Abstract
Background
Physical activity outcomes are poor following total knee arthroplasty (TKA). The purpose was to evaluate feasibility of a physical activity feedback intervention for patients after TKA.
Methods
Participants completing conventional TKA rehabilitation were randomized to a physical activity feedback (PAF; n=22) or control (CTL; n=23) group. The PAF intervention included real-time activity feedback, weekly action planning, and monthly group support meetings (12-weeks). The CTL group received attention control education. Feasibility was assessed using retention, adherence, dose goal attainment, and responsiveness with pre- and post-intervention testing.
Results
The PAF group had 100% retention, 92% adherence (frequency of feedback use), and 65% dose goal attainment (frequency of meeting goals). PAF group average daily step count increased from 5754 (2714) (pre) to 6917 (3445) steps/day (post).
Conclusion
This study describes a feasible intervention to use as an adjunct to conventional rehabilitation for people with TKA.
Keywords: knee osteoarthritis, total knee arthroplasty, physical activity, functional performance
Introduction
Knee osteoarthritis (OA) is the most common cause of chronic disability in the United States.(Dillon, Rasch, Gu, & Hirsch, 2006) To alleviate OA related knee pain, over 700,000 total knee arthroplasties (TKA)s are performed annually,(Kurtz, Ong, Lau, Mowat, & Halpern, 2007) with over 3 million per year projected by 2030.(Kurtz et al., 2007) TKA reliably reduces pain and improves self-reported functional performance post-operatively, (Bruun-Olsen, Heiberg, Wahl, & Mengshoel, 2013) yet, physical activity levels are not typically increased after TKA.(Brandes, Ringling, Winter, Hillmann, & Rosenbaum, 2011) The persistence of sedentary activity levels leads to increased weight gain after surgery,(Riddle, Singh, Harmsen, Schleck, & Lewallen, 2013; Zeni & Snyder-Mackler, 2010) decreased functional performance,(Bade, Kohrt, & Stevens-Lapsley, 2010; Dunlop, Song, Semanik, Sharma, & Chang, 2011) and increased risk for or progression of co-morbid conditions (e.g., type 2 diabetes mellitus, cardiovascular disease).(Tremblay, Colley, Saunders, Healy, & Owen, 2010) Additionally, sedentary physical activity levels provide a deleterious effect on the progression of knee and hip osteoarthritis,(Bade et al., 2010) which can expedite the need for a joint replacement in the contralateral limb.
Studies in other populations, who similarly demonstrate increased weight gain and low physical activity, have sought to increase physical activity and reduce weight gain using real-time physical activity monitoring or face-to face participant group meetings.(Maturi, Afshary, & Abedi, 2011; Tudor-Locke & Lutes, 2009; Wing, Tate, Gorin, Raynor, & Fava, 2006) These studies demonstrated effectiveness in terms of increased physical activity (steps/day), increased daily caloric expenditure, and improved maintenance of weight loss. In spite of these benefits, such promising interventions have not been prospectively studied in the TKA population to address the poor physical activity, weight gain, and poor functional outcomes present after patients undergo TKA.
The overall goal of this study was to evaluate the feasibility of physical activity feedback combined with face-to face intervention (intervention henceforth referred to as physical activity feedback) for patients after completion of standard TKA rehabilitation, with a control group receiving no physical activity feedback intervention. This approach is unique in that while other investigations have characterized physical activity after TKA, we were interested in the ability to alter physical activity levels following TKA. Feasibility of the physical activity feedback intervention was determined using a set of criteria. Specifically, we expected to observe >80% of the weekly goals to be achieved. Furthermore, data regarding objectively measured physical activity and performance-based functional performance (assessed by the 6 minute walk, timed up and go, and 10 meter walk tests) were collected. Finally, characteristics of responders (defined as those participants that increased their physical activity over their 12-week involvement) and nonresponders (defined as those participants that did not increase or decreased their physical activity over their 12-week involvement) are reported to better inform potential differences between these groups for future interventions.
METHODS
Study Design
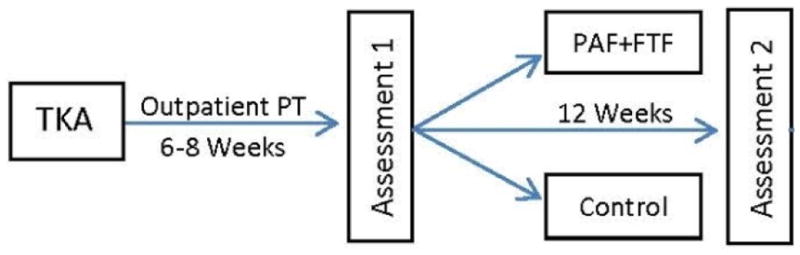
Participants aged 50–75 who underwent unilateral TKA were recruited from the Denver, Colorado, metropolitan area. We conducted initial assessments with participants after they completed outpatient TKA rehabilitation (six to eight weeks after TKA surgery). During this visit, participants performed several objective functional performance assessments in a clinical research laboratory and were provided a physical activity monitor with instruction on use. Upon completion of the seven-day physical activity monitoring period, participants were randomized to the physical activity feedback or control group. The physical activity feedback intervention involved real-time physical activity monitoring using a device to provide activity feedback directly to participants in combination with participant group meetings held monthly during the 12-week intervention for the purposes of mutual support in attaining physical activity goals. The control group represented the current standard of care post-TKA, though we did not collect patient or clinician logs of therapy performed. Participants returned for testing 12 weeks after beginning the intervention (Fig. 1). All assessments were performed at both test sessions. The XXXX Institutional Review Board approved all study activities, and all participants provided written informed consent prior to study participation (NCT02075931).
Figure 1.
Physical Activity Intervention and Attention Control
Following TKA surgery, standard inpatient and home rehabilitation programs were implemented for all participants to improve mobility and activities of daily living. Participants randomized to the physical activity feedback program were prescribed a daily physical activity goal and oriented to the use of the Fitbit real-time physical activity wearable sensor (Fitbit Zip, San Francisco, CA) by which participants were able to self-assess their daily level of physical activity with visual feedback. All data were simultaneously transmitted to the research staff. Each week, a researcher called each participant to address and alleviate any participant-reported barriers to physical activity goal achievement. Physical activity goals were modified weekly, as necessary, and the goal of the research staff was to negotiate a physical activity goal of 5% greater than the previous week when compared to the mean physical activity performed during the previous week. The goal of 5% increase was used as it is defined as a ‘moderate’ increase in physical activity.{Croteau, 2004 #35}
Face-to-face participant group meetings hosted in a meeting space central to participants’ locations were also held monthly in the community during the intervention for the purposes of mutual support in attaining physical activity level goals. At each meeting, participants received a newsletter that included study updates, physical activity guidelines, and notes regarding future meetings. The control program (usual care, no intervention) allowed for assessment of physical activity and functional performance. The control program involved weekly phone meetings to monitor participants’ health status, but without physical activity feedback and face-to-face group meetings.
Feasibility Assessment
Feasibility was assessed through participant retention (percentage of participants finishing 12-week involvement; mean ± SD), intervention adherence (percentage days of successful real-time physical activity data collection in physical activity feedback; mean ± SD), and dose goal attainment (percentage of participants meeting weekly physical activity dose goals). For the intervention to be feasible, we expected >80% retention, >90% adherence, and >80% of the weekly goals to be achieved in the intervention group. These aspects of the feasibility are critical to the potential efficacy and effectiveness of future interventions aimed to increase physical activity (Basu, Kennedy, Tocque, & Jones, 2014).
Physical Activity Assessment
Participants wore a GT3X Actigraph Activity Monitor (Actigraph GT3X, Actigraph, LLC, Fort Walton Beach, FL) for one week to quantify physical activity at both testing points (Figure 1). The Actigraph activity monitor uses triaxial, solid state accelerometers to measure the intensity of activity, walking pace, distance traveled, and step count. The Actigraph allows for quantitative analysis of activity levels when participants are not being supervised, thereby decreasing the discrepancy seen between subjective participant activity reports and quantitative measurements taken by research staff. The Actigraph has been validated against numerous other market versions of accelerometers.(de Vries, Bakker, Hopman-Rock, Hirasing, & van Mechelen, 2006; Kelly LA, 2004; Leenders, Nelson, & Sherman, 2003) When validated against a standard pedometer, the Actigraph was found to be more accurate than the pedometer at gauging steps (98.9% accurate with p<0.05).(Le Masurier & Tudor-Locke, 2003) All presented physical activity data were those collected from the Actigraph. No comparisons were made between step counts as measured by the Actigraph and Fitbit.
Functional Performance Testing
Measures of functional performance included the timed-up-and-go test (TUG), six-minute walk test (6MW), and four-meter walk test. The TUG measures the time it takes a participant to rise from an arm chair (seat height of 46 cm), walk three meters, turn and return to sitting in the same chair without physical assistance.(Podsiadlo & Richardson, 1991) This test has excellent inter-rater (ICC=0.99) and intra-rater reliability (ICC=0.99), as measured in a group of 60 functionally disabled older adults (mean age 80 years).(Podsiadlo & Richardson, 1991) The 6MW test measures the distance walked in six minutes. This test was developed and used extensively to measure endurance.(Steffen, Hacker, & Mollinger, 2002) The test has been validated to measure functional mobility following TKA.{Moffet, 2004 #30;Parent, 2002 #11;Parent, 2003 #10;Ko, 2013 #34} The 6MW test has been demonstrated to have excellent test-retest reliability, with intraclass correlation coefficients from 0.95–0.97, and a low coefficient of variation (10.4%). (Montgomery & Gardner, 1998; Steffen et al., 2002) The four meter walk test was used to quantify the time required by a participant to walk four meters at their self-selected, typical gait speed. Gait speed was calculated from the four meter walk test data.
Analysis
Physical Activity and Functional Performance Outcomes
Baseline, 12-week, and change scores were calculated for all participants, by group, and by responder/nonresponder subgrouping (mean ± SD, CI). Measurements of retention rate, intervention adherence, and activity dose goal achievement were used to assess feasibility. The retention rate cutoff of greater than 80% was assessed as the ratio of the number of participants who completed the 12-week assessment over the number of participants enrolled. The adherence rate (in the physical activity feedback group) cutoff of greater than 90% was assessed as the ratio of the number of weeks that the Fitbit wearable sensor and tablet application were used over the total number of weeks. Use of the Fitbit sensor was assessed by noting daily wear time (≥ 12 hours representing a valid day). Dose goal cutoff of 80% was assessed as the ratio of the total number of participants achieving their goals over the total number of participants, for each week of the intervention. The total dose goal achievement was presented for each week of the intervention (Week1 to Week 12) and over the entire intervention, with the entire intervention percentage used as the assessment of feasibility. Characteristics of responders and nonresponders were also described wherein responders were classified as those participants, in the physical activity feedback and control groups, who demonstrated an increase in their physical activity at the 12-week assessment when compared to the baseline assessment, and nonresponders were classified as those participants who either decreased or did not increase or decrease their physical activity over the same time frame.
Results
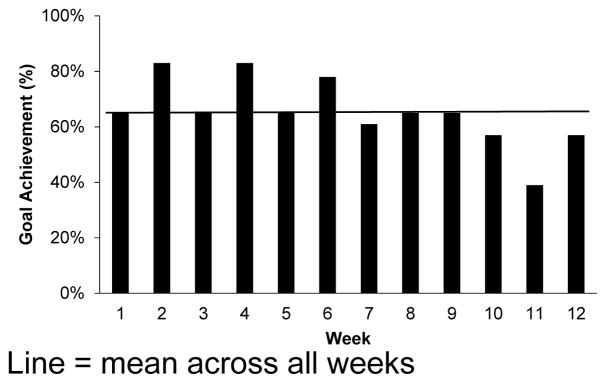
A total of 45 participants (22 physical activity feedback, 23 control) with TKA participated in this feasibility study. Demographic characteristics and feasibility outcomes are shown in Table 1. Participants were anthropometrically similar. Retention rate was greater than 90% overall in both groups, with no loss of participants to follow-up (100% retention) in the intervention group. Adherence to daily use of the Fitbit sensor and peripheral monitors was 92.3% as tracked by remote assessment of use by the study coordinator. Dose goal attainment of the individualized weekly goals was attained 65% of the time overall, with 65% of participants achieving their goals in the first week of intervention and 57% achieving weekly goals in Week 12 (Figure 2). Retention rate in the control group (85%) was lower than the intervention group, with 4 participants lost to follow-up due to moving, change in employment, and lack of time availability.
Table 1.
Demographics
| Control (n = 23) | Intervention (n = 22) | |
|---|---|---|
| Age (y) | 64 ± 6 | 63 ± 7 |
| Sex (m/f) | 12/11 | 9/13 |
| Mass (kg) | 81.1 ± 21.1 | 86.8 ± 17.6 |
| BMI | 26.4 ± 8.6 | 29.9 ± 10.7 |
| Retention (%) | 83 | 100 |
| Adherence (%) | N/A | 92.3 ± 7.9 |
Values are presented as mean ± SD where applicable.
Figure 2.
Participant Goal Achievement
Physical activity and functional performance values are presented for both groups in Table 2. Both groups demonstrated physical activity and functional performance gains during the course of study involvement. These results are also presented as percent change at 12 weeks from baseline in Table 3. The intervention group increased physical activity (daily step count) by 20% (1163 steps/d). Anthropometric, physical activity, and functional performance values, broken down by responder/nonresponder classification are presented in Table 4. Interestingly, responders demonstrated apparently greater functional performance (TUG, gait speed, 6MWT) and BMI at baseline, while baseline physical activity was lower. These may suggest either a greater level of functional capacity at baseline and/or greater room for improvement in terms of physical activity.
Table 2.
Raw Values for Outcome Measures Across Time
| Raw | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Control | Physical Activity Feedback | ||||||||||
| Baseline | 12 wk | Baseline | 12 wk | Baseline | 12 wk | |||||||
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | |
| Physical Activity (steps/d) | 5361 ± 2384 | (4129, 5893) | 6137 ± 3039 | (4183, 6399) | 5011 ± 2038 | (4129, 5893) | 5291 ± 2298 | (4183, 6399) | 5754 ± 2714 | (4620, 6888) | 6917 ± 3445 | (5783, 8052) |
| TUG (s) | 9.25 ± 2.44 | (7.91, 9.61) | 8.91 ± 2.44 | (7.19, 8.98) | 8.76 ± 1.94 | (7.91, 9.61) | 8.09 ± 1.91 | (7.19, 8.98) | 9.17 ± 2.77 | (7.94, 10.34) | 8.23 ± 4.42 | (7.10, 9.37) |
| Gait Speed (m/s) | 1.57 ± 0.44 | (1.13, 2.01) | 1.69 ± 0.35 | (1.34, 2.03) | 1.52 ± 0.35 | (1.18, 1.86) | 1.61 ± 0.54 | (1.08, 2.14) | 1.66 ± 0.33 | (1.33, 1.98) | 1.71 ± 0.37 | (1.35, 2.08) |
| 6MWT (m) | 460 ± 106 | (428, 516) | 515 ± 108 | (480, 574) | 466 ± 98 | (428, 516) | 521 ± 96 | (480, 574) | 455 ± 115 | (408, 512) | 510 ± 122 | (458, 574) |
Values are presented as mean ± SD where applicable.
Table 3.
Percentage Changes for Outcome Measures Across Time
| Percentage Change | ||||||
|---|---|---|---|---|---|---|
| All | Control | Physical Activity Feedback | ||||
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | Mean ± SD | 95% CI | |
| Physical Activity | 17.37 ± 40.60 | (4.56, 30.18) | 8.69 ± 36.14 | (−8.73, 26.11) | 20.24 ± 42.79 | (7.43, 43.21) |
| TUG | −6.85 ± 11.02 | (−10.38, −3.33) | −4.38 ± 10.04 | (−9.07, 0.32) | −0.98 ± 0.08 | (−14.78, −3.88) |
| Gait Speed | 6.06 ± 14.01 | (1.57, 10.54, ) | 5.26 ± 12.75 | (0.70, 11.23) | 6.85 ± 14.08 | (0.04, 14.08 |
| 6MWT | 13.81 ± 32.82 | (3.17, 24.45) | 6.89 ± 7.64 | (3.17, 10.54) | 20.47 ± 50.23 | (−0.53, 41.38) |
Values are presented as mean ± SD where applicable.
Table 4.
Subgroup Characteristics
| Nonresponders (n = 19) | Responders (n = 26) | |||
|---|---|---|---|---|
| Mean ± SD | 95% CI | Mean ± SD | 95% CI | |
| Age (y) | 64 ± 6 | (61, 67) | 65 ± 6.7 | (62, 67) |
| Sex (m/f) | 7/12 | N/A | 14/12 | N/A |
| Mass (kg) | 76.38 ± 18.49 | (66.87, 85.88) | 88.77 ± 18.73 | (81.21, 96.34) |
| BMI | 24.28 ± 11.55 | (17.89, 30.68) | 31.23 ± 6.86 | (27.92, 34.53) |
| Group (Physical Activity Feedback/Control) | 6/13 | N/A | 16/10 | N/A |
| Baseline Physical Activity (steps/d) | 5760 ± 2843 | (4390, 7130) | 5070 ± 1994 | (4264, 5875) |
| Baseline TUG (s) | 9.46 ± 3.25 | (7.63, 10.75) | 8.79 ± 1.51 | (8.17, 9.40) |
| Baseline Gait Speed (m/s) | 1.51 ± 0.43 | (1.09, 1.93) | 1.63 ± 0.48 | (1.16, 2.11) |
| Baseline 6MWT (m) | 459 ± 143 | (388, 530) | 471 ± 76 | (440, 502) |
Values are presented as mean ± SD where applicable.
Discussion
The present study evaluated the feasibility of performing the physical activity feedback intervention with a concurrent control group as a randomized controlled trial. This evaluation will help in the design of future trials aimed to address the problem of low physical activity after TKA. Based on our findings, we believe that implementation of such an intervention in a future trial is feasible, based on retention rate, adherence, and trends seen in physical activity and functional performance. Dose goal attainment was below our set cutoff of 80%, indicating that weekly dose goals may have been set too high for some participants.
While the retention rate of the physical activity feedback group was excellent, the retention rate of the control group could be improved. A recent investigation utilized a similar physical activity intervention over the course of 12 weeks in women after childbirth. In this study, 32 of the 35 participants randomized to the intervention group completed the study while 34 of the 35 participants randomized to the control group completed (Maturi et al., 2011). This rate of attrition is similar to several other previous studies (Ashe et al., 2015; Lombard, Deeks, Jolley, & Teede, 2009; Wing et al., 2006). Similarly, our rate of adherence was similar to a previous study investigating the use of wearable sensors to increase physical activity. Cadmus-Bertrand, et al. achieved a wear time adherence rate of 95% (Cadmus-Bertram, Marcus, Patterson, Parker, & Morey, 2015). Based on the results of these studies, we believe our retention and adherence rates would support a sufficiently powered efficacy study.
The attainment of dose goals is another indication of feasibility. In our study, we expected that over 80% of participants would reach their weekly dose goals, as the intention of setting the weekly goals was to advance participants’ activity in a manner that was realistically conservative. As a guideline, research staff suggested a 5% improvement from the previous week’s physical activity level for each participant. However, weekly goal achievement was 65 ± 12% (Figure 2). Our results suggest that during the time frame of this study (the 12 weeks immediately after conventional rehabilitation), a 5% gain in weekly activity is too great of an expectation for some participants and that other participant-specific considerations should be examined in the future to improve goal attainability. For example, there were some relatively low dose goal adherence measures in later weeks (e.g., Week 11: 39%). It is likely that goals early on were easier to achieve, but became more difficult as intervention progressed. It has been suggested that self-efficacy is a critical factor for engaging in physical activity despite the presence of arthritis.(Knittle et al., 2011) Improvement of self-efficacy can be obtained with training of goal setting and eliciting participant-specific considerations through structured use of established interview techniques, such as motivational interviewing.(Georgopoulou, Prothero, Lempp, Galloway, & Sturt, 2016; Miller & Rollnick, 2002) It is also possible that the timing of the intervention may affect the expected rate of physical activity gain. For example, the physical activity feedback intervention was initiated after graduation from post-TKA rehabilitation. Integration of the physical activity feedback within the conventional rehabilitation time frame could potentially capitalize on participants’ motivation for improvement earlier after surgery.
Physical activity in the intervention group increased by approximately 20% (1163 steps/d). No guidelines exist regarding clinically meaningful differences in patients with TKA. This increase aligns with a previous study that investigated physical activity in similar populations. Brandes, et al. found an increase of ~1,000 steps/d patients with TKA (Brandes et al., 2011). Such a clinically meaningful physical activity improvement in other chronic health condition populations provides further context of physical activity change for participants with TKA. Participants with fibromyalgia, for example, demonstrate improvements in a variety of psychological and functional performance measures when an improvement of 1,000 steps/d is achieved (Kaleth, Slaven, & Ang, 2014). Similarly, 600–1000 additional daily steps taken were found to be beneficial in participants with COPD (Demeyer et al., 2016). These findings suggest that the additional physical activity performed by the physical activity feedback group in our current study may provide clinically important change. Though this feasibility study was not powered to assess efficacy, when comparing group changes with regard to physical activity level, this increase in physical activity aligns with previous studies that used similar interventions (Ashe et al., 2015; Choi, Lee, Vittinghoff, & Fukuoka, 2016; Maturi et al., 2011; Thorup et al., 2016). For example, Ashe, et al. were able to elicit a 26% (1,204 steps/day) increase in steps taken per day by using a Fitbit sensor in combination with physical activity prescription in healthy, inactive women aged 55–70 years over the course of three months (Ashe et al., 2015). Choi, et al. found a 17% (1,096 steps/day) increase in physical activity using a similar Fitbit sensor based intervention in inactive pregnant women (Choi et al., 2016). As our apparent magnitude of change is greater than these previous studies, we believe that our methodology is very promising when considering future efficacy investigations aimed to increase physical activity in orthopedic populations. These studies, in turn, are likely to better inform clinical interventions aimed to reduce participant adiposity and risk of a variety of maladaptive health conditions.
Limitations and Future Directions
There are several items identified in this study that can be considered in the design of future studies examining PA intervention following TKA. First, the retention rate in the control group was 83% and could be improved. In future studies, educational materials not related to physical activity (e.g., nutrition, strength) could be provided to participants. This additional engagement, in turn, may provide for greater participant engagement and enhanced retention of participants randomized to the attention control group. Concurrent health conditions, including lower limb joint dysfunction, should also be assessed in future studies as there are multiple comorbidities that may affect participants’ response to the intervention. Third, this pilot study included a small sample size with outcomes susceptible to individual influential cases. For example, the percent change in 6MWT score (Table 3) gives the appearance of greater group differences than group mean changes (Table 2), secondary to several intervention group participants who substantially increased their distance travelled. Fourth, though no statistical comparisons were performed regarding responders versus nonresponders, both the responders appear to have greater BMI and lower baseline physical activity than the non-responders. The influence of BMI and baseline physical activity should be further investigated as potential predictors of intervention response. In the same regard, a lack of apparent relation between change in functional performance and physical activity outcomes is equally interesting. Future research in this area could include measures of behavioral and psychosocial variables that may impact physical activity response beyond improvement in physical capacity (i.e., functional performance).
Adherence in the intervention group is also a target of refinement. While we believe that an adherence rate of 92.3% is strong for a feasibility study, our experiences suggest that this could be improved. First of all, monitoring of incoming physical activity data was performed weekly during collection. In several cases, the physical activity monitor did not collect data for several days due to battery discharge, thereby decreasing the apparent adherence rate. We suggest that daily monitoring of incoming physical activity data would better allow researchers to reduce missing data. A second method of increasing adherence would be use of a different real-time physical activity feedback device. The Fitbit Zip sensors used in the present study use disposable button-style batteries. When completely discharged, not all participants had the physical ability to replace the battery without assistance from the research staff. In several cases, this resulted in several days of missing physical activity data. A rechargeable device could provide an adequate solution as participants could simply charge the devices when not in use (e.g., while sleeping). This type of limitation may be inherent to the study design, however, as our rate of adherence was superior to a previous study investigating adherence using a Fitbit physical activity wearable sensor (Cadmus-Bertram et al., 2015). This previous study found adherence to be approximately 79%.
Conclusion
The present investigation found a physical activity feedback intervention to be a potentially feasible adjunct to conventional rehabilitation for participants with TKA. Both the retention rate and adherence (for the physical activity feedback group) were deemed acceptable for the purposes of feasibility. The lower than expected rate of dose goal attainment indicates that goal-setting parameters could be better aligned with participant-specific considerations. The retention rate in the physical activity feedback group was numerically greater than that of the control group, and intervention adherence was deemed acceptable in the physical activity feedback group. The feasibility outcomes along with the 20% increase in physical activity in the intervention group suggests the promise of further study targeting physical activity improvement after TKA.
Acknowledgments
Funding: This research was supported by NIH T32 AG000279 and K12 HD055931.
References
- Ashe MC, Winters M, Hoppmann CA, Dawes MG, Gardiner PA, Giangregorio LM, … McKay HA. “Not just another walking program”: Everyday Activity Supports You (EASY) model-a randomized pilot study for a parallel randomized controlled trial. Pilot Feasibility Stud. 2015;1(4):1–12. doi: 10.1186/2055-5784-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes Before and After Total Knee Arthroplasty Compared to Healthy Adults. Journal of Orthopaedic & Sports Physical Therapy. 2010;40(9):559–567. doi: 10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu A, Kennedy L, Tocque K, Jones S. Eating for 1, Healthy and Active for 2; feasibility of delivering novel, compact training for midwives to build knowledge and confidence in giving nutrition, physical activity and weight management advice during pregnancy. BMC Pregnancy Childbirth. 2014;14:218. doi: 10.1186/1471-2393-14-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandes M, Ringling M, Winter C, Hillmann A, Rosenbaum D. Changes in physical activity and health-related quality of life during the first year after total knee arthroplasty. Arthritis Care Res (Hoboken) 2011;63(3):328–334. doi: 10.1002/acr.20384. [DOI] [PubMed] [Google Scholar]
- Bruun-Olsen V, Heiberg KE, Wahl AK, Mengshoel AM. The immediate and long-term effects of a walking-skill program compared to usual physiotherapy care in patients who have undergone total knee arthroplasty (TKA): a randomized controlled trial. Disabil Rehabil. 2013 doi: 10.3109/09638288.2013.770084. [DOI] [PubMed] [Google Scholar]
- Cadmus-Bertram L, Marcus BH, Patterson RE, Parker BA, Morey BL. Use of the Fitbit to Measure Adherence to a Physical Activity Intervention Among Overweight or Obese, Postmenopausal Women: Self-Monitoring Trajectory During 16 Weeks. JMIR Mhealth Uhealth. 2015;3(4):e96. doi: 10.2196/mhealth.4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J, Lee JH, Vittinghoff E, Fukuoka Y. mHealth Physical Activity Intervention: A Randomized Pilot Study in Physically Inactive Pregnant Women. Matern Child Health J. 2016;20(5):1091–1101. doi: 10.1007/s10995-015-1895-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries SI, Bakker I, Hopman-Rock M, Hirasing RA, van Mechelen W. Clinimetric review of motion sensors in children and adolescents. J Clin Epidemiol. 2006;59(7):670–680. doi: 10.1016/j.jclinepi.2005.11.020. S0895-4356(06)00017-5 [pii] [DOI] [PubMed] [Google Scholar]
- Demeyer H, Burtin C, Hornikx M, Camillo CA, Van Remoortel H, Langer D, … Troosters T. The Minimal Important Difference in Physical Activity in Patients with COPD. PLoS One. 2016;11(4):e0154587. doi: 10.1371/journal.pone.0154587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol. 2006;33(11):2271–2279. [PubMed] [Google Scholar]
- Dunlop DD, Song J, Semanik PA, Sharma L, Chang RW. Physical activity levels and functional performance in the osteoarthritis initiative: a graded relationship. Arthritis Rheum. 2011;63(1):127–136. doi: 10.1002/art.27760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgopoulou S, Prothero L, Lempp H, Galloway J, Sturt J. Motivational interviewing: relevance in the treatment of rheumatoid arthritis? Rheumatology (Oxford) 2016;55(8):1348–1356. doi: 10.1093/rheumatology/kev379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaleth AS, Slaven JE, Ang DC. Does increasing steps per day predict improvement in physical function and pain interference in adults with fibromyalgia? Arthritis Care Res (Hoboken) 2014;66(12):1887–1894. doi: 10.1002/acr.22398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly LA, Reilly JJ, Fairweather SC, Barrie S, Grant S, Paton JY. Comparison of Two Accelerometers for Assessment of Physical Activity in Preschool Children. Pediatric Exercise Science. 2004;16(4):324–333. [Google Scholar]
- Knittle KP, De Gucht V, Hurkmans EJ, Vlieland TP, Peeters AJ, Ronday HK, Maes S. Effect of self-efficacy and physical activity goal achievement on arthritis pain and quality of life in patients with rheumatoid arthritis. Arthritis Care Res (Hoboken) 2011;63(11):1613–1619. doi: 10.1002/acr.20587. [DOI] [PubMed] [Google Scholar]
- Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- Le Masurier GC, Tudor-Locke C. Comparison of pedometer and accelerometer accuracy under controlled conditions. Med Sci Sports Exerc. 2003;35(5):867–871. doi: 10.1249/01.MSS.0000064996.63632.10. [DOI] [PubMed] [Google Scholar]
- Leenders NY, Nelson TE, Sherman WM. Ability of different physical activity monitors to detect movement during treadmill walking. Int J Sports Med. 2003;24(1):43–50. doi: 10.1055/s-2003-37196. [DOI] [PubMed] [Google Scholar]
- Lombard C, Deeks A, Jolley D, Teede HJ. Preventing weight gain: the baseline weight related behaviors and delivery of a randomized controlled intervention in community based women. Bmc Public Health. 2009;9 doi: 10.1186/1471-2458-9-2. Artn 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maturi MS, Afshary P, Abedi P. Effect of physical activity intervention based on a pedometer on physical activity level and anthropometric measures after childbirth: a randomized controlled trial. BMC Pregnancy Childbirth. 2011;11:103. doi: 10.1186/1471-2393-11-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller William R, Rollnick Stephen. Motivational interviewing : preparing people for change. 2. New York: Guilford Press; 2002. [Google Scholar]
- Moffet H, Collet JP, Shapiro SH, Paradis G, Marquis F, Roy L. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: A single-blind randomized controlled trial. Arch Phys Med Rehabil. 2004;85(4):546–556. doi: 10.1016/j.apmr.2003.08.080. [DOI] [PubMed] [Google Scholar]
- Montgomery PS, Gardner AW. The clinical utility of a six-minute walk test in peripheral arterial occlusive disease patients. J Am Geriatr Soc. 1998;46(6):706–711. doi: 10.1111/j.1532-5415.1998.tb03804.x. [DOI] [PubMed] [Google Scholar]
- Parent E, Moffet H. Comparative responsiveness of locomotor tests and questionnaires used to follow early recovery after total knee arthroplasty. Arch Phys Med Rehabil. 2002;83(1):70–80. doi: 10.1053/apmr.2002.27337. [DOI] [PubMed] [Google Scholar]
- Parent E, Moffet H. Preoperative predictors of locomotor ability two months after total knee arthroplasty for severe osteoarthritis. Arthritis Rheum. 2003;49(1):36–50. doi: 10.1002/art.10906. [DOI] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- Riddle DL, Singh JA, Harmsen WS, Schleck CD, Lewallen DG. Clinically important body weight gain following knee arthroplasty: a five-year comparative cohort study. Arthritis Care Res (Hoboken) 2013;65(5):669–677. doi: 10.1002/acr.21880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82(2):128–137. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- Thorup C, Hansen J, Gronkjaer M, Andreasen JJ, Nielsen G, Sorensen EE, Dinesen BI. Cardiac Patients’ Walking Activity Determined by a Step Counter in Cardiac Telerehabilitation: Data From the Intervention Arm of a Randomized Controlled Trial. J Med Internet Res. 2016;18(4):e69. doi: 10.2196/jmir.5191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35(6):725–740. doi: 10.1139/H10-079. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Lutes L. Why do pedometers work?: a reflection upon the factors related to successfully increasing physical activity. Sports Med. 2009;39(12):981–993. doi: 10.2165/11319600-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006;355(15):1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- Zeni JA, Jr, Snyder-Mackler L. Most patients gain weight in the 2 years after total knee arthroplasty: comparison to a healthy control group. Osteoarthritis Cartilage. 2010;18(4):510–514. doi: 10.1016/j.joca.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]