Abstract
Background
Trauma exposure is associated with adverse psychological outcomes including anxiety, depression, and obsessive-compulsive (OC) symptoms. Adolescence is increasingly recognized as a period of vulnerability for the onset of these types of psychological symptoms. The current study explored the mediating roles of experiential avoidance and mindfulness processes in the association between retrospective reports of childhood trauma and current internalizing and OC symptoms in adolescents.
Method
A group of at-risk adolescents (N =51) and a group of college students (N =400) reported on childhood trauma, experiential avoidance, mindfulness, anxiety, depressive, and OC symptoms. Mediation analyses were performed to examine the mechanistic roles of avoidance and mindfulness in the association between trauma and internalizing and OC-specific symptoms.
Results
In the group of at-risk adolescents, experiential avoidance and mindfulness both significantly mediated the association between childhood trauma and OC symptoms. In the college student sample, experiential avoidance mediated the association between trauma and OC symptoms. Experiential avoidance, as well as the observe, act with awareness, and nonjudgmental facets of mindfulness all significantly mediated the association between trauma and internalizing symptoms.
Limitations
The group of at-risk adolescents was small, and the college student group was demographically homogeneous. All data was self-report and cross-sectional.
Conclusion
The current study demonstrated that experiential avoidance and mindfulness processes may be the mechanisms through which the association between trauma and obsessive-compulsive and trauma and internalizing symptoms exist in adolescents. These findings provide potential targets for clinical intervention to improve outcomes for adolescents who have experienced trauma.
Keywords: Trauma, Experiential Avoidance, Internalizing, Obsessive-Compulsive, Mindfulness
Exposure to trauma before the age of eighteen is not a rare occurrence, and its ramifications can be significant (Elzy et al., 2013). Trauma exposure is defined as the experience of an event that involves an actual or perceived threat to the physical integrity of self or others (American Psychiatric Association, 2000). Events that fall into this category most commonly include either interpersonal events (i.e., sexual, emotional, or physical abuse or neglect; interpersonal violence; school or community violence) or non-interpersonal events (life-threatening illness; natural disaster; motor vehicle or other serious accident).
According to the most recent data by the U.S. Department of Health & Human Services, over 700,000 children were maltreated in 2014, with 75% of victims experiencing neglect; 17% physical abuse; and 8% sexual abuse (USDHHS, 2016). During adolescence, witnessing violence or surviving any type of assault appears to be a widespread occurrence. Kilpatrick et al. (2000) examined the prevalence of victimization in a representative sample of over 4,000 adolescents aged 12–17, finding that 8% of adolescents reported experiencing sexual assault; 23%, physical assault; and 41%, witnessing violence. In total, 50% of adolescents endorsed witnessing violence or experiencing at least one trauma, with many reporting multiple traumas (Kilpatrick et al., 2000).
Early life stress or trauma is a major risk factor for the development of psychiatric symptoms later in life (Ford, 2013; Heim and Nemeroff, 2001). Trauma-related disorders, such as posttraumatic stress disorder (PTSD), are the psychiatric conditions most often associated with trauma exposure (Kendall-Tackett et al., 1993). However, there is also a robust association between significant childhood adversities and the development of other adult internalizing disorders, such as depression and anxiety (Chapman et al., 2004; Cougle et al., 2010; Edwards et al., 2003; Fierman et al., 1993; Ford et al., 2010). Further, adolescence is a time of increased vulnerability to develop anxiety or depressive symptoms (Paus et al., 2008), especially after experiencing a childhood interpersonal trauma or witnessing violence as a child (Brown et al., 1999; Russell et al., 2010). In addition to trauma-related disorders, there is emerging research examining a unique relation between trauma exposure and obsessive-compulsive (OC) symptoms (Fontenelle et al., 2012).
Empirical and case studies have demonstrated an association between a history of trauma and increased severity of OC symptoms (for review, see Miller and Brock, 2017). For example, individuals with a diagnosis of obsessive-compulsive disorder (OCD) reported significantly more childhood trauma compared to healthy controls (Lochner et al., 2002). Further, in a large clinical sample of individuals diagnosed with OCD, severity of OC symptoms was significantly associated with a history of traumatic events (Cromer et al., 2007).
Onset of OC symptoms often appears in two developmental periods, with one peak around puberty (10–13 years) and another in early adulthood (21-29 years) (De Luca et al., 2011; Zohar, 1999). OCD has been identified as one of the most common psychiatric conditions affecting youth (Stewart et al., 2004; Valleni-Basile et al., 1994), with early-onset symptoms being particularly detrimental (do Rosario-Campos et al., 2001; Wang et al., 2012). Little is known, however, about how exposure to trauma could affect OC symptoms in adolescents. The few studies that have examined trauma history and OC symptoms in adolescents have focused on comorbid OCD and PTSD symptoms rather than history of trauma specifically (Essau et al., 2000; Lafleur et al., 2011). In order to provide appropriate and early intervention for children and adolescents experiencing OC symptoms, it is important to better understand OC symptoms, along with internalizing symptoms, in adolescents with a history of trauma.
Although trauma exposure increases risk for developing psychiatric symptoms, not every young adult who has experienced trauma develops symptoms; individual differences lead to differing outcomes (Kessler et al., 1995). One mechanism that may help explain the role that trauma exposure plays in the development or exacerbation of psychiatric symptoms is experiential avoidance, which can be characterized as an unwillingness or inability to remain in contact with internal experiences (thoughts, memories, emotions, and/or bodily sensations) or any attempt to alter or escape the experiences (Hayes et al., 1996). Importantly, individuals who have experienced trauma often engage in experiential avoidance (Follette et al., 2006; Orsillo and Batten, 2005).
The employment of avoidant coping strategies in response to trauma is associated with potentially problematic behaviors, such as less social engagement or high-risk sexual behavior, as well as with psychological difficulties, such as PTSD symptoms (Batten et al., 2002; Brockman et al., 2016; Orcutt et al., 2005). Experiential avoidance has been identified as an important mechanism which may partially explain the association between trauma exposure and the manifestation of psychopathology in populations of adolescents (Venta et al., 2012) and young adults (Land, 2010). Briggs and Price (2009) examined the interplay of adverse childhood experiences (including neglect and abuse), anxiety and depressive symptoms, OC symptoms, and experiential avoidance in a community sample of young adults and undergraduates (mean age of 28). Experiential avoidance mediated the relation between adverse childhood experiences and OC symptoms, even when controlling for anxiety and depression. Given this finding, the associations between trauma exposure, experiential avoidance, and psychopathology need to be further elucidated, especially in the particularly vulnerable time period of adolescence.
Mindfulness- and acceptance-based therapies, such as Acceptance and Commitment Therapy (Hayes et al., 1999) and Mindfulness-Based Stress Reduction (Kabat-Zinn, 2003), have increasingly been utilized to target and address experiential avoidance. These therapies aim to decrease avoidance while increasing acceptance, the willingness to remain in contact with all current internal and external sensations, even if the internal sensations are aversive, in order to pursue valued living (Cordova, 2001; Kabat-Zinn, 2003). Similarly, these therapies aim to cultivate mindfulness, or a nonjudgmental awareness of the present moment (Kabat-Zinn, 2003). Mindfulness is often characterized in the literature as a multifaceted construct consisting of five distinct yet interrelated facets: 1) observing or noticing present moment experience, 2) the ability to describe or put present-moment experience into words, 3) acting with awareness or concentrating on behavior rather than acting on “automatic pilot” 4) nonjudgment of experience such as thoughts or emotions and 5) nonreactivity to inner experience, or the ability to be aware of inner experiences without immediately reacting to them (Baer et al., 2006). Acceptance- and mindfulness-based therapies have been shown to be effective in addressing symptoms of trauma-related disorders (Orsillo and Batten, 2005; Vujanovic et al., 2013), internalizing disorders (Forman et al., 2007; Swain et al., 2013), and OC symptoms (Bluett et al., 2014; Twohig et al., 2010). There is less information on how interventions based on principles of mindfulness and acceptance may mitigate psychiatric symptoms in adolescents. Considering the high rates of trauma exposure, internalizing disorder symptoms, and OC symptoms in adolescents, basic research needs to clarify how acceptance and mindfulness processes could be incorporated into treatment for young adults.
The current study examined the mediating roles of experiential avoidance and the five facets of mindfulness in linking childhood trauma exposure and OC-specific and internalizing symptomology in young adults. Current age ranges utilized to define adolescence vary, but neuroimaging studies have shown that the brain continues to develop well into a person’s twenties, prompting discussions surrounding the most appropriate way to characterize this important developmental time period (Curtis, 2015; Johnson et al., 2009). Therefore, two populations of adolescents were utilized: 1) at-risk adolescents attending an alternative high school and 2) undergraduate students at a large Midwestern university. The authors hypothesized that experiential avoidance would mediate the relation between trauma exposure and elevated internalizing and OC symptoms in both at-risk adolescents and undergraduate students. Additionally, because recent work has suggested that mindfulness processes build upon one another and therefore may be targeted individually in clinical work (Strosahl et al., 2015), multiple mediation analyses were conducted with mindfulness facets in examining the association between trauma exposure and internalizing and OC symptoms in an attempt to understand which specific aspects of mindfulness may be important targets for intervention.
Method—Study 1
Participants
Participants were recruited from a Midwestern alternative high school, where students are referred for academic failure, substance abuse, risk for dropout, or psychosocial difficulties. Of the 120 students at the school, 53 chose to participate. Sample characteristics are in Table 1.
Table 1.
Descriptive statistics of the adolescent sample, N = 51.
| N (%) | |
|---|---|
|
| |
| Gender | |
| Male | 21 (39.6%) |
| Female | 32 (60.4%) |
| Age, M(SD) | 16.29 (1.01) |
| Race | |
| White, Non-Hispanic | 18 (34.0%) |
| White Hispanic | 6 (11.3%) |
| African American | 22 (41.5%) |
| American Indian or Alaska Native | 1 (1.9%) |
| Native Hawaiian or Pacific Islander | 1 (1.9%) |
| Biracial or Multiracial | 5 (9.4%) |
| Employment Status | |
| Full-time | 3 (5.7%) |
| Part-time | 26 (49.1%) |
| Unemployed | 24 (45.3%) |
| Grade in School | |
| 9 | 5 (9.4%) |
| 10 | 15 (28.3%) |
| 11 | 24 (45.3%) |
| 12 | 9 (17.0%) |
| Sexual Orientation | |
| Heterosexual | 35 (66%) |
| Homosexual, Bisexual, or Other | 15 (28.3%) |
| Missing | 3 (5.7%) |
| ETI, M(SD) | 9.66 (5.66) |
| AFQ-Y, M(SD) | 2.43 (3.86) |
| CAMM, M(SD) | 32.04 (7.82) |
Note. ETI = Early Trauma Inventory. AFQ-Y = Avoidance and Fusion Questionnaire – Youth. CAMM = Child and Adolescent Mindfulness Measure.
Procedure
Institutional Review Board (IRB) approval was obtained. Data were collected using Qualtrics (www.qualtrics.com) in 2014. Participants completed the assessment upon enrollment in the study after providing written informed consent. The data included in the current analyses are cross-sectional baseline data from a longitudinal intervention study.
Measures
Childhood traumatic experiences
Childhood trauma was measured using the Early Trauma Inventory Self-Report Short Form (ETI-SR-SF; Bremner et al., 2007), which measures four domains of trauma, including general trauma and physical, emotional, and sexual abuse. The ETI-SR-SF is a 27-item scale that is based on the endorsement of previous traumatic experiences (0 = No, 1 = Yes). The mean for healthy controls from the validation study was 3.5 ± 3.3 (Bremner et al., 2007). The four domains of trauma display adequate internal consistency (Cronbach’s α’s 0.70–0.87; Bremner et al., 2007), and the short-form correlates highly with the long form. Reliability in this sample was good (α = .87).
Experiential avoidance
The Avoidance and Fusion Questionnaire-Youth (AFQ-Y) was used to measure experiential avoidance (Greco et al., 2008). The 17-item instrument is designed for youth, and higher scores indicate greater avoidance. An example item is “I try hard to erase hurtful memories from my mind.” Items use a 5-point Likert scale (0 = Not at all true, 4 = Very true). The AFQ-Y demonstrates good internal consistency and convergent and construct validity. Reliability in this sample was excellent (α = .97).
Mindfulness
The Child and Adolescent Mindfulness Measure (CAMM-10) was used to measure mindfulness (Greco et al., 2011). The 10-item measure uses a 5-point Likert scale (0 = Never true, 4 = Always true), with higher scores indicating greater mindfulness. Example items include: “It’s hard for me to pay attention to only one thing at a time” and “I get upset with myself for having certain thoughts.” Research has indicated good internal consistency and convergent, construct, and incremental validity (Greco et al., 2011). Reliability in this sample was excellent (α = .96).
Obsessive-compulsive symptoms
To measure the severity of obsessive-compulsive symptoms, the revised Obsessive-Compulsive Inventory-Revised (OCI-R) was utilized (Foa et al., 2002). Example items include “I frequently get nasty thoughts and have difficulty in getting rid of them” and “I get upset if objects are not arranged properly.” The scale uses a 5-point Likert scale (0 = Not at all, 4 = Extremely), representing the extent to which a symptom was bothersome or distressing in the past month. Internal consistency was good (Foa et al., 2002). Higher scores represent more severe OC symptomatology. Reliability in this sample was excellent (α = .95).
Method—Study 2
Participants
Participants were recruited through an online study portal through a large Midwestern university. Students at the university participate in research studies for partial course credit. 414 responses were gathered, of which 400 responses were usable.
Demographic characteristics of the sample indicate that the sample was young (M = 19.16, SD = 1.33), primarily Caucasian (68.1%), and heterosexual (88.1%). The sample consisted of more females (64.0%) than males (34.3%). Participant characteristics are displayed in Table 2.
Table 2.
Descriptive statistics of the college student sample, N = 400.
| N (%) | |
|---|---|
|
| |
| Gender | |
| Male | 142 (34.3%) |
| Female | 265 (64.0%) |
| Unsure, prefer not to answer, other | 4 (0.9%) |
| Missing | 3 (0.7%) |
| Age, M(SD) | 19.16 (1.33) |
| Race | |
| White, Non-Hispanic | 282 (68.1%) |
| White Hispanic | 56 (13.5) |
| African American | 13 (3.1%) |
| Asian American | 40 (9.7%) |
| American Indian or Alaska Native | 1 (0.2%) |
| Native Hawaiian or Pacific Islander | 1 (0.2%) |
| Biracial or Multiracial | 15 (3.6%) |
| Missing | 6 (1.4%) |
| Employment Status | |
| Full-time | 12 (2.9%) |
| Part-time | 188 (45.4%) |
| Unemployed | 211 (51%) |
| Missing | 3 (0.7%) |
| Year in College | |
| 1 | 218 (52.7%) |
| 2 | 106 (25.6%) |
| 3 | 54 (13%) |
| 4 | 29 (7%) |
| Sexual Orientation | |
| Heterosexual | 369 (88.1%) |
| Homosexual, Bisexual, or Other | 40 (9.7%) |
| Missing | 5 (1.2%) |
| ETI, M(SD) | 6.28 (4.89) |
| AAQ-II, M(SD) | 21.10 (8.98) |
| FFMQ | |
| Observe | 24.58 (5.38) |
| Describe | 25.84 (5.46) |
| Act with Awareness | 24.93 (5.46) |
| Nonjudgment | 25.05 (6.11) |
| Nonreactivity | 20.59 (3.9) |
| OCI-R | 14.2 (13.62) |
| PHQ-9 | 8.5 (6.83) |
| GAD-7 | 6.53 (5.52) |
Note. ETI = Early Trauma Inventory. AAQ = Acceptance and Action Questionnaire-II. FFMQ = Five Facet Mindfulness Questionnaire. PHQ-SSS = Patient Health Questionnaire-Somatic Symptom Severity.
Procedure
The project was approved through the University IRB. Qualtrics was used to collect data.
Measures
Childhood traumatic experiences
See Method-Study 1. Reliability in this sample was good (α = .85).
Experiential avoidance
Experiential avoidance was measured with the Acceptance and Action Questionnaire-II (AAQ-II; Bond et al., 2011). The seven-item measure uses a 7-point Likert scale (0 = Never true, 6 = Always true) with higher ratings indicating increased experiential avoidance. Example items include “my painful memories prevent me from having a fulfilling life” and “worries get in the way of my success.” Good internal consistency has been demonstrated in other samples (mean alpha coefficient = .84 across various samples). Reliability in this sample was excellent (α = .91).
Mindfulness
To measure mindfulness, the Five Facet Mindfulness Questionnaire (Baer et al., 2006) was utilized to measure five mindfulness processes: Observing, Describing, Acting with Awareness, Non-Judging of Experience, and Non-Reacting to Inner Experience. The FFMQ is a 39-item questionnaire that uses a 5-point Likert scale (1 = Never or very rarely true, 5 = Very often or always true). Internal consistency of each facet is adequate (αs = .75–.91). Internal consistency in this sample was adequate for each facet: Observe (α = .76), Describe (α = .84), Act with Awareness (α = .87), Nonjudgment (α = .88), and Nonreactivity (α = .72).
Obsessive-compulsive symptoms
See Method-Study 1. Reliability in this sample was excellent (α = .94).
Internalizing symptoms
The presence and severity of anxiety was measured using the General Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006). The 7-item measure uses a 4-point Likert scale (0 = Not at all, 3 = Nearly every day), with higher scores representing more severe anxiety symptoms. Example items include “feeling nervous, anxious or on edge” and “worrying too much about different things.” Internal consistency was adequate in the validation study, and criterion, construct, and procedural validity were established (Spitzer et al., 2006). Reliability in this sample was good (α = .89).
In order to measure depression severity, the Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001) was used to measure depressive symptoms. Using a 4-point Likert scale (0 = Not at all, 3 = Nearly every day), the PHQ-9 measures severity of depression symptoms according to the nine diagnostic criteria in the DSM-IV (e.g., feeling down, losing interest), with higher scores representing more severe depressive symptoms. Criterion, construct, and external validity were established in several samples (Kroenke et al., 2001). Reliability in this sample was excellent (α = .92).
An internalizing composite factor was created using the Dimension Reduction function of SPSS, version 23, with the items from the PHQ-9 and GAD-7. A Principal Components Analysis (PCA) was conducted with the 16 items from both scales, and no rotation was used. The items loaded onto one factor that accounted for 48.55% of the total variance, and all factor loadings were above .64. Thus, a single factor was used to represent internalizing symptoms.
Statistical Analyses
Mediation analyses for both studies were conducted using the PROCESS macro (Hayes, 2013) in SPSS, version 23. In Study 1, two mediation analyses were conducted to examine the mediating role of 1) avoidance and 2) mindfulness in the relation between traumatic experiences and obsessive-compulsive symptoms. In Study 2, the mediating role of avoidance was examined in the relation between traumatic experiences and 1) obsessive-compulsive symptoms and 2) internalizing symptoms. Second, multiple mediation analyses were conducted with the five facets of mindfulness to examine the mediating role of mindfulness facets in the relation between traumatic experiences and 1) obsessive-compulsive symptoms and 2) internalizing symptoms. Results reflect three analyses: 1) effect of traumatic experiences on the mediator, 2) effect of mediator on the outcome of interest and effect of traumatic experiences on the outcome while controlling for the mediator (direct effect), 3) the effect of traumatic experiences on the outcome by way of the mediator—indirect effect. PROCESS uses a bootstrapping method that provides a confidence interval around the indirect effect, and when zero is not included in the confidence interval, this indicates a significant indirect effect. A 95% confidence interval was computed using 10,000 resamplings. All reported coefficients are unstandardized. Percent mediation statistics were calculated to reflect the portion of the total effect accounted for by the indirect effect.
Results—Study 1
Descriptive statistics are reported in Table 1. The sample was slightly more female than male, racially diverse, and about 16 years of age on average. Item-level missing data were handled using mean imputation if less than 10% of the items in a scale were missing. In all cases with this sample, only one item was missing when mean imputation was used. If greater than 10% of the scale’s items were missing, the scale was counted as missing, and the PROCESS macro did not include the data. Only 2 participants were not included (N = 51).
Avoidance
Previous trauma was not significantly related to avoidance (coefficient: 0.19, CI: [-0.004, 0.38], p = .055). Avoidance was significantly related to OC symptoms (coefficient: 1.70, CI: [.78, 2.63]), p < .001). A direct effect of previous traumatic experiences on OC symptoms was not observed (coefficient: 0.31, CI: [-0.34, .95], p = .34). An indirect effect of avoidance was observed (coefficient: 0.32, CI: [.01, .85]), accounting for half of the total effect (PM = .51). See Table 3 and Figure 1a for results.
Table 3.
Association between previous trauma and obsessive-compulsive symptoms, as mediated by avoidance and mindfulness in adolescent sample.
| Outcome Variable | Predictor | Coefficient (SE) | CI | t | p |
|---|---|---|---|---|---|
| Avoidance | ETI | .19 (.10) | [−.004, .38] | 1.97 | .05 |
| OC Symptoms | Avoidance | 1.70 (.46) | [.78, 2.63] | 3.69 | <.001 |
| ETI | .31 (.32) | [−.34, .95] | .96 | .34 | |
| Indirect Effect | Effect (Boot SE) | CI | |||
| OC Symptoms | Avoidance | .32 (.21) | [.01, .85] | ||
|
| |||||
| Outcome Variable | Predictor | Coefficient (SE) | CI | t | p |
| Mindfulness | ETI | −.67 (.18) | [−1.03, −.32] | −3.84 | <.001 |
| OC Symptoms | Mindfulness | −1.21 (.22) | [−1.66, −.76] | −5.38 | <.001 |
| ETI | −.19 (.31) | [−.8189, .4436] | −.60 | .55 | |
| Indirect Effect | Effect (Boot SE) | CI | |||
| OC Symptoms | Mindfulness | .81 (.27) | [.38, 1.45] | ||
Note. N = 51. ETI = Early Trauma Inventory (total number of previous traumatic experiences). OC Symptoms = Obsessive-Compulsive Symptoms, as measured by OCI-R. Boot SE = Bootstrapped Standard Error. CI = Confidence Interval.
Figure 1.
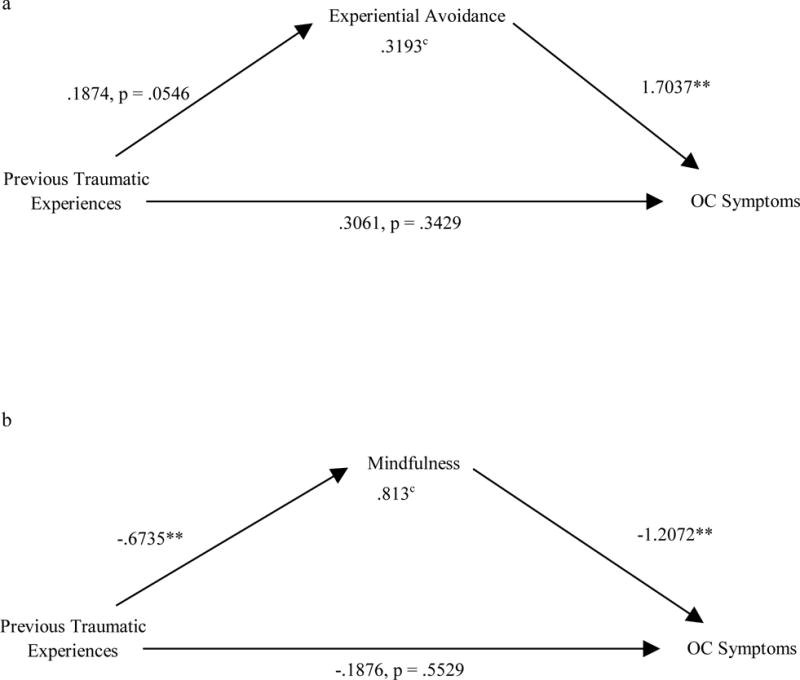
a: Unstandardized coefficients for association between previous trauma and obsessive-compulsive symptoms, as mediated by experiential avoidance in adolescent sample
b: Unstandardized coefficients for association between previous trauma and obsessive-compulsive symptoms, as mediated by mindfulness in adolescent sample
* = p < .05, ** = p < .01, c = CI does not include zero
Previous Traumatic Experiences = ETISR-SF Score
Experiential Avoidance = AAQ-II Score
Mindfulness = CAMM-10 Score
OC symptoms = OCIR-R Score
Mindfulness
Previous trauma was related to mindfulness (coefficient: -0.67, CI: [-1.03, -0.32], p < .001). Mindfulness was related to OC symptoms (coefficient: -1.21, CI: [-1.66, -0.76], p < .001). A direct effect of previous traumatic experiences on OC symptoms was not observed (coefficient: -0.19, CI: [-0.82, -0.44], p = .55). An indirect effect of mindfulness was observed (coefficient: 0.81, CI: [.38, 1.45]), accounting for more than the total effect (PM = 1.301). See Table 3 and Figure 1b for results.
Results—Study 2
Descriptive statistics are reported in Table 2. Item-level missing data for the AAQ, FFMQ, PHQ-9, GAD-7, and OCI-R were handled using mean imputation if only one item on a relevant scale or subscale was missing. If two or more items from the scale were missing, the scale was counted as missing, and the PROCESS macro did not include the data. For the ETI, zeros were imputed in cases where less than 20% of the items were missing. Additionally, three participants did not report their gender and four reported their gender as “other,” and because imputation is not appropriate, these participants were excluded from analyses. The current mediation analyses included 390 participants, and 24 participants were excluded from analyses.
Obsessive-Compulsive Symptoms
Avoidance
When examining the indirect effect of avoidance on the association between previous traumatic experiences and OC symptoms, the following results were observed. Previous trauma was related to avoidance (coefficient: .76, CI: [.59, .93], p < .001). Avoidance was significantly related to OC symptoms (coefficient: .44, CI: [.29, .59], p < .001). A direct effect of previous trauma on OC symptoms was observed (coefficient: .66, CI: [.39, .94], p <.001). An indirect effect of avoidance was observed (coefficient: .33, CI: [.21, .48]), accounting for a proportion of the total effect (PM = .33). See Table 4 and Figure 2a for results.
Table 4.
Association between previous trauma and obsessive-compulsive symptoms, as mediated by experiential avoidance in college student sample.
| Outcome Variable | Predictor | Coefficient (SE) | CI | t | p |
|---|---|---|---|---|---|
| AAQ−II | ETI | .76 (.09) | [.59, .93] | 8.79 | <.001 |
| Gender | .01 (.005) | [−.001, .02] | 1.67 | .10 | |
| OCI−R | AAQ−II | .44 (.08) | [.29, .59] | 5.78 | <.001 |
| ETI | .66 (.14) | [.39, .94] | 4.74 | <.001 | |
| Gender | .01 (.01) | [−.002, .03] | 1.78 | .08 | |
| Indirect Effect | Effect (Boot SE) | BootCI | |||
| OCI−R | AAQ−II | .33 (.07) | [.21, .48] |
Note. N = 390. ETI = Early Trauma Inventory (total number of previous traumatic experiences). AAQ-II = Acceptance and Action Questionnaire, second version. OCI-R = Obsessive Compulsive Inventory – Revised. Boot SE = Bootstrapped Standard Error. CI = Confidence Interval. BootCI = Bootstrapped Confidence Interval.
Figure 2.
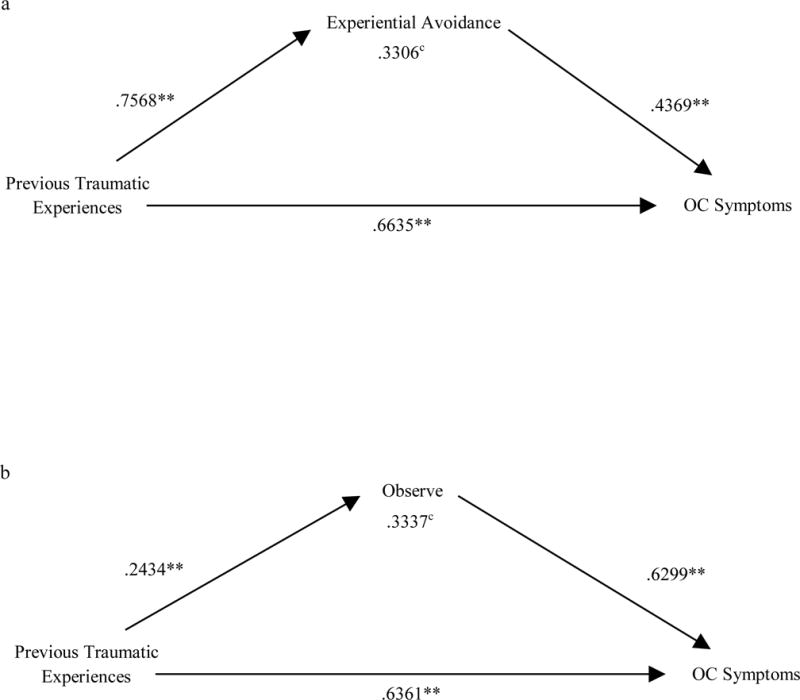
a: Unstandardized coefficients for association between previous trauma and obsessive-compulsive symptoms, as mediated by experiential avoidance in college student sample
b: Unstandardized coefficients for association between previous trauma and obsessive-compulsive symptoms, as mediated by observe facet of mindfulness in college student sample
* = p < .05, ** = p < .01, c = CI does not include zero
Previous Traumatic Experiences = ETISR-SF Score
Experiential Avoidance = AAQ-II Score
Observe = FFMQ Observe Score
OC symptoms = OCIR-R Score
Mindfulness
The FFMQ subscales were included in a multiple mediation model to simultaneously examine the indirect effect of mindfulness facets on the association between previous trauma on OC symptoms. The first model examined if trauma was related to each facet, controlling for gender. Trauma was related to the Observe (coefficient: .24, CI: [.13, .35], p <.001), Act with Awareness (coefficient: −.27, CI: [−.38, −.16], p < .001), and Nonjudgment facets (−.42, CI: [−.54, −.30], p < .001).Trauma was not related to the Describe (p = .16) or Nonreactivity facets (p = .93).
The second model examined if mindfulness facets and previous trauma related to OC symptoms, while controlling for gender. The Observe (coefficient: .63, CI: [.37, .89], p < .001) and Describe (coefficient: −.46, CI: [−.71, −.21], p = .0003) facets related to OC symptoms. The Act with Awareness (p = .08), Nonjudgment (p = .11), and Nonreactivity (p = .87) facets were not related to OC symptoms. A direct effect of previous trauma was observed (coefficient: .64, CI: [.38, .89], p <.001). Gender was a significant covariate (coefficient: .02, CI: [.002, .03], p = .02).
Mediation analyses indicated that the Observe facet was the only significant indirect effect (coefficient: .33, CI: [.20, .51]), accounting for a proportion of the total effect (PM = .16). See Table 5 and Figure 2b for results.
Table 5.
Association between previous trauma and obsessive-compulsive symptoms, as mediated by five facets of mindfulness in college student sample.
| Outcome Variable | Predictor | Coefficient (SE) | CI | t | p |
|---|---|---|---|---|---|
| FFMQ | |||||
| Observe | ETI | .24 (.06) | [.13, .35] | 4.38 | <.001 |
| Gender | .00 (.003) | {−.01, .01] | −.02 | .99 | |
| Describe | ETI | −.08 (.06) | [−.19, .03] | −1.41 | .16 |
| Gender | .002 (.003) | [−.005, .008] | .46 | .64 | |
| Act with Awareness | ETI | −.27 (.06) | [−.38, −.16] | −4.73 | <.001 |
| Gender | −.003 (.003) | [−.01, .003] | −.99 | .32 | |
| Nonjudgmental | ETI | −.42 (.06) | [−.54, −.30] | −6.80 | <.001 |
| Gender | −.0002 (.003) | [−.007, .01] | −.07 | .94 | |
| Nonreactivity | ETI | −.004 (.04) | [−.09, .08] | −.09 | .93 |
| Gender | −.003 (.002) | [−.01, .001] | −1.40 | .001 | |
| OCI−R | FFMQ | ||||
| Observe | .63 (.13) | [.37, .89] | 4.74 | <.001 | |
| Describe | −.46 (.13) | [−.71, −.21] | −3.66 | <.001 | |
| Act with Awareness | −.23 (.13) | [−.48, .03] | −1.75 | .08 | |
| Nonjudgmental | −.20 (.12) | [−.44, .05] | −1.60 | .11 | |
| Nonreactivity | −.03 (.17) | [−.37, .31] | −.16 | .87 | |
| ETI | .64 (.13) | [.38, .89] | 4.85 | < .001 | |
| Gender | .02 (.01) | [.002, .03] | 2.29 | .02 | |
| Indirect Effect | Effect (Boot SE) | BootCI | |||
|
| |||||
| OCI−R | FFMQ | ||||
| Observe | .33 (.08) | [.20, .51] | |||
| Describe | .04 (.03) | [−.01, .10] | |||
| Act with Awareness | .06 (.03) | [−.001, .14] | |||
| Nonjudgmental | .08 (.05) | [−.01, .19] | |||
| Nonreactivity | .0001 (.01) | [−.01, .20] | |||
Note. N = 391. FFMQ = Five Facet Mindfulness Questionnaire; ETI = Early Trauma Inventory (total number of previous traumatic experiences). Boot SE = Bootstrapped Standard Error. CI = Confidence Interval. BootCI = Bootstrapped Confidence Interval.
Internalizing Symptoms
Avoidance
Previous trauma was significantly related to avoidance (coefficient: .73, CI: [.57, .89], p < .001). Avoidance was related to internalizing symptoms (coefficient: .06, CI: [.06, .07], p < .001). A direct effect of previous trauma was observed (coefficient: .04, CI: [.02, .06], p <.001). An indirect effect of avoidance was observed (coefficient: .05, CI: [.03, .06]), accounting for over half of the total effect (PM = .54). See Table 6 and Figure 3a for results.
Table 6.
Association between previous trauma and internalizing symptoms, as mediated by experiential avoidance in college student sample.
| Outcome Variable | Predictor | Coefficient (SE) | CI | t | p |
|---|---|---|---|---|---|
| AAQ-II | ETI | .73 (.08) | [.57, .89] | 8.85 | <.001 |
| Gender | 2.82 (.74) | [1.36, 3.79] | 3.79 | <.001 | |
| Internalizing Symptoms | AAQ-II | .06 (.005) | [.06, .07] | 14.09 | <.001 |
| ETI | .04 (.01) | [.02, .06] | 4.92 | <.001 | |
| Gender | .08 (.07) | [−.05, .22] | 1.21 | .23 | |
| Indirect Effect | Effect (Boot SE) | BootCI | |||
| OCI-R | AAQ-II | .05 (.01) | [.03, .06] |
Note. N = 394. ETI = Early Trauma Inventory (total number of previous traumatic experiences). AAQ-II = Acceptance and Action Questionnaire, second version. OCI-R = Obsessive Compulsive Inventory – Revised. Boot SE = Bootstrapped Standard Error. CI = Confidence Interval. BootCI = Bootstrapped Confidence Interval.
Figure 3.
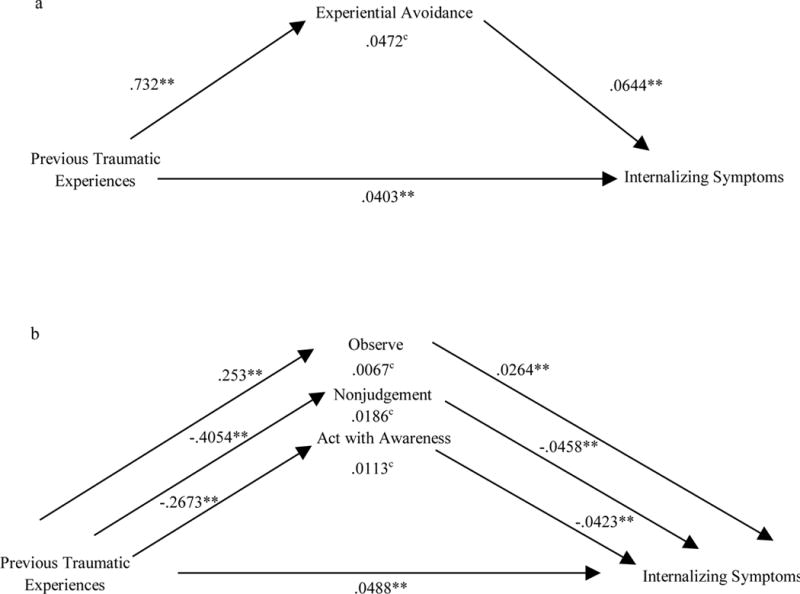
a: Unstandardized coefficients for association between previous trauma and internalizing symptoms, as mediated by experiential avoidance in college student sample
b: Unstandardized coefficients for association between previous trauma and internalizing symptoms, as mediated by observe, nonjudgment, and act with awareness facets of mindfulness in college student sample
* = p < .05, ** = p < .01, c = CI does not include zero
Previous Traumatic Experiences = ETISR-SF Score
Experiential Avoidance = AAQ-II Score
Observe = FFMQ Observe Score
Nonjudgment = FFMQ Nonjudgment Score
Act with Awareness = FFMQ Act with Awareness Score
Internalizing Symptoms = GAD-7 and PHH-9 Internalizing Composite Factor Score
Mindfulness
Trauma was related to the Observe (coefficient: .25, CI: [.15, .36], p <.001), Act with Awareness (coefficient: −.27, CI: [−.38, −.16], p < .001), and Nonjudgment facets (coefficient: −.41, CI: [−.52, −.29], p < .001). Trauma did not predict the Describe (p = .15) or Nonreactivity facets (p = .98).
The second model examined if mindfulness facets and previous trauma related to internalizing symptoms, while controlling for gender. The Observe (coefficient: .03, CI: [.01, .04], p < .01) Act with Awareness (coefficient: −.04, CI: [−.06, −.03], p < .001), Nonjudgment (coefficient: −.05, CI: [−.06, −.03], p <.001), and Nonreactivity (coefficient: −.03, CI: [−.05, −.004], p = .02) facets were related to internalizing symptoms. The Describe facet did not (p = .11). Gender was a significant covariate (coefficient: .21, CI: [.07, .35], p < .01). A direct effect of previous trauma on internalizing symptoms was observed (coefficient: .05, CI: [.03, .06], p <.001).
The Observe, (coefficient: .01, CI: [.003, .01]), Act with Awareness (coefficient: .01, CI: [.01, .02]) and Nonjudgment (coefficient: .02, CI: .01, .03]) facets were significant indirect effects in the relation between previous trauma and internalizing symptoms. Percent mediation statistics indicated that the mindfulness facets accounted for portions of the total effect: Observe (PM = .08), Act with Awareness (PM = .13), and Nonjudgment (PM = .22). See Table 7 and Figure 3b for results.
Table 7.
Association between previous trauma and internalizing symptoms, as mediated by five facets of mindfulness in college student sample.
| Outcome Variable | Predictor | Coefficient (SE) | CI | t | p |
|---|---|---|---|---|---|
| FFMQ | |||||
| Observe | ETI | .25 (.05) | [.15, .36] | 4.67 | <.001 |
| Gender | .03 (.49) | {−.93, .99] | .06 | .95 | |
| Describe | ETI | −.08 (.06) | [−.19, .03] | −1.43 | .15 |
| Gender | −.15 (.51) | [−1.15, .84] | −.30 | .76 | |
| Act with Awareness | ETI | −.27 (.06) | [−.38, −.16] | −4.86 | <.001 |
| Gender | .60 (.49) | [−.37, 1.57] | 1.22 | .22 | |
| Nonjudgmental | ETI | −.41 (.06) | [−.52, −.29] | −6.76 | <.001 |
| Gender | −.65 (.54) | [−1.71, .41] | −1.21 | .23 | |
| Nonreactivity | ETI | −.001 (.04) | [−.08, .08] | −.03 | .98 |
| Gender | −1.17 (.36) | [−1.88, −.46] | −3.25 | .001 | |
| Internalizing Symptoms | FFMQ | ||||
| Observe | .03 (.008) | [.01, .04] | 3.16 | .002 | |
| Describe | −.01 (.008) | [−.03, .003] | −1.59 | .11 | |
| Act with Awareness | −.04 (.008) | [−.06, −.03] | −5.20 | <.001 | |
| Nonjudgmental | −.05 (.008) | [−.06, −.03] | −5.89 | <.001 | |
| Nonreactivity | −.03 (.01) | [−.05, −.004] | −2.37 | .02 | |
| ETI | .05 (.008) | [.03, .06] | 6.01 | < .001 | |
| Gender | .21 (.07) | [.07, .35] | 3.02 | .003 | |
| Indirect Effect | Effect (Boot SE) | BootCI | |||
|
| |||||
| OCI−R | FFMQ | ||||
| Observe | .01 (.003) | [.003, .01] | |||
| Describe | .001 (.001) | [−.0002, .004] | |||
| Act with Awareness | .01 (.003) | [.006, .02] | |||
| Nonjudgmental | .02 (.004) | [.01, .03] | |||
| Nonreactivity | .0000 (.001) | [−.002, .002] | |||
Note. N = 391. FFMQ = Five Facet Mindfulness Questionnaire; ETI = Early Trauma Inventory (total number of previous traumatic experiences). Boot SE = Bootstrapped Standard Error. CI = Confidence Interval. BootCI = Bootstrapped Confidence Interval.
Discussion
These studies illustrate the importance of two important targets for intervention, avoidance and mindfulness, in the relation between traumatic experiences and psychiatric symptoms. The first study examined this association in a sample of at-risk adolescents, where the mean number of previous traumatic events was greater than 1 SD above the normative values in the validation study for the trauma measure (Bremner et al., 2007). In this study, when controlling for the mediators, the direct effect of trauma on obsessive-compulsive symptoms was not significant. Furthermore, the indirect effects of avoidance and mindfulness both accounted for over half of the total effect. These findings indicate that among adolescents who have experienced trauma, avoidance and mindfulness are key determinants in predicting obsessive-compulsive symptoms. Nevertheless, significant limitations of this study (small N, limited power) rendered us unable to explore the impact of trauma and mediating variables on internalizing symptoms. Thus, a second study with a larger sample size allowed for the measurement and examination of internalizing symptoms with gender as a covariate.
In the second study, among a sample of college undergraduates, we examined the mediating role of avoidance and mindfulness in the association between traumatic experiences and obsessive-compulsive symptoms and found that avoidance was a significant mediator. Additionally, through the examination of specific mindfulness processes, findings indicated the Observe facet as a significant indirect effect, associated with higher obsessive-compulsive symptoms. Next, the role of these mediators were examined in the relation between traumatic experiences and internalizing symptoms, and avoidance accounted for over half of this total effect. Further, Observe, Act with Awareness, and Nonjudgment also accounted for a substantial proportion of the total effect, with Nonjudgment accounting for the highest proportion of the total effect.
The differences in findings between the two samples are notable. The inclusion of two samples allowed for comparison of the results between high-risk and normative groups. The younger, high-risk sample reported higher levels of experienced trauma than the older, college student sample. The high-risk sample was also more diverse and were known to be experiencing difficulties academically, socially, or otherwise. Importantly, in Study 1, the direct effect from traumatic experiences to OC symptoms was not significant, though in Study 2, this relation was significant. More recent conceptualizations of mediation (Hayes, 2013) do not require the presence of the X→Y relation to conduct mediation analyses, but previous thinking necessitated such a relation (Baron and Kenny, 1986). This difference in results is important, as it may underscore the importance of avoidance and mindfulness in the progression from experiencing trauma to later OC symptoms. Further, if avoidance and mindfulness are in fact implicated as important determinants in the relation between traumatic experiences and later psychological symptoms, early intervention and prevention programs could specifically target these processes with children and adolescents who have experienced trauma. Future longitudinal research is necessary to examine the role of avoidance and mindfulness in this relation, as well as appropriate interventions to address these processes.
The current findings support previous work that has identified avoidance as a mediator of the association between trauma and various psychological outcomes (Marx and Sloan, 2002; Orcutt et al., 2005; Reddy et al., 2006; Rosenthal et al., 2005). Avoidance was a powerful mediator between trauma exposure and psychological functioning for OC symptoms, in both high-risk and nonclinical samples. These findings are also consistent with the previously identified role of experiential avoidance in other trauma-related psychopathology, such as PTSD (Tull and Roemer, 2003). Avoidance of trauma-related memories, thoughts, and emotions may be one of the most common coping strategies among individuals exposed to trauma (Tull et al., 2004). However, chronic avoidance maintains the power of the internal stimuli, resulting in distress, dysregulation, and continued psychopathology (Gross and Levenson, 1997; Hayes et al., 1999; Shipherd and Beck, 1999). The current study contributes additional evidence showcasing how experiential avoidance after trauma exposure can contribute to psychopathology, in the form of increased OC and internalizing symptoms in young adult samples. Improved treatment efforts aimed at reducing avoidance are crucial in order to address trauma-related psychiatric difficulties, including depression, anxiety, and OCD.
In relation to specific mindfulness facets and psychopathology, higher Observe skills were predictive of more severe OC symptoms and internalizing symptoms. Anxiety disorders are theorized to arise from continual overestimates of the dangerousness of situations (social anxiety, agoraphobia), one’s own physical sensations (panic disorder), or one’s own thoughts (OCD; Abramowitz et al., 2003; Clark, 1999). For individuals with OCD, there is a strong belief that unwanted thoughts about an action are equivalent to completing the action or that it makes the action more likely to occur, known as thought-action fusion (Shafran et al., 1996). These maladaptive cognitions often lead to behavioral or cognitive rituals in an attempt to eliminate the thought, creating a cycle of obsessive thoughts and subsequent compulsions (Rachman, 1998). Therefore, heightened observation of mental imagery may create more distress and, thus, more severe OC symptoms.
The Act with Awareness and Nonjudgment facets predicted lower internalizing symptoms in the college sample. This is in line with previous work by Cash and Whittingham (2010) which found that higher levels of nonjudgment and acting with awareness facets of mindfulness were related to lower levels of depressive symptoms as well as lower levels of anxiety and stress-related symptoms (for the nonjudgment facet only). Further, young adults with a lack of mindfulness skills may be particularly susceptible to depressive and anxiety symptoms. In an undergraduate sample, Soysa and Wilcomb (2015) found that lower levels of acting with mindful awareness and lower levels of nonjudgment of experience predicted depression and stress, while lower levels of mindful nonjudgment also predicted anxiety. Rumination (Aldao et al., 2010), as well as negative judgment of thoughts, internal sensations, and self (Johnson et al., 1992; McNally, 1990; Rimes and Watkins, 2005) have long been characteristic of internalizing disorders—areas for which increased skills in mindful awareness and nonjudgment could be particularly useful.
Clinical Implications
The current studies helped to further elucidate specific targets for clinical interventions. First, individuals who have experienced trauma may be more likely to engage in avoidant coping strategies (Follette et al., 2006), and while these strategies may be effective in providing short-term relief from unpleasant internal experiences, avoidance often leads to an increased salience of the unwanted stimulus in the long-term (Chawla and Ostafin, 2007; Thompson et al., 2011).
Additionally, the identification of specific mindfulness facets as mechanistic processes that help account for the association between trauma and obsessive-compulsive and internalizing symptoms helps to provide a more precise understanding of which individual facets of mindfulness may be particularly important in terms of explaining these associations, and subsequently, which facets may be most important to target clinically in this population. The current study’s identification of the observe facet of mindfulness as a predictor of greater internalizing and OC symptoms is in line with previous work showing that interventions targeted at improving the observation of experience alone may not be particularly helpful unless coupled with the cultivation of other mindfulness processes (Desrosiers et al., 2014, 2013). Further, the current findings indicate that acting with awareness (acting with attention to behavior rather than running on “auto-pilot”) and nonjudgment of inner experience may be important mindfulness processes to focus on for trauma-exposed individuals. Mindfulness- and acceptance-based interventions, including ACT (Hayes et al., 1999) and MBSR (Kabat-Zinn, 1990), which aim to help individuals to increase acceptance, to relate to internal experiences nonjudgmentally, and to remain aware while engaging in behavior, may improve psychological outcomes for individuals who have experienced childhood trauma.
Limitations
The first study had a small sample size, which limited our ability to control for gender. This led us to conduct a second study among a sample of college undergraduates using a larger sample and greater range of measures. Nevertheless, the sample of undergraduates was demographically homogenous, lacking the diversity represented in the first sample. In addition, both studies examined a sample with restricted age range, which limits the generalizability of these conclusions to adults. In addition, in both studies, data were self-reported, which introduces the potential for bias. Report on traumatic experiences was retrospective, so the findings are not specific with regard to the timing of the trauma. In addition, adults with more psychosocial problems may be prone to recall more childhood traumatic experiences (Widom et al., 2004), indicating the need for prospective research on the longitudinal impact of trauma. Finally, the number of traumatic experiences was examined collectively (a total number of traumas). Thus, results are unable to determine if specific traumatic events play a role in later outcomes.
Conclusions
Despite several limitations, the studies have several notable strengths. First, the examination of these associations in two samples of young adults has significant implications for the prevention literature. In samples of youth, particularly those at high-risk for developing psychopathology, interventions that directly address avoidance and mindfulness may be useful for individuals exposed to trauma. Second, the measurement of childhood trauma in the second sample (aged above 18) allows for some degree of temporal precedence to be established. Despite lacking knowledge of when specific traumatic experiences occurred, it is clear that childhood trauma and current avoidance/mindfulness play a significant role in current symptoms. Finally, this study adds to the literature by examining the mediating role of these processes in the relation between trauma and psychiatric symptoms. Given the well-established incidence rates of trauma among both youth and adults, it is critical that research examine the mechanisms by which trauma leads to later adverse outcomes, and this study introduces two key processes that impact said outcomes – avoidance and mindfulness.
In conclusion, the current findings indicate that among two samples of young adults, the association between childhood trauma and obsessive-compulsive symptoms is mediated by avoidance and mindfulness. Furthermore, the second study examined these processes as mediators of the relation between traumatic experiences and internalizing symptoms, finding once again that avoidance and mindfulness were significant mediators. Using the FFMQ, we were able to pinpoint what facets of mindfulness specifically are accounting for this effect. These findings present potential targets for clinical intervention and for examination in future research. Among traumatized young adults, the provision of these specific skills may lead to more favorable psychological outcomes. Thus, changing the way that young adults relate to internal experiences may impact trajectories of psychopathology and help traumatized individuals to build meaningful, rich lives, even in the presence of difficult experiences.
Acknowledgments
Many thanks to Rosaura Orengo-Aguayo, PhD; James Marchman, PhD; and Xin Yu, BA.
Funding: Study 1 was funded by the University of Iowa Graduate and Professional Student Government research grant. Departmental funding from the University of Iowa’s Department of Psychological and Brain Sciences funded Study 2.
Footnotes
Percent mediation statistics can be greater than 1 because the indirect effect is a product of two paths.
References
- Abramowitz JS, Whiteside S, Lynam D, Kalsy S. Is thought-action fusion specific to obsessive-compulsive disorder?: A mediating role of negative affect. Behav Res Ther. 2003;41:1069–1079. doi: 10.1016/S0005-7967(02)00243-7. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clin Psychol Rev. 2010;30:217–237. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Association; 2000. text rev. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Batten SV, Follette VM, Aban IB. Experiential avoidance and high-risk sexual behavior in survivors of child sexual abuse. J Child Sex Abus. 2002;10:101–120. doi: 10.1300/J070v10n02_06. [DOI] [PubMed] [Google Scholar]
- Bluett EJ, Homan KJ, Morrison KL, Levin ME, Twohig MP. Acceptance and Commitment Therapy for anxiety and OCD spectrum disorders: An empirical review. J Anxiety Disord. 2014;28:612–624. doi: 10.1016/j.janxdis.2014.06.008. [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Waltz T, Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire–II: A revised measure of psychological inflexibility and experiential avoidance. Behav Ther. 2011;42:676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Bolus R, Mayer EA. Psychometric properties of the Early Trauma Inventory-Self Report. J Nerv Ment Dis. 2007;195:211–8. doi: 10.1097/01.nmd.0000243824.84651.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs ES, Price IR. The relationship between adverse childhood experience and obsessive-compulsive symptoms and beliefs: The role of anxiety, depression, and experiential avoidance. J Anxiety Disord. 2009;23:1037–1046. doi: 10.1016/j.janxdis.2009.07.004. [DOI] [PubMed] [Google Scholar]
- Brockman C, Snyder J, Gewirtz A, Gird SR, Quattlebaum J, Schmidt N, Pauldine MR, Elish K, Schrepferman L, Hayes C, Zettle R, DeGarmo D. Relationship of service members’ deployment trauma, PTSD symptoms, and experiential avoidance to postdeployment family reengagement. J Fam Psychol. 2016;30:52–62. doi: 10.1037/fam0000152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown J, Cohen P, Johnson JG, Smailes EM. Childhood abuse and neglect: specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry. 1999;38:1490–1496. doi: 10.1097/00004583-199912000-00009. [DOI] [PubMed] [Google Scholar]
- Cash M, Whittingham K. What facets of mindfulness contribute to psychological well-being and depressive, anxious, and stress-related symptomatology? Mindfulness. 2010;1:177–182. doi: 10.1007/s12671-010-0023-4. [DOI] [Google Scholar]
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82:217–225. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- Chawla N, Ostafin B. Experiential avoidance as a functional dimensional approach to psychopathology: An empirical review. J Clin Psychol. 2007;63:871–890. doi: 10.1002/jclp.20400. [DOI] [PubMed] [Google Scholar]
- Clark DM. Anxiety disorders: Why they persist and how to treat them. Behav Res Ther. 1999 doi: 10.1016/S0005-7967(99)00048-0. [DOI] [PubMed] [Google Scholar]
- Cordova JV. Acceptance in behavior therapy: Understanding the process of change. Behav Anal. 2001;24:213–226. doi: 10.1007/BF03392032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cougle JR, Timpano KR, Sachs-Ericsson N, Keough ME, Riccardi CJ. Examining the unique relationships between anxiety disorders and childhood physical and sexual abuse in the National Comorbidity Survey-Replication. Psychiatry Res. 2010;177:150–155. doi: 10.1016/j.psychres.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Cromer KR, Schmidt NB, Murphy DL. An investigation of traumatic life events and obsessive-compulsive disorder. Behav Res Ther. 2007;45:1683–1691. doi: 10.1016/j.brat.2006.08.018. [DOI] [PubMed] [Google Scholar]
- Curtis AC. Defining adolescence. J Adolesc Fam Heal. 2015;7 article 2. http://scholar.utc.edu/jafh/vol7/iss2/2. [Google Scholar]
- De Luca V, Gershenzon V, Burroughs E, Javaid N, Richter MA. Age at onset in Canadian OCD patients: Mixture analysis and systematic comparison with other studies. J Affect Disord. 2011;133:300–304. doi: 10.1016/j.jad.2011.03.041. [DOI] [PubMed] [Google Scholar]
- Desrosiers A, Klemanski DH, Nolen-Hoeksema S. Mapping mindfulness facets onto dimensions of anxiety and depression. Behav Ther. 2013;44:373–384. doi: 10.1016/j.beth.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desrosiers A, Vine V, Curtiss J, Klemanski DH. Observing nonreactively: A conditional process model linking mindfulness facets, cognitive emotion regulation strategies, and depression and anxiety symptoms. J Affect Disord. 2014;165:31–37. doi: 10.1016/j.jad.2014.04.024. [DOI] [PubMed] [Google Scholar]
- do Rosario-Campos MC, Leckman JF, Mercadante MT, Shavitt RG, Prado H da S, Sada P, Zamignani D, Miguel EC. Adults with early-onset obsessive-compulsive disorder. Am J Psychiatry. 2001;158:1899–1903. doi: 10.1176/appi.ajp.158.11.1899. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. Am J Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Elzy M, Clark C, Dollard N, Hummer V. Adolescent girls’ use of avoidant and approach coping as moderators between trauma exposure and trauma symptoms. J Fam Violence. 2013;28:763–770. doi: 10.1007/s10896-013-9546-5. [DOI] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Frequency, comorbidity, and psychosocial impairment of anxiety disorders in German adolescents. J Anxiety Disord. 2000;14:263–279. doi: 10.1016/S0887-6185(99)00039-0. [DOI] [PubMed] [Google Scholar]
- Fierman EJ, Hunt MF, Pratt LA, Warshaw MG, Yonkers KA, Peterson LG, Epstein-Kaye TM, Norton HS. Trauma and posttraumatic stress disorder in subjects with anxiety disorders. Am J Psychiatry. 1993;150:1872–1874. doi: 10.1176/ajp.150.12.1872. [DOI] [PubMed] [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, Salkovskis PM, Coles ME, Amir N. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychol Assess. 2002;14:485–496. doi: 10.1037/1040-3590.14.4.485. [DOI] [PubMed] [Google Scholar]
- Follette V, Palm KM, Pearson AN. Mindfulness and trauma: implications for treatment. J Ration Cogn Ther. 2006;24:45–61. doi: 10.1007/s10942-006-0025-2. [DOI] [Google Scholar]
- Fontenelle LF, Cocchi L, Harrison BJ, Shavitt RG, do Rosário MC, Ferrão YA, de Mathis MA, Cordioli AV, Yücel M, Pantelis C, Mari J de J, Miguel EC, Torres AR. Towards a post-traumatic subtype of obsessive-compulsive disorder. J Anxiety Disord. 2012;26:377–383. doi: 10.1016/j.janxdis.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Ford JD. Trauma exposure and posttraumatic stress disorder in the lives of adolescents. J Am Acad Child Adolesc Psychiatry. 2013;52:780–783. doi: 10.1016/j.jaac.2013.05.012. [DOI] [PubMed] [Google Scholar]
- Ford JD, Elhai JD, Connor DF, Frueh BC. Poly-victimization and risk of posttraumatic, depressive, and substance use disorders and involvement in delinquency in a national sample of adolescents. J Adolesc Heal. 2010;46:545–552. doi: 10.1016/j.jadohealth.2009.11.212. [DOI] [PubMed] [Google Scholar]
- Forman EM, Herbert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of Acceptance and Commitment Therapy and cognitive therapy for anxiety and depression. Behav Modif. 2007;31:772–799. doi: 10.1177/0145445507302202. [DOI] [PubMed] [Google Scholar]
- Gradus JL. Epidemiology of PTSD. 2017 Retrieved from http://www.ptsd.va.gov/professional/PTSD-overview/epidemiological-facts-ptsd.asp.
- Greco L, Baer R, Smith G. Assessing mindfulness in children and adolescents: Development and validation of the Child and Adolescent Mindfulness Measure (CAMM) Psychol Assess. 2011;23:606–614. doi: 10.1037/a0022819. [DOI] [PubMed] [Google Scholar]
- Greco L, Lambert W, Baer R. Psychological inflexibility in childhood and adolescence: Development and evaluation of the Avoidance and Fusion Questionnaire for Youth. Psychol Assess. 2008;20:93–102. doi: 10.1037/1040-3590.20.2.93. [DOI] [PubMed] [Google Scholar]
- Gross JJ, Levenson RW. Hiding feelings: the acute effects of inhibiting negative and positive emotion. J Abnorm Psychol. 1997;106:95–103. doi: 10.1037/0021-843X.106.1.95. [DOI] [PubMed] [Google Scholar]
- Hayes A. Introduction to mediation, moderation, and conditional process analysis. New York, NY: Guilford; 2013. pp. 3–4. doi: 978-1-60918-230-4. [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: An experiential approach to behavior change. New York: 1999. [DOI] [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Follette VMK, et al. Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. J Consult Clin Psychol. 1996;64:1152–1168. doi: 10.1037/0022-006X.64.6.1152. [DOI] [PubMed] [Google Scholar]
- Heim CM, Nemeroff CB. The role of childhood trauma in the neurobiology of mood and anxiety disorders: Preclinical and clinical studies. Biol Psychiatry. 2001;49:1023–1039. doi: 10.1016/S0006-3223(01)01157-X. [DOI] [PubMed] [Google Scholar]
- Johnson K, Johnson J, Petzel T. Social anxiety, depression, and distorted cognitions in college students. Soc Clin Psychol. 1992;11:181–195. doi: 10.1521/jscp.1992.11.2.181. [DOI] [Google Scholar]
- Johnson SB, Blum RW, Giedd JN. Adolescent maturity and the brain: the promise and pitfalls of neuroscience research in adolescent health policy. J Adolesc Heal. 2009;45:216–221. doi: 10.1016/j.jadohealth.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clin Psychol Sci Pract. 2003;10:144–156. doi: 10.1093/clipsy/bpg016. [DOI] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Dell Publishing; New York: 1990. [Google Scholar]
- Kendall-Tackett KA, Williams LM, Finkelhor D. Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychol Bull. 1993;113:164–180. doi: 10.1037/0033-2909.113.1.164. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Saunders B, Resnick HS, Best CL, Schnurr PP. Risk factors for adolescent substance abuse and dependence: Data from a national sample. J Consult Clin Psychol. 2000;68:19–30. doi: 10.1037/0022-006X.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafleur DL, Petty C, Mancuso E, McCarthy K, Biederman J, Faro A, Levy HC, Geller DA. Traumatic events and obsessive compulsive disorder in children and adolescents: Is there a link? J Anxiety Disord. 2011;25:513–519. doi: 10.1016/j.janxdis.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Land K. Doctoral Dissertation. Alliant International University; San Francisco, CA: 2010. Examining the role of experiential avoidance specific to post-trauma symptoms. [Google Scholar]
- Lochner C, du Toit PL, Zungu-Dirwayi N, Marais A, van Kradenburg J, Seedat S, Niehaus DJH, Stein DJ. Childhood trauma in obsessive-compulsive disorder, trichotillomania, and controls. Depress Anxiety. 2002;15:66–68. doi: 10.1002/da.10028. [DOI] [PubMed] [Google Scholar]
- Marx BP, Sloan DM. The role of emotion in the psychological functioning of adult survivors of childhood sexual abuse. Behav Ther. 2002;33:563–577. doi: 10.1016/S0005-7894(02)80017-X. [DOI] [Google Scholar]
- McNally RJ. Psychological approaches to panic disorder: a review. Psychol Bull. 1990;108:403–419. doi: 10.1037/0033-2909.108.3.403. [DOI] [PubMed] [Google Scholar]
- Miller ML, Brock RL. The effect of trauma on the severity of obsessive-compulsive spectrum symptoms: A meta-analysis. J Anxiety Disord. 2017;47:29–44. doi: 10.1016/j.janxdis.2017.02.005. [DOI] [PubMed] [Google Scholar]
- Orcutt HK, Pickett SM, Pope EB. Experiential avoidance and forgiveness as mediators in the relation between traumatic interpersonal events and posttraumatic stress disorder symptoms. J Soc Clin Psychol. 2005;24:1003–1029. doi: 10.1521/jscp.2005.24.7.1003. [DOI] [Google Scholar]
- Orsillo SM, Batten SV. Acceptance and Commitment Therapy in the treatment of posttraumatic stress disorder. Behav Modif. 2005;29:95–129. doi: 10.1177/0145445504270876. [DOI] [PubMed] [Google Scholar]
- Paus T, Keshavan M, Giedd JN. Why do many psychiatric disorders emerge during adolescence? Nat Rev Neurosci. 2008;9:947–957. doi: 10.1038/nrn2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachman S. A cognitive theory of obsessions: Elaborations. Behav Res Ther. 1998;36:385–401. doi: 10.1016/S0005-7967(97)10041-9. [DOI] [PubMed] [Google Scholar]
- Reddy MK, Pickett SM, Orcutt HK. Experiential avoidance as a mediator in the relationship between childhood psychological abuse and current mental health symptoms in college students. J Emot Abus. 2006;6:67–85. doi: 10.1300/J135v06n01_04. [DOI] [Google Scholar]
- Rimes KA, Watkins E. The effects of self-focused rumination on global negative self-judgements in depression. Behav Res Ther. 2005;43:1673–1681. doi: 10.1016/j.brat.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Rosenthal ZM, Rasmussen Hall ML, Palm KM, Batten SV, Follette V. Chronic avoidance helps explain the relationship between severity of childhood sexual abuse and psychological distress in adulthood. J Child Sex Abus. 2005;14:25–41. doi: 10.1300/J070v14n04_02. [DOI] [PubMed] [Google Scholar]
- Russell D, Springer KW, Greenfield EA. Witnessing domestic abuse in childhood as an independent risk factor for depressive symptoms in young adulthood. Child Abuse Negl. 2010;34:448–453. doi: 10.1016/j.chiabu.2009.10.004. http://dx.doi.org/10.1016/j.chiabu.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafran R, Thordarson DS, Rachman S. Thought-action fusion in obsessive compulsive disorder. J Anxiety Disord. 1996;10:379–391. doi: 10.1016/0887-6185(96)00018-7. [DOI] [Google Scholar]
- Shipherd JC, Beck JG. The effects of suppressing trauma-related thoughts on women with rape-related posttraumatic stress disorder. Behav Res Ther. 1999;37:99–112. doi: 10.1016/S0005-7967(98)00136-3. [DOI] [PubMed] [Google Scholar]
- Soysa CK, Wilcomb CJ. Mindfulness, self-compassion, self-efficacy, and gender as predictors of depression, anxiety, stress, and well-being. Mindfulness (N Y) 2015;6:217–226. doi: 10.1007/s12671-013-0247-1. [DOI] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B, Faraone SV. Long-term outcome of pediatric obsessive-compulsive disorder: A meta-analysis and qualitative review of the literature. Acta Psychiatr Scand. 2004;110:4–13. doi: 10.1111/j.1600-0447.2004.00302.x. [DOI] [PubMed] [Google Scholar]
- Strosahl KD, Robinson PJ, Gustavsson T. Inside this moment: A clinician’s guide to promoting radical change using Acceptance and Commitment Therapy. Oakland, CA: Context Press; 2015. [Google Scholar]
- Swain J, Hancock K, Hainsworth C, Bowman J. Acceptance and Commitment Therapy in the treatment of anxiety: A systematic review. Clin Psychol Rev. 2013;33:965–978. doi: 10.1016/j.cpr.2013.07.002. [DOI] [PubMed] [Google Scholar]
- Thompson RW, Arnkoff DB, Glass CR. Conceptualizing mindfulness and acceptance as components of psychological resilience to trauma. Trauma Violence Abuse. 2011;12:220–235. doi: 10.1177/1524838011416375. [DOI] [PubMed] [Google Scholar]
- Tull MT, Gratz KL, Salters K, Roemer L. The role of experiential avoidance in posttraumatic stress symptoms and symptoms of depression, anxiety, and somatization. J Nerv Ment Dis. 2004;192:754–761. doi: 10.1097/01.nmd.0000144694.30121.89. [DOI] [PubMed] [Google Scholar]
- Tull MT, Roemer L. Alternative explanations of emotional numbing of posttraumatic stress disorder: An examination of hyperarousal and experiential avoidance. J Psychopathol Behav Assess. 2003;25:147–154. doi: 10.1023/A:1023568822462. [DOI] [Google Scholar]
- Twohig MP, Hayes SC, Plumb JC, Pruitt LD, Collins AB, Hazlett-Stevens H, Woidneck MR. A randomized clinical trial of Acceptance and Commitment Therapy versus Progressive Relaxation Training for obsessive compulsive disorder. J Consult Clin Psychol. 2010;78:705–716. doi: 10.1037/a0020508.A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Child maltreatment 2014. 2016 Retrieved from https://www.acf.hhs.gov/cb/resource/child-maltreatment-2014.
- Valleni-Basile LA, Garrison CZ, Jackson KL, Waller JL, McKeown RE, Addy CL, Cuffe SP. Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad Child Adolesc Psychiatry. 1994;33:782–91. doi: 10.1097/00004583-199407000-00002. [DOI] [PubMed] [Google Scholar]
- Venta A, Sharp C, Hart J. The relation between anxiety disorder and experiential avoidance in inpatient adolescents. Psychol Assess. 2012;24:240–248. doi: 10.1037/a0025362. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Niles B, Pietrefesa A, Schmertz SK, Potter CM. Mindfulness in the treatment of posttraumatic stress disorder among military veterans. Spiritual Clin Pract. 2013;1:15–25. doi: 10.1037/2326-4500.1.S.15. [DOI] [Google Scholar]
- Wang X, Cui D, Wang Z, Fan Q, Xu H, Qiu J, Chen J, Zhang H, Jiang K, Xiao Z. Cross-sectional comparison of the clinical characteristics of adults with early-onset and late-onset obsessive compulsive disorder. J Affect Disord. 2012;136:498–504. doi: 10.1016/j.jad.2011.11.001. [DOI] [PubMed] [Google Scholar]
- Widom CS, Raphael KG, DuMont KA. The case for prospective longitudinal studies in child maltreatment research: Commentary on Dube, Williamson, Thompson, Felitti, and Anda (2004) Child Abus Negl. 2004;28:715–722. doi: 10.1016/j.chiabu.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Zohar AH. The epidemiology of obsessive-compulsive disorder in children and adolescents. Child Adolesc Psychiatr Clin N Am. 1999;8:445–60. [PubMed] [Google Scholar]


