04.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaw LJ, Merz CNB, Pepine CJ, Reis SE, Bittner V, Kelsey SF, et al. Insights from the NHLBI-Sponsored Women’s Ischemia Syndrome Evaluation (WISE) Study: Part I: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies. Journal of the American College of Cardiology. 2006;47(3s1):S4–S20. doi: 10.1016/j.jacc.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 3.Sawlani RN, Collins JD. Cardiac MRI and Ischemic Heart Disease: Role in Diagnosis and Risk Stratification. Current atherosclerosis reports. 2016;18(5):23. doi: 10.1007/s11883-016-0576-3. [DOI] [PubMed] [Google Scholar]
- 4.Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. J Nucl Cardiol. 2002;9(2):240–5. doi: 10.1067/mnc.2002.123122. [DOI] [PubMed] [Google Scholar]
- 5.Thomson LEJ, Fieno DS, Abidov A, Slomka PJ, Hachamovitch R, Saouaf R, et al. Added value of rest to stress study for recognition of artifacts in perfusion cardiovascular magnetic resonance. J Cardiovasc Magn R. 2007;9(5):733–40. doi: 10.1080/10976640701544415. [DOI] [PubMed] [Google Scholar]
- 6.Bugiardini R, Manfrini O, Pizzi C, Fontana F, Morgagni G. Endothelial function predicts future development of coronary artery disease: a study of women with chest pain and normal coronary angiograms. Circulation. 2004;109(21):2518–23. doi: 10.1161/01.CIR.0000128208.22378.E3. [DOI] [PubMed] [Google Scholar]
- 7.Mieres JH, Gulati M, Bairey Merz N, Berman DS, Gerber TC, Hayes SN, et al. Role of noninvasive testing in the clinical evaluation of women with suspected ischemic heart disease: a consensus statement from the American Heart Association. Circulation. 2014;130(4):350–79. doi: 10.1161/CIR.0000000000000061. [DOI] [PubMed] [Google Scholar]
- 8.Jahnke C, Nagel E, Gebker R, Kokocinski T, Kelle S, Manka R, et al. Prognostic value of cardiac magnetic resonance stress tests adenosine stress perfusion and dobutamine stress wall motion imaging. Circulation. 2007;115(13):1769–76. doi: 10.1161/CIRCULATIONAHA.106.652016. [DOI] [PubMed] [Google Scholar]
- 9.Coelho-Filho OR, Seabra LF, Mongeon F-P, Abdullah SM, Francis SA, Blankstein R, et al. Stress myocardial perfusion imaging by CMR provides strong prognostic value to cardiac events regardless of patient's sex. JACC: Cardiovascular Imaging. 2011;4(8):850–61. doi: 10.1016/j.jcmg.2011.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller CD, Hwang W, Case D, Hoekstra JW, Lefebvre C, Blumstein H, et al. Stress CMR imaging observation unit in the emergency department reduces 1-year medical care costs in patients with acute chest pain: a randomized study for comparison with inpatient care. JACC: Cardiovascular Imaging. 2011;4(8):862–70. doi: 10.1016/j.jcmg.2011.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]