Abstract
To determine some of the key clinical features that help prompt clinicians to pursue additional work-up for evaluation of CNS involvement of MF, we conducted a systematic review to better define characteristics, treatments, outcomes, and mortality in these patients. Our analyses indicated that neurologic surveillance after the diagnosis of MF is crucial. Review of systems should include change in mentation, vestibular, and ocular symptoms. Progression to CNS involvement does not always occur in tandem with cutaneous disease burden. Single-agent therapies can delay disease progression and improve prognosis. Multi-agent treatment does not improve survival.
Keywords: Cutaneous T-cell lymphoma, Lymphoma, Mycosis fungoides, Central nervous system diseases, Brain metastasis
1. Introduction
Mycosis fungoides (MF) is the most common cutaneous T-cell lymphoma. It is more common in older adults, and lesion types include: patches, plaques, and tumors with a variable disease course [1], [2], [3]. Patients with plaques and tumors have greater morbidity and mortality and many develop blood and lymph nodes involvement. Ultimately many patients die due to overwhelming infections, and some develop fatal metastatic disease. The most common sites of extracutaneous involvement are the liver, spleen and lungs [4]. Central nervous system (CNS) involvement is very rare and associated symptoms are scattered amongst case reports and case series. To determine some of the key clinical features that help prompt clinicians to pursue additional work-up for evaluation of CNS involvement of MF, we conducted a systematic review to better define patient characteristics, treatments, outcomes, and mortality in these patients. We did this with the hope of providing clinicians and researchers with the distinguishing symptoms experienced by MF patients with CNS metastases, and informing expectations about the disease course and treatment selection when managing these patients.
2. Methods
2.1. Data search
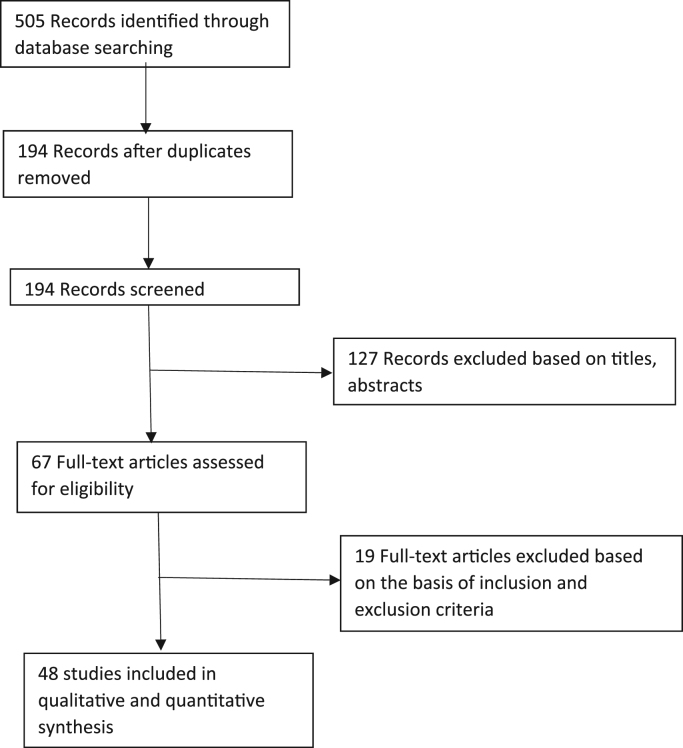
Our study followed the "PRISMA Statement" guidelines [5]. We independently searched Ovid MEDLINE, Scopus, and PubMed for studies published in English. For Ovid MEDLINE, the following search terms were used: “mycosis fungoides”, combined with “CNS”, “central nervous system”, “brain”, “central nervous system neoplasm”, “brain metastasis”, and “spinal cord”. From this initial search 194 unique reports were identified. Only case reports, case series, and cohort studies published in the English language were included. If cohort studies included other peripheral T-cell lymphomas, only the patients with diagnoses of MF were included in the analyses. There were no restrictions regarding time periods in which the articles were published. Patients with radiographic and cerebrospinal fluid (CSF) analyses consistent with CNS involvement of MF but without reported brain biopsies were also included. Studies involving T-cell lymphomas other than MF, studies not in English, or studies in which there were cranial involvement such as the ears, mouth, throat without direct involvement of the CNS were excluded. After review, 48 articles were included in our analyses (Fig. 1) [3], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [54], [44], [45], [46], [47], [48], [49], [50], [51], [52].
Fig. 1.
Flowchart of selected studies for systematic review.
2.2. Study selection and data extraction
For relevant articles, the entire text was thoroughly reviewed. Information regarding age, gender, ethnicity, cutaneous findings, stage at the time of diagnosis, sites of visceral involvement, symptoms at the time of CNS metastasis, treatments prior to and after CNS involvement, cerebrospinal fluid (CSF) analysis, computed tomography (CT), and magnetic resonance imaging (MRI) studies were extracted from the selected articles. A Pearson's chi-squared test was performed to compare treatment modalities between survivors and deceased patients. Analyses were run at a nominal 0.05 type I error rate.
3. Results
From the 40 case reports and 8 case series meeting the inclusion criteria, a total of 77 patients were identified with CNS metastasis of MF: 47% Caucasian, 4% Black, 1% Asian, 48% unstated ethnicity. The clinical and demographic characteristics of patients in the 48 selected studies are listed in Table 1. Data was analyzed based on reported variables since not all 48 studies provided information for each item of interest. The median interval from the time of MF diagnosis to CNS metastasis was 36 months while the median interval from CNS involvement to death was 9 weeks. Ten patients achieved complete remission and one patient was lost to follow-up.
Table 1.
Clinical and demographic characteristics.
| Total number of patients | 77 |
| Average age (years) | 44 |
| Median age (years) | 58 |
| Age range (years) | 17–87 |
| Female | 22% |
| Male | 78% |
| Caucasian | 47% |
| Black | 4% |
| Asian | 1% |
| No Ethnicity Stated | 48% |
| Cutaneous Presentation at the time of CNS involvement | |
| Tumor | 34 |
| Plaques Only | 27 |
| Erythroderma | 9 |
| Ulcerated | 6 |
| Granulomatous MF | 1 |
| Staging (n = 31) | |
| IA/B | 12 |
| IIA/B | 6 |
| IIIA | 8 |
| IVB | 5 |
The clinical stage at the time of MF diagnosis was reported in 31 patients as follows: 12 were IA/B, 6 were at stage IIA/B, 8 were at stage IIIA/B and 5 were IVA/B. Cutaneous plaques and tumors were the most common types of cutaneous lesions at the time of CNS involvement, accounting for 35% and 44%, respectively (Table 1).
3.1. CNS symptoms and visceral involvement
All but two patients exhibited neurologic deficits as MF progressed to the CNS. Symptoms included: general systemic abnormality, vestibular, cognitive, and ocular changes. The data was summarized in Table 2. Specifically, gait instability, dizziness, weakness in extremities were the most common manifestations, accounting for 44% of the presentations. Cognitive dysfunction included confusion, amnesia, and slowed thinking were presented in 39% of patients; whereas lethargy, fatigue, malaise and somnolence were seen in 31% of the cases. Of note, ocular manifestations including diplopia, blurred vision, blindness, eye pain, nystagmus, hemianopia or quadrantanopia, proptosis, papillary edema were exhibited in 29% of the patients. For the two patients who lacked neurologic deficits, infiltration of the cerebrum and/or cerebellum were found at autopsy.
Table 2.
CNS manifestations.
| CNS Symptoms | Number of Patients (n = 77) | Percent of Respondents |
|---|---|---|
| Gait Instability/Dizziness/Weakness in extremities | 34 | 44% |
| Confusion/Slowed Thinking/Memory Problems | 30 | 39% |
| Lethargy/Fatigue/Somnolence/Malaise | 24 | 31% |
| Ocular changes (diplopia, blurred vision, blindness, eye pain, nystagmus, hemi/quandrantopsia, proptosis, papillary edema) | 22 | 29% |
| Headache | 16 | 21% |
| Dysarthria/Dysphasia/Aphasia | 15 | 19% |
| AMS | 14 | 18% |
| Peripheral Neuropathy/Numbness/Loss of Sensation/Paresthesias | 9 | 12% |
| Personality Change/Withdrawal/Depression | 8 | 10% |
| Nausea/Vomiting | 8 | 10% |
| Auditory (hearing loss, tinnitus) | 6 | 8% |
| Incontinence/Constipation/Urinary retention | 6 | 8% |
| Movement Disorder: Hyperreflexia, chorea | 6 | 8% |
| Fever of Unknown Origin | 3 | 4% |
| Hallucinations | 2 | 3% |
| No CNS symptoms | 2 | 3% |
At the time of CNS metastasis, 53% (27/51) of the patients had lymphadenopathy, 33% (16/48) had Sezary cells in peripheral blood, and 24% (13/55) had large cell transformation. Overall, 53% (34/64) had concurrent metastasis to other extracutaneous organs including lung (27%), gastrointestinal systems including pancreas (20%), liver (16%), spleen (15%), nasopharynx or oropharynx (13%), kidney (10%), eye (10%). Only 1 patient presented MF metastasis to the genital system.
3.2. Work-up and diagnostic imaging
Almost all the patients exhibited abnormal findings on imaging studies. MRI identified 91% (20/22) of CNS abnormalities while 74% (28/38) of CNS lesions were identified with CT scans. Only two studies utilized PET-CT scans to confirm initial CNS involvement, track response to treatment, and examine other extracranial involvement. None of the case reports or case series mentioned HTLV-1 status or travel history. CNS involvement was diagnosed based on clinical presentation, biopsy, CSF analysis, and autopsy.
Of the 42 cases with CSF analysis, 34 revealed Sezary cells or lymphocytic pleocytosis in CSF, 28 exhibited protein elevations, 13 showed glucose elevation, and 13 had opening pressure elevation. Only two cases revealed no imaging abnormalities. Of these two cases, CNS extension was diagnosed only on CSF analysis.
3.3. Treatment
Over half of the patients had more than one treatment modality prior to CNS metastasis. Data regarding prior treatments was summarized in Table 3. After CNS involvement was detected, the most common treatment modalities were radiation (60% cranial, 40% systemic), intrathecal methotrexate, and single agent chemotherapy.
Table 3.
Treatments before CNS metastasis.
| Number of Patients (n = 72) | Percent of all respondents | |
|---|---|---|
| Focal XRT | 33 | 46% |
| Topical Mustard/Carmustine | 25 | 35% |
| PUVA/UVB | 23 | 32% |
| TSEB | 17 | 24% |
| IFN | 15 | 21% |
| Combination Chemo: CMED/CEOP/COPP/MOPP/MCVP | 13 | 18% |
| MTX (PO or IV) | 12 | 17% |
| Single Agent Chemo: Doxorubicin/Gemcitabine/Cyclophosphamide/Vincristine/Chlorambucil | 12 | 17% |
| Steroids (Topical) | 11 | 15% |
| Bexarotene/Other Retinoid | 9 | 13% |
| Steroids (Systemic) | 8 | 11% |
| HDACi (Vorinostat/Romidepsin) | 2 | 3% |
| Bortezomib | 1 | 1% |
| IL2 | 1 | 1% |
| Zanolimumab | 1 | 1% |
| Arsenic Drop | 1 | 1% |
| Apheresis | 1 | 1% |
Pearson's chi-squared test was performed to compare treatment modalities for patients who achieved remission (median age, 56) to deceased patients (median age, 58), and no statistically significant differences were found (Table 4). The median interval from the time of MF diagnosis to CNS metastasis was 36 weeks for both survivors and deceased patients. When comparing the number of treatment modalities, approximately 60% of both groups received one or two types of therapy; however, 21% of the deceased patients received more than 4 different therapies compared to only 10% of the surviving patients. Of the twelve patients who refused CNS treatment, half died within one month after CNS diagnosis compared with a median survival time of 12 weeks for patients who received CNS treatment.
Table 4.
Compare treatments of survivors with deceased MF patients after CNS metastasis.
| Survivor (n = 10) | Deceased (n = 54) | p-value | |
|---|---|---|---|
| Temozol | 2 | 2 | 0.1 |
| Single Agent Chemotherapy | 1 | 14 | 0.15 |
| MTX (intrathecal/IV/PO) | 2 | 18 | 0.2 |
| Surgery | 2 | 3 | 0.2 |
| Cranial or Systemic Radiotherapy | 7 | 24 | 0.41 |
| Systemic Steroids | 6 | 20 | 0.44 |
| Palliation | 0 | 2 | 0.49 |
| Topical Mustard/Carmustine | 0 | 1 | 0.63 |
| IL2 | 0 | 1 | 0.63 |
| IFN | 0 | 1 | 0.63 |
| Vitamin A Derivatives | 1 | 0 | 0.63 |
| HDACi (Vorinostat/Romidepsin) | 1 | 0 | 0.63 |
| Arsenic | 1 | 0 | 0.63 |
| Combination Chemotherapy | 2 | 11 | 0.71 |
4. Discussion
Analyses of these 77 cases demonstrated that CNS involvement typically occurred 3–5 years after cutaneous diagnosis. These patients were of similar age as the general MF patient population (median age, 55) and the male to female ratio was approximately 3.5:1. Gait instability/weakness were the most common CNS symptoms followed by confusion/amnesia/slowed thinking. Our study also found that ocular manifestations, including diplopia, blurred vision, blindness, eye pain, nystagmus, hemianopia or quadrantanopia, proptosis, papillary edema, were relatively common symptoms seen in MF patients with CNS involvement. Therefore, CNS dissemination should be considered in patients with extremity weakness, confusion, cognitive changes or ocular symptoms. Additionally, review of systems in patients with late-stage disease should include review of neurologic or visual changes, and if present, a thorough ophthalmologic exam is warranted, along with consideration for imaging or CSF analysis.
According to previously published data, almost all cases of MF patients with CNS involvement had skin lesions and advanced infiltration of other organs at the time of CNS metastasis [6], [7]. Nearly half of the cases in our study did not experience visceral involvement. Only half of the patients experienced lymphadenopathy when neurologic symptoms developed. Importantly, five of the 77 patients were in clinical remission on cutaneous exam or had minimal cutaneous disease burden at the time of CNS metastasis. Therefore, neurologic deficits maybe the only manifestation of the metastatic disease.
Diagnosis of CNS involvement can be made by CT scan, MRI, and CSF analysis. According to our data, there is a consistent pattern in CSF analysis, including the presence of Sezary cells, lymphocytic pleocytosis, and elevation in protein, glucose, or opening pressure. Two cases with no abnormal brain imaging findings revealed lymphoma cells in CSF along with CSF protein elevation. This demonstrates that no individual test is completely reliable. Further workup including brain imaging and lumbar puncture for CSF analysis should be considered for patients with neurologic symptoms and a history of mycosis fungoides tumors or plaques, even if the skin is clear of disease at the onset of neurologic deficits.
Our findings validated the aggressive course of patients with tumor-stage disease, as this was the most common lesion type observed in patients with CNS metastases. Older males were more likely to develop CNS involvement of their lymphoma. Unfortunately, only 31 of the 77 cases clarified the patients’ stages at the time of MF diagnoses and at time of CNS metastases, and no cases reported HTLV-1 status. It is important for future reports to clearly define patient characteristics at the time of diagnosis and disease progression.
The available demographic and clinical characteristics were similar between survivors and patients who died of the metastatic disease. There were no symptoms or other features that were predictive of mortality, suggesting that other variables such as genetic mutations or other constitutional variables influence patient survival.
In our study, all treated patients received systemic therapy once CNS diagnosis was established. Twelve untreated patients all died within one month; treated patients survived a median duration of 3 months from the time of CNS presentation. Given the poor prognosis of untreated cases, early diagnosis and treatment of CNS involvement is crucial to improve patient survival. Additionally, combining radiation with single-agent chemotherapy should be considered for synergy and reduction of side effects. Almost all cases utilized more than one treatment modality; no specific therapy was significantly associated with a better prognosis for survivors compared to deceased patients. Importantly, those who achieved remission had fewer agents used in their treatment compared to patients who died. This finding suggests that patients not responding to the first treatment are less likely to achieve remission, and will likely have a fatal disease course. However, this conclusion is limited by a lack of available data on the frequency and duration of each treatment modality.
5. Conclusion
Our analyses underscored the importance of neurologic surveillance after the diagnosis of MF, particularly those with tumor-stage disease. Clinicians should consider a review of systems that includes ocular symptoms and neurologic alterations. Patients with neurologic deficits may warrant imaging studies and lumbar puncture for CSF analyses. There are no specific treatment guidelines for CNS metastasis in MF. Therefore, management should be customized based on the disease burden, clinical presentation, and functional status of each patient, with utilization of single-agent chemotherapy and radiation when possible to avoid overaggressive multi-agent treatment which does not improve survival.
Acknowledgements
None.
Acknowledgments
Funding sources
None.
Conflict of interest
None.
Contributors
Conceived and designed the experiments: YY, HW. Analysed the data: YY. Wrote the first draft of the manuscript: YY. Contributed to the writing of the manuscript: HW. Agree with manuscript results and conclusions: YY, HW. Jointly developed the structure and arguments for the paper: YY, HW. Made critical revisions and approved final version: HW. All authors reviewed and approved of the final manuscript.
Contributor Information
Yi Yang, Email: Yi1.Yang@utsouthwestern.edu.
Heather Wickless, Email: Heather.Wickless@utsouthwestern.edu.
References
- 1.Block J., Edglomb J., Eisen A., van Scot J. Mycosis fungoides: natural history and aspects of its relationship to other magnant lymphomas. Am. J. Med. 1963;34:218–235. doi: 10.1016/0002-9343(63)90056-1. [DOI] [PubMed] [Google Scholar]
- 2.van Scott E.J., Vonderheld E.C. 2nd ed. McGraw-Hill Book Company; New York: 1977. Mycosis Fungoides and Sezary Syndrome in Hematology. [Google Scholar]
- 3.del Carpio-O'Donovan R., Freeman C. Brainstem involvement with mycosis fungoides: an unusual central nervous system complication. Am. J. Neuroradiol. 2002;23(4):533–534. [PMC free article] [PubMed] [Google Scholar]
- 4.Weinstock M.A., Reynes J.F. The changing survival of patients with mycosis fungoides: a population-based assessment of trends in the United States. Cancer. 1977;139:299–301. [PubMed] [Google Scholar]
- 5.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62(10):e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 6.Stein M., Farrar N., Jones G.W., Wilson L.D., Fox L., Wong R.K., Kuten A. Central neurologic involvement in mycosis fungoides: ten cases, actuarial risk assessment, and predictive factors. Cancer J. 2006;12(1):55–62. doi: 10.1097/00130404-200601000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Li N., Kim J.H., Glusac E.J. Brainstem involvement by mycosis fungoides in a patient with large-cell transformation: a case report and review of literature. J. Cutan. Pathol. 2003;30(5):326–331. doi: 10.1034/j.1600-0560.2003.00061.x. [DOI] [PubMed] [Google Scholar]
- 8.Gold J.H., Shelburne J.D., Bossen E.H. Meningeal mycosis fungoides: cytologic and ultrastructural aspects. Acta Cytol. 1976;20(4):349–355. [PubMed] [Google Scholar]
- 9.Bodensteiner D.C., Skikne B. Central nervous system involvement in mycosis fungoides: diagnosis, treatment and literature review. Cancer. 1982;50(6):1181–1184. doi: 10.1002/1097-0142(19820915)50:6<1181::aid-cncr2820500625>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 10.Hallahan D., Griem M., Griem S., Duda E., Baron J. Mycosis fungoides involving the central nervous system. J. Clin. Oncol. 1986;4(11):1638–1644. doi: 10.1200/JCO.1986.4.11.1638. [DOI] [PubMed] [Google Scholar]
- 11.Chua S.L., Seymour J.F., Prince H.M. Deafness from eighth cranial nerve involvement in a patient with large-cell transformation of mycosis fungoides. Eur. J. Haematol. 2000;64(5):340–343. doi: 10.1034/j.1600-0609.2000.9c119.x. [DOI] [PubMed] [Google Scholar]
- 12.Vu B.A., Duvic M. Central nervous system involvement in patients with mycosis fungoides and cutaneous large-cell transformation. J. Am. Acad. Dermatol. 2008;59(2Suppl 1):S16–S22. doi: 10.1016/j.jaad.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 13.Peris K., Fargnoli M.C., Berardelli A., Crecco M., Tomaselli R., Chimenti S. Peripheral nervous system involvement in a patient with large T-cell lymphoma arising from a pre-existing mycosis fungoides. Br. J. Dermatol. 1998;139(2):299–301. doi: 10.1046/j.1365-2133.1998.02371.x. [DOI] [PubMed] [Google Scholar]
- 14.Bird T.G., Whittaker S., Wain E.M., Child F., Morris S.L. Temozolomide for central nervous system involvement in mycosis fungoides. Int. J. Dermatol. 2016;55(7):751–756. doi: 10.1111/ijd.13007. [DOI] [PubMed] [Google Scholar]
- 15.Schowinsky J., Leppert M., Ney D., Kleinschmidt-DeMasters B.K. Prominent vascular and perivascular eosinophilic infiltrates. J. Neuropathol. Exp. Neurol. 2015;74(10):948–951. doi: 10.1097/NEN.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 16.Zhao G., Chamberlain M.C., Khot S.P., Shustov A., Olerud J.E., Shinohara M.M. Central nervous system involvement in cutaneous T-cell lymphoma: 2 illustrative cases and a review of current literature. Clin. Lymphoma Myeloma Leuk. 2014;14(1):e25–e30. doi: 10.1016/j.clml.2013.09.016. [DOI] [PubMed] [Google Scholar]
- 17.Elisa G., Elisabetta T., Luana B., Simona Z., Bruno D.S., Giannamaria C., Massimiliano G. Central nervous system involvement in mycosis fungoides: relevance of tcr gene testing in cerebrospinal fluid. SpringerPlus. 2014;3:29. doi: 10.1186/2193-1801-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harrington L., Sokol L., Holdener S., Shao H., Zhang L. Cutaneous gamma-delta T-cell lymphoma with central nervous system involvement: report of a rarity with review of literature. J. Cutan. Pathol. 2014;41(12):936–943. doi: 10.1111/cup.12395. [DOI] [PubMed] [Google Scholar]
- 19.Lindae M.L., Luy J., Abel E.A., Kaplan R. Mycosis fungoides with CNS involvement: neuropsychiatric manifestations and complications of treatment with intrathecal methotrexate and whole-brain irradiation. J. Dermatol. Surg. Oncol. 1990;16(6):550–553. doi: 10.1111/j.1524-4725.1990.tb00078.x. [DOI] [PubMed] [Google Scholar]
- 20.Zackheim H.S., Lebo C.F., Wasserstein P., McNutt N.S., Epstein E.H., Jr, Meyler S., Rosenbaum E.H., Grekin D.A. Mycosis fungoides of the mastoid, middle ear, and CNS. Literature review of mycosis fungoides of the CNS. Arch. Dermatol. 1983;119(4):311–318. [PubMed] [Google Scholar]
- 21.Weber M.B., McGavran M.H. Mycosis fungoides involving the brain. Arch. Neurol. 1967;16(6):645–650. doi: 10.1001/archneur.1967.00470240083012. [DOI] [PubMed] [Google Scholar]
- 22.Hauch T.W., Shelbourne J.D., Cohen H.J., Mason D., Kremer W.B. Meningeal mycosis fungoides: clinical and cellular characteristics. Ann. Intern. Med. 1975;82(4):499–505. doi: 10.7326/0003-4819-82-4-499. [DOI] [PubMed] [Google Scholar]
- 23.Zonenshayn M., Sharma S., Hymes K., Knopp E.A., Golfinos J.G., Zagzag D. Mycosis fungoides metastasizing to the brain parenchyma: case report. Neurosurgery. 1998;42(4):933–937. doi: 10.1097/00006123-199804000-00144. [DOI] [PubMed] [Google Scholar]
- 24.Beylot-Barry M., Dubus P., Vergier B., Cogrel O., Marit G., Beylot C., Merlio J.P. Meningeal involvement by a transformed mycosis fungoides following Hodgkin's disease. Br. J. Dermatol. 1999;141(5):909–913. doi: 10.1046/j.1365-2133.1999.03168.x. [DOI] [PubMed] [Google Scholar]
- 25.Lundberg W.B., Cadman E.C., Skeel R.T. Leptomeningeal mycosis fungoides. Cancer. 1976;38(5):2149–2153. doi: 10.1002/1097-0142(197611)38:5<2149::aid-cncr2820380545>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 26.Makepeace A.R., Sebag-Montefiore D., Spittle M.F., Smith N.P. Mycosis fungoides of the central nervous system. J. R. Soc. Med. 1989;82(2):116–117. doi: 10.1177/014107688908200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ward J.H., Kjeldsberg C.R. Spinal cord compression in mycosis fungoides. Cancer. 1982;50(11):2510–2512. doi: 10.1002/1097-0142(19821201)50:11<2510::aid-cncr2820501142>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 28.Jayakar V.V., Tilve G.H., Fernandes R.J., Rege U.G., Soman R.N. CNS involvement in mycosis fungoides. J. Postgrad. Med. 1980;26(3):204–206. [PubMed] [Google Scholar]
- 29.Rozati S., Kempf W., Ostheeren-Michaelis S., Bode-Lesniewska B., Zimmermann D.R., Dummer R., Cozzio A. Cutaneous diffuse large B-cell lymphoma, leg type, with bilateral intraocular involvement and infiltration to the CNS. J. Clin. Oncol. 2016;34(11):e93–e96. doi: 10.1200/JCO.2013.51.6559. [DOI] [PubMed] [Google Scholar]
- 30.Keltner J.L., Fritsch E., Cykiert R.C., Albert D.M. Mycosis fungoides. Intraocular and central nervous system involvement. Arch. Ophthalmol. 1977;95(4):645–650. doi: 10.1001/archopht.1977.04450040111017. [DOI] [PubMed] [Google Scholar]
- 31.DeCarvalho C., Shuttleworth E., Knox D., Dandalides P., Lowney E. Bilateral gaze paralysis with positive computerized tomography findings. Arch. Neurol. 1980;37(3):184–186. doi: 10.1001/archneur.1980.00500520082019. [DOI] [PubMed] [Google Scholar]
- 32.Lally A., Hollowood K., Whittaker S., Turner R. Central nervous system involvement in stage 1b mycosis fungoides. Br. J. Dermatol. 2007;157(4):815–816. doi: 10.1111/j.1365-2133.2007.08075.x. [DOI] [PubMed] [Google Scholar]
- 33.Hengstman G.J., van Rossum M.M., van der Kerkhof P.C., Bloem B.R. Chorea due to mycosis fungoides metastasis. J. Neurooncol. 2005;73(1):87–88. doi: 10.1007/s11060-004-3349-8. [DOI] [PubMed] [Google Scholar]
- 34.Law M., Teicher N., Zagzag D., Knopp E.A. Dynamic contrast enhanced perfusion MRI in mycosis fungoides. J. Magn. Reson. Imaging. 2003;18(3):364–367. doi: 10.1002/jmri.10361. [DOI] [PubMed] [Google Scholar]
- 35.Downs A.M., Love S., Kennedy C.C. Sudden death secondary to mycosis fungoides of the midbrain. Acta Derm. Venereol. 1999;79(6):475. doi: 10.1080/000155599750009960. [DOI] [PubMed] [Google Scholar]
- 36.Tacconi L., Eccles S., Johnston F.G., Symon L. Mycosis fungoides with central nervous system involvement – a case report: T-cell lymphoma of the brain. Surg. Neurol. 1995;43(4):389–392. doi: 10.1016/0090-3019(95)80069-s. [DOI] [PubMed] [Google Scholar]
- 37.Howlett D.C., Malcolm P.N., Wong W.L., Pembakian H., Smith N.P., Ayers A.B. Symptomatic intracranial involvement by mycosis fungoides. Clin. Oncol. 1995;7(6):395–396. doi: 10.1016/s0936-6555(05)80014-7. [DOI] [PubMed] [Google Scholar]
- 38.Tremblay G.F., Anderson J.M., Davidson D.L. Brain biopsy in the diagnosis of cerebral mycosis fungoides. J. Neurol. Neurosurg. Psychiatry. 1982;45(2):175–178. doi: 10.1136/jnnp.45.2.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pariser D.M. Mycosis fungoides involving the brain and optic nerves. Arch. Dermatol. 1978;114(3):397–399. [PubMed] [Google Scholar]
- 40.Aach R., Kissane J. Mycosis fungoides with pulmonary and neurologic complications. Am. J. Med. 1967;42(1):129–138. doi: 10.1016/0002-9343(67)90010-1. [DOI] [PubMed] [Google Scholar]
- 41.Ramesh V., Saxena U., Misra R.S., Mukherjee A. Mycosis fungoides with fatal brain involvement. Australas. J. Dermatol. 1989;30(2):73–75. doi: 10.1111/j.1440-0960.1989.tb00421.x. [DOI] [PubMed] [Google Scholar]
- 42.Conomy J.P., Michel B., Ferguson J., Graham R., Kellermeyer R. Central nervous system involvement in mycosis fungoides: pre mortem diagnosis by light and electron microsocopic study of the spinal fluid. Neurol. Neurocir. Psiquiatr. 1977;18(2–3 Suppl):S421–S426. [PubMed] [Google Scholar]
- 54.Wabulya A., Imitola J., Santagata S., Kesari S. Mycosis fungoides with leptomeningeal involvement. J. Clin. Oncol. 2007;25(35):5658–5661. doi: 10.1200/JCO.2007.14.3800. [DOI] [PubMed] [Google Scholar]
- 44.Chang A.H., Ng A.B. The cellular manifestations of mycosis fungoides in cerebrospinal fluid. A case report. Acta Cytol. 1975;19(2):148–151. [PubMed] [Google Scholar]
- 45.Vitek J.J., Duvall E.R. Cranial computed tomography in the tumorous stage of mycosis fungoides. J. Comput. Assist. Tomogr. 1982;6(4):702–705. doi: 10.1097/00004728-198208000-00006. [DOI] [PubMed] [Google Scholar]
- 46.Conrad M.E., Omura G.A. Mycosis fungoides: carcinogens and cerebral involvement. Am. J. Med. Sci. 1987;293(2):122–124. doi: 10.1097/00000441-198702000-00010. [DOI] [PubMed] [Google Scholar]
- 47.Tien R.D., Brown M., Massey E.W. CNS mycosis fungoides: CT and MR findings. J. Comput. Assist. Tomogr. 1992;16(4):529–533. doi: 10.1097/00004728-199207000-00005. [DOI] [PubMed] [Google Scholar]
- 48.van Erp M.G., van Vloten W.A., de Groot-Verhaar J.C., Buruma O.J. Neurological sequelae in mycosis fungoides. Report of a case. Eur. Neurol. 1981;20(5):388–393. doi: 10.1159/000115266. [DOI] [PubMed] [Google Scholar]
- 49.Görg C., Görg K., Bepler G., Adler G., Gropp C., Havemann K. Atypical mycosis fungoides with cerebral involvement. J. Cancer Res. Clin. Oncol. 1985;110(2):123–126. doi: 10.1007/BF00402724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ke M.S., Kamath N.V., Nihal M., Mikkola D.L., Koc O.N., Stevens S.R., Gilliam A.C., Cooper K.D., Wood G.S. Folliculotropic mycosis fungoides with central nervous system involvement: demonstration of tumor clonality in intrafollicular T cells using laser capture microdissection. J. Am. Acad. Dermatol. 2003;48(2):238–243. doi: 10.1067/mjd.2003.43. [DOI] [PubMed] [Google Scholar]
- 51.Kim E.E., DeLand F.H., Maruyama Y. Brain and lung involvement of mycosis fungoides demonstrated by radionuclide imaging. J. Nucl. Med. 1979;20(3):240–242. [PubMed] [Google Scholar]
- 52.Hagedorn M., Freudenberg N., Petres J. Mycosis fungoides with marked brain involvement – a case report. Arch. Dermatol. Forsch. 1975;252(3):179–186. doi: 10.1007/BF00557917. [DOI] [PubMed] [Google Scholar]