Abstract
Background
The positions of the mandibular lingula and foramen have been set as indexes for inferior alveolar nerve (IAN) block and ramus osteotomies in orthognathic surgery. This study aimed to evaluate the anatomical structures of mandibular ramus, especially the mandibular lingula and foramen, by analyzing the cone-beam computed tomography (CBCT) data of young adults.
Methods
We evaluated 121 sides of hemi-mandibular CBCT model of 106 patients (51 male and 55 female patients; 18 to 36 years old). All the measurements were performed using the 2- and 3-dimensional rulers of OnDemand3D® software.
Results
Statistical analysis of the data revealed that there was no significant difference in the mandibular angle between the genders. The mandibular lingula was found to be located at the center of ramus in males, but a little posterior in relation to the center in females. The mandibular lingula was rarely located below the occlusal plane; however, the position of the mandibular foramen was more variable (84.3% below, 12.4% above, and 3.3% at the level of the occlusal plane).
Conclusions
The results of this study provide a valuable guideline for IAN block anesthesia and orthognathic surgery. CBCT can be considered effective and accurate in evaluating the fine structures of the mandible.
Keywords: 3D Anatomy, Mandibular ramus, Lingula, Foramen, Cone-beam CT
Background
It is important to know the precise anatomical positions of the mandibular lingula (ML) and mandibular foramen (MF) in routine dental practice, especially during block anesthesia of inferior alveolar nerve (IAN) and orthognathic surgery. The failure rate of IAN block has been reported to range between 10 and 39% [1, 2], and the most common reason for this failure points to the inaccurate placement of the hypodermic needle tip, which is not close enough to the MF [3]. Proper evaluation of the anatomical landmarks in relation to the IAN, such as the MF and ML, is the key to the achievement of effective anesthesia of the IAN in clinical practices of the mandible. Dentofacial deformities, especially mandibular prognathism and retrognathism that are caused by abnormal growth of the jaw, occur in a relatively high incidence among Asians [4]. In recent years, sagittal split ramus osteotomy has become a routine surgical technique for the correction of these deformities owing to its advantages, such as the intraoral approach, easy internal fixation, decreased healing time, and early jaw function [5–7]. Determining the precise anatomical locations of the ML and MF is essential in order to achieve a favorable fracture line on the mandibular ramus and prevent IAN damage and other complications during orthognathic surgery. The ML has been described as an important surgical landmark for horizontal osteotomy in orthognathic surgery because the horizontal osteotomy is positioned close to the ML and IAN [5–8]. Further, the accurate location of the ML is critical to a large number of other oral and maxillofacial surgical procedures, such as mandibular trauma management, benign and malignant tumor removal, mandibular and temporomandibular joint (TMJ) reconstruction, and pre-prosthetic surgery [9].
The application of cone-beam computed tomography (CBCT) in dentistry has rapidly developed in recent years, especially in implantology, because CBCT has been shown to overcome many disadvantages of conventional medical computed tomography (CT), such as the high dose of radiation, long radiation exposure time, and low resolution ratio. It has been reported that the radiation dose of CBCT is just 25% of the radiation dose of a panoramic radiograph and 1.6 to 2.5% of that of a conventional medical CT [10, 11]. One of the most remarkable advantages of CBCT is its high resolution ratio; a voxel size as small as 0.125 mm can be achieved with CBCT, which translates into a powerful ability to obtain accurate 3-dimensional (3D) reconstructions [12–15].
Recently, CBCT has been used frequently to determine the accurate anatomy of oral and maxillofacial structures, such as the root canal system, inferior alveolar canal, impacted teeth, TMJ, and even the upper respiratory tract [15–23]. Therefore, this retrospective study is designed to use CBCT data to verify the positions of the MF and ML in relation to the surrounding landmarks; and to give an accurate description of the anatomical morphology of the mandibular ramus.
Methods
This retrospective study was based on the CBCT data collected from the Division of Oral and Maxillofacial Surgery, Department of Dentistry, Korea University Anam Hospital, Seoul, between 4 June, 2013, and 29 July, 2014 (IRB approval: AN14291-001). Patients under 18 years of age were excluded from the study owing to the incomplete development of the mandible. Also, the patients with syndromic craniofacial deformity were excluded. Most of the patients had been advised to undergo CBCT scans of the mandibular body and ramus in order to determine the 3D relationship of the third molar with the inferior alveolar canal prior to its extraction.
All the CBCT examinations had been carried out using an AZ3000CT 3D imaging system (Asahi Roentgen Co., Kyoto, Japan). The imaging parameters had been set as follows: 6 mA, 85 kV, 0.5 × 0.5 mm fixed focal spot, and the field of view (FOV) of 80-mm height and 75-mm diameter. The total scanning time had been 17 s.
Using the CBCT data, 3D models of the mandibles were constructed using OnDemand3D® software (CyberMed International, Seoul, Korea) with a voxel size of 0.2 mm and slice thickness of 0.2 mm. Prior to obtaining measurements, two reference planes were defined to standardize the 3D positions of all the mandibular models. The occlusal plane was defined using three points (mesiobuccal cusp tips of both mandibular first molars and a mid-point of both mandibular central incisors) as the horizontal reference plane, and a plane along the line from the cusp of the canine to the mesiobuccal cusp of the first molar and perpendicular to the occlusal plane was defined as the sagittal reference plane (Figs. 1 and 2).
Fig. 1.
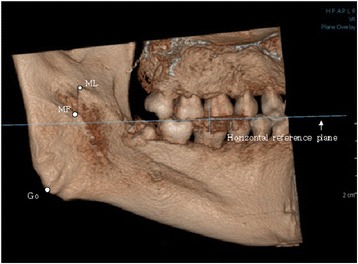
The occlusal plane was set as the horizontal reference plane to standardize the 3D positions of all the mandible models. (ML, mandibular lingula; MF, mandibular foreman; Go, gonion)
Fig. 2.
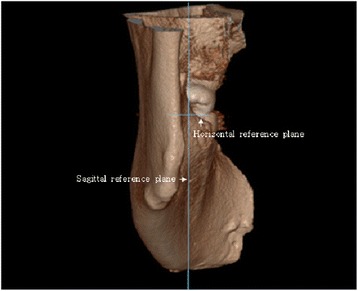
The plane perpendicular to the occlusal plane and along the line from the cusp of canine to the mesiobuccal cusp of the first molar was set as the sagittal reference plane
All measurements were carried out twice by the same operator with the mandibular models placed in a standardized position. Analysis was conducted using mean values of two repeated measurements and if two measurement values showed over 1-mm differences measured again and used two values having lower differences. The ML was set as the reference point for the measurements; measurements were obtained using the 3D ruler of OnDemand3D® software (Table 1). With the occlusal plane for reference, the anteroposterior and vertical relationships of the ML and MF were measured using the 2-dimensional (2D) ruler.
Table 1.
Measurements of mandibular ramus morphology
| 1. Mandibular angle: angle between two tangent lines of ower border and posterior border |
| 2. ML–MF: distance from ML to MF |
| 3. AP: anteroposterior ramal dimension at ML parallel to OP |
| 4. ML–internal line: distance from ML to internal oblique line parallel to OP |
| 5. ML–external line: distance from ML to external oblique line parallel to OP |
| 6. ML–posterior line: distance from ML to posterior border of the ramus parallel to OP |
| 7. ML–SN: distance from ML to the lower point of sigmoid notch |
| 8. ML–second molar: distance from ML to the CEJ of mandibular second molar |
| 9. ML–lower border: distance from ML to the lower border of ramus |
| 10. ML–Go: distance from ML to Go |
Abbreviations: ML, mandibular lingula; MF, mandibular foreman; AP, anteroposterior; OP, occlusal plane; SN, sigmoid notch; Go, gonion
The statistical differences in the mandibular ramus morphology between male and female subjects were determined using independent t-tests with a significance level of P < 0.05. All the statistical analyses were performed using SPSS 21.0 (SPSS Inc., IL, USA).
Results
In this study, 121 sides of hemi-mandibular CBCT models of 106 patients (51 male and 55 female patients; mean age 26.8 ± 8.7 years, range 18 to 36 years) were examined. Of these, 101 patients had undergone CBCT examination for determining the 3D relationship of the third molar with the inferior alveolar canal prior to its extraction; the remaining 5 patients had undergone this test in order for examination of cystic lesions in the molar region.
The results of the measurements of the mandibular ramus are presented in Table 2. The mean mandibular angle was 125.1° in males and 124.1° in females. No statistically significant difference in the mandibular angle based on gender was detected (P > 0.05). At the ML level, the anteroposterior ramal dimension was significantly greater in males (34.6 ± 2.4 mm) than in females (31.5 ± 2.4 mm) (P < 0.05). In males, the ML was found to be located in the center of the width of the ramus, with the same mean distance of 18.2 mm from the most anterior and posterior border of the ramus. However, it was positioned a little posterior to the center of the ramus in females, with a mean distance of 18.3 ± 2.2 mm from the anterior border and 17.0 ± 1.8 mm from the posterior border of the ramus.
Table 2.
Data of measurements on mandibular ramus morphology
| Measurement | Sex | Mean ± SD | Min~Max | P value |
|---|---|---|---|---|
| Mandibular angle (°) | M | 125.1 ± 4.9 | 112.3~134.9 | 0.240 |
| F | 124.1 ± 4.9 | 108.3~134.0 | ||
| ML–MF (mm) | M | 10.1 ± 2.3 | 4.8~15.9 | 0.385 |
| F | 9.8 ± 2.1 | 5.4~15.7 | ||
| AP (mm) | M | 34.6 ± 2.4 | 29.4~39.6 | 0.014* |
| F | 31.5 ± 2.4 | 29.2~39.8 | ||
| ML–internal line (mm) | M | 13.9 ± 1.9 | 10.7~19.4 | 0.424 |
| F | 13.6 ± 2.1 | 8.6~17.7 | ||
| ML–external line (mm) | M | 18.2 ± 2.4 | 14.3~25.6 | 0.894 |
| F | 18.3 ± 2.2 | 12.8~24.1 | ||
| ML–posterior line (mm) | M | 18.2 ± 1.7 | 15.2~21.7 | 0.000* |
| F | 17.0 ± 1.8 | 12.1~21.4 | ||
| ML–SN (mm) | M | 15.7 ± 2.7 | 11.1~23.1 | 0.768 |
| F | 15.5 ± 2.3 | 11.7~22.9 | ||
| ML–second molar (mm) | M | 31.0 ± 3.3 | 21.6~36.3 | 0.001* |
| F | 28.1 ± 2.9 | 24.4~37.4 | ||
| ML–lower border (mm) | M | 35.3 ± 3.3 | 27.0~42.8 | 0.000* |
| F | 30.5 ± 2.8 | 25.2~38.5 | ||
| ML–Go (mm) | M | 33.8 ± 3.2 | 24.5~41.9 | 0.000* |
| F | 28.9 ± 3.0 | 22.7~35.9 |
Abbreviations: ML, mandibular lingula; MF, mandibular foreman; AP, anteroposterior; SN, sigmoid notch; Go, gonion
*Statistical significance
The distance of the ML from the lower border of mandible (35.3 ± 3.3 mm in males; 30.5 ± 2.8 mm in females) was always greater than its distance from the mandibular sigmoid notch (15.7 ± 2.7 mm in males; 15.5 ± 2.3 mm in females). The ML was located approximately at the junction of the upper one third and lower two thirds of the line joining the lower border of the ramus and the sigmoid notch. The distance of the ML from the CEJ of the second molar in males (31.0 ± 3.3 mm) was found to be statistically greater than that in females (28.1 ± 2.9 mm) with P < 0.05. The data showed a statistically significant difference between males and females in relation to the distance of the ML from the gonion (P < 0.05); the ML was farther from the gonion in males.
The data revealed great variation in the 3D distance between ML and MF (4.8 to 15.9 mm in males; 5.4 to 15.7 mm in females). Further, the anatomical forms of the ML and MF displayed great variability, too. In the standard position, the relationship of the ML and MF to the occlusal plane was evaluated. We found that 98.3% of the lingulae were located 6.0 ± 2.9 mm above the occlusal plane (Figs. 3 and 4); one ML (0.8%) was equal with the occlusal plane (Fig. 5) and one (0.8%) was below the occlusal plane (Table 3).
Fig. 3.
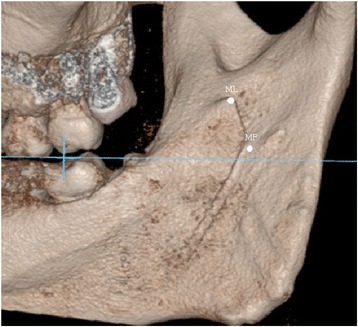
Both of the ML and MF above the occlusal plane; ML in front of MF. The blue line indicates the occlusal plane
Fig. 4.
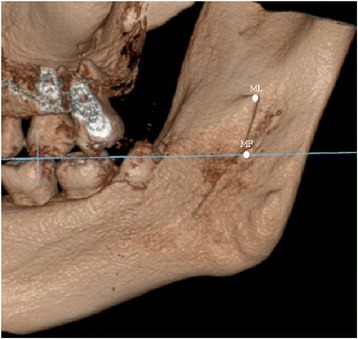
ML above the occlusal plane; MF at the level of occlusal plane. The blue line indicates the occlusal plane
Fig. 5.

ML at the level of occlusal plane; MF below the occlusal plane; MF in front of ML. The blue line indicates the occlusal plane
Table 3.
Relationship of mandibular lingula to occlusal plane
| Sex | Above | Equal | Below | Total | |||
|---|---|---|---|---|---|---|---|
| No. | Mean ± SD (mm) | No. | No. | Mean ± SD (mm) | No. | Mean ± SD (mm) | |
| Male | 58 | 6.2 ± 2.8 | 0 | 0 | 0 | 58 | 6.2 ± 2.8 |
| Female | 61 | 5.8 ± 2.9 | 1 | 1 | -1.9 | 63 | 5.6 ± 3.1 |
| Total | 119 (98.3%) | 6.0 ± 2.9 | 1 (0.8%) | 1 (0.8%) | -1.9 | 121 (100%) | 5.9 ± 3.0 |
Abbreviations: No., number of sides; MD, mean distance from mandibular lingula to occlusal plane
With regard to the MF, it was found that 84.3% of the foramina were inferior to the occlusal plane with a mean distance of 4.5 ± 2.6 mm (Fig. 5); 12.4% were located 2.5 ± 2.3 mm above the occlusal plane (Fig. 3); and only 3.3% were equal with the occlusal plane (Fig. 4; Table 4).
Table 4.
Relationship of mandibular foramen to occlusal plane
| Sex | Above | Equal | Below | Total | |||
|---|---|---|---|---|---|---|---|
| No. | Mean ± SD (mm) | No. | No. | Mean ± SD (mm) | No. | Mean ± SD (mm) | |
| Male | 5 | 3.5 ± 3.4 | 3 | 50 | -4.2 ± 2.3 | 58 | -3.2 ± 3.3 |
| Female | 10 | 2.1 ± 1.6 | 1 | 52 | -4.8 ± 2.9 | 63 | -3.6 ± 3.7 |
| Total | 15 (12.4%) | 2.5 ± 2.3 | 4 (3.3%) | 102 (84.3%) | -4.5 ± 2.6 | 121 (100%) | -3.4 ± 3.5 |
Abbreviations: No., number of sides; MD, mean distance from mandibular lingula to occlusal plane
The anteroposterior relationship of the ML and MF on the occlusal plane was evaluated, too. The MF was primarily located 2.6 ± 1.7 mm in front of the ML (75.2%; Fig. 5), although sometimes it was located 1.4 ± 0.7 mm behind the ML (17.4%; Fig. 3); the line connecting the MF and ML was rarely perpendicular to the occlusal plane (7.4%; Table 5).
Table 5.
Anteroposterior relationship of ML and MF on occlusal plane
| Sex | MF in front of ML | Line connecting MF and ML perpendicular to OP | ML in front of MF | ||
|---|---|---|---|---|---|
| No. | Mean ± SD (mm) | No. | No. | Mean ± SD (mm) | |
| Male | 46 | 2.5 ± 1.8 | 2 | 10 | 1.6 ± 0.5 |
| Female | 45 | 2.7 ± 1.6 | 7 | 11 | 1.2 ± 0.8 |
| Total | 91 (75.2%) | 2.6 ± 1.7 | 9 (7.4%) | 21 (17.4%) | 1.4 ± 0.7 |
Abbreviations: ML, mandibular lingula; MF, mandibular foreman; OP, occlusal plane; No., number of sides; MD, mean distance from ML to MF on OP
Discussion
During the procedures of block anesthesia of IAN and orthognathic surgery, it is important to locate the ML and MF accurately. Nevertheless, there is still some disagreement in the anatomical description of the mandibular ramus, especially in relation to the ML and MF. Thus far, the available anatomical data on the mandibular ramus has mostly been based on the measurements of dry human skulls. In most cases, however, dry human skulls cannot adequately provide the data on sex, age, or race due to lack of information [6]. This study mainly included patients 20 to 30 years of age. However, most of the patients undergoing third molar extraction and orthognathic surgery are around 20 to 30 years of age, it is likely that this age distribution is meaningful.
CBCT, in contrast to conventional CT, offers higher resolution with lower radiation exposure [10–15]. The accuracy of 3D measurement is influenced by the slice thickness and voxel size. The slice thickness of the CBCT used in this study was 0.2 mm and the voxel size was 0.2 mm. Therefore, the accuracy of the 3D images reconstructed in this study can be considered acceptable.
In cosmetic surgery, the mandibular angle is identified as an important indicator in the evaluation of the shape of the face [24]. In an earlier study, Hetson et al. [25] measured the mandibular angle on 317 hemisected dried human mandibles using a precisely designed photographic technology and found the mean mandibular angle to be 123°. After measuring 60 panoramic radiographs, Pirgousis et al. [26] reported that the mean mandibular angle was 123.6° in females and 123.43° in males with no significant difference between the genders. This corroborates the result of the present study. Depending on our study conducted on young Koreans, mean mandibular angle was 125.1° in females and 124.1° in males. The distances of the ML from the mandibular second molar, lower border of the mandible, and the angle of the mandible were found to be statistically greater in males than in females. However, we did not find statistically significant differences between males and females in relation to the distance of the ML from the sigmoid notch. It can therefore be concluded that the segment of the mandibular ramus below the ML may be bigger in males than in females.
As a surgical reference point in orthognathic surgery, prior to performing the medial horizontal osteotomy, the ML must be located in order to maintain a safe distance of at least 5 mm from the MF [27]. The positions of ML and MF have been reported in many studies; however, the results are variable. After measuring the panoramic radiographs of 73 Thai adult mandibles, Kositbowornchai et al. [9] found that the ML was located posterior to the center of the width of the ramus and the MF was much closer to the sigmoid notch than to the lower border of mandible. Nicholson [28] measured 80 dry adult mandibles of East Indian ethnic origin and reported that the foramen was exactly halfway between the mandibular notch and the inferior border of mandible in the upper third of the line connecting the coronoid process with gonion. In this study, it was found that the ML was located at the center of the width of the ramus in males and slightly posterior to the center of the ramus in females. In the vertical direction, the ML was found at the junction of the upper one third and lower two thirds of the line joining the lower border of the ramus and the sigmoid notch. The mean distance of ML to the occlusal plane was 5.9 mm above the occlusal plane, which could be a valuable indicator for locating the ML during orthognathic surgery. The present study indicated that 75.2% of the foramina were located in the front of the ML when the occlusal plane was set as the reference plane. However, in a previous study, Hayward et al. [29] reported the MF was located just posterior to the ML. This difference can probably be explained by the different reference points and planes used during the measurement procedure. Also, we measured distance from ML to Go. In our study, mean distance was 28.9 mm in females and 33.8 mm in males. Above information could help approximatively estimate inferior alveolar nerve position in orthognathic surgery on gonion area such as mandibular angle reduction.
If the relationship between MF and occlusal plane can be confirmed, it will be much easier to achieve successful IAN block anesthesia. Nicholson [28] reported that 75% of the foramina were below the occlusal plane and 22.5% of them leveled with the occlusal plane. After studying 38 dry mandibles of adult black Zimbabweans, Mbajiorgu [30] found that 47.1% of the foramina leveled with the occlusal plane and 29.4% were above the occlusal plane. In the present study, we found that 84.3% of the foramina were 4.5 mm below the occlusal plane. In contrast, Kositbowornchai et al. [9] found that the MF was 10 mm above the occlusal plane in their study using panoramic radiographs. Since there is a great degree of variability regarding the position of the MF, it is difficult to define the accurate needling position and depth during the IAN block.
Conclusion
Depending on our study, we found that 84.3% of the mandibular foramina were 4.5 mm below the occlusal plane. Also, the mean distance of mandibular lingula to the occlusal plane was 5.9 mm above the occlusal plane. Above information as anatomical indications may be helpful for block anesthesia of inferior alveolar nerve (IAN) and orthognathic surgery.
Acknowledgements
None declared.
Funding
This work was supported by the Basic Science Research Program through the National Research Foundation funded by the Ministry of Education (NRF-2013R1A1A1065373),
This work was supported by Korea Health Technology R&D Project through the Korea Health Industry Development Institute, funded by the Ministry of Health & Welfare, Republic of Korea (HI15C3136).
Availability of data and materials
The datasets supporting the conclusions of this article are available in the Open Science Framework.
Repository https://osf.io/t8gk9/.
Authors’ contributions
Each author took part in the design of the study, the clinical data collection, writing the manuscript and all agreed with the accuracy of the content of the paper. This work has not been published elsewhere in any form and any language. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Approved by Korea University Anam Hospital in Seoul, South Korea: AN14291-001.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Cong Zhou and Tae-Hyun Jeon contributed equally to this work.
Contributor Information
Cong Zhou, Phone: +15098776833, Email: zhoucong@sdu.edu.cn.
Tae-Hyun Jeon, Phone: +82 2 920 5423, Email: zalkka@hanmail.net.
Sang-Ho Jun, Phone: +82 2 920 6776, Email: Omfs.junsang@gmail.com.
References
- 1.Goldberg S, Reader A, Drum M, Nusstein J, Beck M. Comparison of the anesthetic efficacy of the conventional inferior alveolar, Gow-Gates, and Vazirani-Akinosi techniques. J Endod. 2008;34:1306–1311. doi: 10.1016/j.joen.2008.07.025. [DOI] [PubMed] [Google Scholar]
- 2.Ezoddini Ardakani F, Bahrololoumi Z, Zangouie Booshehri M, Navab Azam A, Ayatollahi F. The position of lingula as an index for inferior alveolar nerve block injection in 7-11-year-old children. J Dent Res Dent Clin Dent Prospects. 2010;4(2):47–51. doi: 10.5681/joddd.2010.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cvetko E. Bilateral anomalous high position of the mandibular foramen: a case report. Surg Radiol Anat. 2014;36(6):613–616. doi: 10.1007/s00276-013-1209-y. [DOI] [PubMed] [Google Scholar]
- 4.Archer WH. Oral and maxillofacial surgery. Philadelphia: WB Saunders; 1975. pp. 1448–1449. [Google Scholar]
- 5.Monnazzi MS, Passeri LA, Gabrielli MF, Bolini PD, de Carvalho WR, da Costa Machado H. Anatomic study of the mandibular foramen, lingula and antilingula in dry mandibles, and its statistical relationship between the true lingula and the antilingula. Int J Oral Maxillofac Surg. 2012;41(1):74–78. doi: 10.1016/j.ijom.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 6.Yu IH, Wong YK. Evaluation of mandibular anatomy related to sagittal split ramus osteotomy using 3-dimensional computed tomography scan images. Int J Oral Maxillofac Surg. 2008;37(6):521–528. doi: 10.1016/j.ijom.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Noleto JW, Marchiori E, Da Silveira HM. Evaluation of mandibular ramus morphology using computed tomography in patients with mandibular prognathism and retrognathia: relevance to the sagittal split ramus osteotomy. J Oral Maxillofac Surg. 2010;68(8):1788–1794. doi: 10.1016/j.joms.2009.12.028. [DOI] [PubMed] [Google Scholar]
- 8.Smith BR, Rajchel JL, Waite DE, Read L. Mandibular ramus anatomy as it relates to the medial osteotomy of the sagittal split ramus osteotomy. J Oral Maxillofac Surg. 1991;49(2):112–116. doi: 10.1016/0278-2391(91)90095-4. [DOI] [PubMed] [Google Scholar]
- 9.Kositbowornchai S, Siritapetawee M, Damrongrungruang T, Khongkankong W, Chatrchaiwiwatana S, Khamanarong K, Chanthaooplee T. Shape of the lingula and its localization by panoramic radiograph versus dry mandibular measurement. Surg Radiol Anat. 2007;29(8):689–694. doi: 10.1007/s00276-007-0270-9. [DOI] [PubMed] [Google Scholar]
- 10.Clark DE, Danforth RA, Barnes RW, Burtch ML. Radiation absorbed from dental implant radiography: a comparison of linear tomography, CT scan, and panoramic and intra-oral techniques. J Oral Implantol. 1990;16(3):156–164. [PubMed] [Google Scholar]
- 11.Mish CE (2007) Contemporary implant dentistry, 3rd edn. Publisher: Elsevier Health Sciences, pp 38–67
- 12.Kau CH, Richmond S, Palomo JM, Hans MG. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32(4):282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 13.Razavi T, Palmer RM, Davies J, Wilson R, Palmer PJ. Accuracy of measuring the cortical bone thickness adjacent to dental implants using cone beam computed tomography. Clin Oral Implants Res. 2010;21(7):718–725. doi: 10.1111/j.1600-0501.2009.01905.x. [DOI] [PubMed] [Google Scholar]
- 14.Ozaki Y, Watanabe H, Nomura Y, Honda E, Sumi Y, Kurabayashi T. Location dependency of the spatial resolution of cone beam computed tomography for dental use. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116(5):648–655. doi: 10.1016/j.oooo.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 15.Jun SH, Kim CH, Ahn JS, Padwa BL, Kwon JJ. Anatomical differences in lower third molars visualized by 2D and 3D X-ray imaging: clinical outcomes after extraction. Int J Oral Maxillofac Surg. 2013;42(4):489–496. doi: 10.1016/j.ijom.2012.12.005. [DOI] [PubMed] [Google Scholar]
- 16.Matherne RP, Angelopoulos C, Kulild JC, Tira D. Use of cone-beam computed tomography to identify root canal systems in vitro. J Endod. 2008;34(1):87–89. doi: 10.1016/j.joen.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 17.De Vos W, Casselman J, Swennen GR. Cone-beam computerized tomography (CBCT) imaging of the oral and maxillofacial region: a systematic review of the literature. Int J Oral Maxillofac Surg. 2009;38(6):609–625. doi: 10.1016/j.ijom.2009.02.028. [DOI] [PubMed] [Google Scholar]
- 18.Hatcher DC. Cone beam computed tomography: craniofacial and airway analysis. Dent Clin N Am. 2012;56(2):343–357. doi: 10.1016/j.cden.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 19.Shin HS, Hwang SJ. Study on the relationship of the inferior alveolar nerve position between buccal and lingual side using CT and orthpantomogram. J Korean Assoc Oral Maxillofac Surg. 2002;28(1):1–6. [Google Scholar]
- 20.Yun SH, Park JY, Ko YK, Park JU, Pyo SW. Cone-beam computed tomography measurement of the position of the inferior alveolar Nerve Canal in Mandibular Prognathism. J Korean Assoc Oral Maxillofac Surg. 2009;35(1):26–30. [Google Scholar]
- 21.Kim HW, Kwon KH, Min SK, Oh SH, Chee YD, Koh SW, Ohn BH. The study on course of the inferior Alveolar Canal in the Mandibular Ramus using Conebeam CT. J Korean Assoc Maxillofac Plast Reconstr Surg. 2009;31(5):386–393. [Google Scholar]
- 22.Kim JK, Gu H, An JS, Kook MS, Park HJ, Oh HK, Cho JH. The study by using the computerized tomography imaging in order to access to mandibular foramen while inferior alveolar nerve anesthesia. J Korean Assoc Oral Maxillofac Surg. 2006;32(6):566–574. [Google Scholar]
- 23.Kim HG, Yoon JH. A study of the anteroposterior positional and radiographical measurement of the mandibular foramen of the Korean adult. J Korean Assoc Oral Maxillofac Surg. 1982;8(1):137–145. [Google Scholar]
- 24.Cho IG, Chung JY, Lee JW, Yang JD, Chung HY, Cho BC, Choi KY. Anatomical study of the mandibular angle and body in wide mandibular angle cases. Aesthet Plast Surg. 2014;38(5):933–940. doi: 10.1007/s00266-014-0370-y. [DOI] [PubMed] [Google Scholar]
- 25.Hetson G, Share J, Frommer J, Kronman JH. Statistical evaluation of the position of the mandibular foramen. Oral Surg Oral Med Oral Pathol. 1988;65(1):32–34. doi: 10.1016/0030-4220(88)90187-9. [DOI] [PubMed] [Google Scholar]
- 26.Pirgousis P, Brown D, Fernandes R. Digital measurements of 120 mandibular angles to determine the ideal fibula wedge osteotomy to re-create the mandibular angle for microvascular reconstruction. J Oral Maxillofac Surg. 2013;71(12):2169–2175. doi: 10.1016/j.joms.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 27.Muto T, Shigeo K, Yamamoto K, Kawakami J. Computed tomography morphology of the mandibular ramus in prognathism: effect on the medial osteotomy of the sagittal split ramus osteotomy. J Oral Maxillofac Surg. 2003;61(1):89–93. doi: 10.1053/joms.2003.50014. [DOI] [PubMed] [Google Scholar]
- 28.Nicholson ML. A study of the position of the mandibular foramen in the adult human mandible. Anat Rec. 1985;212(1):110–112. doi: 10.1002/ar.1092120116. [DOI] [PubMed] [Google Scholar]
- 29.Hayward J, Richardson ER, Malhotra SK. The mandibular foramen: its anteroposterior position. Oral Surg Oral Med Oral Pathol. 1977;44(6):837–843. doi: 10.1016/0030-4220(77)90027-5. [DOI] [PubMed] [Google Scholar]
- 30.Mbajiorgu EF. A study of the position of the mandibular foramen in adult black Zimbabwean mandibles. Cent Afr J Med. 2000;46(7):184–190. doi: 10.4314/cajm.v46i7.8554. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are available in the Open Science Framework.
Repository https://osf.io/t8gk9/.


