Highlights
-
•
Rectovaginal fistula (RVF) is one of the complications after low anterior resection for rectal cancer.
-
•
RVF has been considered to be refractory to conservative treatment.
-
•
We report a case of RVF in which conservative treatment was successful.
Abbreviations: RVF, rectovaginal fistula; FXIII, freeze-dried coagulation factor XIII
Keywords: Rectovaginal fistula, Low anterior resection, Double-stapling technique
Abstract
Background
Rectovaginal fistula (RVF) is a serious complication after colorectal anastomosis using a double-stapling technique. RVF following this procedure has been considered to be refractory to conservative treatment.
Case presentation
A 75-year-old woman who underwent laparoscopy-assisted low anterior resection for early rectal cancer developed RVF on the 12th postoperative day. Conservative treatment was chosen and was successful. She was discharged from the hospital after 3 weeks with a normal oral diet. Colonoscopy on the 50th postoperative day showed that the RVF was closed.
Conclusion
Conservative treatment may be effective for RVF after colorectal anastomosis using a double-stapling technique when there is no evidence of defecation through the vagina.
1. Introduction
Colorectal anastomosis using a double-stapling technique has become a common procedure in low anterior resection for rectal cancer [1], [2]. Rectovaginal fistula (RVF) is a serious complication of this method, with reported incidence of 1.6%–9.9% [3], [4], [5], [6]. Management of RVF is difficult and conservative treatment has been considered to be ineffective [7], [8]. Fecal diversion is generally recommended as the initial step to facilitate resolution of acute inflammation and associated infection [8], while additional surgical procedures, such as closure of the fistula or muscle flap repair, often are required, though outcomes are not always satisfactory [9], [10], [11], [12]. Thus far, successful conservative treatment has been reported in only one case of a pinhole fistula [13].
Here, we report a case of a relatively large RVF after low anterior resection for rectal cancer using a double-stapling technique, in which conservative treatment was successful. This work has been reported in line with the SCARE criteria [14].
2. Case report
A 75-year-old woman was admitted to our hospital with bloody feces, and was diagnosed as having rectal cancer by colonoscopy. She had no particular past history, no family history, or no medication. A quarter-circular, type 1 tumor was found on the anterior wall of the lower rectum, with its lower edge approximately 6 cm from the anal verge. Laparoscopy-assisted low anterior resection with D3 lymph node dissection was performed. Intraoperatively, bleeding from the posterior wall of the vagina was insistent, with total blood loss of 630 g. After total mesorectal excision, the rectal stump was closed at 2 cm below the cancer using two 45-mm cartridges of a linear stapler. Anastomosis was performed with a circular stapler using a double-stapling technique. Pathologic stage was confirmed to be pT1b (SM, 4.5 mm), pN0, pPM0 (150 mm), pDM0 (5 mm), pStage I.
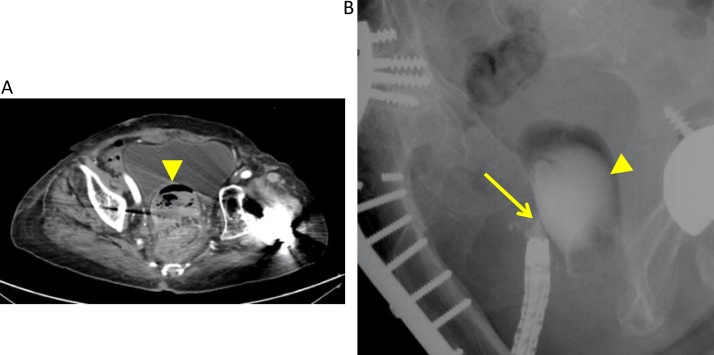
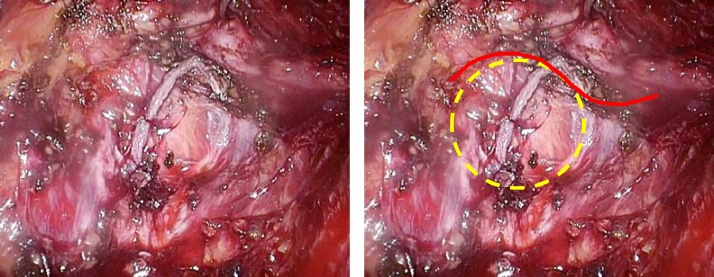
Oral diet was started on the third postoperative day, and discharge from the hospital was planned for the 12th postoperative day. However, massive fresh bleeding from the anus and vagina was observed on the day of discharge. Computed tomography showed air and coagulate in the vagina and no air in the peritoneal cavity (Fig. 1A). Enema using amidotrizoate sodium meglumine confirmed RVF formation (Fig. 1B). Colonoscopy showed the anastomosis at 4 cm from the anal verge and RVF formation between the anterior wall of the anastomotic ring and the posterior wall of the vagina. The diameter of the fistula was over 1 cm, and a thin scope (10.2 mm in diameter) could pass through it (Fig. 2A). Gynecologists examined the vagina and confirmed the fistula was located on the posterior to right wall of the upper vagina. Retrospective inspection of our operative video revealed that the linear stapler might have slightly included the vaginal wall (Fig. 3).
Fig. 1.
Rectovaginal fistula was diagnosed by computed tomography (A) and contrast enema (B). The triangles show the vagina, and the arrow shows rectovaginal fistula.
Fig. 2.
Colonoscopy images, showing rectovaginal fistula on the 12th (A) and 20th (B) postoperative days. It was closed on the 50th postoperative day (C). The arrows show the fistula (A, B) or its scar (C).
Fig. 3.
Operative video still frames, suggesting the linear stapler might have included the vaginal wall. The red line is the border between the rectum and vagina, while the yellow line is the suspected line that the blade of the circular stapler might have punched.
We chose conservative treatment because the bleeding stopped and vital signs were stable. Oral intake was stopped and total parenteral nutrition was started on the same day. Freeze-dried coagulation factor XIII (FXIII), derived from human plasma, was administered for 5 days (1440 U/day) because FXIII activity decreased to 66%. Oral intake was restarted on the 20th postoperative day after we confirmed by colonoscopy that the RVF decreased in size (Fig. 2B). Magnesium oxide and antiflatulent were administered so that soft defecation was observed 2 or 3 times a day. We judged that she could be discharged from the hospital on the 34th postoperative day because no fever or inflammatory response was observed, and there was no evidence of defecation from the vagina. Colonoscopy on the 50th postoperative day showed that the RVF was closed (Fig. 2C). No recurrence has been observed for 4 months.
3. Discussion
Low anterior resection with anastomosis using a double-stapling technique for rectal cancer is widely performed. Recently, advances in laparoscopic techniques have made it possible to apply a double-stapling technique even for very low rectal anastomosis.
As for etiology, RVF has been thought to arise from inclusion of the vagina in the stapled anastomosis, spontaneous drainage of a pelvic abscess through the vagina, or injury of the vagina by the “dog ear” of the rectal stump [7]. In our case, the linear stapler might have slightly included the vaginal wall and we infer that the circular stapler might have punched just the edge of the included vaginal wall, and the point of intersection of the staples might have popped out on the 12th postoperative day, resulting in the sudden bleeding and RVF formation.
RVF following anastomosis using a double-stapling technique has been considered to be refractory to conservative treatment [3], [4], [5], [6], [7], [8]. Thus, various surgical procedures, such as transvaginal or transanal resection or closure of the fistula, repair with a gracilis muscle flap, and diverting stoma for local preservation, have been reported [9], [10], [11].
In our case, the RVF closed without any surgical procedure, even though it was so large a thin scope could pass through it. There may be several reasons for this successful conservative treatment. First, there was no evidence of defecation through the vagina throughout the course. Second, good nutritional status was maintained because total parenteral nutrition was started immediately and the fasting period was only 8 days. Administration of FXIII also might have helped to heal the fistula. FXIII is a transglutaminase that is the last step in the coagulation cascade, which plays an important role in wound healing by stabilizing the fibrin clot [15]. Thus, administration of FXIII might accelerate wound healing by increasing circulating growth factors [16].
Although RVF following anastomosis using a double-stapling technique has been thought to be refractory to conservative treatment, our case may indicate that conservative treatment can be attempted when there is no evidence of defecation through the vagina.
Conflicts of interest
The authors declare that they have no competing interests.
Funding
None.
Ethical approval
Treatments for the patient were in accordance with the ethical standards of the responsible committees on human experimentation (institution and national).
Consent
Written informed consent to publish was obtained from the patient.
Author contribution
SE, SY and MI carried out the diagnosis of the tumor, and carried out the surgery of this patient. SE, SY, KO, TN, KM, HS, YT, AH, HS and MI participated in the patient’s care. SE and NA participated in writing and revising the manuscript critically. All authors read and approved the final manuscript.
Guarantor
Shigenobu Emoto and Toshiaki Watanabe.
References
- 1.Knight C.D., Griffen F.D. An improved technique for low anterior resection of the rectum using the EEA stapler. Surgery. 1980;88(5):710–714. [PubMed] [Google Scholar]
- 2.Baran J.J., Goldstein S.D., Resnik A.M. The double-staple technique in colorectal anastomoses: a critical review. Am. Surg. 1992;58(4):270–272. [PubMed] [Google Scholar]
- 3.Watanabe J., Ota M., Kawaguchi D., Shima H., Kaida S., Osada S., Kamimukai N., Kamiya N., Ishibe A., Watanabe K. Incidence and risk factors for rectovaginal fistula after low anterior resection for rectal cancer. Int. J. Colorectal Dis. 2015;30(12):1659–1666. doi: 10.1007/s00384-015-2340-5. [DOI] [PubMed] [Google Scholar]
- 4.Matthiessen P., Hansson L., Sjodahl R., Rutegard J. Anastomotic-vaginal fistula (AVF) after anterior resection of the rectum for cancer–occurrence and risk factors. Colorectal Dis. 2010;12(4):351–357. doi: 10.1111/j.1463-1318.2009.01798.x. [DOI] [PubMed] [Google Scholar]
- 5.Zheng H., Guo T., Wu Y., Li C., Cai S., Liu F., Xu Y. Rectovaginal fistula after low anterior resection in Chinese patients with colorectal cancer. Oncotarget. 2017 doi: 10.18632/oncotarget.17046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kosugi C., Saito N., Kimata Y., Ono M., Sugito M., Ito M., Sato K., Koda K., Miyazaki M. Rectovaginal fistulas after rectal cancer surgery: incidence and operative repair by gluteal-fold flap repair. Surgery. 2005;137(3):329–336. doi: 10.1016/j.surg.2004.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Rex J.C., Jr., Khubchandani I.T. Rectovaginal fistula: complication of low anterior resection. Dis. Colon Rectum. 1992;35(4):354–356. doi: 10.1007/BF02048113. [DOI] [PubMed] [Google Scholar]
- 8.Vogel J.D., Johnson E.K., Morris A.M., Paquette I.M., Saclarides T.J., Feingold D.L., Steele S.R. Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis. Colon Rectum. 2016;59(12):1117–1133. doi: 10.1097/DCR.0000000000000733. [DOI] [PubMed] [Google Scholar]
- 9.Nakagoe T., Sawai T., Tuji T., Nanashima A., Yamaguchi H., Yasutake T., Ayabe Y. Successful transvaginal repair of a rectovaginal fistula developing after double-stapled anastomosis in low anterior resection: report of four cases. Surg. Today. 1999;29(5):443–445. doi: 10.1007/BF02483037. [DOI] [PubMed] [Google Scholar]
- 10.Yodonawa S., Ogawa I., Yoshida S., Ito H., Kobayashi K., Kubokawa R. Rectovaginal fistula after low anterior resection for rectal cancer using a double stapling technique. Case Rep. Gastroenterol. 2010;4(2):224–228. doi: 10.1159/000318745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takagi C., Baba H., Yamafuji K., Asami A., Takeshima K., Okamoto N., Takahashi H., Kubochi K. Simultaneously diagnosed and successfully treated rectovaginal and vesicovaginal fistulae after low anterior resection with concomitant resection of female genitalia. Case Rep. Gastroenterol. 2017;11(1):17–22. doi: 10.1159/000455187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottgens K.W., Smeets R.R., Stassen L.P., Beets G., Breukink S.O. The disappointing quality of published studies on operative techniques for rectovaginal fistulas: a blueprint for a prospective multi-institutional study. Dis. Colon Rectum. 2014;57(7):888–898. doi: 10.1097/DCR.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 13.Tsutsumi N., Yoshida Y., Maehara Y., Kohnoe S. Rectovaginal fistula following double-stapling anastomosis in low anterior resection for rectal cancer. Hepatogastroenterology. 2007;54(78):1682–1683. [PubMed] [Google Scholar]
- 14.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P., Group S. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 15.Saigusa S., Yamamura T., Tanaka K., Ohi M., Kawamoto A., Kobayashi M., Inoue Y., Kusunoki M. Efficacy of administration of coagulation factor XIII with definitive surgery for multiple intractable enterocutaneous fistulae in a patient with decreased factor XIII activity. BMJ Case Rep. 2011;2011 doi: 10.1136/bcr.09.2010.3342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inbal A., Dardik R. Role of coagulation factor XIII (FXIII) in angiogenesis and tissue repair. Pathophysiol. Haemost. Thromb. 2006;35(1–2):162–165. doi: 10.1159/000093562. [DOI] [PubMed] [Google Scholar]