Abstract
To establish the point prevalence of hallucinations in borderline personality disorder (BPD), telephone interviews were conducted with 324 outpatients diagnosed with BPD. Then a subgroup (n = 98) was interviewed in person to investigate the co-occurrence of these phenomena with other psychotic symptoms, comorbid psychiatric disorders, prior childhood adversities, and adult life stressors. For hallucinations in general a point prevalence of 43% was found, with rates for hallucinations in separate sensory modalities ranging from 8–21%. Auditory verbal hallucinations consisted mostly of verbal abuse and were generally experienced as distressing. A significant association was found between the severity of hallucinations on the one hand, and delusions and unusual thought content on the other; this association was absent for negative symptoms and disorganization. The presence of hallucinations also correlated with the number of comorbid psychiatric disorders, and with posttraumatic stress disorder (PTSD) specifically. Childhood emotional abuse and adult life stressors were also associated with hallucinations. The latter three associations suggest that patients with BPD might have an etiological mechanism in common with other patient/nonpatient groups who experience hallucinations. Based on these findings, we advise to treat PTSD and hallucinations when found to be present in patients with BPD.
Introduction
In clinical practice, hallucinations experienced by patients with borderline personality disorder (BPD) are often designated as ‘pseudohallucinations’ to express the suspicion that they do not qualify as hallucinations proper1. One reason for this may be that the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) states that, in the context of BPD, hallucinations occur “only in some individuals during times of stress”2. As a consequence, clinicians may be reluctant to label all positive disorders of perception in this group as hallucinations. However, studies during the last decade indicate that hallucinations proper are far from rare in patients with BPD, with prevalence rates ranging from 26–54%3,4. Moreover, these hallucinations are not restricted to a single sensory modality: 21–59% of them are auditory, 30–33% visual, 10–30% olfactory, and 13% tactile in nature1,3,5–7. In addition, they are often experienced as equally or more severe than those in patients diagnosed with a schizophrenia spectrum disorder6,8 and tend to be present for long periods of time, with a mean history for auditory verbal hallucinations (AVH) of 18 years8,9.
The number of studies on hallucinations in BPD is small, as is the sample size of most of those studies. Moreover, a limitation of the prevalence studies is the impossibility to generalize their results to the overall BPD population, as most of them focused on hospitalized patients3,4,6,9, solely AVH1, and lifetime prevalence rates7. As a consequence, our insights in hallucinations experienced by patients in the BPD group as a whole are still somewhat sketchy. Nevertheless, they are not as rudimentary as our insights into the occurrence of other psychotic symptoms in the context of BPD. Studies have found prevalence rates for delusions ranging from 10% to a full 100%1,4,6,7, whereas negative symptoms and disorganization have hardly been studied in this group. The few authors who did study them, found them to be far less prevalent in the context of BPD than in schizophrenia spectrum disorders4,9.
Regarding etiology, it has been suggested that comorbid psychiatric disorders might well constitute the true cause of hallucinations in BPD10. However, the evidence in support of that view is not univocal. Albeit four studies in the field of BPD found hallucinations and other psychotic symptoms to be associated with comorbid affective and substance-use disorders4,10–12, the presence of these disorders failed to predict any subsequent psychotic symptoms in a study by Miller et al.13 Moreover, Benvenuti et al.14 were unable to establish a difference between psychotic symptoms experienced by patients with BPD with and without a co-morbid mood disorder on a lifetime basis. Also noteworthy is the strong association between childhood adversity and psychotic symptoms in both patient and nonpatient groups15. The latter association was studied in patients with BPD by Tschoeke, Steinert, Flammer & Uhlmann9, who found a positive association between childhood trauma and suspiciousness, active social avoidance, and various specific characteristics of AVH in a group of 23 hospitalized patients with BPD.
Regarding the DSM-5 criterion which states that hallucinations in BPD are only experienced during times of stress2, we found only one empirical study to support that view, i.e. Glaser, van Os, Thewissen & Myin-Germeys16 reported that hallucinatory reactivity in response to self-reported daily life stresses was indeed significantly stronger in this group than in healthy controls and patients with a cluster C personality disorder.
To increase our knowledge on hallucinations in BPD, we studied patients from a specialized outpatient clinic for personality disorders while focusing on the following research questions:
What is the point prevalence of hallucinations in BPD in five sensory modalities, and what are their phenomenological characteristics?
Are hallucinations in BPD associated with other positive and negative symptoms of psychosis?
Are hallucinations in BPD associated with any comorbid psychiatric disorders?
Are childhood adversities and adult life stressors predictors of hallucinations in BPD?
Methods
Participants
From May 2012 through March 2015, all patients receiving treatment at the Outpatient Department for Personality Disorders at Parnassia Psychiatric Institute, The Hague, were approached by telephone for participation in this study. Inclusion criteria were 1) age ≥ 18 years; 2) a diagnosis of BPD, as established per May 1, 2012 in accordance with the operational criteria issued by the DSM-IV-TR17; 3) no comorbid DSM-IV diagnosis of schizophrenia or schizoaffective disorder, both ruled out on the basis of two clinical interviews by a trained psychologist and psychiatrist; and 4) sufficient mastery of Dutch or English. Patients were first approached by telephone, and then requested to be interviewed in person and fill out various self-report questionnaires.
Instruments and procedure
During the telephone interview, which was tailor-made for this specific purpose, data were collected on the presence, content, and frequency of hallucinations. Each sensory modality was addressed separately, i.e., by asking whether the patient ever heard, saw, tasted, smelled or felt something that other people did not perceive, or for which they had no explanation. They were also asked about the frequency of these hallucinations and about their phenomenological characteristics. During the face-to-face interviews that followed, we used the following semi-structured interviews. The AVH-related subscale of the Psychotic Symptom Rating Scale (PSYRATS)18 was used to assess the phenomenological characteristics and ensuing distress of AVH, and the Positive and Negative Syndrome Scale (PANSS) was used to measure the severity of psychotic symptoms19. In conformity with the van der Gaag Five-Factor Model20, the PANSS data were limited to positive, negative, and disorganized symptoms. Only items that loaded at least nine times out of ten on the same factor were used. To establish the number of comorbid psychiatric disorders, and to identify any disorders considered capable of mediating hallucinations (i.e., unipolar depression, bipolar disorder, alcohol and drug abuse, and PTSD)2,17,21, we used the MINI-International Neuropsychiatric Interview (MINI PLUS 2000)22. The presence of childhood adversities and life stressors was assessed with the aid of two self-report questionnaires, i.e., the Childhood Trauma Questionnaire Short-Form, (CTQ-SF)23 and the Life Stressor Checklist-Revised (LSC-R)24. The CTQ-SF is designed to retrospectively assess five subtypes of childhood maltreatment, i.e., emotional abuse, sexual abuse, physical abuse, emotional neglect, and physical neglect, whereas the LSC-R assesses the presence and number of life stressors, which may vary from serious financial problems to being robbed or physically attacked. Assessors who carried out the telephone and face-to-face interviews were psychologists and residents of psychology and psychiatry who had been trained in conducting these specific interviews, and who during the inclusion phase participated in monthly meetings to safeguard the interrater reliability.
The study was approved by the National Medical Ethical Committee (Stichting Medisch-Ethische Toetsingscommissie Instellingen Geestelijke Gezondheidszorg; METiGG). Written informed consent was obtained from all patients who participated in the face-to-face interviews and filled out the self-report questionnaires. The study was carried out in accordance with all relevant guidelines and regulations. The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Statistics
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 23.0 (Armonk, NY: IBM Corp). Participant characteristics were compared between telephone and face-to-face interviews through independent samples T test (age), Mann-Whitney U test (GAF) and Chi square test (sex). The point prevalence of hallucinations was calculated by dividing the number of patients who experienced hallucinations at least once per month by the total number of patients that participated in the telephone interviews. As four patients failed to complete the telephone interviews, the denominator for calculating the point prevalence of the separate sensory modalities was 323 for auditory, 322 for gustatory and tactile, 321 for olfactory, and 134 for multimodal hallucinations. Because of tied ranks in the ordinal variables, we chose Kendall’s tau for correlation analyses to investigate the association between the severity of hallucinations (PANSS item P3) and other positive, negative, and disorganized symptoms (other PANSS items), as well as the number of comorbid psychiatric disorders and the presence of childhood adversities and adult life stressors. The Benjamini-Hochberg correction, allowing for a false discovery rate of 5%, was used after conducting multiple comparisons in the Kendall’s tau analyses of hallucinations and other positive, negative, and disorganized symptoms. To exclude childhood adversities from the analysis of adult life stressors, life stressors that had occurred before the age of 18 years were omitted. The association between the presence of hallucinations and the number of comorbid psychiatric disorders was analyzed with the Mann-Whitney U test, and between the presence of hallucinations and specific comorbid psychiatric disorders with logistic regression with backward Wald selection. Comorbid psychiatric disorders were clustered into three groups, i.e., mood disorders (unipolar depression, bipolar I and II disorder), PTSD, and substance-use disorders (alcohol abuse and dependence, drug abuse and dependence, or both). A proportional odds model with backward selection was used to analyze the association between the severity of hallucinations and specific comorbid psychiatric disorders, and between hallucinations and the five subtypes of childhood adversities. The odds ratios and their 95% confidence intervals were generated by converting the differences in log odds into the odds ratios via the Output Management System (OMS) Control Panel. The presence of hallucinations was defined as a PANSS item P3 score of ≥ 4, and absence as a score of < 4.
Results
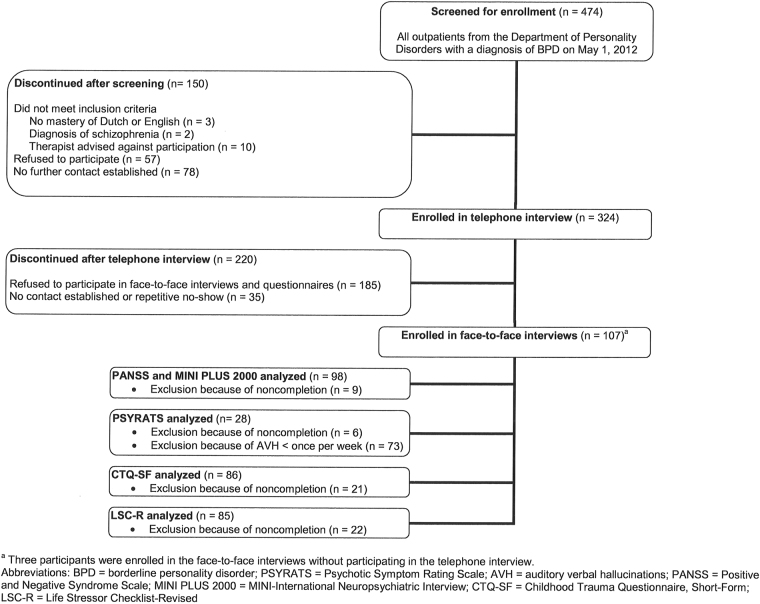
A total of 324 patients participated in the telephone interview. All of these patients were invited for subsequent face-to-face interviews, which were completed by 98 patients (Figure 1). Reasons for not completing were refusal to participate, failure on our side to establish further contact, and drop-out because of the duration of the interviews (which took 2–3 hours). Table 1 shows the participants’ demographic characteristics. There were no significant demographic and functioning differences between the patients who participated in the telephone interviews and the patients who participated in the face-to-face interviews.
Figure 1.
Flowchart participant disposition. The first panel shows all patients with a diagnosis of borderline personality disorder (BPD) from the Outpatient Department for Personality Disorders at Parnassia Psychiatric Institute who participated in the study. The next two panels show the patients that were excluded (discontinued) or included (enrolled) in the telephone interviews. Panels 4 and 5 display the patients who were excluded (discontinued) or included (enrolled) in the face-to-face interviews. Panels 6 through 10 show how many patients completed which questionnaires.
Table 1.
Participant characteristics.
| Characteristic | Telephone interviews | Face-to-face interviews |
|---|---|---|
| N | 324 | 107 |
| Age, mean (SD) | 37.4 (10.8) | 37.3 (11.1)a |
| Female sex, n (%) | 300 (92.6) | 100 (93.5)a |
| GAF, median (range) | 55 (40–80) | 55 (40–80)a |
Abbreviation: GAF = Global Assessment of Functioning.
aThere were no significant differences between the two groups.
Point prevalence of hallucinations and their phenomenological characteristics
Of the 324 patients who participated in the telephone interviews, 43% (n = 138) experienced hallucinations at least once per month, with a median frequency of at least once per week. Auditory hallucinations were reported by 87 patients (27%), including 69 (21%) who experienced AVH. In 50% of the cases (n = 67), the hallucinations were experienced in multiple sensory modalities. The PSYRATS interview was conducted among 28 of the patients who participated in the face-to-face interviews and experienced AVH at least once per week. Most of the AVH experienced by these patients had been present for long periods of time. Their content often involved verbal abuse directed at the patient, and they were mostly experienced as distressing in nature. Table 2 summarizes the prevalence rates of hallucinations as experienced in the five different sensory modalities that we studied. Table 3 presents the phenomenological characteristics of AVH and the distress caused by them.
Table 2.
Point prevalence of hallucinations.
| Hallucinations experienced at least once per month | na | % | Example |
|---|---|---|---|
| Auditory (AVH) | 87 (69) | 27 (21) | Voice that gives assignments |
| Visual | 37 | 11 | Person, wraith or shadow |
| Gustatory | 26 | 8 | Taste related to past events |
| Olfactory | 54 | 17 | Smell of gas |
| Tactile | 48 | 15 | Sense of someone touching |
aFour patients did not complete the telephone interview; the total sample consisted of 323 patients for auditory hallucinations, 322 for gustatory and tactile and 321 for olfactory hallucinations. Patients who experienced multimodal hallucinations were included in the calculation of the point prevalence of every sensory modality they experienced.
Abbreviation: AVH = auditory verbal hallucinations.
Table 3.
Phenomenological characteristics of hallucinations (PSYRATS).
| Characteristic of AVH | Item on PSYRATS | Scorea | Description of score |
|---|---|---|---|
| Period, mean (SD), years | Additional question | 15.3 (12.2) | |
| Number of different voices, median (range) | Additional question | 2 (1–20) | |
| Voices of known person, n (%) | Additional question | 17 (61%) | |
| Frequency, median (range) | 1 | 3 (1–4) | Voices occur at least once per hour |
| Duration, median (range) | 2 | 2 (1–4) | Voices last for several minutes |
| Location, median (range) | 3 | 2 (1–4) | Voice close to or inside head |
| Loudness, median (range) | 4 | 2 (1–4) | Same loudness as own voice |
| Explanation of origin, median (range) | 5 | 3 (1–4) | Conviction that voice originates from external cause is 50% |
| Emotional valence, median (range) | 6 | 3 (1–4) | Majority of content is unpleasant |
| 7 | 3 (1–4) | Personal verbal abuse related to self-concept | |
| Total distress, median (range) | 8 | 3 (1–4) | Majority of voices are distressing |
| 9 | 2.5 (1–4) | Voices are moderately to very distressing | |
| 10 | 2 (1–4) | Moderate amount of disruption of life | |
| Controllability, median (range) | 11 | 4 (1–4) | No control over voices |
aThe sample consisted of 28 BPD patients who experienced AVH at least once per week.
Abbreviations: PSYRATS = Psychotic Symptom Rating Scale; AVH = auditory verbal hallucinations.
Association with other positive symptoms, negative symptoms, and disorganization
Table 4 presents the median scores of the PANSS items, as collected during the face-to-face interviews, as well as the results of the correlation analyses. After correction for multiple comparisons, the only significant correlations were those between severity of hallucinations and delusions (tau-b = 0.371, p < 0.001), and between severity of hallucinations and unusual thought content (tau-b = 0.330, p < 0.001). Item scores for unusual thought content, however, did not reach the cut-off point of 4 (presence of symptoms), which makes this correlation less likely to be clinically relevant. After correction, correlations with negative symptoms and disorganization were both non-significant.
Table 4.
Association between hallucinations and other positive symptoms of psychosis, negative symptoms, and disorganization.
| Item score, median (%)a | tau_b | p-value | |||
|---|---|---|---|---|---|
| Hall −b (n = 71) | Hall+c (n = 27) | ||||
| PANSS-POSITIVE | P1 Delusions | 1 (8.5) | 3 (44.4) | 0.371 | <0.001d |
| P3 Hallucinatory behavior | — | — | — | — | |
| P5 Grandiosity | 1 (1.4) | 1 (0) | 0.046 | 0.614 | |
| P6 Suspiciousness/persecution | 3 (21.1) | 3 (37.0) | 0.208 | 0.013 | |
| G9 Unusual thought content | 1 (0) | 2 (0) | 0.330 | <0.001d | |
| PANSS-NEGATIVE | N1 Blunted affect | 1 (4.2) | 1 (7.4) | 0.141 | 0.113 |
| N2 Emotional withdrawal | 1 (5.6) | 1 (7.4) | 0.097 | 0.267 | |
| N3 Poor rapport | 1 (1.4) | 1 (3.7) | 0.071 | 0.434 | |
| N4 Passive/apathetic social withdrawal | 2 (4.2) | 2 (11.1) | 0.228 | 0.008 | |
| N6 Lack of spontaneity and flow of conversation | 1 (2.8) | 1 (3.7) | −0.031 | 0.737 | |
| G7 Motor retardation | 1 (0) | 1 (3.7) | 0.064 | 0.475 | |
| G8 Uncooperativeness | 1 (0) | 1 (0) | 0.022 | 0.809 | |
| G16 Active social avoidance | 2 (8.5) | 3 (18.5) | 0.206 | 0.015 | |
| PANSS-DISORGANIZATION | P2 Conceptual disorganization | 1 (1.4) | 1 (7.4) | 0.206 | 0.022 |
| N5 Difficulty in abstract thinking | 1 (4.2) | 1 (0) | −0.027 | 0.757 | |
| N7 Stereotyped thinking | 1 (0) | 1 (0) | 0.153 | 0.092 | |
| G5 Mannerisms and posturing | 1 (2.8) | 1 (0) | 0.141 | 0.122 | |
| G10 Disorientation | 1 (0) | 1 (3.7) | 0.137 | 0.128 | |
| G11 Poor attention | 1 (4.2) | 2 (7.4) | 0.098 | 0.263 | |
| G12 Lack of judgement and insight | 1 (0) | 1 (7.4) | 0.095 | 0.287 | |
| G13 Disturbance of volition | 1 (1.4) | 1 (0) | −0.083 | 0.352 | |
aThe sample consisted of 98 patients with BPD who completed the PANSS interview.
bHallucinations absent, defined as PANSS item P3 score <4.
cHallucinations present, defined as PANSS item P3 score ≥4.
dStatistically significant after Benjamini-Hochberg correction.
Abbreviation: PANSS = Positive and Negative Syndrome Scale.
Association with comorbid psychiatric disorders
Patients with BPD who did experience hallucinations (median = 5) had received significantly more comorbid psychiatric diagnoses than those who did not (median = 2; U = 536.500; z = −3.379, p = 0.001). In addition, the severity of hallucinations in these patients was associated with the number of comorbid psychiatric disorders (tau-b = 0.374, p < 0.001). Sixty-three percent (n = 17) of patients with hallucinations met criteria for PTSD, against 28% (n = 20) of patients without hallucinations. The association between both the presence and severity of hallucinations and PTSD was significant (OR 5.051, CI 2.193–11.628, p < 0.001, OR 3.311, CI 1.237–8.863, p = 0.017), whereas the association between the presence and severity of hallucinations and mood and substance-use disorders was not.
Association with childhood adversities and adult life stressors
Positive and significant correlations were found between the severity of hallucinations and preceding childhood adversities (tau-b = 0.200, p = 0.014). The odds ratio for higher scores on emotional abuse (as compared to lower scores) to experience more severe hallucinations was 1.237 (CI 1.116–1.371, p < 0.001), whereas the reverse was found to be true for emotional neglect (OR = 0.867, CI 0.785–0.958, p < 0.001). The subtypes sexual abuse, physical abuse, and physical neglect were not significantly associated with the severity of hallucinations. Finally, a greater number of current life stressors correlated positively with more severe types of hallucination (tau-b = 0.275, p = 0.001).
Discussion
Our analysis of 324 outpatients diagnosed with BPD yields a point prevalence for hallucinations of 43%, with half of the hallucinations being multimodal in nature. In comparison with prevalence rates of hallucinations in the general population (3–6%)25,26 and in schizophrenia (75%)27, BPD thus seems to occupy some middle ground on this spectrum of nosology. However, regarding the phenomenological characteristics of their hallucinations, these patients seem to fall squarely in the severe end of the spectrum. In a review by Johns et al.28, the authors describe the difference between benign types of hallucination and pathological ones (neutral vs. negative content, high vs. low control, and low vs. high frequency). The hallucinations experienced by patients participating in the present study fall in the latter category. This is in line with an earlier study, reporting that the phenomenological characteristics of hallucinations in patients with BPD do not differ significantly from those in patients with schizophrenia6,8,9, and that the ensuing distress is often even higher6. In the present study, although hallucinations experienced by patients with BPD were often found to co-occur with delusional thinking, they did not tend to be accompanied by negative symptoms and disorganization. In clinical practice, this may help to distinguish between patients with BPD and those with schizophrenia2,29 .
As the number of comorbid psychiatric disorders was associated with the presence and severity of hallucinations, and PTSD was the only specific comorbid psychiatric disorder for which this association was established, we consider it unlikely that hallucinations in this patient group are caused by any particular comorbid psychiatric disorder, as has been suggested4,10–12, at least not in the majority of them. Even the presence of comorbid PTSD does not seem to provide a sufficient explanation for the presence of hallucinations in BPD, since 37% of the BPD patients who experienced hallucinations did not meet the diagnostic criteria for PTSD. If we are allowed to consider a greater number of comorbid disorders as an index of illness severity, then patients with BPD and hallucinations seem to belong to a subgroup with a more severe type of personality disorder. If this is correct, this would be in line with Glaser et al.16, who found a dose-response relation between the number of BPD symptoms and psychotic reactivity.
Another noteworthy finding from the present study is the correlation between prior childhood adversities and the present severity of hallucinations, especially when those adversities involve emotional abuse. Such a relation between childhood adversities and a future chance of developing psychotic symptoms has been reported15, but not specifically for patients with BPD. Our finding that the odds ratio for the severity of hallucinations is higher for emotional than for sexual and physical abuse is in line with others30,31, and underlines the importance of exploring this type of abuse in patients (whatever their diagnosis) who experience hallucinations. Interestingly, we found an inverse relationship between the severity of hallucinations and prior emotional neglect. Two studies on patients at ultra-high risk for psychosis found similar results, i.e., a positive association between prior emotional abuse and the chance of transition to psychosis in the first32 and the severity of positive psychotic symptoms in the second study33, plus a negative association between emotional neglect on the transition to psychosis32 and (albeit non-significant) the severity of positive psychotic symptoms33. Together, these findings suggest that a history of childhood emotional abuse increases the susceptibility for hallucinations (often with a content directly/indirectly related to the traumatic experience)21, whereas emotional neglect does not appear to have that effect. Although the underlying mechanisms remain to be elucidated, it is hypothesized that the susceptibility for psychosis might be lowered when children learn that (even without noteworthy emotional support) they are still able to acquit themselves32.
Regarding the role of stress in promoting hallucinations in BPD, our study highlights the need for a discussion that strikes more of a balance than the traditional ones. Glaser et al.16 found hallucinatory reactivity in patients with BPD in response to ‘daily hassles and minor stresses’, while our study indicates that the severity of hallucinations is associated with adult life stressors. However, it seems that this type of response to stress is not specific for BPD. Various studies report the pivotal role of psychosocial stresses on hallucinations and other psychotic symptoms in healthy individuals, in individuals with an at-risk mental state, and in patients diagnosed with a schizophrenia spectrum disorder34,35. We consider this an argument in favor of the ideas i) that hallucinations in the context of BPD do not differ significantly from those in other disorders, ii) that they may even share a common etiology, and iii) that investigation of these hallucinations may benefit from a transdiagnostic approach. A further argument for the transdiagnostic approach stems from our finding that in BPD, PTSD was the only comorbid psychiatric disorder associated with the presence and severity of hallucinations. In a comprehensive review, McCarthy et al.21 describe the various phenomenological similarities between AVH experienced in the context of schizophrenia and in PTSD, as well as a possible shared etiology involving traumatic experiences; the authors also propose a transdiagnostic approach to AVH. Given our finding that these phenomenological similarities also exist for AVH in patients with schizophrenia and with BPD6,8,9, and given the associations we found between hallucinations and childhood adversities and PTSD, we believe that the hypothesis of a common etiology for AVH in BPD, schizophrenia and PTSD warrants further study.
Limitations
An initial limitation of the present study is that, in our outpatient group, we established the point prevalence of hallucinations based on telephone interviews. As some of the participants seemed reluctant to discuss their symptoms freely during telephone conversations, this may have led to an underestimation of the actual prevalence figure. In the final analysis, of the 11 patients who stated during telephone interviews that they had never experienced hallucinations, all later admitted during the ‘live’ PANSS interview that they had. Conversely, 12 patients who stated over the telephone that they had experienced hallucinations, failed to meet the criteria for these phenomena during the PANSS interview. However, as these numbers are very similar, the point prevalence we established may still have been reasonably accurate. On the other hand, in patients with BPD, these discrepancies may indicate the instability of hallucinations over time, especially since some patients had face-to-face interviews several months or even up to two years after their telephone interview. Consequently, we may have to conclude that the point prevalence of hallucinations in this patient group is a priori subject to some change.
A second limitation is our use of questionnaires (e.g. the PSYRATS and the PANSS) which are validated for patients diagnosed with schizophrenia, but not for use in those with BPD. To our knowledge, however, no questionnaires validated specifically for use in patients with BPD are currently available.
A third limitation is the strikingly high percentage of female participants in our study (93%), which might limit the generalization of our findings to male patients with BPD. This despite that BPD is far more common in women than in men, i.e. on average 25% of BPD patients are male2,36. That said, in the present study, the female/male ratio was an accurate representation of the population under care at our Outpatient Department for Personality Disorders where, in 2012, women made up 92% of the population.
A final limitation is that we did not focus on dissociative symptoms and disorders. Dissociation is common in patients with BPD37, and a comprehensive review and meta-analysis by Pilton, Varese, Berry & Bucci38 suggests a strong relationship with AVH, as well as with other types of hallucination. Dissociation might be an important mediating factor between childhood adversities and hallucinations in patients (whatever their diagnosis) and healthy individuals. Therefore, for future studies, our advice is to take these symptoms and disorders into account when investigating the mechanisms underlying hallucinations in patients with BPD.
Further recommendations for research
Although the prevalence, phenomenological characteristics and comorbidity of hallucinations were adequately addressed with our cross-sectional approach, even more accurate data on causality, the role of childhood adversities, the role of life stressors, and the role of dissociation can be obtained by means of prospective studies. In doing so, the interactions and associations between BPD, PTSD and dissociation in patients who develop hallucinations are of particular importance.
Further research might also focus on delusions in patients with BPD, which constitute yet another group of underexposed symptoms. In addition, the inverse relationship between emotional neglect and hallucinations deserves further attention. Finally, studies on treatment for hallucinations in patients with BPD are needed, to examine whether these patients can benefit from the same interventions as used in patients with schizophrenia spectrum disorders, i.e., antipsychotics, cognitive-behavioral therapy, eye-movement desensitization and reprocessing, and transcranial magnetic stimulation39,40.
Acknowledgements
The authors thank Mathijs Deen, MSc (Parnassia Psychiatric Institute, The Hague) for his statistical assistance.
Author Contributions
M.N., C.S., and J.D.B. wrote the main manuscript text. M.N. prepared the figures and tables. M.N., C.S., J.D.B., I.F., H.W., I.S., and M.G. revised the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yee L, Korner AJ, McSwiggan S, Meares RA, Stevenson J. Persistent hallucinosis in borderline personality disorder. Compr Psychiatry. 2005;46:147–154. doi: 10.1016/j.comppsych.2004.07.032. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (American Psychiatric Association, 2013).
- 3.Chopra HD, Beatson JA. Psychotic symptoms in borderline personality disorder. Am J Psychiatry. 1986;143:1605–1607. doi: 10.1176/ajp.143.12.1605. [DOI] [PubMed] [Google Scholar]
- 4.Links PS, Steiner M, Mitton J. Characteristics of psychosis in borderline personality disorder. Psychopathology. 1989;22:188–93. doi: 10.1159/000284595. [DOI] [PubMed] [Google Scholar]
- 5.George A, Soloff PH. Schizotypal symptoms in patients with borderline personality disorders. Am J Psychiatry. 1986;143:212–215. doi: 10.1176/ajp.143.2.212. [DOI] [PubMed] [Google Scholar]
- 6.Kingdon DG, et al. Schizophrenia and borderline personality disorder: similarities and differences in the experience of auditory hallucinations, paranoia, and childhood trauma. J Nerv Ment Dis. 2010;198:399–403. doi: 10.1097/NMD.0b013e3181e08c27. [DOI] [PubMed] [Google Scholar]
- 7.Pearse LJ, Dibben C, Ziauddeen H, Denman C, McKenna PJ. A study of psychotic symptoms in borderline personality disorder. J Nerv Ment Dis. 2014;202:368–371. doi: 10.1097/NMD.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 8.Slotema CW, et al. Auditory verbal hallucinations in patients with borderline personality disorder are similar to those in schizophrenia. Psychol Med. 2012;42:1873–1878. doi: 10.1017/S0033291712000165. [DOI] [PubMed] [Google Scholar]
- 9.Tschoeke S, Steinert T, Flammer E, Uhlmann C. Similarities and differences in borderline personality disorder and schizophrenia with voice hearing. J Nerv Ment Dis. 2014;202:544–549. doi: 10.1097/NMD.0000000000000159. [DOI] [PubMed] [Google Scholar]
- 10.Schroeder K, Fisher HL, Schäfer I. Psychotic symptoms in patients with borderline personality disorder: Prevalence and clinical management. Curr Opin Psychiatry. 2013;26:113–119. doi: 10.1097/YCO.0b013e32835a2ae7. [DOI] [PubMed] [Google Scholar]
- 11.Nishizono-Maher A, et al. Psychotic symptoms in depression and borderline personality disorder. J Affect Disord. 1993;28:279–285. doi: 10.1016/0165-0327(93)90063-P. [DOI] [PubMed] [Google Scholar]
- 12.Pope HG, et al. An empirical study of psychosis in borderline personality disorder. Am J Psychiatry. 1985;142:1285–1290. doi: 10.1176/ajp.142.11.1285. [DOI] [PubMed] [Google Scholar]
- 13.Miller FT, Abrams T, Dulit R, Fyer M. Psychotic symptoms in patients with borderline personality disorder and concurrent axis I disorder. Hosp Community Psychiatry. 1993;44:59–61. doi: 10.1176/ps.44.1.59. [DOI] [PubMed] [Google Scholar]
- 14.Benvenuti A, et al. Psychotic features in borderline patients: Is there a connection to mood dysregulation? Bipolar Disord. 2005;7:338–343. doi: 10.1111/j.1399-5618.2005.00217.x. [DOI] [PubMed] [Google Scholar]
- 15.Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: A meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glaser JP, van Os J, Thewissen V, Myin-Germeys I. Psychotic reactivity in borderline personality disorder. Acta Psychiatr Scand. 2010;121:125–134. doi: 10.1111/j.1600-0447.2009.01427.x. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision. (American Psychiatric Association, 2000).
- 18.Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS) Psychol Med. 1999;29:879–89. doi: 10.1017/S0033291799008661. [DOI] [PubMed] [Google Scholar]
- 19.Kay SR, Fiszbein A, Opler LA. The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 20.Van der Gaag M, et al. The five-factor model of the positive and negative syndrome scale II: A ten-fold cross-validation of a revised model. Schizophr Res. 2006;85:280–287. doi: 10.1016/j.schres.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 21.McCarthy-Jones S, Longden E. Auditory verbal hallucinations in schizophrenia and post-traumatic stress disorder: Common phenomenology, common cause, common interventions? Front Psychol. 2015;28:1071. doi: 10.3389/fpsyg.2015.01071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheehan DV, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 23.Bernstein DP, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–190. doi: 10.1016/S0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 24.Ungerer O, Deter HC, Fikentscher E, Konzag TA. Improved diagnostics of trauma-related disease through the application of the Life-Stressor Checklist. Psychother Psychosom Med Psychol. 2010;60:434–441. doi: 10.1055/s-0030-1247497. [DOI] [PubMed] [Google Scholar]
- 25.Van O J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: A psychosis continuum in the general population? Schizophr Res. 2000;45:11–20. doi: 10.1016/S0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- 26.Nuevo R, et al. The continuum of psychotic symptoms in the general population: A cross-national study. Schizophr Bull. 2012;38:475–485. doi: 10.1093/schbul/sbq099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bauer SM, et al. Culture and the prevalence of hallucinations in Schizophrenia. Compr Psychiatry. 2011;52:319–25. doi: 10.1016/j.comppsych.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 28.Johns LC, et al. Auditory verbal hallucinations in persons with and without a need for care. Schizophr Bull. 2014;40:S255–S264. doi: 10.1093/schbul/sbu005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bobes J, Arango C, Garcia-Garcia M, Rejas J, CLAMORS Study Collaborative Group Prevalence of negative symptoms in outpatients with schizophrenia spectrum disorders treated with antipsychotics in routine clinical practice: Findings from the CLAMORS study. J Clin Psychiatry. 2010;7:280–286. doi: 10.4088/JCP.08m04250yel. [DOI] [PubMed] [Google Scholar]
- 30.Daalman K, et al. Childhood trauma and auditory verbal hallucinations. Psychol Med. 2012;42:2475–84. doi: 10.1017/S0033291712000761. [DOI] [PubMed] [Google Scholar]
- 31.Whitfield CL, Dube SR, Felitti VJ, Anda RF. Adverse childhood experiences and hallucinations. Child Abuse Negl. 2005;29:797–810. doi: 10.1016/j.chiabu.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 32.Kraan, T. et al. Child maltreatment and clinical outcome in individuals at ultra-high risk for psychosis in the EU-GEI high risk study. Schizophr Bull. Accepted for publication (2017). [DOI] [PMC free article] [PubMed]
- 33.Ramsay CE, Flanagan P, Gantt S, Broussard B, Compton MT. Clinical correlates of maltreatment and traumatic experiences in childhood and adolescence among predominantly African American, socially disadvantaged, hospitalized, first-episode psychosis patients. Psychiatry Research. 2011;188:343–9. doi: 10.1016/j.psychres.2011.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reininghaus U, et al. Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: An experience sampling study. Schizophr Bull. 2016;42:712–722. doi: 10.1093/schbul/sbv190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rutten BP, Mill J. Epigenetic mediation of environmental influences in major psychotic disorders. Schizophr Bull. 2009;35:1045–1056. doi: 10.1093/schbul/sbp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gunderson, J. G. & Links, P. Borderline Personality Disorder: A Clinical Guide. (American Psychiatric Press, Inc. 2008).
- 37.Zanarini MC, Frankenburg FR, Jager-Hyman S, Reich DB, Fitzmaurice G. The course of dissociation for patients with borderline personality disorder and axis II comparison subjects: a 10-year follow-up study. Acta Psychiatr Scand. 2008;118:291–6. doi: 10.1111/j.1600-0447.2008.01247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pilton M, Varese F, Berry K, Bucci S. The relationship between dissociation and voices: A systematic literature review and meta-analysis. Clin Psychol Rev. 2015;40:138–55. doi: 10.1016/j.cpr.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 39.Van den Berg DP, et al. Trauma-focused treatment in PTSD patients with psychosis: Symptom exacerbation, adverse events, and revictimization. Schizophr Bull. 2016;42:693–702. doi: 10.1093/schbul/sbv172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sommer IEC, et al. The treatment of hallucinations in schizophrenia. Schizophr Bull. 2012;38:704–714. doi: 10.1093/schbul/sbs034. [DOI] [PMC free article] [PubMed] [Google Scholar]