Abstract
Despite well-documented benefits of colorectal cancer (CRC) screening, African Americans are less likely to be screened and have higher CRC incidence and mortality than Whites. Emerging evidence suggests medical mistrust may influence CRC screening disparities among African Americans. The goal of this systematic review was to summarize evidence investigating associations between medical mistrust and CRC among African Americans, and variations in these associations by gender, CRC screening type, and level of mistrust. MEDLINE, CINAHL, Web of Science, PsycINFO, Google Scholar, Cochrane Database, and EMBASE were searched for English-language articles published from January 2000 to present. 27 articles were included for this review (15 quantitative, 11 qualitative and 1 mixed methods study). The majority of quantitative studies linked higher mistrust scores with lower rates of colorectal screening among African Americans. All studies examined mistrust at the physician level, but no studies analyzed mistrust at an organizational level (i.e. healthcare systems, insurance, etc.). Quantitative differences in mistrust and CRC screening by gender were mixed, but qualitative studies highlighted fear of experimentation and intrusiveness of screening methods as unique themes among African American men. Limitations include heterogeneity in mistrust and CRC measures, and possible publication bias. Future studies should address methodological challenges found in this review, such as limited use of validated and reliable mistrust measures, examination of colorectal screening outcomes beyond beliefs and intent, and a more thorough analysis of gender roles in the cancer screening process.
Keywords: medical mistrust, African Americans, colorectal cancer, preventive screening
Background
Colorectal cancer (CRC) is the second leading cause of cancer-related deaths in the United States, and approximately 51,000 Americans die each year from this disease (1). National guidelines from the U.S. Preventive Services Task Force and the American Cancer Society recommend screening for CRC using fecal occult blood testing, sigmoidoscopy, or colonoscopy among average risk adults (2). Adherence to these screening recommendations, which are in place for asymptomatic individuals between 50 and 75 years old, has been associated with a net reduction in CRC incidence and survival rate among the general population. However, these commonly adopted recommendations do not offer targeted strategies for individuals at highest risk for developing colorectal cancer. African Americans have a higher incidence of and mortality from CRC, and also experience greater morbidity, and lower quality of health care compared with non-Hispanic Whites (3, 4). Given these disparities in outcomes, access and timely use of approved screening procedures is of critical importance among African Americans compared to the general population.
In fact, despite the life-saving potential and enhanced net benefits of screening, approximately 27.7% of Americans age 50–75 have not received timely screening for colorectal cancer (5) and African Americans have a lower uptake of CRC screening than non-Hispanic whites (6–8). Racial disparities in CRC screening adherence are further exacerbated by gender, with African American men exhibiting a lower likelihood of being screened than African American women (9, 10). Economic and interpersonal factors associated with reduced uptake of CRC screening among African American have been well documented in previous empirical studies and include poor patient/provider communication, and socioeconomic challenges, such as insurance status, SES, and cost, in obtaining quality CRC screening (11, 12). However, emerging literature also identifies psychosocial influences, such as cultural norms, differential perceptions of risk, and negatives attitudes towards healthcare, as primary barriers to receiving timely colorectal cancer screening in the African American population (6, 13). Among these factors, lack of trust in the healthcare system remains a paramount psychosocial influence for reduced uptake of cancer screening in the United States (14). Mistrust of the healthcare system and its providers, also known as medical mistrust, is associated with lower health services utilization among African American patients(15, 16) and is a widely cited attitudinal barrier to CRC screening and treatment seeking (17).
Many studies consider mistrust from an interpersonal perspective, assessing this construct specifically within the patient-provider relationship. However, medical mistrust also reflects a belief system that, because of historical and lived experiences, patients are guarded about organizational-level policies and health care system procedures (18). Investigations measuring medical mistrust at the physician and organizational levels and their associations with cancer screening appear to yield conflicting results (19, 20). Organizational-level mistrust has also only recently received focused empiric attention and its impact on cancer screening has not been thoroughly explored. As a result, less is known about its contribution to poor CRC screening uptake among African Americans. In addition, as African American men report higher levels of medical mistrust than African American women (21, 22) it is important to synthesize what is known about gender differences in associations between medical mistrust and CRC screening.
The primary goal of this study is to systematically review studies investigating associations between medical mistrust, at both the physician and organizational level, and uptake of colorectal screening among African Americans. To examine whether medical mistrust has a significant influence on colorectal cancer screening patterns among African Americans, we reviewed empirical literature assessing the role of mistrust in providers or the health system to determine whether this indicator has an impact on colorectal screening utilization, beliefs, and attitudes among African Americans in the United States. Additionally, we examined gender differences in medical mistrust as well as preferred methods of CRC screening (e.g. FOBT, colonoscopy, etc.) within this population. We specifically address the following key questions:
KQ1: How does mistrust of health care providers and/or organizations impact colorectal cancer screening behavior among African Americans?
KQ2: How does medical mistrust differentially impact colorectal screening patterns among African American men and women?
KQ3: How does medical mistrust impact the types of colorectal screening African Americans receive (e.g., FOBT, colonoscopy, or flexible sigmoidoscopy)?
KQ4: Is there a differential impact on colorectal cancer screening behavior depending on whether mistrust is measured at the individual provider or organization level?
Methods
An a priori study protocol was submitted to PROSPERO to guide implementation of the review. Original, empirical studies investigating medical mistrust and colorectal cancer screening outcomes published from January 2000 to November 2016 were examined for this study. Studies with a sample of African American adult participants and a measure or theme related to physician or health organization mistrust were included in our study. The primary outcome of interest was CRC screening outcomes (i.e., screening—receipt: yes/no, beliefs, knowledge, and attitudes towards screening). We searched MEDLINE (Pubmed), CINAHL, Web of Science, PsycINFO, Google Scholar, Cochrane Database, and EMBASE. Search strategies for each database were developed in coordination with a research librarian specializing in systematic reviews. We limited searches to articles published in English and using search terms and Medical Subject Headings (MeSH) terms related to colorectal cancer, African Americans, and mistrust (See Appendix 1). We also included search terms for various types of colorectal screening methods (i.e. FOBT, colonoscopy, etc.). Additional studies were also included by examining reference lists of included studies.
Two investigators independently screened abstracts and titles for inclusion to the full text review. Full text articles were screened by the same two investigators. Discrepancies between investigators were resolved by consensus at team meetings. We included studies using the following criteria: Studies must (1) Only include human subjects and be published in English; (2) Empirical or analytical studies; (3) Conducted in the United States; (4) Published between January 2000 (two years before the USPSTF’s CRCS recommendations for screening starting at age 50 or older were published) and November 2016; (5) Include African Americans; (6) Discuss changes in colorectal screening outcomes. Alternatively, studies were excluded if they: (1) Were commentaries or non-empirical studies; (2) Focus exclusively on foreign born blacks or other racial/ethnic groups; (3) Focus solely on policy reviews and implementation
Subgroup analyses were pre-specified in the Key Questions. The impact of medical mistrust on colorectal cancer screening rates was stratified by gender. This analysis was conducted to clarify gender differences in associations between medical mistrust and CRC screening outcomes. Additionally, we stratified data by preferred colorectal cancer screening type (i.e. FOBT, colonoscopy, etc.). Finally, articles examining medical mistrust of providers and those measuring mistrust of the health care system were compared to determine if differences emerged in their association with CRC screening.
Adherence to colorectal screening guidelines (e.g. completed a colonoscopy/FOBT/etc. or not) was the primary outcome measure of this study. We also included studies that assessed attitudes or beliefs regarding CRC screening, such as intention to screen. We used a descriptive approach to summarize study characteristics and outcomes for all research questions. For each quantitative article, we examined strength of association between medical mistrust and CRC screening. For qualitative studies, we identified common themes associated with medical mistrust within participant responses. Findings disaggregated by gender and level of mistrust (e.g. provider or organizational) were also highlighted in order to assess Key Questions 2 and 4.
Results
Study Selection
Figure 1 provides details regarding the article selection and inclusion process. The overall database search yielded 777 articles. We included an additional 19 articles relevant to our research questions from reference lists of included studies. After adjusting for duplicates, a total of 598 original articles were yielded from the initial database search, and the title and abstracts of these articles were reviewed. 476 articles were excluded during the title and abstract screening because they did not meet our inclusion criteria. We retrieved 122 full-text articles for further review and excluded another 95 articles, leaving 27 articles representing 26 unique studies for further analysis. None of the studies obtained from our manual search of reference lists from our included studies were eligible for inclusion. Of the 27 included articles, 15 were quantitative, 11 were qualitative, and one was mixed methods.
Figure 1.
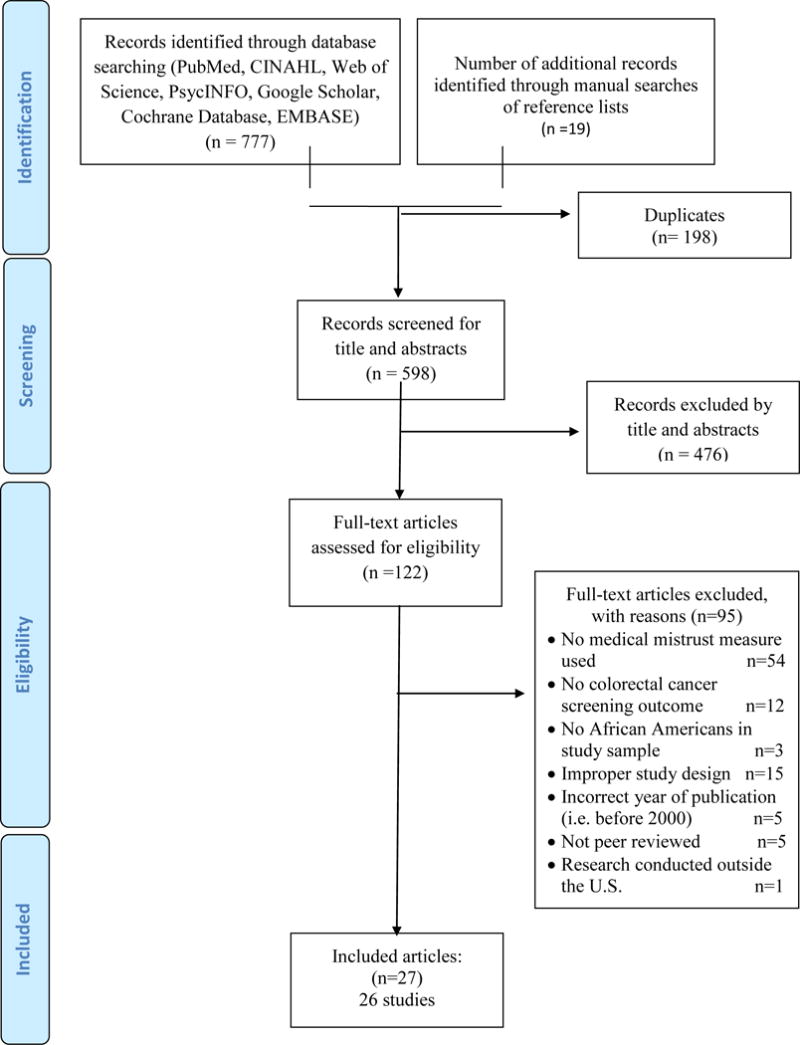
Prisma Diagram of Included Studies
Study characteristics of included studies
Characteristics of included studies are described in Table 1. The majority (37%) of studies were cross-sectional designs, followed by focus groups (26%). Two studies were randomized control trials. Sample sizes of the included studies ranged from 14 to 41 participants for qualitative studies, and 43 to 961 participants for quantitative studies. The majority of articles (42%) focused on FOBT, colonoscopy, and sigmoidoscopy and these screening outcomes were primarily assessed through self-reported surveys measuring past screening behavior or intention to screen. Only 2 articles measured CRC screening directly through methods such as chart audits or FOBT card return. While all articles focused on mistrust measured at the physician level, 15 articles (56%) measured both physician and organization levels of mistrust. Other outcomes addressed in studies included: knowledge of CRC risk factors, cancer fatalism, physician recommendation, and self-rated health. The majority of articles (60%) included only African American participants in the sample, and most articles (56%) sampled individuals who were 50 years of age and older. However, 11 articles included participants who were younger than age 50, and one of these articles assessed CRC screening attitudes and beliefs among participants that were 18 years or younger. Of note, one article did not specify the age of participants included in the study (23). However, 6 articles (23%) sampled individuals who were not up to date with colorectal cancer screening or who were currently eligible for their next regular screening. Two articles (8%) sampled individuals who were first degree relatives of someone diagnosed with colorectal cancer.
Table 1.
Summary Characteristics of Included Studies
| Author(s) | Method Type |
Study Design Type |
Sample Characteristics |
% African Americans |
Risk subgroup |
Sample Size |
Type(s) of Colorectal Cancer Addressed |
Level of Trust Measured |
Measure of Trust |
Measure of Colorectal Cancer Screening Behavior |
|---|---|---|---|---|---|---|---|---|---|---|
| Bass et. al, 2011 | Qualitative | Focus groups | African American patients ages 50+ with varying CRC screening status | 100% | 50 and older | 23 | FOBT and Colonoscopy | Physician | N/A | Ever screened vs. Never Screened |
| Bastani, et. al., 2001 | Mixed methods | Telephone survey and focus groups | Hispanic, African American, Asian, and White first-degree relatives of an individual diagnosed with CRC | 48% (focus group); 25% (telephone survey) | 50 and older; first degree relatives | 123 | FOBT, Colonoscopy, Sigmoidoscopy | Physician | N/A | Survey item: (1) “Ever had FOBT, sigmoidoscopy/colonoscopy? (2)”Had FOBT in last year“(3) Ever had sigmoidoscopy/colonoscopy in past three years” |
| BeLue et. al, 2011 | Quantitative | Cross-sectional design | Male African American veterans | 100% | 50 and older | 260 | FOBT, Colonoscopy, Sigmoidoscopy | Physician | Primary Care Assessment Survey subscale (Trust in Provider) | Screening adherence was assessed according to the American Cancer Society guidelines. |
| Brandzel et. al, 2016 | Qualitative | Focus Groups | Latina and Black/African American women with no previous history of cancer | 62% | 30 and older | 39 | General CRC screening was discussed | Physician and Organizational | N/A | N/A |
| Born et. al., 2009 | Quantitative | Cross-sectional survey | Men and women ages 40+ without acute illness or apparent cognitive deficit | 75.5% (<50 yo); 63.9% (>50+) | 40 and older | 282 | FOBT | Physician | Trust in Most Doctors (MDs) Scale | Report of FOBT within the last 2 years |
| Brittain et. al., 2016 | Quantitative | Cross-sectional | African American primary care patients ages 50+ who were currently non-adherent to CRC screening guidelines | 100% | 50 and older | 817 | FOBT, Colonoscopy, Sigmoidoscopy | Physician | Health care provider (HCP) Trust Scale | Survey items to assess intention to screen for FOBT/colonoscopy in the next 6 months |
| Bynum et. al., 2012 | Quantitative | Cross-sectional | Ethnically diverse men and women ages 50+ | 29.5% | 50 and older | 454 | General CRC screening was assessed | Physician | Survey item: How much of the following interfere with your taking part in a cancer screening exam?-lack of trust in medical people | Survey item from the Cancer screening questionnaire (CSQ): “How likely are you to have a cancer screening exam if the screening were for colon cancer?” |
| Fyffe et. al., 2008 | Qualitative | Focus groups | Black adult men ages 18+ | 100% | 18 and older | 24 | Colonoscopy | Physician and Organization | N/A | N/A |
| Gao et. al., 2009 | Qualitative | Videotaped observations of clinic visits and semi-structured interviews that doctors and patients separately completed following the visit | Patients ages 50+ that are not up-to-date on CRC screening and patients of participating physicians | 29.5% | 50 and older | 44 | General CRC screening was assessed | Physician and Organization | N/A | N/A |
| Gordon et. al., 2014 | Quantitative | Cross-sectional | African Americans ages 50+ with low literacy | 100 | 50 and older | 102 | Colonoscopy | Physician | Survey items: (1) Don’t go to doctor unless needed and (2) Get colonoscopy if trusted doctor recommended; | Survey items to assess perceived barriers and perceived facilitators of colonoscopy. Participants were asked whether or not they had ever had a screening test for CRC. |
| Greiner et. al, 2005 | Qualitative | Focus groups | African Americans ages 40+ without obvious mental or cognitive impairment | 100 | 40 and older | 55 | FOBT, Colonoscopy, Sigmoidoscopy | Physician and Organization | n/a | N/A |
| Greiner et. al, 2005 | Quantitative | Prospective | Men and women ages 40+ without acute illness or apparent cognitive deficit | 68.8% | 40 and older | 293 | FOBT, Colonoscopy, Sigmoidoscopy | Physician | Trust in Health Care Providers Scale | FOBT card return (dichotomous: yes/no) |
| Griffith et. al., 2012 | Qualitative | Focus groups | African American men and women age 40+ with at least one first-degree family member affected by CRC | 100% | 40 and older; first degree relatives | 14 | Colonoscopy | Physician and Organization | N/A | n/a |
| Gupta et. al, 2014 | Quantitative | Prospective | Patients ages 50+ not current with screening | 17.8% | 50 and older | 701 | FOBT and Colonoscopy | Physician and Organization | Wake Forest Trust | CRC screening completion within 12 mo following enrollment |
| Holmes-Rovner et. al, 2002 | Qualitative | Focus groups | African American and White men and women ages 50+ | 29% | 50 and older | 21 | FOBT | Physician and Organization | N/A | N/A |
| Jandorf et. al, 2013 | Quantitative | Randomized control trial | African American patients ages 50+ referred for colonoscopy screening | 100% | 50 and older | 240 | Colonoscopy | Trust in navigator | Trust in Navigator Scale | Completion of colonoscopy determined by chart audit |
| Lasser et al., 2008 | Qualitative | Semi-structured Interviews | Outpatients ages 50+ who were eligible for colorectal cancer screening | 39.1% | 50 and older | 23 | Colonoscopy, FOBT | Physician | N/A | N/A |
| Lumpkins et al., 2015 | Qualitative | Focus Groups | Men from predominantly African American churches ages 35+ | 100% | 35 and older | 28 | FOBT, Colonoscopy, Sigmoidoscopy | Physician and Organization | N/A | Participants completed a survey asking about their colorectal cancer knowledge regarding screening age, whether they had been screened, and whether they had brought up screening to their doctor. |
| Nicholson et al., 2008 | Quantitative | Double-blind Randomized Study | African American men and women age 40 and older with no history of colorectal cancer and able to reach and respond to printed information | 100% | 40 and older | 300 | Not specified | Physician and Organization | Group-Based Medical Mistrust Scale | Participants were asked if they had previously been screened for CRC and the extent to which they were planning on being screened in the next 6 months |
| O’Malley et al., 2004 | Quantitative | Cross-sectional | African-American women ages 40+ with a usual source of care | 100% | 40 and older | 961 | FOBT | Physician | Survey items from the Primary Care Assessment (1) ‘‘Thinking about how much you trust your doctor, how strongly do you agree or disagree with the following statement: My doctor cares more about holding down costs than about doing what is needed for my health.’’ (2) ‘‘All things considered, how much do you trust your doctor?” | Respondents were asked about their adherence to colorectal cancer screening |
| Palmer et al., 2008 | Qualitative | In-depth Interviews | African Americans ages 50+ with no personal history of colorectal cancer screening | 100% | 50 and older | 36 | FOBT, Colonoscopy, Sigmoidoscopy | Physician and Organization | N/A | Adherence to CRC screening: Having a fecal occult blood test (FOBT) within the past year, a flexible sigmoidoscopy within the past 5 years, or a colonoscopy within the past 10 years |
| Purnell et al., 2010 | Quantitative | Cross-sectional | African Americans ages 45+ with no personal history of cancer or colorectal disease | 100% | 45 and older | 198 | FOBT, Colonoscopy, Sigmoidoscopy, Barium enema | Physician and Organization | Group-Based Medical Mistrust Scale | The Colorectal Cancer Screening Questionnaire (CCSQ) |
| Sanders Thompson et al., 2010 | Quantitative | Randomized control trial | African Americans ages 45+ | 100% | 45 and older | 771 | FOBT, Colonoscopy, Sigmoidoscopy | Physician and Organization | Group Based Medical Mistrust Scale | Baseline survey items adapted from the National Cancer Institute Colorectal Cancer Screening Questionnaire; Intent to screen was assessed by a single item, which asked whether participants had decided against screening, were considering it, planning to or discussing it with a physician, or actively scheduling and seeking screening. |
| Sanders Thompson et al., 2013 | Qualitative | Cognitive response interviews | African American men and women with no history of colorectal cancer and who had a mailing address and a working telephone number. | 100% | 50 and older | 41 | Not specified | Physician | Not specified | N/A |
| Sanders Thompson et al., 2013 | Quantitative | Cross-sectional | African Americans age 50–75 who were born in the U.S, had a mailing address, and a working telephone. | 100% | 50 and older | 655 | FOBT, Colonoscopy, Sigmoidoscopy, Barium Enema | Physician and Organization | Not specified | The National Cancer Institute (NCI) CRCS questionnaire |
| Stacy et al., 2008 | Quantitative | Cross-sectional | Individuals ages 50+ who went to 4 senior centers located in a racially diverse Midwestern metropolitan area. | 19% | 50 and older | 43 | FOBT, Colonoscopy, Sigmoidoscopy | Physician and Organization | Not specified | Study questionnaire developed to assess knowledge about CRC screening and perceptions about barriers to screening |
| Tabbarah et al., 2005 | Quantitative | Cross-sectional | Adults age 50 and older. Individuals were not excluded if they had colorectal cancer. | 47% | 50 and older | 375 | FOBT, Colonoscopy, Lower Endoscopy | Physician and Organization | Survey items: level of trust in the health information they received from different sources | Colorectal cancer screening behavior and attitudes were measured with items based on the Triandis model for consumer decision-making |
Dominant Themes from Qualitative Studies
Table 2 summarizes the dominant themes in the qualitative studies included in this review. In 9 qualitative articles, participants noted their mistrust of doctors and/or the health care system during discussions about barriers to CRC screening. In 5 articles, participants expressed skepticism of provider motives for recommending colorectal cancer screening (e.g., that doctors might recommend screening unnecessarily to make money from conducting the procedure). In 3 articles, participants expressed mistrust of some providers’ competence and training as well as the quality of care they received from the health care system. Similarly, in 3 articles, participants expressed worry that health care providers might treat them unfairly or give them poor quality treatment due to their race, ethnicity, gender, or socioeconomic status.
Table 2.
Summary of Dominant Themes from Included Qualitative Studies
| Theme | Description | Sample Quote(s) | Contributing Studies |
|---|---|---|---|
| Mistrust as a Barrier to Screening | Participants noted that their mistrust of doctors and/or the U.S. health care system within discussions about barriers to colorectal cancer screening. | “Like I say, I do have a fear of hospitals…. Like I said to you, if it’s not broke, don’t fix it. Looking for trouble…,” and “You know they don’t like doctors, they don’t trust doctors.” (Griffith et al. 2012). | (Bastani et al. 2001), (Brandzel et al., 2016), (Fyffe et al. 2008), (Gao et al. 2009), (Greiner et al. 2005), (Griffith et al. 2012), (Holmes-Rovner et al. 2002), (Lasser et al. 2008), (Palmer et al. 2008) |
| Skepticism of Provider Motives | Participants expressed skepticism about provider motives for recommending colorectal cancer screening tests and about screening promotion in general. For example, participants worried that doctors and health care systems might recommend screening due to money instead of concern for the patient’s health. | “Anything that’s concerned with that dollar bill, I don’t care what you say, you can’t trust them (doctor). They go to that money” (Lumpkins et al. 2015). | (Bastani et al. 2001), (Brandzel et al., 2016), (Gao et al. 2009), (Greiner et al. 2005), (Lumpkins et al. 2015) |
| Mistrust of Competence and Quality of Providers/Systems | Participants mistrusted some providers’ competence and training as well as the quality of care they received from the health care system. | “Yeah like now that’s my problem I don’t have trust in the intern. I want the doctor, you know the young guy comes in and tells me that he didn’t study this in the book yet. Let me go talk to the doctor” (Fyffe et al. 2008). | (Fyffe et al. 2008), (Griffith et al. 2012), (Holmes-Rovner et al. 2002) |
| Equity of Health Care Treatment | Participants worried that doctors and other health care providers may not treat them to the best of their ability due to their race, ethnicity, gender, or socioeconomic status. | “The men or African American—a lot of people that I know, they don’t have insurance and they feel, well, they going to just brush me off and look at me and send me on home anyway, so it’s no use to even going” (Griffith et al. 2012) | (Gao et al. 2009), (Griffith et al. 2012), (Holmes-Rovner et al. 2002) |
| Fear of Experimentation | Participants expressed fear of experimentation (e.g., due to historical medical abuse in the Tuskegee Study of Untreated Syphilis in the Negro Male). | “Oh yeah… experiments in a medical field on African Americans in this country have occurred… I have no reason to believe they won’t [experiment on us]” (Holmes-Rovner et al. 2002). | (Bastani et al. 2001), (Brandzel et al., 2016), (Fyffe et al. 2008), (Holmes-Rovner et al. 2002) |
| Invasiveness of Procedure | Participants discussed sexual connotation and invasive nature of CRC screening as a barrier | “It just makes you feel a little queasy, you know, somebody putting something up in there like that you understand as a man.” (Palmer et. al, 2008) | (Palmer et. al 2008), (Lumpkins et. al 2015), (Bass et. al, 2011) |
In terms of qualitative differences by gender, themes were similar across articles for men and women. However, African American men expressed more explicit fears of medical experimentation and uneasiness about the invasiveness of colorectal cancer screening procedures, such as colonoscopies.
Psychometric properties of trust scales
Table 3 provides information about the trust scale properties used in the included quantitative studies. Eight different scales were used in the articles included in this review. Five of these scales measured trust in physicians/providers, 1 scale measured trust in the health care system, one scale measured trust in both health care providers and the health care system, and 1 scale measured trust in patient navigators. No specific scale was used predominantly across the articles; however, the most frequently used measure was the Group-Based Medical Mistrust Scale (used in 3 articles). Most studies did not report measures of scale reliability or validity. However, some studies measure scale reliability and reported Cronbach’s alphas. Of those studies, most reported Cronbach’s alpha coefficients of above 0.80.
Table 3.
Specific Trust Scales Used in Studies
| Name of Measure | Entity of Trust Measured | No. of Items | Cronbach’s α of measure | Sample Item | Associated Studies and Study-specific Cronbach’s α |
|---|---|---|---|---|---|
| Primary Care Assessment Survey subscale trust (Safran et al. 1998) | Primary Physician | 8 | 0.86 | My doctor cares more about holding down costs than about doing what is needed for my health | (BeLue et al. 2011) (α=0.83), (O’Malley et al. 2004)a(α=NS), |
| Trust in Most Doctors (Born et al. 2009)b | Most Physicians | 8 | 0.85 | Most doctors can be trusted to offer high quality medical care | (Born et al. 2009) (α=0.85) |
| Wake Forest Trust in a Physician Subscale (Dugan et al. 2005) | Primary Physician | 5 | 0.87 | You completely trust your doctor’s decisions about medical treatments best for you | (Brittain et al. 2016), (α=NS), (Gupta et al. 2014) (α=0.85), |
| Wake Forest Trust in the Medical Profession Subscale (Dugan et al. 2005) | Doctors in General | 5 | 0.77 | Sometimes doctors care more about what is convenient for them than about their patients’ medical needs | (Gupta et al. 2014) (α=NS), |
| Trust in Health Care Providers Scale (Greiner et al. 2005b)c | Health Care Providers | 8 | 0.85 | No sample item provided | (Greiner et al. 2005b) (α=NS) |
| Trust in Navigator Scale (Jandorf et al. 2013)d | Patient Navigators | 6 | Not Provided | I doubt that the Navigator really cares about me as a person | (Jandorf et al. 2013) (α=NS) |
| Group-Based Medical Mistrust Scale (Thompson et al. 2004) | Medical/Health System | 12 | 0.83 | Doctors and health care workers treat people of my ethnic group like “guinea pigs” | (Nicholson et al. 2008) (α=0.82), (Purnell et al. 2010) (α=0.88), (Sanders Thompson et al. 2010)e(α=0.73), |
| Mistrust/Discrimination Scale (Sanders Thompson et al. 2013b) | Health Care Providers/System | 9 | 0.81 | Health care workers do not take the medical complaints of African Americans seriously | (Sanders Thompson et al. 2013b) (α=0.81) |
O’Malley et al. (2004) used a subset of two items from the Primary Care Assessment Survey
Born et al. (2009) wrote one item on the Trust in Most Doctors Scale and adapted the other seven from other scales
Greiner et al. (2005b) developed the Trust in Health Care Providers Scale by adapting items from other scales
The Trust in Navigator Scale appears to be adapted from Anderson & Dedrick’s (1990) Trust in Physician Scale
Sanders Thompson et al. (2010) used a subset of three items from the Group-Based Medical Mistrust Scale
NS=Not specified
Two studies listed items used to measure trust that were not from a specific scale. Bynum et al. (2012) used the item “How much does lack of trust in medical people interfere with your taking part in a cancer screening exam?” Gordon et al. (2014) asked respondents if they would get a colonoscopy if a trusted doctor recommended it (24). Three studies measured trust but did not specify which measures or items were used in the study (25–27).
Associations between Medical Mistrust and CRC screening for Quantitative Studies
Table 4 illustrates detected associations between medical mistrust and CRC screening outcomes by screening type across the 14 included quantitative studies. A positive association indicates studies in which higher scores of medical mistrust are associated with higher rates of CRC screening. Negative association studies show higher scores of medical mistrust associated with lower rates in CRC screening. A conditional association indicated either a positive or negative association, but only for certain subpopulations, such as gender or age group. Of the 14 studies, 18 total associations were captured, with one positive, 5 negative, 4 conditional and 8 studies with no association. Across included studies, 8 associations were statistically significant (p<0.05), primarily within negative association studies (n=5). Because included studies examined multiple associations across subgroups, the number of associations is higher than the total number of quantitative studies analyzed.
Table 4.
Associations between Medical Mistrust and CRC Screening among African Americans for Quantitative Studies (n= 14)
| Colorectal Screening Type | Positive Associationa | Negative Associationb | Conditional Associationc | No Associationd | Total |
|---|---|---|---|---|---|
| Colonoscopy only | 0 | 0 | 1 (Gordon et. al) | 1 (Jandorf et. al) | 2 |
| FOBT only | 0 | 0 | 1 (Born et. al)* | 2 (O’ Malley et. al; Born et. al.) | 3 |
| FOBT and Colonoscopy | 0 | 1 (Gupta et. al)* | 0 | 1 (Gupta et. al) | 2 |
| FOBT, Colonoscopy, Sigmoidoscopy | 0 | 3 (BeLue et. al*, Tabbarah et. al*, Greiner et. al*) | 0 | 3 (Brittain et. al; Stacy et. al, Greiner et. al) | 6 |
| FOBT, Colonoscopy, Sigmoidoscopy, Barium Enema | 0 | 0 | 1 (Purnell et. al*) | 1(Sanders Thompson 2013) | 2 |
| Not specified | 1 (Bynum et. al*) | 1 (Nicholson et. al*) | 1 (Nicholson et. al) | 0 | 3 |
|
| |||||
| Overall total | 1 | 5 | 4 | 8 | 18 |
Because many studies included multiple outcomes, the total number of associations (n=18) exceeds the total number of included studies (n=14).
When higher scores of medical mistrust were associated with higher rates of CRC screening
When higher scores of medical mistrust were associated with lower rates of CRC screening
When a positive or negative association existed but only under certain conditions (e.g. differences by gender or age subgroup)
When medical mistrust was not associated with CRC screening
= Significant association (p<0.05)
Of the 11 studies examining mistrust at the physician level, one positive, 4 negative, 2 conditional, and 4 no association articles were included. The majority of statistically significant associations (67%) fell in the negative association group, meaning that higher scores of medical mistrust were significantly associated with lower rates of colorectal cancer screening. Of the 5 studies examining mistrust at the physician and organization level, one negative, two conditional, and two no association studies were found. A single study (28) examined mistrust of patient navigators and found no significant association between medical mistrust and CRC screening.
Comparative Analysis of findings between men and women for quantitative studies
No studies quantitatively examined gender differences in the associations between mistrust and CRC screening. However, eight studies examined gender differences in either CRC screening adherence or medical mistrust. Results for the association between medical mistrust and CRC screening adherence among men were mixed. One study illustrated that men with low provider trust were more likely to be classified low CRC screening latent profiles (29). However, in comparative studies, men did not have statistically different rates of mistrust than women and male gender role was not significantly associated with colorectal cancer adherence (25, 30). Among women, results were also inconclusive. Greiner and colleagues found that women were significantly more likely to report barriers to endoscopy screening. However, one study found that females were more likely to report colonoscopy receipt and less likely to report receiving an FOBT than men (27). Additional studies found that women were not significantly more likely to participate in CRC screening than men (24, 31, 32).
Discussion
This systematic review identified 27 studies that empirically assessed relationships between medical mistrust and CRC screening among African Americans. Overall, results linking medical mistrust to colorectal screening outcomes were mixed. However, when examined by statistical significance, higher medical mistrust scores were associated with lower rates of CRC screening in our study population. This finding was notable in articles examining FOBT, colonoscopy, and sigmoidoscopy as well as in cases where physician level medical mistrust was measured. Although our quantitative results did not yield definitive linkages between medical mistrust and colorectal cancer, findings from included qualitative studies identified multiple aspects during the clinical interaction contributing to mistrust, highlighting that medical mistrust may be mitigated by positive patient-provider interactions and shared decision-making. Qualitative themes centered on aspects of the patient-provider interactions that contributed to mistrust, such as skepticism of motives, perceived equity of treatment, and competence of providers.
Findings from our review confirmed important deficits in the evidence base regarding colorectal cancer screening among African Americans. We found that articles quantitatively assessing the relationship found that medical mistrust was significantly and negatively associated with lower rates in CRC screening. Furthermore, we found limited evidence evaluating mistrust and organizational level mistrust and differences in CRC screening by gender. Studies examining the direct association between medical mistrust and CRC screening also indicate significant variability in measures used to capture our outcomes of interest. This finding presents emerging opportunities for future research using valid and reliable medical mistrust measures in order to fully capture the impact of mistrust in healthcare utilization and subsequent health outcomes. Emerging research is also poised to investigate more nuanced and iterative expressions of mistrust in the cancer care continuum through longitudinal or qualitative investigations. Although CRC incidence is highest among African Americans, few studies took into account CRC risk factors in recruitment and sampling strategies in this population (33, 34). Future investigations examining CRC screening barriers among African Americans should acknowledge early incidence and severity of CRC in these populations in the recruiting and analytic framework.
Our comparative analysis of studies investigating gendered patterns of mistrust suggests that there are no distinct differences between CRC screening and mistrust associations between African American men and women. However, due to the small number of included quantitative studies (n=8) that compared findings by gender, future studies are needed to directly examine how gender modifies the relationship between medical mistrust and CRC screening. Qualitative studies highlighted patterns of mistrust, particularly among men, that prevented CRC screening, such as fear of experimentation and invasiveness of procedure. These patterns may reflect gender role norms (e.g., beliefs about masculinity) that have scarcely been attended to in studies assessing CRC screening barriers. Several studies document associations between masculinity norms and disparate use of health services among African American men (16, 35, 36). In one of the few studies examining psychosocial correlates of medical mistrust among African American men, Hammond determined that medical mistrust was largely influenced by masculinity norms discouraging disclosure of vulnerability (16). Future studies investigating associations between medical mistrust and CRC screening should also include measures assessing gender norms.
This review was limited by the varied definitions and measures used to conceptualize medical mistrust among African Americans. In addition, CRC screening outcomes were largely assessed through self-reported surveys assessing attitudes and beliefs rather than rates of CRC screening completion. Due to this heterogeneity in study measures, we were unable to complete a more in-depth meta-analysis. There is also potential for publication bias due to the under-representation of null or negative findings in published research. Finally, the majority of studies utilized cross-sectional study design, thus limiting the confirmation of temporal associations between medical mistrust and subsequent CRC screening patterns. Reasons for employing a one-time, observational method of assessing screening behavior are not unusual, given the length of time between screening occurrences (i.e. every 5 years for FOBT and 10 years for colonoscopy). However, future studies utilizing a sequential cohort design may mitigate issues of attrition that may arise in longitudinal research while simultaneously addressing issues of temporality that arise in cross-sectional studies.
Despite these limitations, this review highlights the importance of medical mistrust as an important construct in help-seeking for colorectal cancer screening. Emerging interest in the effects of medical mistrust and health outcomes has led to an increase in studies exploring its relationship among marginalized groups (37–40). More recently, studies exploring the role of mistrust in the African American community illustrate the importance of this construct, particularly in underutilization of preventive health services (15, 16). This review highlights the influence of cultural attitudes and mistrust on preventive cancer services. Data synthesized in this review confirms that medical mistrust is a key construct in the CRC screening decision-making process among African Americans. Many studies included in this review rigorously examined the role of mistrust in the health care utilization process, but there is more to work to be done in determining the role of trust as African Americans move across the CRC care continuum. The paucity of available literature for this review highlights the need for additional studies to establish more conclusive linkages between medical mistrust and CRC screening patterns. Future research should continue to explore determinants of medical mistrust, both at the patient/provider and organizational level of the healthcare system. Additionally, consistent and psychometrically sound measures are needed to further build the causal relationship between mistrust and CRC screening. Findings from this review will facilitate more in-depth studies and interventions assessing trust-related barriers to CRC screening among African Americans.
Acknowledgments
Funding
This research was partially supported by a National Service Research Award Pre-Doctoral Traineeship from the Agency for Healthcare Research and Quality sponsored by the Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, Grant No. 5T32 HS000032-28.Wizdom Powell is supported by the National Center for Minority Health and Health Disparities (# L60 MD010134), National Institutes of Drug Abuse (#1K01 DA032611-01A1), and the National Cancer Institute (#5U54CA15673306-07). Additional support for Jennifer Richmond was provided by a grant from the Robert Wood Johnson Foundation Health Policy Research Scholars program (#73921).
Footnotes
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Tammana VS, Laiyemo AO. Colorectal cancer disparities: issues, controversies and solutions. World journal of gastroenterology. 2014;20(4):869–76. doi: 10.3748/wjg.v20.i4.869. Epub 2014/02/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.USPTF. Final Update Summary: Colorectal Cancer: Screening. 2015 [Google Scholar]
- 3.Steele CB, Rim SH, Joseph DA, King JB, Seeff LC, Centers for Disease C et al. Colorectal cancer incidence and screening - United States, 2008 and 2010. MMWR supplements. 2013;62(3):53–60. Epub 2013/11/23. [PubMed] [Google Scholar]
- 4.Dimou A, Syrigos KN, Saif MW. Disparities in colorectal cancer in African-Americans vs Whites: before and after diagnosis. World journal of gastroenterology. 2009;15(30):3734–43. doi: 10.3748/wjg.15.3734. Epub 2009/08/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease C, Prevention. Vital signs: colorectal cancer screening test use–United States, 2012. MMWR Morbidity and mortality weekly report. 2013;62(44):881–8. Epub 2013/11/08. [PMC free article] [PubMed] [Google Scholar]
- 6.Agrawal J, Syngal S. Colon cancer screening strategies. Current opinion in gastroenterology. 2005;21(1):59–63. Epub 2005/02/03. [PubMed] [Google Scholar]
- 7.Agrawal S, Bhupinderjit A, Bhutani MS, Boardman L, Nguyen C, Romero Y, et al. Colorectal cancer in African Americans. The American journal of gastroenterology. 2005;100(3):515–23. doi: 10.1111/j.1572-0241.2005.41829.. discussion 4. Epub 2005/03/04. [DOI] [PubMed] [Google Scholar]
- 8.Gwede CK, Ward BG, Luque JS, Vadaparampil ST, Rivers D, Martinez-Tyson D, et al. Application of Geographic Information Systems and Asset Mapping to Facilitate Identification of Colorectal Cancer Screening Resources. Online journal of public health informatics. 2010;2(1):2893. doi: 10.5210/ojphi.v2i1.2893. Epub 2010/01/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wallace PM, Suzuki R. Regional, racial, and gender differences in colorectal cancer screening in middle-aged African-Americans and Whites. Journal of cancer education : the official journal of the American Association for Cancer Education. 2012;27(4):703–8. doi: 10.1007/s13187-012-0396-2. Epub 2012/07/14. [DOI] [PubMed] [Google Scholar]
- 10.Martinez KA, Pollack CE, Phelan DF, Markakis D, Bone L, Shapiro G, et al. Gender differences in correlates of colorectal cancer screening among Black Medicare beneficiaries in Baltimore. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2013;22(6):1037–42. doi: 10.1158/1055-9965.epi-12-1215. Epub 2013/05/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bromley EG, May FP, Federer L, Spiegel BM, van Oijen MG. Explaining persistent under-use of colonoscopic cancer screening in African Americans: a systematic review. Preventive medicine. 2015;71:40–8. doi: 10.1016/j.ypmed.2014.11.022. Epub 2014/12/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz ML, James AS, Pignone MP, Hudson MA, Jackson E, Oates V, et al. Colorectal cancer screening among African American church members: a qualitative and quantitative study of patient-provider communication. BMC public health. 2004;4(1):1. doi: 10.1186/1471-2458-4-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarfaty M, Feng S. Choice of screening modality in a colorectal cancer education and screening program for the uninsured. Journal of cancer education : the official journal of the American Association for Cancer Education. 2006;21(1):43–9. doi: 10.1207/s15430154jce2101_14. Epub 2006/08/22. [DOI] [PubMed] [Google Scholar]
- 14.Ozawa S, Sripad P. How do you measure trust in the health system? A systematic review of the literature. Social science & medicine. 2013;91:10–4. doi: 10.1016/j.socscimed.2013.05.005. Epub 2013/07/16. [DOI] [PubMed] [Google Scholar]
- 15.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev. 2000;57(Suppl 1):146–61. doi: 10.1177/1077558700057001S07. Epub 2000/11/25. [DOI] [PubMed] [Google Scholar]
- 16.Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical mistrust, and preventive health services delays among community-dwelling African-American men. Journal of general internal medicine. 2010;25(12):1300–8. doi: 10.1007/s11606-010-1481-z. Epub 2010/08/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKinstry B, Ashcroft RE, Car J, Freeman GK, Sheikh A. Interventions for improving patients’ trust in doctors and groups of doctors. The Cochrane database of systematic reviews. 2006(3):CD004134. doi: 10.1002/14651858.CD004134.pub2. Epub 2006/07/21. [DOI] [PubMed] [Google Scholar]
- 18.Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Preventive medicine. 2004;38(2):209–18. doi: 10.1016/j.ypmed.2003.09.041. Epub 2004/01/13. [DOI] [PubMed] [Google Scholar]
- 19.Yang TC, Matthews SA, Hillemeier MM. Effect of health care system distrust on breast and cervical cancer screening in Philadelphia, Pennsylvania. American journal of public health. 2011;101(7):1297–305. doi: 10.2105/AJPH.2010.300061. Epub 2011/05/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carpenter WR, Godley PA, Clark JA, Talcott JA, Finnegan T, Mishel M, et al. Racial differences in trust and regular source of patient care and the implications for prostate cancer screening use. Cancer. 2009;115(21):5048–59. doi: 10.1002/cncr.24539. Epub 2009/07/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suite DH, La Bril R, Primm A, Harrison-Ross P. Beyond misdiagnosis, misunderstanding and mistrust: relevance of the historical perspective in the medical and mental health treatment of people of color. Journal of the National Medical Association. 2007;99(8):879–85. Epub 2007/08/29. [PMC free article] [PubMed] [Google Scholar]
- 22.Fiscella K, Franks P, Clancy CM. Skepticism toward medical care and health care utilization. Medical care. 1998;36(2):180–9. doi: 10.1097/00005650-199802000-00007. Epub 1998/02/25. [DOI] [PubMed] [Google Scholar]
- 23.Thompson VLS, Bugbee A, Meriac JP, Harris JK. The utility of cancer-related cultural constructs to understand colorectal cancer screening among African Americans. Journal of public health research. 2013;2(2) doi: 10.4081/jphr.2013.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gordon TF, Bass SB, Ruzek SB, Wolak C, Rovito MJ, Ruggieri DG, et al. Developing a Typology of African Americans With Limited Literacy Based on Preventive Health Practice Orientation: Implications for Colorectal Cancer Screening Strategies. J Health Commun. 2014;19(11):1259–77. doi: 10.1080/10810730.2013.872725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sanders Thompson V, Lewis T, Williams S. Refining the use of cancer-related cultural constructs with African Americans. Health promotion practice. 2013;14(1):38. doi: 10.1177/1524839911399431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stacy R, Torrence WA, Mitchell CR. Perceptions of knowledge, beliefs, and barriers to colorectal cancer screening. Journal of cancer education : the official journal of the American Association for Cancer Education. 2008;23(4):238–40. doi: 10.1080/08858190802189030. Epub 2008/12/06. [DOI] [PubMed] [Google Scholar]
- 27.Tabbarah M, Nowalk MP, Raymund M, Jewell IK, Zimmerman RK. Barriers and facilitators of colon cancer screening among patients at faith-based neighborhood health centers. Journal of community health. 2005;30(1):55–74. doi: 10.1007/s10900-004-6095-0. Epub 2005/03/09. [DOI] [PubMed] [Google Scholar]
- 28.Jandorf L, Cooperman JL, Stossel LM, Itzkowitz S, Thompson HS, Villagra C, et al. Implementation of culturally targeted patient navigation system for screening colonoscopy in a direct referral system. Health Educ Res. 2013;28(5):803–15. doi: 10.1093/her/cyt003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.BeLue R, Menon U, Kinney AY, Szalacha LA. Psychosocial risk profiles among black male veterans administration patients non-adherent with colorectal cancer screening. Psycho-oncology. 2011;20(11):1151–60. doi: 10.1002/pon.1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brittain K, Christy SM, Rawl SM. African American Patients’ Intent to Screen for Colorectal Cancer: Do Cultural Factors, Health Literacy, Knowledge, Age and Gender Matter? J Health Care Poor U. 2016;27(1):51–67. doi: 10.1353/hpu.2016.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bynum SA, Davis JL, Green BL, Katz RV. Unwillingness to Participate in Colorectal Cancer Screening: Examining Fears, Attitudes, and Medical Mistrust in an Ethnically Diverse Sample of Adults 50 Years and Older. American Journal of Health Promotion. 2012;26(5):295–300. doi: 10.4278/ajhp.110113-QUAN-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Malley AS, Sheppard VB, Schwartz M, Mandelblatt J. The role of trust in use of preventive services among low-income African-American women. Preventive medicine. 2004;38(6):777–85. doi: 10.1016/j.ypmed.2004.01.018. Epub 2004/06/15. [DOI] [PubMed] [Google Scholar]
- 33.Griffith KA, Passmore SR, Smith D, Wenzel J. African Americans with a family history of colorectal cancer: Barriers and facilitators to screening. Oncology nursing forum. 2012;39(3):299–306. doi: 10.1188/12.ONF.299-306. [DOI] [PubMed] [Google Scholar]
- 34.Bastani R, Gallardo NV, Maxwell AE. Barriers to colorectal cancer screening among ethnically diverse high- and average-risk individuals. Journal of Psychosocial Oncology. 2001;19(3–4):65–84. doi: 10.1300/J077v19n03_06. [DOI] [Google Scholar]
- 35.Powell W, Adams LB, Cole-Lewis Y, Agyemang A, Upton RD. Masculinity and Race-Related Factors as Barriers to Health Help-Seeking Among African American Men. Behav Med. 2016;42(3):150–63. doi: 10.1080/08964289.2016.1165174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheatham CT, Barksdale DJ, Rodgers SG. Barriers to health care and health‐seeking behaviors faced by black men. Journal of the American Academy of Nurse Practitioners. 2008;20(11):555–62. doi: 10.1111/j.1745-7599.2008.00359.x. [DOI] [PubMed] [Google Scholar]
- 37.Born W, Engelman K, Greiner KA, Bhattacharya SB, Hall S, Hou Q, et al. Colorectal cancer screening, perceived discrimination, and low-income and trust in doctors: a survey of minority patients. BMC public health. 2009;9:363. doi: 10.1186/1471-2458-9-363. Epub 2009/09/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grenier KA, James AS, Born W, Hall S, Engelman KK, Okuyemi KS, et al. Predictors of fecal occult blood test (FOBT) completion among low-income adults. Preventive medicine. 2005;41(2):676–84 9. doi: 10.1016/j.ypmed.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 39.Purnell JQ, Katz ML, Andersen BL, Palesh O, Figueroa-Moseley C, Jean-Pierre P, et al. Social and cultural factors are related to perceived colorectal cancer screening benefits and intentions in African Americans. Journal of behavioral medicine. 2010;33(1):24–34 11p. doi: 10.1007/s10865-009-9231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.LaVeist TA, Isaac LA, Williams KP. Mistrust of Health Care Organizations Is Associated with Underutilization of Health Services. Health Services Research. 2009;44(6):2093–105. doi: 10.1111/j.1475-6773.2009.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


