Abstract
Intensive care medicine is a relatively new specialty, which was created in the 1950’s, after invent of mechanical ventilation, which allowed caring for critically ill patients who otherwise would have died. First created for treating mechanically ventilated patients, ICUs extended their scope and care to all patients with life threatening conditions. Over the years, intensive care medicine developed further and became a truly multidisciplinary speciality, encompassing patients from various fields of medicine and involving specialists from a range of base specialties, with additional (subspecialty) training in intensive care medicine. In Bosnia and Herzegovina, the founding of the society of intensive care medicine in 2006, the introduction of non invasive ventilation in 2007, and opening of a multidisciplinary ICUs in Banja Luka and Sarajevo heralded a new age of intensive care medicine. The number of admissions, high severity scores and needs for mechanical ventilation during the first several months in the medical ICU in Banja Luka confirmed the need of these kinds of units in the country. In spite of still suboptimal personnel training, creation of ICUs in Bosnia and Herzegovina may serve as example for other developing countries in the region. However, in order to achieve modern ICU standards and follow European trends toward harmonisation of medicine, Bosnia and Herzegovina needs to take up this challenge by recognizing intensive care medicine as a distinctive specialty, by implementing a specific training program and by setting up multidisciplinary ICUs in acute care hospitals.
Keywords: intensive care, mechanical ventilation, critical care, non invasive ventilation, developing countries
INTRODUCTION
From the first attempts of resuscitation to modern and sophisticated intensive care medicine, many centuries have passed. However, the major development occurred from the 1950’s. Over the last 60 years, me-chanical ventilation and other life sustaining interventions dramatically improved, and intensive care units (ICUs) became able to treat patients presenting with more and more critically ill conditions. In this review, we would like to describe the parallel history of me-chanical ventilation and intensive care medicine, and to point out the current situation of intensive care medicine in Bosnia and Herzegovina, with special focus on the main requirements that are necessary in order to reach modern standards in intensive care medicine.
History of Mechanical Ventilation
The early ages
The first experiments of respiratory resuscitation have been reported in the middle of the 16th century, describing insufflations of air into the lungs through a pipe introduced into the trachea. Between the 16th and the 19th century, various attempts of mechanical insufflations were made, using a positive airway pressure. In the late 19th, the first ventilators were described, namely “tank respirators”: the patient was put into the ventilator and inspiration was provoked by a negative pressure applied in the ventilator. This system was subsequently developed as “iron lung”, which was commonly used in the first half of the 20th century. The emergence of mechanical ventilation in its modern sense began in Denmark in the 1950th, when an epidemics of poliomyelitis devastated northern Europe. In 1952, hundreds of patients were hospitalised in Copenhagen because of respiratory paralysis related to poliomyelitis and were put in iron lungs. Despite this treatment, almost all patients died. A young anaesthetist, named Dr Bjorn Ibsen, showed that the addition of an intermittent external positive airway pressure through tracheotomy would save lives, and described the first standardizes approach of treatment of respiratory failure, including tracheal intubation, tracheotomy, and artificial respiration by manual ventilation (1-3). During several months, hundreds of medical students, nurses and physiotherapists spent ours applying manual ventilation and provided the 24-hours coverage (1-3). That was the starting point of mechanical ventilation and modern intensive care medicine. Because of high requirements in human resources could not be easily filed, several types of machines were tried out during this period. The Engstrom respirator was then developed, widely used, and became the first respirator that could deliver a predetermined volume at a preset frequency. The efficiency of this respirator was subsequently confirmed in Stockholm Hospital in 1953, where 54 patients with poliomyelitis were ventilated with a 27% mortality rate (4). Meanwhile, major progress was made in understanding lung physiology and pathology. Several physiologists allowed a better understanding of respiration and gas exchanges. Measurements of PCO2, pH and oxygen saturation were developed (5). Similarly to Ibsen, Astrup gained great experience during the 1952’s epidemics in Denmark, and subsequently described the influence of artificial ventilation on modification of pH and PCO2. He even reported the risk of over-ventilation, which, 40 years later, became a major issue in mechanical ventilation. During the following two decades, improvements in laboratory measurements helped clinicians evaluate the effectiveness of ventilation and various physiological conditions such as circulatory collapse, renal function or fluid balance. In addition, new knowledge and modern equipment facilitated safer and more successful use of mechanical ventilation. From the 70’s, ventilators became more sophisticated, with new modes and the ability to continuously monitor various parameters such as pressures, volumes and flows that were actually delivered to the patients. Consequently, blood gas analysis, ventilator monitoring and other forms of physiologic monitoring were increasingly used to guide ventilator settings. Particularity of respiratory physiology of mechanically ventilated lungs was better understood thanks to both research works and daily use of monitoring system at the bedside. In 1967 the first description of Acute Respiratory Distress Syndrome (ARDS) was published (6), and simultaneously Positive End Expiratory Pressure (PEEP) was found to be an effective treatment for severe hypoxemia in ARDS (7). The number of patients successfully treated with mechanical ventilation dramatically increased, as did the number of beds dedicated to intensive care medicine.
Complications of mechanical ventilation
From the 80’s however, awareness of the complications of invasive mechanical ventilation led to interest in less aggressive, potentially less injurious ventilatory support, despite more and more higher acuity of critically ill patients. New ventilator modes were proposed, most of them aiming to improve synchronisation between patient and ventilator, or to increase patient’s participation in his ventilation, reducing aggressiveness of fully controlled ventilation. The most important deleterious effect of mechanical ventilation was described in 1988 by Didier Dreyfuss who showed that excessive volume insufflated could seriously damage the lung (8). This phenomenon was subsequently called Ventilator Induced Lung Injury (VILI) (9) and led a complete reappraisal of ventilation strategies by the end of the 90’s (10), in which the reduction of the tidal volume and the airway pressure was a priority. Clinicians soon recognized that short term acceptance of abnormal blood gas analysis (“permissive hypercapnia”) is tolerated by mechanically ventilated patients (10). However, despite improvement of respiratory care long term exposure to ventilarory support was shown to lead to various complications, such as ventilator associated pneumonia (VAP), poor nutrition, neu-romyopathy, tracheal complications, etc… VAP became a major issue in patients on prolonged invasive mechanical ventilation, occurring in 20 to 60% of all ventilated patients. VAP is responsible for increased costs and prolonged length of stay, and maybe mortality. Several attempts were made in order to reduce the frequency of VAP, including patient positioning (11), more accurate diagnostic strategies (12), rational use of antibiotics and better use of enteral feeding. Paradoxically, although the effectiveness of invasive mechanical ventilation as a life-saving therapy was largely proven, it became obvious that its duration should be reduced, or even avoided, if possible. In addition to VAP, complications of artificial airway included the need for prolonged sedation and prolonged immobility. Considerable efforts were made to reduce the duration of sedation and ventilation, using sedation protocols (13, 14) or strategies of daily interruption (14), and to improve weaning process. In the early 90’s, a new strategy, so called non invasive ventilation (NIV) was promoted as an alternative to invasive ventilation in certain conditions. The potential benefit of continuous positive airway pressure using a face mask in patients with acute respiratory failure was recognized decades earlier (15,16), but the interest of NIV was renewed in more recent years, with the combination of pressure support and positive end-expiratory pressure delivered via a face mask or nasal mask. En-dotracheal tube or tracheotomy was replaced by face mask, allowing mechanical ventilation without invasive airway device (18). Over the last 20 years, evidence has accumulated to support the use of NIV in exacerbations of chronic obstructive pulmonary disease, cardiogenic pulmonary edema, and acute respiratory failure in im-munocompromised patients (19, 20, 21, 22). For these patients, there is a demonstrated benefit in terms of intubation rate, incidence of hospital acquired infection, duration of stay in the ICU and the hospital, and finally mortality (20-23). As a result, the use of NIV dramatically increased over the years, and has become the first line of treatment in these indications (24).
History of Intensive Care Medicine
By the end of the 1940’s, anaesthesia began to develop as an entire specialty. The Danish school of anaesthesia was one of the most famous, for both education and organisation of care. In 1950, Copenhagen hospital stated that anaesthetists should care for the patients during the operation and postoperatively “maintaining a sufficient circulation of blood…and in/use salt and water to restore the fluid balance and secure the best possible oxygen delivery by an energetic support of the respiratory /unction’ (25). More importantly, the statement added that “these principles for supportive therapy should also be applied to patients with medical diseases and self-poisoning”(25). By 1952, newly created recovery rooms were exclusively dedicated to postoperative patients, but the 1952 poliomyelitis epidemic in Copenhagen led to high number of patients placed on artificial ventilation (1,2). Soon, it became obvious that mechanically ventilated patients should be observed and treated in special wards by physicians and nurses trained in restoring and/or maintaining the function of vital organs. Subsequently, this concept was extended to all critically ill patients (medical as well as surgical) by Dr Bjorn Ibsen who created the first ICU in 1953, which was dedicated to the treatment of respiratory and circulatory failure (26).
Definition and organization of ICUs
At the end of the 50’s, most of European and North American countries had started to implement ICUs. During the following decades, the importance of ICUs was recognized worldwide, and the number of ICU beds increased, but with important discrepancies between countries. At the end of the 90’s, the number of ICUs in Europe was estimated between 3000 and 4000. The a number of ICU beds is ranging from 3,3/100 000 (UK) to 20-25/100 000 population (USA, Germany, Belgium), and from 1,2% (UK) to 9% of all hospital beds (USA) (27). Not surprisingly, the volume of admission varies between countries (10-fold difference from least to greatest), as does the severity of patients, measured by physiological scores such as APACHE, SAPS, and mortality rate, which are higher in countries with low number of ICU beds (27).
During the first decades, each country has developed its own approach, regarding to organization of ICUs. Even definition of an ICU appeared to be different between countries. However, there is a now consensus among health care professionals to consider that ICUs are unit designed to provide care for patients presenting or susceptible to present with acute organ failures, directly threatening life and necessitating auxiliary support, mainly mechanical ventilation. Finally, the current definition emphasizes the overlap between intensive care medicine and mechanical ventilation from which it was born. Given the predominant involvement of anaesthesiologists in the early age of intensive care medicine, most of patients admitted to the ICUs were surgical patients. Other specialists however, such as pneumologists, cardiologists, neurologists…, recognized the need of critically care for their patients, and got involved in the ICUs. Consequently, the development of ICUs in hospitals has not followed a single pathway. In some countries, each specialty developed its own ICU, called “specialty ICUs”, while in others a distinction between surgical and medical ICUs was apparent, the later admitting all non surgical patients. Some other countries, such as Spain and Australia, chose immediately to disconnect ICUs from any other specialty, and implemented multidisciplinary and independent ICUs. At the end of the 90’s, a consensus emerged that the problems presented by medical and surgical patients were similar, so that separate units should merge and mixed medical-surgical departments became the standard (29). European countries are now willing to harmonize the organization of ICUs, recognize intensive care medicine as a specialty, and help intensivists to set up common standards.
Education
When intensive care medicine began to develop it appeared that the management of such complex and multidisciplinary patients was no longer possible by doctors who did not have a specific knowledge. Nevertheless, education in intensive care developed heterogeneously from one country to another, leading to high diversity in access, structures, assessment, accreditation, and regulation of trainings between countries (30). Four main models can be described:
The single subspecialty model, in which access to intensive care medicine is limited to trainees from anaesthesiology.
The multiple specialty model: multiple base specialities each offer a programme of intensive care medicine training to their own trainees. Nationally, the content, duration and standards often vary between each base speciality.
The primary speciality model, in which intensive care medicine is an independent primary speciality which can be accessed directly after undergraduate medical training.
The supraspecialty or subspecialty model (such as proposed in Bosnia and Herzegovina), which permits multidisciplinary access from a range of base specialities (for example, internal medicine, anaesthesia, neurology…) to a common intensive care medicine training programme.
Over the time, it became obvious that an extra expertise (intensive care medicine) outside the domain of the primary speciality was required to provide high quality patient care by multidisciplinary input from doctors from various medical specialities. As a result, the supraspecialty model, based on multidisciplinarity, is being adopted by more and more countries. Moreover, there is currently a strong will of many countries in Europe to harmonize their training programme in order to provide similar level of education to intensivists. As part of this process, the European Society of Intensive Care Medicine is supporting a training programme called (CoBaTrICE) which aim is to develop an internationally acceptable competency-based training programme in intensive care for Europe and other world regions, by using consensus techniques to develop minimum core competencies for specialists in intensive care medicine” (31).
Current Development of Intensive Care Medicine in Bosnia and Herzegovina
First use of non invasive ventilation
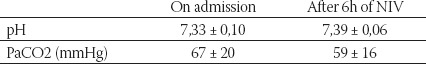
Until recently in Bosnia and Herzegovina, ICUs were almost exclusively surgical ICUs and only anaesthesiologists were involved in the care of critically ill patients. Although many non surgical clinics have their own semi-ICU, all patients requiring mechanical ventilation or presenting life threatening organ failures had to be transferred to the surgical ICU. Moreover, intensive care medicine was not defined as a specialty, but rather as part of anaesthesiology. As a result, access to intensive care medicine was not possible for non-anaesthesiologist trainees. Intensive care is however necessary in many non surgical situations, such as respiratory diseases, infectious diseases, neurological diseases, etc. In these cases, when patients suffered from acute respiratory failure, providing appropriate care was uncertain because of inadequate access to invasive mechanical ventilation. The use of non invasive ventilation (NIV) in this setting was thus proposed, based on published recommendations that support its use in patients with chronic obstructive pulmonary disease (COPD) and patients with pulmonary edema (21, 22). The first aim was to use modern standards of care in these patients. The second aim was to supply the lack of invasive mechanical ventilation in some situations. Based on this, a multidisciplinary Society of Intensive Care Medicine was founded in November of 2006 (Udruzenje za Intenzivnu Medicinu Bosne i Hercegovine, UIMBIH). Only six months later, the Clinical Centre Banja Luka implemented NIV to nonsurgical critically ill patients. From 1st June 2007 to 1st March 2008, 36 patients with acute respiratory failure where placed on NIV (table 1 and 2). All patients underwent NIV in the semi-ICU pulmonary ward. All patients were ventilated in pressure support mode with face masks. In case of failure of NIV, patients were to be transferred to the surgical ICU and placed on invasive mechanical ventilation. In some cases however, transfer to the surgical ICU was denied, and this often resulted in the patient’s death. The main reasons for refusals were the lack of available beds and the general reluctance of anaesthesiologists to admit non surgical critically ill patients. The overall ICU-survival rate was 72%.
TABLE 1.
Characteristics and outcome of patients receiving non invasive ventilation
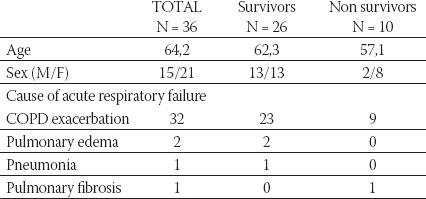
TABLE 2.
Blood Gas Analysis of the first 30 patients placed under non invasive ventilation
Implementation of multidisciplinary ICUs
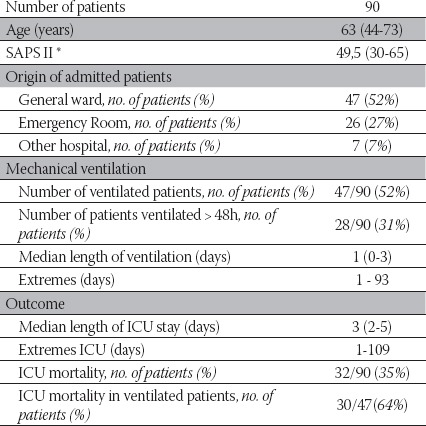
Based on initial experience, the Clinical Centre in Banja Luka decided to set up a multidisciplinary ICU. In the same time, the Clinical Centre of University in Sarajevo started a similar project. Both projects were led simultaneously, with a help of American and French ICU specialists. The main aim was to extend access to intensive care to all patients, both surgical and non surgical, and to implement modern standards of care for critically ill patients. The Clinical Centre Banja Luka opened the multidisci-plinary ICU on December 15th 2008. It consists of 6 beds equipped for caring for mechanically ventilated patients. The medical staff consists of one anaesthesiologist, one pneumologist, and one French intensivist who spends a week per month in this ICU. Three young doctors in training were added to the medical staff. Night shifts are shared by ICU staff and non-ICU anaesthesiologists. The nurse-to-patient ratio is 1:3. All nurses have at least at least 4 months of ICU experience, having worked previously in surgical ICU. Patients were admitted to the ICU if they presented with life threatening condition and/or with need for mechanical ventilation. The ICU functions as a closed-ICU; the decision to admit and all treatment decisions are done by intensivists. During the first 4 months, 90 patients were admitted, 52% of whom were ventilated. The overall ICU-survival rate was 65%, decreasing to 35% among ventilated patients (table 3).
TABLE 3.
Characteristics and outcomes of patients admitted in the ICU from December 15th to April 15th
*SAPS II: Simplified Acute Physiological Score (28)
Values are median with interquartile range shown in parentheses
The Challenges of Intensive Care Medicine in Bosnia and Herzegovina
Developing countries need to use the lessons from the 50-year history of intensive care medicine in western countries and to avoid the mistakes already made. Moreover, many European countries are now trying to harmonize their educational programs in intensive care medicine. Bosnia and Herzegovina, as a European country should therefore follow this process and move towards the same.
Lessons from 50-year history in developed countries
The first lesson is the position and state of ICU in acute care hospitals. Access to ICU must be given to all patients in need whether they come from surgical department, medical department or emergency room, provided they may benefit from admission to the ICU. The experience of Banja Luka’s new ICU, its activity and growth, highlights the strong need for such unit in this hospital. One can assume that same situation would apply to other acute care hospitals in the country. In other words, patients requiring ICU do exist everywhere. Artificial distinctions between surgical and medical ICUs or between ICUs connected with each different department or specialty are no longer relevant, but this organizational division remains to be present in many hospitals. In Western European countries, the majority of patients admitted to the ICU are non surgical patients, and 75% of the ICUs are defined as mixed medical-surgical ICUs (29). The problems presented by surgical and medical patients, or by patients from various fields of medical specialties are similar, so that they all fall under the competence of intensivists and should be treated in centralized multidisciplinary units. This concept has been shown to be more cost-effective than separate units, by concentrating human resources and expensive medical equipment in one place, instead of disseminating expenditure in various locations, which is simply unsustainable for economic reasons. This model seems discrepant with the current process of developing multidisciplinary medical ICU in Clinical Centres in Sarajevo and Banja Luka. However, considering local conditions, the first step of setting up medial ICUs is essential to move towards modern standards of care, and to facilitate access to ICUs for non-surgical patients. For that matter, the experience of implementing NIV for patients with acute respiratory failure has been an essential starting point. Just as intensive care medicine was born from mechanical ventilation, we can assume that development of NIV may play a major role in the extension of intensive care to various types of patients.
The second lesson refers to internal organization of ICUs. There have been lots of debates about the issue of open or closed policy ICUs. In many places ICUs operate with an open policy; physicians from different sub-specialties give orders after a patient is admitted to an ICU. On the contrary, most ICUs in Europe work with a closed policy; patients are screened for admission to the ICU by the intensivist, and the intensivist is solely responsible thereafter. Some investigators have reported that closed policy improves resources utilization and outcomes (32, 33). A prospective study has been conducted in Turkey, evaluating the effect of a closed policy on resources utilization and outcomes. Compared to open policy, the closed policy is associated with higher severity of illness among admitted patients, increased use of mechanical ventilation, and lower mortality (34). In addition, this study demonstrated that the appointment of a full time intensivist, with a 24h-coverage was associated with better quality of care (29). In 1992, 70% of all European ICUs had an intensivist present at night and during the weekend. Several authors reported better patient outcomes in units managed by a full time staff, and the 24h-coverage is now the rule. The challenge for Bosnia and Herzegovina is therefore to implement such closed units, managed by full time intensivists.
The third lesson refers to education issues. It is now recognized worldwide that intensive care medicine as a specialty requires it’s own training program. As previously stated, there are substantial variations in training programs in intensive care medicine across European Countries (30). Because of the European Union aim and objective for free movement of professionals and mutual recognition of qualifications, there is now a strong trend toward harmonization of curricula across European countries among health care professionals and especially intensivists (31). Therefore it is essential for Bosnia and Herzegovina, which is on the way to European integration, to timely move towards these harmonized standards of education. Moreover, this is also the best way to involve younger doctors in the specialty. The main parts of this process are:
The recognition of intensive care medicine as a specialty
The implementation of a training program based on subspecialty model, which permits multidisciplinary access from a range of base specialties to a common intensive care medicine training program.
A training program in which trainees have to conduct practical work in the ICU and to complete several pre established learning objectives.
This form of training program in intensive care medicine has been proposed in early 2009 to ministries of Health in both entities in Bosnia and Herzegovina, and is currently being considered.
The fourth lesson is the need that all specialists in this field of intensive care medicine organize themselves in an efficient and recognized scientific society. The duties of such a society are:
1) to promote knowledge exchange within Bosnia and Herzegovina and in connection with other countries,
2) to be responsible for education,
3) to set up research projects,
4) to be the official representative of intensive care medicine in cooperation with administrative authorities.
Udruženje za Intenzivnu Medicinu Bosne i Hercegovine (UIMBIH) was founded in 2006 in this aim. There is however an urgent need for this society to grow and to develop partnership with similar societies in other countries. The French Society of intensive care medicine (So-ciété de Réanimation de Langue Française, SRLF) and the American Society of Critical Care Medicine (SCCM) are already involved in Bosnia and Herzegovina. It is without doubt that the development of intensive care medicine in a country depends on such cooperation.
CONCLUSION
Born in the 1950’s, intensive care medicine is now a complex specialty that saves lives all over the world. Intensive care medicine can be defined as the active treatment and support of all life threatening conditions and mechanical ventilation and hemodynamic support remain it’s cornerstones. Because of the high diversity of patients requiring admission to the ICU, intensive care medicine is, above all, a multidisciplinary specialty. Various models exist in terms of organizations of ICUs and training programs. However, European countries are moving toward one common model. It is essential that Bosnia and Herzegovina timely takes part in this movement. With that in mind, we propose three major recommendations.
Bosnia and Herzegovina needs to set up multidisciplinary ICUs with closed policies, managed by full time intensivists, and which should admit both medical and surgical patients. Hospitals should avoid dispersion of human resources and medical equipment in numerous “semi-ICU” wards and should concentrate all these resources into multidisciplinary ICUs, which are more cost-effective and provide better outcomes.
Bosnia and Herzegovina needs to recognize intensive care medicine as a specialty, and to implement a specific training program based on subspecialty model, which permits multidisciplinary access.
Communication, share of knowledge and research must be encouraged, through an efficient scientific society, in order to benefit from major improvements in our specialty all over the world.
List of Abbreviations
MV -mechanical ventilation
NIV -non invasive ventilation
ICU -intensive care unit
ARDS -acute respiratory distress syndrome
COPD -Chronic obstructive pulmonary disease
VAP -Ventilator associated pneumonia
REFERENCES
- 1.Lassen A. A preliminary report on the 1952 epidemic of poliomyelitis in Copenhagen with special reference to the treatment of acute respiratory insufficiency. Lancet. 1953;1:37. doi: 10.1016/s0140-6736(53)92530-6. [DOI] [PubMed] [Google Scholar]
- 2.Ibsen B. The anaesthetist’s viewpoint on the treatment of respiratory complications in poliomyelitis during the epidemic in Copenhagen. Proc. Royal. Soc. Med. 1952-1954;47:72–74. doi: 10.1177/003591575404700120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andersen E.W, Ibsen B. The anaesthetic management of patients with poliomyelitis and respiratory paralysis. B.M.J. 1954;1:786–788. doi: 10.1136/bmj.1.4865.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ensgtrom C.G. Treatment of severe cases of respiratory paralysis by the Engstrom universal respitator. B.M.J. 1954;2:666–669. doi: 10.1136/bmj.2.4889.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Astrup P, Gotzche H, Neukirch F. Laboratory investigations during treatment of patients with poliomyelitis and respiratory paralysis. Br. Med. J. 1954;1:780–786. doi: 10.1136/bmj.1.4865.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ashbaugh D.G, Bigelow D.B, Petty T.L, Levine B.E. Acute respiratory distress in adults. Lancet. 1967;2(7511):319–323. doi: 10.1016/s0140-6736(67)90168-7. [DOI] [PubMed] [Google Scholar]
- 7.Ashbaugh D.G, Petty T.L, Bigelow D.B, Harris T.M. Continuous positive-pressure breathing (CPPB) in adult respiratory distress syndrome. J. Thorac. Cardiovasc. Surg. 1969;57(1):31–41. [PubMed] [Google Scholar]
- 8.Dreyfuss D, Soler P, Basset G, Saumon G. High inflation pressure pulmonary edema. Respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am. Rev. Respir. Dis. 1988;137(5):1159–1164. doi: 10.1164/ajrccm/137.5.1159. [DOI] [PubMed] [Google Scholar]
- 9.Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons from experimental studies. Am. J. Respir. Crit. Care. Med. 1998;157(1):294–323. doi: 10.1164/ajrccm.157.1.9604014. [DOI] [PubMed] [Google Scholar]
- 10.Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 11.Drakulolovic M.B, Torres A, Bauer T.T, et al. Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomised trial. Lancet. 1999;354:1851–1858. doi: 10.1016/S0140-6736(98)12251-1. [DOI] [PubMed] [Google Scholar]
- 12.Fagon J.Y, Chastre J, Wolff M, et al. Invasive and noninvasive strategies for management of suspected ventilator-associated pneumonia: a randomized trial. Ann. Intern. Med. 2000;132(8):621–630. doi: 10.7326/0003-4819-132-8-200004180-00004. [DOI] [PubMed] [Google Scholar]
- 13.Payen J.F, Bru O, Bosson J.L, et al. Assessing pain in critically ill sedated patientsby using a behavioral pain scale. Crit. Care. Med. 2001;29(12):2258–2263. doi: 10.1097/00003246-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Ely E.W, Truman B, Shintani A, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS) JAMA. 2003;289(22):2983–2991. doi: 10.1001/jama.289.22.2983. [DOI] [PubMed] [Google Scholar]
- 15.Kress J.P, Pohlman A.S, O’Connor M.F, Hall J.B. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N. Engl. J. Med. 2000;342(20):1471–1477. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]
- 16.Barach A.L, Martin J, Eckman M. Positive pressure respiration and its application to the treatment of acute pulmonary edema. Ann. Intern. Med. 1938;12:754–795. [Google Scholar]
- 17.Greenbaum D.M, Millen J.E, Eross B, et al. Continuous positive airway pressure without tracheal intubation in spontaneously breathing patients. Chest. 1976;69(5):615–620. doi: 10.1378/chest.69.5.615. [DOI] [PubMed] [Google Scholar]
- 18.Brochard L, Isabey D, Piquet J, et al. Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask. N. Engl. J. Med. 1990;323(22):1523–1530. doi: 10.1056/NEJM199011293232204. [DOI] [PubMed] [Google Scholar]
- 19.Brochard L, Mancebo J, Wysocki M, et al. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N. Engl. J. Med. 1995;333(13):817–822. doi: 10.1056/NEJM199509283331301. [DOI] [PubMed] [Google Scholar]
- 20.Hilbert G, Gruson D, Vargas F, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N. Engl. J. Med. 2001;344(7):481–487. doi: 10.1056/NEJM200102153440703. [DOI] [PubMed] [Google Scholar]
- 21.Vital F.M, Saconato H, Ladeira M.T, et al. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database Syst Rev. 2008;3:CD005351. doi: 10.1002/14651858.CD005351.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Ram F.S, Picot J, Lightowler J, Wedzicha J.A. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Co-chrane Database Syst. Rev. 2004;3:CD004104. doi: 10.1002/14651858.CD004104.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Girou E, Schortgen F, Delclaux C, Brun-Buisson C, Blot F, Lefort Y. Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. JAMA. 2000;284(18):2361–2367. doi: 10.1001/jama.284.18.2361. [DOI] [PubMed] [Google Scholar]
- 24.Demoule A, Girou E, Richard J.C, faille S, Brochard L. Increased use of noninvasive ventilation in French intensive care units. Intensive Care Med. 2006;32(11):1747–1755. doi: 10.1007/s00134-006-0229-z. [DOI] [PubMed] [Google Scholar]
- 25.Berthelsen P.G, Cronqvist M. The first intensive care unit in the world: Copenhagen 1953. Acta. Anaesthesiol. Scand. 2003;47(10):1190–1195. doi: 10.1046/j.1399-6576.2003.00256.x. [DOI] [PubMed] [Google Scholar]
- 26.Ibsen B, Kvittingen T.D. Arbejdet pa°en an^sthesiologisk observation safdeling. Nordisk. Med. 1958;38:1349–1355. [PubMed] [Google Scholar]
- 27.Wunsch H, Angus D.C, Harrison D.A, et al. Variation in critical care services across North America and Western Europe. Crit. Care Med. 2008;36(10):2787–2793. doi: 10.1097/CCM.0b013e318186aec8. [DOI] [PubMed] [Google Scholar]
- 28.Le Gall J.R, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270(24):2957–2963. doi: 10.1001/jama.270.24.2957. [DOI] [PubMed] [Google Scholar]
- 29.Vincent J.L, Suter P, Bihari D, Bruining H. Organization of intensive care units in Europe: lessons from the EPIC study. Intensive Care Med. 1997;23(11):1181–1184. doi: 10.1007/s001340050479. [DOI] [PubMed] [Google Scholar]
- 30.Barrett H, Bion J. F. An international survey of training in adult intensive care medicine. Intensive Care. Med. 2005;31(4):553–561. doi: 10.1007/s00134-005-2583-7. [DOI] [PubMed] [Google Scholar]
- 31.The CoBaTrICE Collaboration. Development of core competencies for an international training programme in intensive care medicine. Intensive Care Med. 2006;32(9):1371–1383. doi: 10.1007/s00134-006-0215-5. [DOI] [PubMed] [Google Scholar]
- 32.Carson S.S, Stocking C, Podsadecki T, et al. Effects of organizational change in the medical intensive care unit of a teaching hospital: A comparison of ‘open’ and ‘closed’ formats. JAMA. 1996;276(4):322–328. [PubMed] [Google Scholar]
- 33.Multz A.S, Chalfin D.B, Samson I.M, et al. A ‘closed’ medical intensive care unit (MICU) improves resource utilization when compared with an ‘open’ MICU. Am. J. Respir. Crit. Care Med. 1998;57(5 Pt 1):1468–1473. doi: 10.1164/ajrccm.157.5.9708039. [DOI] [PubMed] [Google Scholar]
- 34.Topeli A, Laghi F, Tobin M.J. Effect of closed unit policy and appointing an intensivist in a developing country. Crit. Care. Med. 2005;33(2):299–306. doi: 10.1097/01.ccm.0000153414.41232.90. [DOI] [PubMed] [Google Scholar]


