Abstract
Following a peak in the mid 1960s, there has been a steady decline in coronary heart disease (CHD) mortality in the United States of 2.8%/y to 5.1%/y.1,2 This shift in mortality patterns is most dramatic in the age-adjusted rates. Age adjustment compensates for the transition of CHD in older age groups and the increase in the aged population. The absolute number of total CHD deaths showed little change until recently (Figure 1). Life expectancy of adults dramatically increased, largely as a result of these improved CHD outcomes.3 However, the reduction in mortality was not associated with a decline in hospital morbidity as CHD was pushed into the older age groups.1 Prevalence actually increased with more individuals diagnosed, treated, and surviving.1 CHD hospitalizations for those >65 years of age increased from 1965 to 2000 while declining in younger age groups.1
Keywords: Editorials, acute coronary syndrome, epidemiology, myocardial infarction
The decline in US mortality was first described at a National Heart, Lung, and Blood Institute conference in 1978.4 At that time, the causes of this pattern were not well understood. Subsequently, it became clear that improvements in classic risk factors (hypertension, lipids, and smoking), acute myocardial infarction (AMI) care, and secondary prevention are associated factors.5–12 In the 1970s, risk factor control appeared largely responsible, but in recent years, short- and long-term care for CHD predominates in modeling exercises.12–14
In this issue of Circulation, Chen and colleagues15 add important information to our understanding of these trends and help inform future directions for the delivery of care for AMI. Using the large Medicare fee-for-service database, they find a substantial reduction in AMI hospitalization rates of 23.4% from 2002 to 2007 for those ≥65 years of age. They describe similar declines for white men and women but smaller declines for blacks compared with their white counterparts. Importantly, these reductions occurred across all age categories, including the very old, those ≥85 years of age. Alternative explanations such as diagnostic code shifting are considered by evaluating data on other cardiovascular diagnoses and non-AMI hospitalizations. Discharges for unstable angina (International Classification of Diseases [ICD] 411), chronic coronary artery disease (ICD 414), heart failure (ICD 428), and dysrhythmias (ICD 427) and non-AMI hospitalizations are also falling, suggesting that the changes are real. The Medicare fee-for-service database includes 81% of all older adults; the remainder are managed care beneficiaries.16,17 Those in managed care are usually healthier than fee-for-service patients.16 These and other alternative explanations are considered and discarded, suggesting that these are genuine population trends in AMI.
Similar data are observed nationally in surveillance of hospitalization rates for AMI from 1965 to 2006 (Figure 2).1 This figure also includes the middle-aged group (45 to 64 years of age). The rates of AMI hospitalization in this group consistently fell, averaging 2.8%/y since 1987. For those ≥65 years of age, hospitalization rates for AMI were variable but declined dramatically from 1999 to 2006, averaging 4.1%/y. These patterns are consistent with the long-term movement in AMI in older age groups. However, recent benefit is found in those ≥65 years of age, as observed by Chen et al.15
Figure 2.
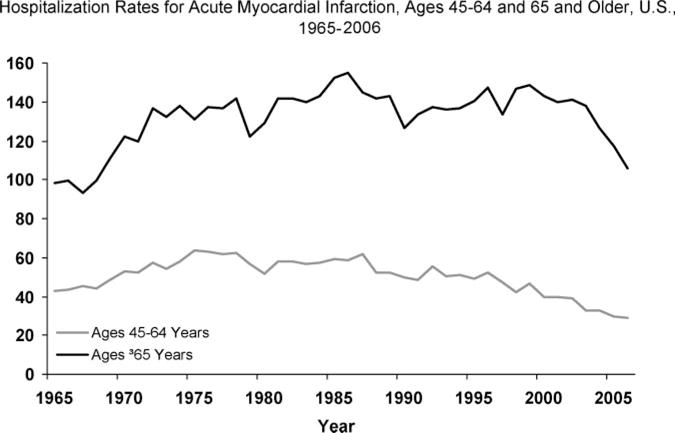
National trends (in the United States) in hospitalization for acute myocardial infarction by younger (45 to 64 years) and older (65 and older) age categories. From the National Center for Health Statistics.
Other indicators also suggest a decline in AMI in the 21st century. Data from the National Center for Health Statistics show a decline in hospital admissions for CHD from 2000 to 2006 for both men and women.2 Similarly, all hospital discharges for cardiovascular diseases declined from 2000 to 2006.2
Are these changes real? Converging evidence from this and other sources confirms this decline. The work by Chen and colleagues is well done; alternative explanations carefully eliminated.15 The consistency of the trend over the 8 or more years of the 21st century adds evidence that this is not a statistical artifact. Other technologies such as the widespread use of sensitive troponins since the late 1990s for AMI diagnosis would be expected to increase AMI discharges, not decrease them.
What might underlie this change? During this period, there have been major improvements in the control of cholesterol, smoking, and blood pressure. For example, the proportion of Minnesotans 65 to 74 years of age taking statins to lower cholesterol was 22% among women and 27% among men in 2000 to 2002.6 This is a sizable fraction of the population. Similarly, there were major reductions in saturated fat and dietary cholesterol over time associated with declines in blood cholesterol levels in the population.6 Smoking rates have plummeted; the National Health Interview Survey found that 42.4% of adults smoked cigarettes in 1965 and 19.8% in 2007.18
Improvements in cardiac care also play a role. However, that care is more likely to be at the outpatient level aimed at primary or secondary prevention rather than inpatient interventions. Chen et al find that recurrent AMI admissions are a small proportion of AMI cases in the same year (5% to 7%), declining modestly. Thus, the drop in AMI discharges is mainly in new events, those most likely to be the result of primary prevention.
What are the implications of these positive trends? It is clear that we are making progress in both mortality and morbidity from CHD in the 21st century. These findings need follow-up to ensure that the trends continue, but they also should inform planning of healthcare resource allocation. The “baby-boom” generation may not require additional cardiovascular services. For example, do we need more coronary care unit beds or intervention facilities in the next decades? It is clear that there will be a shortage of physicians in the coming decades, but do we need more primary care providers or specialists such as cardiologists?19 Data such as that provided by the work of Chen and colleagues and other surveillance systems must inform those decisions.
Figure 1.
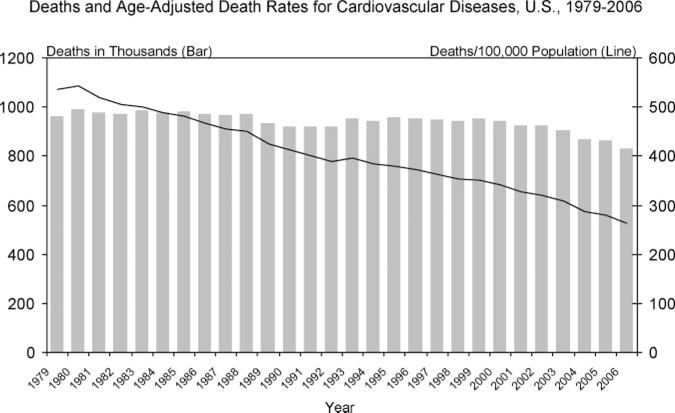
National trends (in the United States) in total mortality and age-adjusted mortality from cardiovascular diseases. From the National Center for Health Statistics.
Acknowledgments
Sources of Funding
This work was supported in part by NIH R01 HL023727 and NIH K08 HL083611.
Footnotes
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
Disclosures
None.
References
- 1.National Heart, Lung, and Blood Institute. Morbidity and Mortality: 2009 Chart Book on Cardiovascular, Lung, and Blood Diseases. Bethesda, Md: National Institutes of Health; 2009. [Google Scholar]
- 2.American Heart Association. Heart Disease and Stroke Statistics: 2010 Update. Dallas, Tex: American Heart Association; 2009. [Google Scholar]
- 3.Arias E. United States life tables, 2004. Natl Vital Stat Rep. 2007;56:1–40. [PubMed] [Google Scholar]
- 4.Havlik RJ, Feinlieb M, editors. Proceedings of NHLBI Conference on Decline of Coronary Heart Disease Mortality. Bethesda, Md: National Institutes of Health; 1978. (Publication No 79-16-10). [Google Scholar]
- 5.Luepker RV, Arnett DK, Jacobs DR, Jr, Duval SJ, Folsom AR, Armstrong C, Blackburn H. Trends in blood pressure, hypertension control, and stroke mortality: the Minnesota Heart Survey. Am J Med. 2006;119:42–49. doi: 10.1016/j.amjmed.2005.08.051. [DOI] [PubMed] [Google Scholar]
- 6.Arnett DK, Jacobs DR, Jr, Luepker RV, Blackburn H, Armstrong C, Claas SA. Twenty-year trends in serum cholesterol, hypercholesterolemia, and cholesterol medication use: the Minnesota Heart Survey, 1980–1982 to 2000–2002. Circulation. 2005;112:3884–3891. doi: 10.1161/CIRCULATIONAHA.105.549857. [DOI] [PubMed] [Google Scholar]
- 7.Rosamond WD, Chambless LE, Folsom AR, Cooper LS, Conwill DE, Clegg L, Wang CH, Heiss G. Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998;339:861–867. doi: 10.1056/NEJM199809243391301. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decade (1975 to 1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 9.Roger VL, Jacobsen SJ, Weston SA, Goraya TY, Killian J, Reeder GS, Kottke TE, Yawn BP, Frye RL. Trends in the incidence and survival of patients with hospitalized myocardial infarction, Olmsted County, Minnesota, 1979 to 1994. Ann Intern Med. 2002;136:341–348. doi: 10.7326/0003-4819-136-5-200203050-00005. [DOI] [PubMed] [Google Scholar]
- 10.McGovern PG, Pankow JS, Shahar E, Doliszny KM, Folsom AR, Blackburn H, Luepker RV. Recent trends in acute coronary heart disease-mortality, morbidity, medical care, and risk factors: the Minnesota Heart Survey Investigators. N Engl J Med. 1996;334:884–890. doi: 10.1056/NEJM199604043341403. [DOI] [PubMed] [Google Scholar]
- 11.Dobson R. US cigarette consumption falls to lowest point since 1951. BMJ. 2006;332:687. doi: 10.1136/bmj.332.7543.687-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 13.Goldman L, Cook F, Hashimotso B, Stone P, Muller J, Loscalzo A. Evidence that hospital care for acute myocardial infarction has not contributed to the decline in coronary mortality between 1973–1974 and 1978–1979. Circulation. 1982;65:936–942. doi: 10.1161/01.cir.65.5.936. [DOI] [PubMed] [Google Scholar]
- 14.McGovern PG, Jacobs DR, Jr, Shahar E, Arnett DK, Folsom AR, Blackburn H, Luepker RV. Trends in acute coronary heart disease mortality: mortality, morbidity, and medical care from 1985 through 1997: the Minnesota Heart Survey. Circulation. 2001;104:19–24. doi: 10.1161/01.cir.104.1.19. [DOI] [PubMed] [Google Scholar]
- 15.Chen J, Normand ST, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 16.Shimada SL, Zaslavsky AM, Zaborski LB, O’Malley AJ, Heller A, Cleary PD. Market and beneficiary characteristics associated with enrollment in Medicare managed care plans and fee-for-service. Med Care. 2009;47:517–523. doi: 10.1097/MLR.0b013e318195f86e. [DOI] [PubMed] [Google Scholar]
- 17.Morgan RO, Virnig BA, DeVito CA, Persily NA. The Medicare-HMO revolving door: the healthy go in and the sick go out. N Engl J Med. 1997;337:169–175. doi: 10.1056/NEJM199707173370306. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. State-specific prevalence and trends in adult cigarette smoking – United States, 1998–2007. MMWR Morb Mortal Wkly Rep. 2009;58:221–226. [PubMed] [Google Scholar]
- 19.Association of American Medical Colleges. AAMC Statement on the Physician Workforce. Available at: http://www.aamc.org/workforce/. Accessed February 26, 2010.


