Abstract
Several studies have shown that anti-diabetic medications may modify the risk of cancer. We performed a systematic review and meta-analysis to evaluate the effect of alpha-glucosidase inhibitors (AGIs) on the risk of cancer in patients with diabetes mellitus. We conducted a systematic search of Medline, EMBASE, and Web of Science databases, up to September 30, 2016. Random-effects model was used to estimate the summary odds ratios (ORs) with 95% CI. Twenty-five studies (14 cohort, 7 case-control, and 4 randomized controlled trials) involving 1,285,433 patients with diabetes were included. Meta-analysis of observational studies showed that the use of AGIs was associated with a lower risk of developing cancer (OR = 0.86, 95% CI 0.78-0.96), especially gastrointestinal cancer (OR = 0.83, 95% CI 0.71-0.97). There was considerable heterogeneity across the studies introduced partly by the quality of included studies and adjustment for potential confounders. Meta-analysis of randomized controlled trials did not reveal any significant association between AGIs and cancer risk. Meta-analysis of observational studies indicated that AGIs may decrease the risk of cancer in individuals with diabetes.
Keywords: alpha-glucosidase inhibitor, diabetes mellitus, cancer risk, meta-analysis, systematic review
INTRODUCTION
Diabetes mellitus (DM) is a prevalent disease associated with considerable global health burden [1]. The number of patients with DM has significantly increased in the past few decades globally, especially in China [2, 3]. As DM is considered a risk factor for several types of cancer [4, 5], anti-diabetic medications (ADMs) have the potential to modify the risk of cancer [6, 7]. Metformin, an ADM, has been shown to exert antineoplastic effects through both insulin-dependent and insulin-independent mechanisms [8, 9]. However, data from various studies analyzing the anticancer effects of other types of ADMs, such as insulin, sulfonylureas, thiazolidinediones, alpha-glucosidase inhibitors (AGIs), dipeptidyl peptidase-4 inhibitors, glinides, glucagon-like peptide-1 (GLP-1) agonists, and sodium glucose cotransporter type 2 inhibitors, are not consistent [7, 10–14]. AGIs such as acarbose, voglibose, and miglitol are commonly used oral hypoglycemic agents in China and other eastern Asian countries. The association between AGI and risk of cancer has been inconsistently reported.
A meta-analysis of 13 studies (6 case-control studies, 2 cohort studies, and 5 randomized controlled trials [RCTs]) published in 2015 concluded that AGI was associated with a significantly higher risk (10%) of cancer [7]. The meta-analysis noted a significant risk in the case-control studies, but not in the cohort studies or RCTs, compared with risk in the control population [7]. However, the meta-analysis had several limitations such as a mixture of studies with observational studies and RCTs; a mixture of studies with different tumor types; small case numbers in most studies; and lack of differentiation between cases of type 1 and type 2 diabetes. Studies published after this meta-analysis also yielded inconsistent results. Most recently, a cohort study of DM patients in Taiwan showed that acarbose use reduced the risk of incident colorectal cancer in patients with diabetes in a dose-dependent manner [15], but a cohort study performed in Italy did not find any association between AGI use and cancer risk [16].
Our objective was to conduct a systematic review and meta-analysis of observational studies and RCTs to investigate the effect of AGI use on cancer risk in patients with DM.
RESULTS
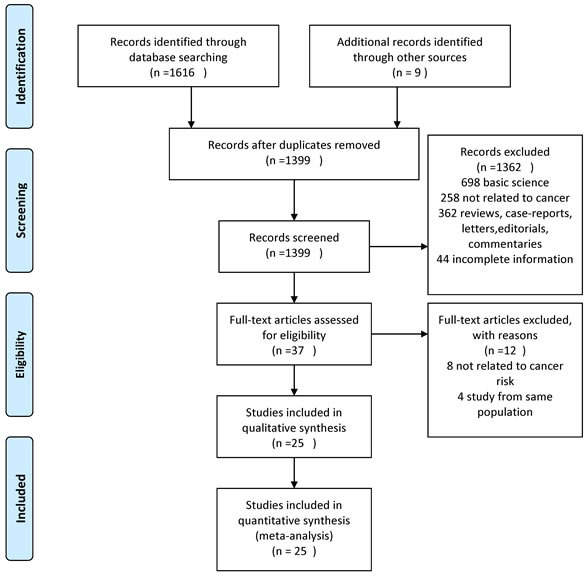
A total of 1399 unique studies were identified using the search strategy, of which 25 studies involving 1,285,433 patients with DM fulfilled the inclusion criteria and were pooled in the meta-analysis (14 cohort, 7 case-control, and 4 RCTs) [15–39].
Study characteristics
The study characteristics are shown in Table 1. The earliest study period began in 1989 and the latest period ended in 2015. Fifteen of these studies were population-based studies, and the remaining 10 were hospital-based studies. Nineteen studies were from Asia and 5 studies were from Europe. One RCT was multicenter trial and included mixed populations (from China, Romania, and Spain). A majority of the included studies (22 studies) demonstrated cancer risk in patients with type 2 DM, and the remainders did not report the subtype of DM. Two studies assessed the modification of cancer risk with duration and dose of exposure to AGI [15, 34].
Table 1. Characteristics of included studies assessing the risk of cancer in patients with DM on AGI.
| Study | Design | Location / setting | Time period; mean F/U (years) | Sample size (AGI/total) | Type of cancer | Type of DM | Mean duration of DM (years) | Mean age | Type of AGI | Exposure ascertainment | Outcome ascertainment | Potential confounders |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nakamura, T[17] | RCT | Japan; HB | NR; 1 | 15/45 | NR | 2 | 16.8 | 55.5 | voglibose | RCT | Adverse event review | NR |
| Pan, C[18] | RCT | China, Romania, Spain; HB | NR; 0.5 | 220/661 | NR | 2 | 1.3 | 51.9 | Acarbose | RCT | Adverse event review | NR |
| Kawaguchi, T[19] | C-C | Japan; HB | 2004.1-2008.12; NR | 40/241 | Liver | 2 | NR | 68.8 | NR | HDMS | Medical record review | NR |
| Yang, X[20] | Cohort | Hong Kong; HB | 1996.12.1-2005.1.9; 4.9 | 829/6103 | NR | 2 | 6 | 57 | Acarbose | Medical record review | ICD-9 | NR |
| Bosco, J. L[21] | C-C | Denmark; PB | 1989-2008; NR | 204/4323 | Breast | 2 | NR | NR | NR | Prescription databases | ICD-8 or ICD-10 | NR |
| Monami, M[22] | C-C | Italy; HB | 1998-2007, 6.3 | 8/482 | NR | 2 | 8.4 | 68.9 | Acarbose | Medical record review | ICD-9 | NR |
| Tseng, C. H.[23] | Cohort | Taiwan; PB | 2003.1-2005.12; 3 | NR/115731 | Bladder | 2 | NR | NR | Acarbose | NHI database | ICD-9 | 1, 2, 3, 7 |
| Tseng, C. H.[24] | Cohort | Taiwan; PB | 2003.1-2005.12; 3 | NR/52131 | Prostate | 2 | NR | NR | Acarbose | NHI database | ICD-9 | 1, 2, 3, 7 |
| Chang, C. H.[25] | C-C | Taiwan; PB | 2000.12.31-2007.12.31; 7.9 | 3207/40969 | Colon, Liver | 2 | New-onset | NR | NR | Pharmacy prescription database | ICD-9 | NR |
| Kawamori, R.[26] | RCT | Japan; HB | 2008-2010; 0.5 | 162/561 | NR | 2 | NR | 58.5 | voglibose | RCT | Adverse event review | NR |
| Lai, S. W.[28] | Cohort | Taiwan; PB | 2000-2008; 9 | 4638/19624 | Lung | 2 | New-onset | 56.4 | NR | NHI database | ICD-9 | 1, 2, 3 |
| Lai, S. W.[27] | Cohort | Taiwan; PB | 2000-2008; 9 | 4449/19349 | Liver | 2 | New-onset | 56.4 | NR | NHI database | ICD-9 | 1, 2, 3 |
| Liao, K. F.[29] | Cohort | Taiwan; PB | 1998–2007; NR | 12301/49803 | Pancreas | 2 | New-onset | 55.9 | NR | NHI database | ICD-9 | NR |
| Tseng, C. H.[30] | Cohort | Taiwan; PB | 1996-2005; NR | NR/115928 | Thyroid | 2 | NR | NR | NR | NHI database | ICD-9 | 1, 2, 3, 6, 7 |
| Chen, Y. L.[31] | Cohort | Taiwan; PB | 2000-2008; 5.5 | 4472/19625 | Gastric | NR | New-onset | 56 | Acarbose | NHI database | ICD-9 | 1, 2 |
| Chiu, C. C.[32] | Cohort | Taiwan; PB | 2000-2007; 7 | 2918/39515 | Colon, Esophagus, Gastric, Rectum, Pancreas, Liver | NR | New-onset | 58.52 | NR | NHI database | ICD-9 | 1, 2, 3 |
| Origasa H,[33] | C-C | Japan; HB | 2005-2011; NR | 26/95 | Bladder | 2 | NR | 69 | NR | Medical record review | Medical record review | 1, 6 |
| Simo, R.[34] | C-C | Spain; HB | 2008-2010; NR | 115/2438 | NR | 2 | 6.4 | 72.0 | NR | Pharmacy prescription database | ICD-10 | 1, 4, 5, 6, 8 |
| Chen, Y. C.[35] | Cohort | Taiwan; PB | 1998-2007; 2.5 | 150/7325 | NR | 2 | New-onset | 62.6 | Acarbose | NHI database | ICD-9 | 1, 2, 3, 7 |
| Lin, C. M[36] | Cohort | Taiwan; PB | 2005–2010; NR | NR /34823 | Lung, Liver, Colorectal, Breast, Oral cavity, Pancreas | 2 | New-onset | 54.26 | NR | NHI database | ICD-9 | 1, 2, 3, 6 |
| Son, J. W.[37] | RCT | Korea; HB | 2008.2-2009.1; 0.3 | 81/156 | Gastric | 2 | 12.2 | 56.1 | voglibose | RCT | Adverse event review | NR |
| Tseng, Y. H.[15] | Cohort | Taiwan; PB | 1998-2010; 3.4 | 199296/398592 | Colorectal | NR | New-onset | 54.1 | Acarbose | NHI database | ICD-9 | 1, 2, 3, 6, 7 |
| Valent, F.[16] | Cohort | Italy; PB | 2002-2014; NR | NR/109255 | Esophagus, Gastric, Colon, Rectum, Liver, Pancreas | 2 | NR | NR | NR | Pharmaceutical prescription database, | ICD-9 | 1, 2, 6 |
| Dabrowski, M.[38] | C-C | Poland; HB | 1998–2015; NR | 32/406 | NR | 2 | 10.7 | 67.1 | Acarbose | Medical record review | Medical record review | 3, 4, 6, 7, 8 |
| Tseng, C. H[39] | Cohort | Taiwan; PB | 1998-2009, NR | 47734/247252 | Kidney | 2 | New-onset | NR | Acarbose | NHI database | ICD-9 | NR |
RCT, randomized controlled trial; C-C, case-control; PB, population based; HB, hospital based; DM, diabetes mellitus; F/U, follow-up; ICD-8/9/10, International Classification of Diseases, Eighth/Ninth/Tenth Revision; NR, not reported; NHI, National Health Insurance in Taiwan; HDMS, HCV-related diabetes mellitus study in Japan.
Potential confounders: 1 - age; 2 - sex; 3 - comorbidities; 4 - smoking; 5 - alcohol; 6 - diabetes status, including DM duration, DM control, other ADM use; 7 - social status, including living region, occupation, and income; 8 - BMI.
Quality of included studies
The median Newcastle-Ottawa quality score for the observational studies was 7 (range 5-8). Table 2 depicts the methodological quality of all observational studies. The quality of the RCTs was moderate (Figure S1). The overall methodological quality of this body of evidence was moderate to high.
Table 2. Assessment of quality of included studies using Newcastle-Ottawa Scale.
| Cohort study | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Selection | Comparability | Outcome | ||||||||
| Study | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that the outcome of interest was not present at start of the study | Comparability of cohorts on the basis of design or analysis | Assessment of outcome | Was follow-up long enough for the outcome to occur? | Adequacy of follow up of cohorts | Total stars | Risk of bias |
| Yang, X[20] | * | * | * | * | * | * | * | - | 7 | Low |
| Tseng, C. H.[23] | * | * | * | * | ** | * | - | * | 8 | Low |
| Tseng, C. H.[24] | * | * | * | * | ** | * | - | * | 8 | Low |
| Lai, S. W.[28] | * | * | * | * | ** | * | * | - | 8 | Low |
| Lai, S. W.[27] | * | * | * | * | ** | * | * | - | 8 | Low |
| Liao, K. F.[29] | * | * | * | * | * | * | * | - | 7 | Low |
| Tseng, C. H.[30] | * | * | * | * | ** | * | - | - | 7 | Low |
| Chen, Y. L.[31] | * | * | * | * | ** | * | - | 8 | Low | |
| Chiu, C. C.[32] | * | * | * | * | ** | * | * | - | 8 | Low |
| Chen, Y. C.[35] | * | * | * | * | ** | * | - | * | 8 | Low |
| Lin, C. M[36] | * | * | * | * | ** | * | - | - | 7 | Low |
| Tseng, Y. H.[15] | * | * | * | * | ** | * | - | - | 7 | Low |
| Valent, F.[16] | * | * | * | * | * | * | - | - | 6 | Moderate |
| Tseng, C. H[39] | * | * | * | * | - | * | - | - | 5 | Moderate |
| Case-control study | ||||||||||
| Selection | Comparability | Exposure | ||||||||
| Study | Is the case definition adequate? | Representativeness of the cases | Selection of controls | Definition of controls | Comparability of cases and controls on the basis of design or analysis | Ascertainment of exposure | Same method of ascertainment for cases and controls | Non-response rate | Total stars | Risk of bias |
| Kawaguchi, T[19] | * | * | - | * | - | * | * | - | 5 | Moderate |
| Bosco, J. L[21] | * | * | * | * | * | * | * | - | 7 | Low |
| Monami, M[22] | * | * | - | * | * | * | * | - | 6 | Moderate |
| Chang, C. H.[25] | * | * | - | * | * | * | * | - | 6 | Moderate |
| Origasa H,[33] | * | - | - | * | * | * | * | - | 5 | Moderate |
| Simo, R.[34] | * | - | * | * | * | * | * | - | 6 | Moderate |
| Dabrowski, M.[38] | * | - | - | * | ** | * | * | - | 6 | Moderate |
AGI and the risk of any cancer
Of the 25 studies (21 observational and 4 RCTs) that reported on the association between AGI use and cancer risk, 4 demonstrated a decreased risk of cancer with AGI use [15, 28, 31, 36], 1 showed an increased risk [25], and 20 reported no significant relationship [16–24, 26, 27, 29, 30, 32–35, 37–39]. A meta-analysis of the observational studies demonstrated that AGI use (as compared with nonuse) was associated with a statistically significant 14% reduction in cancer incidence (n = 21 studies; odds ratio [OR] = 0.86, 95% CI 0.78-0.96) (Figure 2). There was considerable heterogeneity between studies (Cochran Q test P < 0.01; I2 = 82.4%). Of the study characteristics assessed in meta-regression, the quality of study and adjustment for potential confounders were statistically significant (P < 0.01) (Table 3). Meta-regression analysis did not show any significant effect size modification by other specific study characteristics considered, such as study design, setting, location, or duration of DM.
Figure 2. Summary of OR of observational studies assessing the risk of cancer with AGI use.
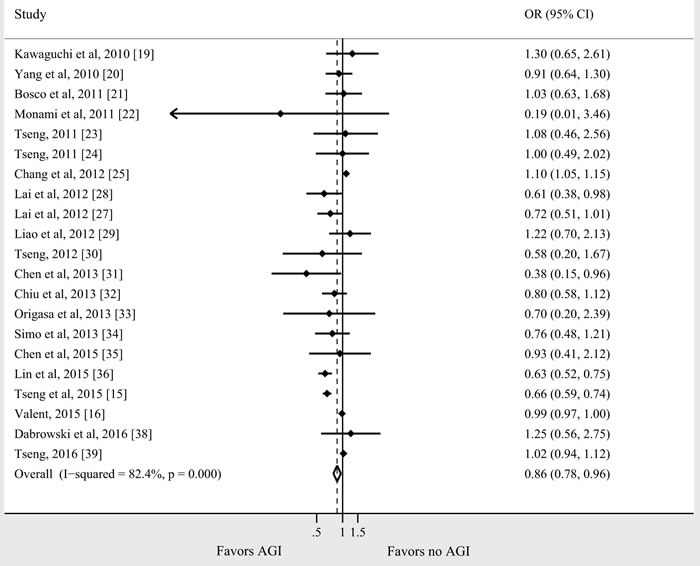
Table 3. Subgroup analysis.
| Subgroups | No. of studies | OR | 95 % CI | I2 | Meta-Regression P-Value |
|---|---|---|---|---|---|
| Study design | 0.116 | ||||
| Cohort | 14 | 0.81 | 0.70-0.94 | 84.6% | |
| C-C | 7 | 1.10 | 1.05-1.15 | 0% | |
| Study location | 0.409 | ||||
| Western | 5 | 0.99 | 0.97-1.00 | 0% | |
| Asian | 16 | 0.83 | 0.70-0.98 | 86.5% | |
| Study setting | 0.629 | ||||
| Hospital based | 6 | 0.91 | 0.72-1.16 | 0% | |
| Population based | 15 | 0.86 | 0.77-0.95 | 87.3% | |
| Quality of study | 0.000 | ||||
| Low risk of bias | 13 | 0.73 | 0.65-0.83 | 25.3% | |
| Moderate risk of bias | 8 | 1.03 | 0.95-1.11 | 70.0% | |
| Multivariate adjusted analysis | 0.007 | ||||
| Yes | 14 | 0.76 | 0.63-0.92 | 84.5% | |
| No | 7 | 1.08 | 1.04-1.13 | 0% | |
| Duration of DM | 0.577 | ||||
| New-onset | 10 | 0.80 | 0.66-0.97 | 91.7% | |
| Less than 10 years | 3 | 0.84 | 0.63-1.11 | 0% | |
| Moe than 10 years | 1 | 1.25 | 0.56-2.75 | - |
In subgroup analyses, the proactive association was detected in cohort studies, population-based studies, studies adjusting for covariates, Asian population, new-onset diabetic patients, and studies with low risk of bias. The subgroup analyses suggested an increased risk in case-control studies and in studies not adjusted for potential confounders. Sufficient data were not available to analyze the impact of AGI dose and duration.
Meta-analysis of RCTs revealed no significant association of AGI with cancer risk (n = 4 studies; OR = 0.83, 95% CI 0.20-3.46, I2 = 0%) (Figure S2).
AGI and cancer risk for individual tumor types
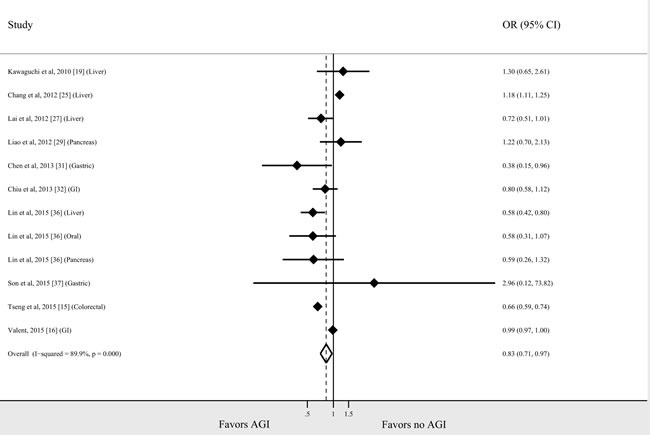
Seventeen studies (16 observational studies and 1 RCT) reported the risk of cancer for individual tumor types in AGI users compared with non-users. The relationship between AGI use and risk for each tumor type is shown in Figure 3. As there were 4 Taiwanese studies on colorectal cancer from the same cohort [15, 25, 32, 36], the study with the largest cohort size was included [15]. Two studies presented data on colon and rectum cancer separately, which were pooled to derive a summary estimate for the study [16, 32]. The association between AGI use and decreased risk of cancer was most prominent in patients with lung cancer (n = 2 studies; OR = 0.70, 95% CI 0.52-0.93, I2 = 0%). There was a slight trend toward lower risk of colorectal, liver, gastric, and breast cancer with AGI use (OR = 0.79, 95% CI 0.54-1.15, I2 = 96%; OR = 0.89, 95.5 % CI 0.75-1.05, I2 = 89.7%; OR = 0.69, 95% CI 0.36-1.31, I2 = 55.6%; OR = 0.74, 95% CI 0.37-1.51, I2 = 66.2%, respectively); however, these associations were not statistically significant. No significant associations were identified for pancreatic, esophageal, and urothelial cancer. A meta-analysis of studies of gastrointestinal cancer (Figure 4) showed a significant association between AGI use and reduced cancer risk (OR = 0.83, 95% CI 0.71-0.97, I2 = 89.9%).
Figure 3. AGI and the cancer risk for individual tumor types.
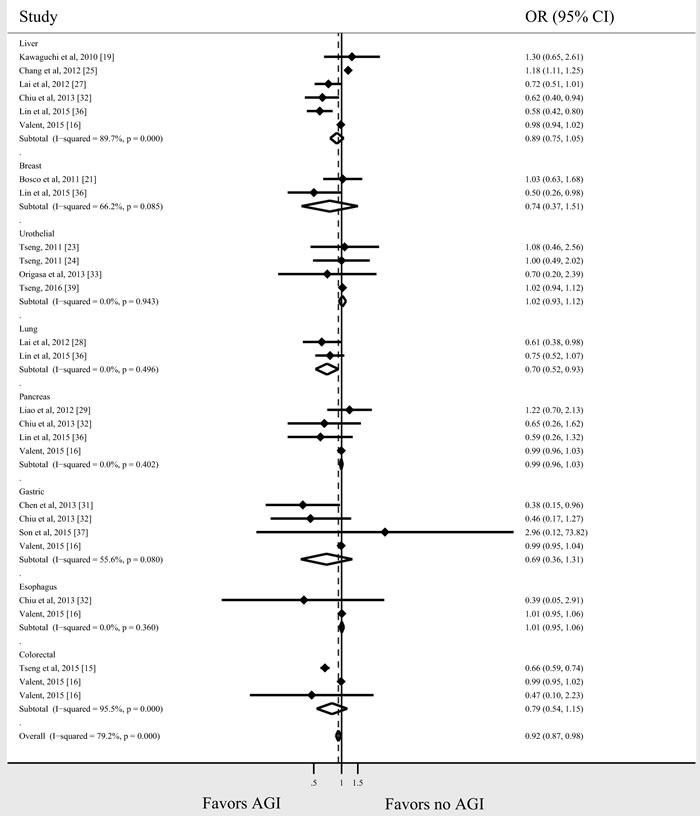
Figure 4. AGI and the risk for gastrointestinal cancer.
Publication bias
There was no evidence of significant publication bias, both quantitatively (P = 1.0 for Begg's test, P = 0.116 for Egger's test) and qualitatively, on visual inspection of the funnel plot (Figure S3).
DISCUSSION
This study showed an overall reducing effect of AGI on cancer risk, which was inconsistent with the previous meta-analysis [7]. The previous meta-analysis noted a significantly increased risk with AGI only in the case-control studies, but not in the cohort studies or RCTs [7]. In addition, the meta-analysis included only two cohort studies and omitted important recent studies on the influence of AGI on cancer risk. Furthermore, subgroup analyses were not performed. In subgroup analyses of our present analysis, the association between AGI and cancer risk was more prominent in population-based studies, studies with low risk of bias, and studies adjusted for covariates, indicating that more prospective, well-designed studies are warranted to confirm the results.
Various explanations have been provided for the association between diabetes and cancer. Metformin has been shown to possess anti-cancer property both in vivo and in vitro [9]. It has been proposed that metformin exerts its anti-cancer properties through direct effects on cancer cells, particularly through inhibition of the AMPK/mTOR pathway, and indirect effects by decreasing glucose, insulin, insulin-like growth factor 1 (IGF-1) levels, and other inflammatory factors [9].
Metformin is the only first-line oral ADM recommended by international guidelines for the treatment of type 2 diabetes [40]. AGI is another inexpensive and well-tolerated drug that has been widely used to treat DM for more than 20 years [41]. AGIs have shown better glucose-lowering effect in Asian populations than in Western populations [42], and acarbose has shown to exhibit an efficacy similar to that of metformin in China [43]. Yang et al showed that acarbose diminished insulin and glucagon concentrations while increasing GLP-1 concentration in Chinese type 2 diabetic patients [43]. A previous study also revealed that acarbose treatment reduced postprandial hyperinsulinemia [44].
Besides hypoglycemic effect, acarbose has been shown to possess anti-inflammatory and immunomodulatory effects in animal and human studies involving both Western and Asian type 2 DM patients [45–47]. Three mechanisms can be implicated for these actions. First, acarbose may regulate gut hormones. Previous studies demonstrated that acarbose use increased GLP-1 in the serum [43, 48–51]. Second, acarbose may interact with gut microbiota. A recent study found that acarbose increased the content of gut Bifidobacterium longum in type 2 DM patients [47], which could help to reduce intestinal inflammation [52]. Third, the unabsorbed acarbose may have an effect on the intestinal immune system by suppressing pro-inflammatory cytokine expression in the gut [53].
Owing to the known effects of AGI on the gut, it can be hypothesized that AGI may modify the risk of gastrointestinal cancer. A study of transformed cells suggested that acarbose exerts antineoplastic effect by increasing butyrate production [54], which has protective effect against colonic cancer [55]. Previous studies suggested that fecal butyrate, which is a short-chain fatty acid, is a key colonocyte nutrient and an important survival factor for colonic epithelial cells [56]. Acarbose has been found to reduce the colonic transit time and thus change the fecal concentration of bile acids, which may have protective effect against colorectal cancer [57, 58]. In addition, acarbose use has been found to be associated with increased production of GLP-1 [43, 48–51]. Previous studies indicated GLP-1 as a potent inducer of cAMP and an inhibitor of breast cancer cell proliferation [59]. A study using CT26 tumor-bearing BALB/c mice showed that GLP-1 receptor agonist treatment increased tumor apoptosis [60]. In the APC gene knockout animal model, which develops multiple intestinal adenomas, acarbose had a regressive effect on the size of gastrointestinal adenomas but did not significantly decrease the number of colonic neoplasms [61]. Most recently, a cohort study of DM patients in Taiwan showed that acarbose use reduced the risk of incident colorectal cancer in patients with diabetes in a dose-dependent manner [15]. Our analysis showed an overall reducing effect of AGI on gastrointestinal cancer risk. However, only a slight trend toward lower risk was observed in colorectal cancer, liver cancer, and gastric cancer, which was not statistically significant. It is difficult to identify the effects of AGI on gastrointestinal cancer based on retrospective studies due to confounding by indication and reverse causality. More prospective observational studies, which account for these sources of heterogeneity, would be required to truly assess the impact of AGI on the risk of gastrointestinal cancer.
Our analysis showed that AGI use was associated with a slightly decreased risk in patients with lung cancer (n = 2 studies; OR, 0.86; 95% CI, 0.76-0.97). The associations observed between ADMs and lung cancer were not consistent [62–64]. The precise mechanism of the observed cancer risk reduction is not clear. The results of our analysis should be interpreted with caution as only two studies were included in the analysis.
The strengths of our study include the comprehensive and simultaneous assessment of the effects of AGI on the risk modification of cancer, and findings from multiple subgroup analyses to ensure stability of the association and identify factors responsible for heterogeneity.
There were also several limitations to our meta-analysis. First, the cancer-modifying association between AGI and cancer risk were based on data from observational studies, was apparent based on the RCT cases. In observational studies, random allocation of the intervention is not done, which is necessary to test the exposure-outcome hypothesis optimally. As a result, the chemopreventive effect of AGI seen in observational studies may be an overestimate of its true effect. However, we should acknowledge that the average follow-up time in observational studies is much longer than that in RCTs, which could explain why current clinical trials of AGI for the management of DM do not demonstrate a significant effect on cancer. Second, all studies were not adjusted for the same confounders. In addition, most patients with DM in these studies were on multiple ADMs simultaneously. As a result, as compared with patients on AGI, patients “not on AGI” (the comparator group) would be more likely to be on metformin. Therefore, it is difficult to interpret whether the risk modification inferred for any one agent is real or confounded by exposures to other ADMs. In the only monotherapy, population-based observational study conducted by Chen et al to compare cancer incidence with metformin and other ADMs in patients with DM, AGI use was not found to be associated with risk of cancer [35]. The true clinical effect of AGI on cancer risk should ideally be studied by comparing patients on AGI therapy for DM with those managed by non-medical/dietary therapy over an extended period of time.
In conclusion, meta-analysis of existing studies suggests a protective association between AGI use and risk of cancer in patients with DM. As there was considerable heterogeneity across studies, future, well-designed, prospective studies are warranted to evaluate this association better.
MATERIALS AND METHODS
This systematic review was conducted following guidance provided by the Cochrane Handbook [65] and is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [66].
Data sources, searches, and study selection
First, a systematic literature search of MEDLINE (1966 through September 30, 2016), EMBASE (1988 through September 30, 2016), and Web of Science (1993 through September 30, 2016) databases was conducted by two study investigators for all relevant articles on the association between AGI use and risk of cancer in patients with DM. The following keywords and/or corresponding MeSH terms were used: (acarbose OR voglibose OR miglitol OR alpha glucosidase inhibitor OR alpha glucoside hydrolase inhibitor OR α glucosidase inhibitor OR α glycoside hydrolase inhibitor) AND (cancer OR tumor OR neoplasm). The title and abstract of studies identified in the search were reviewed by two authors independently to exclude studies that did not answer the research question of interest. The full text of the remaining articles was examined to determine whether it contained relevant information. Next, bibliographies of the selected articles, as well as review articles on the topic were manually searched for additional articles. Third, manual search of abstracts from major endocrinology and oncology conferences (2007-2016) was performed for additional abstracts on the topic. When information available was not complete, attempts were made to contact the corresponding authors of the studies for additional information.
Studies considered in this meta-analysis were either observational studies or RCTs that met the following inclusion criteria: (1) evaluated and clearly defined exposure to AGI, (2) reported cancer outcomes in patients with DM, and (3) reported relative risks or odds ratio (OR) or provided data for their estimation. Inclusion was not otherwise restricted by study size, language, or publication type. When there were multiple publications from the same population, only data from the most comprehensive report were included. The flow diagram summarizing study identification and selection is shown in Figure 1.
Figure 1. Study flow diagram in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations.
Data extraction and quality assessment
Data were independently abstracted onto a standardized form by two reviewers. The following data were collected from each study: study design, time period of study/year of publication, location/setting of the population studied, type of DM, duration of DM, age/sex of patients included, type of tumor, dose and duration of AGI use (if reported), information source of exposure ascertainment and outcome assessment, total number of persons, OR, and 95% CI with and without adjustment for confounding factors. When data on individual tumor types were reported separately, we pooled these to derive a summary estimate for the study. For all analysis, referent group was composed of patients with DM not exposed to AGI. Conflicts in data abstraction were resolved by consensus, referring back to the original article.
Quality assessment for observational studies was performed using the Newcastle Ottawa scale [67]. A score of 7-9 represents low risk of bias, 4-6 represents moderate risk of bias, and 0-3 represents high risk of bias. The quality of RCTs was assessed using a revised form of Cochrane Collaboration's tool for assessing risk of bias in randomized trials [68]. This tool focuses on the adequacy of randomization and allocation concealment procedures, blinding, and loss to follow-up. Any discrepancies were addressed by a joint reevaluation of the original article.
Data synthesis and analysis
The primary analysis focused on assessing the relationship between AGI and risk of cancer in patients with DM. A priori hypotheses to explain potential heterogeneity in the direction and magnitude of effect among different observational studies included type of cancer, location/setting of study (Western population vs. Asian population; population based vs. hospital based), study design (case-control vs. cohort), quality of study (low bias vs. moderate bias vs. high bias), and whether the study was adjusted for the potential confounding factors. Because of significant differences in the design of observational studies and RCTs, data from these RCTs were analyzed and presented separately.
We used the random-effects model described by DerSimonian and Laird to calculate meta-analytic OR and 95% CI [69]. Adjusted ORs reported in studies were used for analysis to account for confounding variables. We assessed heterogeneity between study-specific estimates with the Cochran Q statistic (P < 0.10) and I2 statistic [69, 70]. Once heterogeneity was noted, between-study sources of heterogeneity were investigated using subgroup and meta-regression analyses by study characteristics (as described above). All P values were two-tailed. For all tests (except for heterogeneity and publication bias), a P value of less than 0.05 was considered statistically significant. Subgroup analysis was conducted on all relevant study characteristics regardless of statistical significance. We investigated the presence and the effect of publication bias using a combination of the Begg's test [70] and Egger's test [71]. Statistical analyses were performed using Stata 12.1 (StataCorp). An overview of the study protocol is provided in S1 Protocol.
SUPPLEMENTARY FIGURES
Acknowledgments
We thank Dr. Pengfei Shan from Department of Endocrinology and Metabolism, Second Affiliated Hospital of Zhejiang University School of Medicine, China, for his constructive suggestions to improve the quality of this paper. We would also like to extend our gratitude to Prof. Giuseppe Derosa from Diabetes and Metabolic Diseases Unit, University of Pavia, Italy, who returned important information on request. This work was supported by Natural Science Foundation of Zhejiang Province.
Abbreviations
- ADM
anti-diabetic medication
- AGI
alpha-glucosidase inhibitor
- DM
diabetes mellitus
- GLP-1
glucagon-like peptide-1
- RCT
randomized controlled trial
Footnotes
Author contributions
Conception and design: Y.M.Z. and Y.J.W.; data collection, analysis, and interpretation of the data: Y.M.Z., H.Y.L., and L.Z.S.; drafting of the manuscript: Y.M.Z.; critical revision: Y.M.Z. and Y.J.W. All authors read and approved the final version of the manuscript.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
FUNDING
This work was supported by Natural Science Foundation of Zhejiang Province (grants LY14H160023).
REFERENCES
- 1.Vinicor F. The public health burden of diabetes and the reality of limits. Diabetes Care. 1998;21(Suppl 3):C15–C18. doi: 10.2337/diacare.21.3.c15. [DOI] [PubMed] [Google Scholar]
- 2.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, et al. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362:1090–1101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 4.Vigneri R. Diabetes: diabetes therapy and cancer risk. Nat Rev Endocrinol. 2009;5:651–652. doi: 10.1038/nrendo.2009.219. [DOI] [PubMed] [Google Scholar]
- 5.Nicolucci A. Epidemiological aspects of neoplasms in diabetes. Acta Diabetol. 2010;47:87–95. doi: 10.1007/s00592-010-0187-3. [DOI] [PubMed] [Google Scholar]
- 6.Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, Pollak M, Regensteiner JG, Yee D. Diabetes and cancer: a consensus report. CA Cancer J Clin. 2010;60:207–221. doi: 10.3322/caac.20078. [DOI] [PubMed] [Google Scholar]
- 7.Wu L, Zhu J, Prokop LJ, Murad MH. Pharmacologic therapy of diabetes and overall cancer risk and mortality: a meta-analysis of 265 studies. Sci Rep. 2015;5:10147. doi: 10.1038/srep10147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coyle C, Cafferty FH, Vale C, Langley RE. Metformin as an adjuvant treatment for cancer: a systematic review and meta-analysis. Ann Oncol. 2016;27:2184–2195. doi: 10.1093/annonc/mdw410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Daugan M, Dufay Wojcicki A, d’Hayer B, Boudy V. Metformin: an anti-diabetic drug to fight cancer. Pharmacol Res. 2016;113:675–685. doi: 10.1016/j.phrs.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 10.Nauck MA, Friedrich N. Do GLP-1-based therapies increase cancer risk? Diabetes Care. 2013;36(Suppl 2):S245–S252. doi: 10.2337/dcS13-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh S, Singh PP, Singh AG, Murad MH, McWilliams RR, Chari ST. Anti-diabetic medications and risk of pancreatic cancer in patients with diabetes mellitus: a systematic review and meta-analysis. Am J Gastroenterol. 2013;108:510–519. doi: 10.1038/ajg.2013.7. quiz 20. [DOI] [PubMed] [Google Scholar]
- 12.Lin HW, Tseng CH. A review on the relationship between SGLT2 inhibitors and cancer. Int J Endocrinol. 2014;2014:719578. doi: 10.1155/2014/719578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davidson MB. Pioglitazone (Actos) and bladder cancer: legal system triumphs over the evidence. J Diabetes Complications. 2016;30:981–985. doi: 10.1016/j.jdiacomp.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Tseng CH. Sitagliptin and pancreatic cancer risk in patients with type 2 diabetes. Eur J Clin Invest. 2016;46:70–79. doi: 10.1111/eci.12570. [DOI] [PubMed] [Google Scholar]
- 15.Tseng YH, Tsan YT, Chan WC, Sheu WH, Chen PC. Use of an alpha-glucosidase inhibitor and the risk of colorectal cancer in patients with diabetes: a nationwide, population-based cohort study. Diabetes Care. 2015;38:2068–2074. doi: 10.2337/dc15-0563. [DOI] [PubMed] [Google Scholar]
- 16.Valent F. Diabetes mellitus and cancer of the digestive organs: an Italian population-based cohort study. J Diabetes Complications. 2015;29:1056–1061. doi: 10.1016/j.jdiacomp.2015.07.017. [DOI] [PubMed] [Google Scholar]
- 17.Nakamura T, Matsuda T, Kawagoe Y, Ogawa H, Takahashi Y, Sekizuka K, Koide H. Effect of pioglitazone on carotid intima-media thickness and arterial stiffness in type 2 diabetic nephropathy patients. Metabolism. 2004;53:1382–1386. doi: 10.1016/j.metabol.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Pan C, Yang W, Barona JP, Wang Y, Niggli M, Mohideen P, Foley JE. Comparison of vildagliptin and acarbose monotherapy in patients with Type 2 diabetes: a 24-week, double-blind, randomized trial. Diabet Med. 2008;25:435–441. doi: 10.1111/j.1464-5491.2008.02391.x. [DOI] [PubMed] [Google Scholar]
- 19.Kawaguchi T, Taniguchi E, Morita Y, Shirachi M, Tateishi I, Nagata E, Sata M. Association of exogenous insulin or sulphonylurea treatment with an increased incidence of hepatoma in patients with hepatitis C virus infection. Liver Int. 2010;30:479–486. doi: 10.1111/j.1478-3231.2009.02191.x. [DOI] [PubMed] [Google Scholar]
- 20.Yang X, So WY, Ma RC, Yu LW, Ko GT, Kong AP, Ng VW, Luk AO, Ozaki R, Tong PC, Chow CC, Chan JC. Use of sulphonylurea and cancer in type 2 diabetes-The Hong Kong Diabetes Registry. Diabetes Res Clin Pract. 2010;90:343–351. doi: 10.1016/j.diabres.2010.08.022. [DOI] [PubMed] [Google Scholar]
- 21.Bosco JL, Antonsen S, Sorensen HT, Pedersen L, Lash TL. Metformin and incident breast cancer among diabetic women: a population-based case-control study in Denmark. Cancer Epidemiol Biomarkers Prev. 2011;20:101–111. doi: 10.1158/1055-9965.EPI-10-0817. [DOI] [PubMed] [Google Scholar]
- 22.Monami M, Colombi C, Balzi D, Dicembrini I, Giannini S, Melani C, Vitale V, Romano D, Barchielli A, Marchionni N, Rotella CM, Mannucci E. Metformin and cancer occurrence in insulin-treated type 2 diabetic patients. Diabetes Care. 2011;34:129–131. doi: 10.2337/dc10-1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tseng CH. Diabetes and risk of bladder cancer: a study using the National Health Insurance database in Taiwan. Diabetologia. 2011;54:2009–2015. doi: 10.1007/s00125-011-2171-z. [DOI] [PubMed] [Google Scholar]
- 24.Tseng CH. Diabetes and risk of prostate cancer: a study using the National Health Insurance. Diabetes Care. 2011;34:616–621. doi: 10.2337/dc10-1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chang CH, Lin JW, Wu LC, Lai MS, Chuang LM, Chan KA. Association of thiazolidinediones with liver cancer and colorectal cancer in type 2 diabetes mellitus. Hepatology. 2012;55:1462–1472. doi: 10.1002/hep.25509. [DOI] [PubMed] [Google Scholar]
- 26.Kawamori R, Inagaki N, Araki E, Watada H, Hayashi N, Horie Y, Sarashina A, Gong Y, von Eynatten M, Woerle HJ, Dugi KA. Linagliptin monotherapy provides superior glycaemic control versus placebo or voglibose with comparable safety in Japanese patients with type 2 diabetes: a randomized, placebo and active comparator-controlled, double-blind study. Diabetes Obes Metab. 2012;14:348–357. doi: 10.1111/j.1463-1326.2011.01545.x. [DOI] [PubMed] [Google Scholar]
- 27.Lai SW, Chen PC, Liao KF, Muo CH, Lin CC, Sung FC. Risk of hepatocellular carcinoma in diabetic patients and risk reduction associated with anti-diabetic therapy: a population-based cohort study. Am J Gastroenterol. 2012;107:46–452. doi: 10.1038/ajg.2011.384. [DOI] [PubMed] [Google Scholar]
- 28.Lai SW, Liao KF, Chen PC, Tsai PY, Hsieh DP, Chen CC. Antidiabetes drugs correlate with decreased risk of lung cancer: a population-based observation in Taiwan. Clin Lung Cancer. 2012;13:143–48. doi: 10.1016/j.cllc.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 29.Liao KF, Lai SW, Li CI, Chen WC. Diabetes mellitus correlates with increased risk of pancreatic cancer: a population-based cohort study in Taiwan. J Gastroenterol Hepatol. 2012;27:709–713. doi: 10.1111/j.1440-1746.2011.06938.x. [DOI] [PubMed] [Google Scholar]
- 30.Tseng CH. Thyroid cancer risk is not increased in diabetic patients. PLoS One. 2012;7:e53096. doi: 10.1371/journal.pone.0053096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen YL, Cheng KC, Lai SW, Tsai IJ, Lin CC, Sung FC, Lin CC, Chen PC. Diabetes and risk of subsequent gastric cancer: a population-based cohort study in Taiwan. Gastric Cancer. 2013;16:389–396. doi: 10.1007/s10120-012-0197-7. [DOI] [PubMed] [Google Scholar]
- 32.Chiu CC, Huang CC, Chen YC, Chen TJ, Liang Y, Lin SJ, Chen JW, Leu HB, Chan WL. Increased risk of gastrointestinal malignancy in patients with diabetes mellitus and correlations with anti-diabetes drugs: a nationwide population-based study in Taiwan. Intern Med. 2013;52:939–946. doi: 10.2169/internalmedicine.52.8276. [DOI] [PubMed] [Google Scholar]
- 33.Origasa H, Lee SH, Nakagawa H, Kumagai N, Fuse H, Tobe K. Pioglitazone use and bladder cancer - hospital-based results from a nested case-control study in Japan. Jpn Pharmacol Ther. 2013;41:5. [Google Scholar]
- 34.Simo R, Plana-Ripoll O, Puente D, Morros R, Mundet X, Vilca LM, Hernandez C, Fuentes I, Procupet A, Tabernero JM, Violan C. Impact of glucose-lowering agents on the risk of cancer in type 2 diabetic patients. The Barcelona case-control study. PLoS One. 2013;8:e79968. doi: 10.1371/journal.pone.0079968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen YC, Kok VC, Chien CH, Horng JT, Tsai JJ. Cancer risk in patients aged 30 years and above with type 2 diabetes receiving antidiabetic monotherapy: a cohort study using metformin as the comparator. Ther Clin Risk Manag. 2015;11:1315–1323. doi: 10.2147/TCRM.S91513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin CM, Huang HL, Chu FY, Fan HC, Chen HA, Chu DM, Wu LW, Wang CC, Chen WL, Lin SH, Ho SY. Association between Gastroenterological Malignancy and Diabetes Mellitus and Anti-Diabetic Therapy: A Nationwide, Population-Based Cohort Study. PLoS One. 2015;10:e0125421. doi: 10.1371/journal.pone.0125421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Son JW, Lee IK, Woo JT, Baik SH, Jang HC, Lee KW, Cha BS, Sung YA, Park TS, Yoo SJ, Yoon KH. A prospective, randomized, multicenter trial comparing the efficacy and safety of the concurrent use of long-acting insulin with mitiglinide or voglibose in patients with type 2 diabetes. Endocr J. 2015;62:1049–1057. doi: 10.1507/endocrj.EJ15-0325. [DOI] [PubMed] [Google Scholar]
- 38.Dabrowski M, Szymanska-Garbacz E, Miszczyszyn Z, Derezinski T, Czupryniak L. Risk factors for cancer development in type 2 diabetes: a retrospective case-control study. BMC Cancer. 2016;16:785. doi: 10.1186/s12885-016-2836-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tseng CH. Use of metformin and risk of kidney cancer in patients with type 2 diabetes. Eur J Cancer. 2016;52:19–25. doi: 10.1016/j.ejca.2015.09.027. [DOI] [PubMed] [Google Scholar]
- 40.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2012;55:1577–1596. doi: 10.1007/s00125-012-2534-0. [DOI] [PubMed] [Google Scholar]
- 41.Rosak C, Mertes G. Critical evaluation of the role of acarbose in the treatment of diabetes: patient considerations. Diabetes Metab Syndr Obes. 2012;5:357–367. doi: 10.2147/DMSO.S28340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhu Q, Tong Y, Wu T, Li J, Tong N. Comparison of the hypoglycemic effect of acarbose monotherapy in patients with type 2 diabetes mellitus consuming an Eastern or Western diet: a systematic meta-analysis. Clin Ther. 2013;35:880–899. doi: 10.1016/j.clinthera.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 43.Yang W, Liu J, Shan Z, Tian H, Zhou Z, Ji Q, Weng J, Jia W, Lu J, Liu J, Xu Y, Yang Z, Chen W. Acarbose compared with metformin as initial therapy in patients with newly diagnosed type 2 diabetes: an open-label, non-inferiority randomised trial. Lancet Diabetes Endocrinol. 2014;2:46–55. doi: 10.1016/S2213-8587(13)70021-4. [DOI] [PubMed] [Google Scholar]
- 44.Inoue I, Takahashi K, Noji S, Awata T, Negishi K, Katayama S. Acarbose controls postprandial hyperproinsulinemia in non-insulin dependent diabetes mellitus. Diabetes Res Clin Pract. 1997;36:143–151. doi: 10.1016/s0168-8227(97)00045-4. [DOI] [PubMed] [Google Scholar]
- 45.Derosa G, Maffioli P, Ferrari I, Fogari E, D’Angelo A, Palumbo I, Randazzo S, Bianchi L, Cicero AF. Acarbose actions on insulin resistance and inflammatory parameters during an oral fat load. Eur J Pharmacol. 2011;651:240–250. doi: 10.1016/j.ejphar.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 46.Chen HH, Chen DY, Chao YH, Chen YM, Wu CL, Lai KL, Lin CH, Lin CC. Acarbose decreases the rheumatoid arthritis risk of diabetic patients and attenuates the incidence and severity of collagen-induced arthritis in mice. Sci Rep. 2015;5:18288. doi: 10.1038/srep18288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Su B, Liu H, Li J, Sunli Y, Liu B, Liu D, Zhang P, Meng X. Acarbose treatment affects the serum levels of inflammatory cytokines and the gut content of bifidobacteria in Chinese patients with type 2 diabetes mellitus. J Diabetes. 2015;7:729–739. doi: 10.1111/1753-0407.12232. [DOI] [PubMed] [Google Scholar]
- 48.Groop PH, Groop L, Totterman KJ, Fyhrquist F. Effects of acarbose on the relationship between changes in GIP and insulin responses to meals in normal subjects. Acta Endocrinol (Copenh) 1986;112:361–366. doi: 10.1530/acta.0.1120361. [DOI] [PubMed] [Google Scholar]
- 49.Qualmann C, Nauck MA, Holst JJ, Orskov C, Creutzfeldt W. Glucagon-like peptide 1 (7-36 amide) secretion in response to luminal sucrose from the upper and lower gut. A study using alpha-glucosidase inhibition (acarbose) Scand J Gastroenterol. 1995;30:892–896. doi: 10.3109/00365529509101597. [DOI] [PubMed] [Google Scholar]
- 50.Enc FY, Imeryuz N, Akin L, Turoglu T, Dede F, Haklar G, Tekesin N, Bekiroglu N, Yegen BC, Rehfeld JF, Holst JJ, Ulusoy NB. Inhibition of gastric emptying by acarbose is correlated with GLP-1 response and accompanied by CCK release. Am J Physiol Gastrointest Liver Physiol. 2001;281:G752–G763. doi: 10.1152/ajpgi.2001.281.3.G752. [DOI] [PubMed] [Google Scholar]
- 51.Zheng MY, Yang JH, Shan CY, Zhou HT, Xu YG, Wang Y, Ren HZ, Chang BC, Chen LM. Effects of 24-week treatment with acarbose on glucagon-like peptide 1 in newly diagnosed type 2 diabetic patients: a preliminary report. Cardiovasc Diabetol. 2013;12:73. doi: 10.1186/1475-2840-12-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jeon SG, Kayama H, Ueda Y, Takahashi T, Asahara T, Tsuji H, Tsuji NM, Kiyono H, Ma JS, Kusu T, Okumura R, Hara H, Yoshida H, et al. Probiotic Bifidobacterium breve induces IL-10-producing Tr1 cells in the colon. PLoS Pathog. 2012;8:e1002714. doi: 10.1371/journal.ppat.1002714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang Q, Xiao X, Li M, Li W, Yu M, Zhang H, Wang Z, Xiang H. Acarbose reduces blood glucose by activating miR-10a-5p and miR-664 in diabetic rats. PLoS One. 2013;8:e79697. doi: 10.1371/journal.pone.0079697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Weaver GA, Tangel CT, Krause JA, Parfitt MM, Stragand JJ, Jenkins PL, Erb TA, Davidson RH, Alpern HD, Guiney WB, Jr, Higgins PJ. Biomarkers of human colonic cell growth are influenced differently by a history of colonic neoplasia and the consumption of acarbose. J Nutr. 2000;130:2718–2725. doi: 10.1093/jn/130.11.2718. [DOI] [PubMed] [Google Scholar]
- 55.Holt PR, Atillasoy E, Lindenbaum J, Ho SB, Lupton JR, McMahon D, Moss SF. Effects of acarbose on fecal nutrients, colonic pH, and short-chain fatty acids and rectal proliferative indices. Metabolism. 1996;45:1179–1187. doi: 10.1016/s0026-0495(96)90020-7. [DOI] [PubMed] [Google Scholar]
- 56.Hague A, Singh B, Paraskeva C. Butyrate acts as a survival factor for colonic epithelial cells: further fuel for the in vivo versus in vitro debate. Gastroenterology. 1997;112:1036–1040. doi: 10.1053/gast.1997.v112.agast971036. [DOI] [PubMed] [Google Scholar]
- 57.Ron Y, Wainstein J, Leibovitz A, Monastirsky N, Habot B, Avni Y, Segal R. The effect of acarbose on the colonic transit time of elderly long-term care patients with type 2 diabetes mellitus. J Gerontol A Biol Sci Med Sci. 2002;57:M111–M114. doi: 10.1093/gerona/57.2.m111. [DOI] [PubMed] [Google Scholar]
- 58.Potter JD. Reconciling the epidemiology, physiology, and molecular biology of colon cancer. JAMA. 1992;268:1573–1577. [PubMed] [Google Scholar]
- 59.Ligumsky H, Wolf I, Israeli S, Haimsohn M, Ferber S, Karasik A, Kaufman B, Rubinek T. The peptide-hormone glucagon-like peptide-1 activates cAMP and inhibits growth of breast cancer cells. Breast Cancer Res Treat. 2012;132:449–461. doi: 10.1007/s10549-011-1585-0. [DOI] [PubMed] [Google Scholar]
- 60.Koehler JA, Kain T, Drucker DJ. Glucagon-like peptide-1 receptor activation inhibits growth and augments apoptosis in murine CT26 colon cancer cells. Endocrinology. 2011;152:3362–3372. doi: 10.1210/en.2011-1201. [DOI] [PubMed] [Google Scholar]
- 61.Quesada CF, Kimata H, Mori M, Nishimura M, Tsuneyoshi T, Baba S. Piroxicam and acarbose as chemopreventive agents for spontaneous intestinal adenomas in APC gene 1309 knockout mice. Jpn J Cancer Res. 1998;89:392–396. doi: 10.1111/j.1349-7006.1998.tb00576.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nie SP, Chen H, Zhuang MQ, Lu M. Anti-diabetic medications do not influence risk of lung cancer in patients with diabetes mellitus: a systematic review and meta-analysis. Asian Pac J Cancer Prev. 2014;15:6863–6869. doi: 10.7314/apjcp.2014.15.16.6863. [DOI] [PubMed] [Google Scholar]
- 63.Wu Y, Liu HB, Shi XF, Song Y. Conventional hypoglycaemic agents and the risk of lung cancer in patients with diabetes: a meta-analysis. PLoS One. 2014;9:e99577. doi: 10.1371/journal.pone.0099577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhu N, Zhang Y, Gong YI, He J, Chen X. Metformin and lung cancer risk of patients with type 2 diabetes mellitus: a meta-analysis. Biomed Rep. 2015;3:235–241. doi: 10.3892/br.2015.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Higgins J PT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2011. [Google Scholar]
- 66.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. 2013 [Google Scholar]
- 68.Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 70.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 71.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


