Abstract
Objective: Indigenous people's ceremonies using rhythm and dance have been used for countless generations throughout the world for healing, conflict resolution, social bonding, and spiritual experience. A previous study reported that a ceremony based on the Central African ngoma tradition was favorably received by a group of Americans. The present trial compared the effects of the modified ngoma ceremony (Ngoma) with those of mindfulness-based stress reduction (MBSR) in a randomized pilot study.
Methods: Twenty-one women were randomized to either Ngoma or MBSR. Both groups had sessions on a weekly basis for 8 weeks and completed questionnaires at baseline, week 8, and 1 month after the intervention. Participants completed questionnaires, which included self-report of depressive and anxiety symptoms, health status (e.g., quality of life and functioning), social bonding, and perception of the credibility of the two interventions.
Results: Both groups showed improvements in depression, anxiety, emotional well being, and social functioning as measured by respective scales. Social bonding also increased in both groups during the study and may be a mechanism for both interventions. Participants found both interventions credible.
Conclusions: In this pilot study, Ngoma showed significant and durable beneficial effects comparable to MBSR. The effects of Ngoma and other indigenous rhythm-dance ceremonies on distress and health status in western culture should be investigated in larger clinical studies.
Keywords: : mindfulness, stress–psychological, indigenous medicine, depression, anxiety
Introduction
Stress reduction around the world takes many forms. American culture often takes the approach of diverting the attention away from stressors, an approach commonly referred to as experiential avoidance1; this often occurs through various forms of entertainment. Another western approach commonly includes various forms of psychotherapy or pharmacotherapy in the form of antidepressants, anxiolytic agents, and medications used to assist in sleep. In the past three decades, investigators have shown the effectiveness of programs using meditation adapted from eastern religions.2–4 In the distant past, however, most humans probably engaged in rituals involving drum and dance to reduce stress.5 Indeed, this approach is still used by most indigenous cultural groups around the world. It shares with meditation an alteration of consciousness to focus on the mind and body of the present moment and in doing so to gain understanding from a large and dispassionate perspective.
The authors recently reported a study done to test the acceptability and appropriateness of a modified ngoma ceremony in a group of individuals who lived in the southeastern United States.6 Ngoma is a broad tradition involving rhythms, generally with drums, and dance; it is practiced throughout Central and Southern Africa. People come together, usually with a spiritual leader, for social support, to address difficult issues, to support psychodynamic growth and to heal body and mind.7,8 In our previous study, which involved participating in the ceremony once, almost every member of a group of 17 women reported a positive experience. In a focus group discussion, participants reported feeling more energetic as well as being more calm and relaxed than before participation. They also reported decreased anxiety, stress reduction, and feelings of social support. Based on these results, the authors moved forward with the current pilot study to compare the effects of the modified ngoma ceremony with standard mindfulness-based stress reduction (MBSR). MBSR was chosen because it is the most studied and best established method that uses meditation practice for stress reduction.
Materials and Methods
Participants
This study was approved by the Duke University Office of Research Support Institutional Review Board (IRB). All participants went through an IRB approved informed consent process. Subjects between the ages of 25 and 60 years were recruited through posters and advertisements in written periodicals as well as by word of mouth. The only exclusion criterion was inability to exercise at a moderate level for 1.25 h with breaks. Participants were assigned randomly with a computer algorithm to treatment groups.
Interventions
The ngoma ceremony (Ngoma) has been described previously.6 It was designed by two members of our group (P.M. and M.B.), who are from Republic of the Congo, working together with the first author (A.L.V.), who is a Lucumí priest. Ms. Baegne is in a direct family lineage of nganga or healer. Mr. Mounzeo is an expert in the musical form involved. In brief, participants were invited to focus on the activity at hand by performing 10 min of a meditative practice of their choosing such as mindfulness meditation, prayer, qigong, or yoga. The authors' goal was to drop the requirement for a particular belief system, yet, leave the experience open to a feeling of reverence or spirituality. The facilitator was dressed in traditional white Lucumí attire and performed ritual cleansing of the space and the drummers during the 10 min of quiet time. The purification process and the participants' meditative activity were followed by 1 h and 15 min during which participants danced to drums with a short rest break every 20 min. The drumming consisted of Congolese rhythms performed on ngomas, which are large, sonorous drums covered with goatskin heads. Indeed, the term “ngoma” used widely for healing ceremonies relates to the ngoma drum as used in western Congo, where “ngo” is a Kikongo word “strength of the panther” and “ma” means “to give.” No more than four dance steps were introduced in any session. The ceremony required only moderate effort as defined in the 2008 Physical Activities Guidelines for Americans. After the dancing, subjects discussed for 20 min their experience and how it interfaced with their daily lives. This intervention was repeated on a weekly basis for 8 weeks.
The MBSR intervention followed the standard format used by Duke Integrative Medicine (www.dukeintegrativemedicine.org/programs-training/public/mindfulness-based-stress-reduction). In brief, the group participated in an 8-week training to learn various mindfulness-based techniques for more balance and ease in their lives. Each session lasted for two-and-a-half hours and included instruction and practice on different meditation techniques, mindful walking, gentle yoga, relaxation, mindful speaking and listening, and group dialogue to enhance understanding of the practices. In addition, the course included a 6-h day of mindfulness for an opportunity to experience a longer meditation practice. Throughout the course, the participants were encouraged to investigate their own reactive patterns related to stress and taught how to develop alternative responses to challenging circumstances. A key component of the course was guidance in developing one's own meditation practice and as such it included individually tailored instruction.
Questionnaires and statistical analysis
Before starting activities on the first day, after the sessions on week 8, and 1 month after the last session, participants filled out the following questionnaires: The Center for Epidemiological Studies Depression Scale-Revised (CESD),9 Depression Anxiety Stress Scales (DASS),10 Standard Form 36 (SF-36),11 and Group Cohesion Scale.12 Depression and anxiety scales were chosen because they have been consistently shown to improve with MBSR.2,3 The SF-36 is a measure of the perception of one's own health. The group cohesion scale13 was included because the ngoma tradition in Africa stresses group cohesion. The Credibility Scale was administered before starting activities on day 1 to determine if there was equipoise among the participants in the two intervention groups.
To examine treatment effects on the above measures, the authors modeled baseline, posttreatment, and 1-month follow-up scores using multilevel modeling (MLM). MLM is analogous to repeated-measures analysis of variance (ANOVA) and thus appropriate for analyzing repeated-measures data. However, unlike ANOVA, MLM uses all available data and can accommodate unbalanced variances and data missing at random.14 As such, MLM provides more robust estimates of longitudinal effects than repeated-measures ANOVA.
Specifically, we examined 2 (treatment group) × 3 (time of measurement) models for each of the following outcomes: CESD total score, DASS total score, Cohesion Scale score, SF-36 Emotional Well-Being score, and the SF-36 Social Functioning score. Analyses were conducted using PROC MIXED, available with SAS 9.4.
Results
Participants
Forty-four people responded to recruitment materials, of whom 3 were male and the remaining 41 were female. One person did not meet age criteria and was therefore not enrolled in the study. Eighteen screened in for the study but chose not to participate, mostly either because of personal logistical problems or because they did not want to participate in a study that did not pay them. Twenty-five women ages 31–59 years signed informed consent and four withdrew before the start of the study. Of the remaining 21 women, 11 women participated in the Ngoma group and 10 participated in the MBSR group. As shown in Table 1, in terms of age, ethnicity, religious affiliation, and gender, the groups were comparable.
Table 1.
Descriptive Analysis of Demographics (N = 21)
| Characteristics | Mean (SD)/N (%) | ||
|---|---|---|---|
| Total | Ngoma (N = 11) | MBSR (N = 10) | |
| Age | 47.86 (8.1) | 49.1 (7.9) | 46.5 (8.8) |
| Gender | |||
| Female | 21 (100.00%) | 11 | 10 |
| Ethnicity | |||
| African American | 10 (47.62%) | 6 (55%) | 4 (40%) |
| White | 9 (42.86%) | 5 (45.5%) | 4 (40%) |
| Asian | 1 (4.76%) | 0 | 1 (10%) |
| Hispanic | 1 (4.76%) | 0 | 1 (10%) |
| Religion | |||
| Christian | 6 (55%) | 6 (60%) | |
| Mystic | 1 (9%) | 0 | |
| Pagana | 1 (9%) | 0 | |
| None or N/A | 4 (36%) | 4 (40%) | |
| Otherb | 0 | 1 (10%) | |
One person claimed paganism and Christianity.
One person claimed “many religions” and Christianity.
MBSR, mindfulness-based stress reduction; N/A, not applicable; SD, standard deviation.
Missing data
Thirteen participants were missing posttreatment data, and 10 were missing follow-up data. Before modeling treatment effects, the authors examined missing posttreatment and follow-up data to determine whether the distribution of missing data was systematic (i.e., associated with measured baseline characteristics). Missing posttreatment data were not significantly associated with age, t(19) = −0.11, p = 0.91; baseline depression (CESD), t(19) = 1.24, p = 0.23; baseline anxiety (DASS), t(19) = 1.00, p = 0.33; baseline cohesion, t(16) = −1.77, p = 0.096; baseline emotional well being, t(19) = −0.22, p = 0.83; or baseline social functioning, t(19) = −1.66, p = 0.11, although poorer functioning was generally associated with absence of data. Similar results were found for missing follow-up data: age, t(19) = 0.60, p = 0.56; baseline depression, t(19) = 1.64, p = 0.12; baseline anxiety, t(19) = 1.62, p = 0.12; baseline cohesion, t(16) = 0.69, p = 0.50; baseline emotional well being, t(19) = 0.38, p = 0.71; and baseline social functioning, t(19) = 0.87, p = 0.40.
Analysis of questionnaires
According to MLM analyses, Time of Measurement effects on depression were significant, F(2, 15) = 14.84, p < 0.001, but Treatment effects, F(1, 19) = 0.00, p = 0.99, and Treatment X Time of Measurement effects, F(2, 15) = 2.54, p = 0.11, were not. In other words, scores improved over time in both groups, but there was not a difference between the Ngoma and MBSR groups. A similar pattern of findings was evident in the models of anxiety (Time of Measurement, F[2, 15] = 15.39, p < 0.001; Treatment, F[1, 19] = 0.02, p = 0.89; Treatment X Time of Measurement, F[2, 15] = 0.19, p = 0.83), cohesion (Time of Measurement, F[2, 13] = 5.10, p = 0.023; Treatment, F[1, 17] = 0.11, p = 0.74; Treatment X Time of Measurement, F[2, 13] = 0.08, p = 0.93), emotional well being (Time of Measurement, F[2, 15] = 14.16, p < 0.001; Treatment, F[1, 19] = 0.21, p = 0.65; Treatment X Time of Measurement, F[2, 15] = 1.89, p = 0.18), and social functioning (Time of Measurement, F[2, 15] = 5.25, p = 0.019; Treatment, F[1, 19] = 2.88, p = 0.11; Treatment X Time of Measurement, F[2, 15] = 0.75, p = 0.49).
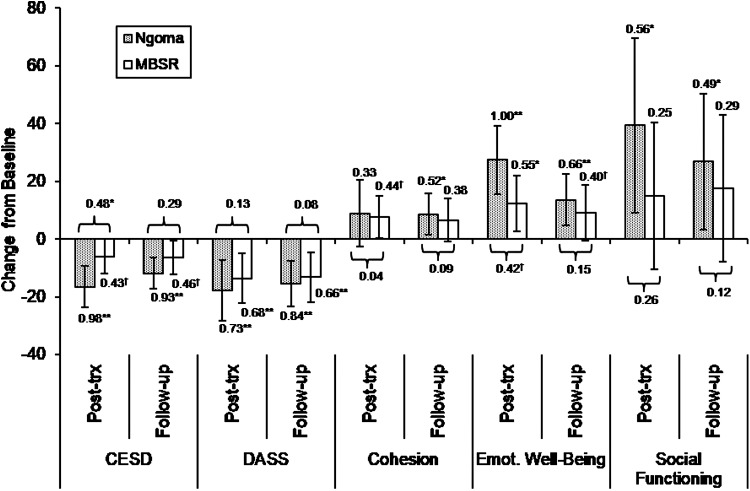
To illustrate treatment-related change in outcomes, Figure 1 depicts the change in each outcome from baseline to posttreatment and follow-up, with negative scores reflecting reductions from baseline levels and positive scores reflecting increases from baseline levels. For both Ngoma and MBSR, there was a robust decrease in depression and anxiety. Group cohesion increased in both groups. Within the SF-36, there were improvements in all scales. Statistical analysis was performed for the most relevant scales for this study—social well being and social functioning, where the changes were robust. Comparing the effect size of Ngoma with that of MBSR showed that there were no significant differences between effect sizes for any of these comparisons except for CESD at posttreatment, in which the effect size for Ngoma was larger (p < 0.05). This difference, although moderate in size, was not sustained at the 1-month follow-up. Other noteworthy, although nonsignificant, contrasts in treatment effects were observed at posttreatment in emotional well being and social functioning, with the Ngoma treatment outperforming MBSR.
FIG. 1.
Modeled effects of Ngoma and MBSR. Error bars reflect 95% confidence intervals. Modeled treatment effect sizes (Cohen's d) are presented for each treatment. Effect sizes contrasting Ngoma and MBSR treatments are depicted beside brackets. †p < 0.10, *p < 0.05, **p < 0.01. CESD, Center for Epidemiological Studies Depression Scale; DASS, Depression Anxiety Stress Scales; MBSR, mindfulness-based stress reduction.
Discussion
This paper presents the results of a pilot study comparing the effects of Ngoma with the better known MBSR program on two markers of stress, on social cohesion, and on emotional well being and social functioning. Ngoma showed significant and durable beneficial effects on all these measures that were not substantially different from those of MBSR, a well-established intervention for stress reduction. It did as well, despite not including a 6-h retreat and thus being a shorter intervention. Although a small pilot study such as this is not definitive, the effect sizes for Ngoma suggest that it is worthy of further study. In Central and Southern Africa, ngoma ceremonies are intentionally used for social cohesion.7,8 The positive effect on social cohesion seen in this study suggests that social support may be at least one mechanism by which both Ngoma and MBSR confer benefits. These results are in keeping with the findings of Hewson et al.,15 who showed that a similar healing ceremony conducted for 6 h was followed by improvement in several quality-of-life measures for up to a month.
Limitations to this study include small sample size, lack of a null control group, lack of an exercise control, and lack of male participants. In addition, although the authors tried to correct for missing data, the incompleteness of the data set still weakens the strength of our conclusions. It would be straightforward to conduct a larger trial with a null control group and controlling for exercise. It may be worthwhile to explore factors related to the underrepresentation of men in the current study as well as in the first qualitative feasibility study. Other limitations include the limited availability of individuals with expertise in leading ngoma ceremonies as well as the limited availability of ngoma drums and drummers. However, as already mentioned, it is likely that these results are generalizable to a variety of forms with similar format.
In adapting an indigenous healing practice to our culture, care should be taken not to misappropriate from another culture. In that spirit, our work represents a collaboration between people with appropriate cultural backgrounds and healthcare professionals. The authors adapted the indigenous cultural practices while trying to respect all cultural traditions involved. If work continues on integrating indigenous healing practices, we hope it is done with veneration for the paradigms and practices concerned and with the understanding involvement of members of the cultures from which non-indigenous people draw.16,17 Cultural sensitivities and expectations vary,16 so the approach must be adapted in each instance for people of a specific culture. These considerations may be especially important when the practice being appropriated involves a spiritual dimension. In that regard, simply having a music therapist/dance therapist to lead dancing to live drumming could be an avenue for future research.
The rationale for studying this kind of intervention is broad. It is widely accepted that ceremonies using rhythm and dance were once universally used for healing, conflict resolution, social bonding, and spiritual experience.5,18 Human beings appear to have engaged in this kind of activity for at least 50,000 years. Thus, this approach is likely to be mediated by a biological pathway for stress reduction and could be quite complementary to western medicine. There are still many existing indigenous traditions with similar ceremonies and benefits seem unlikely to be restricted to the African ngoma tradition and the format used by Hewson et al.15 Thus, further work should explore the potential range of such interventions. These diverse cultural rhythm and dance practices and meditation practice appear to have common roots in the human shamanic experience.5 Both engage what anthropologist Michael Winkelman terms the “integrative mode of consciousness”. Thus, although they may appear quite different on the surface, the bio-psycho-social mechanisms at play may be similar. People with different temperaments and different preferences for activity level may accrue the same benefit by participating in different forms of stress reduction. In the multicultural society, it would be reasonable to derive various stress reduction practices from different parts of the world. In that regard, ngoma ceremonies, West African healing ceremonies, and similar ceremonies of Native Americans would have already been part of the broader American culture if they had not been deliberately suppressed for political reasons. In addition, it would be reasonable to ask whether combining Ngoma with MBSR or other mindfulness-based practices would have a synergistic effect. Thus, the authors feel that the present study and the work of Hewson et al.15 open up a rather broad field of research.
Conclusions
In a pilot study, a drum and dance ceremony based on the ngoma tradition of Central and Southern Africa led to improvement in markers of stress that were of a magnitude similar to a standard MBSR protocol. Further study of rhythm and dance ceremonies from indigenous cultures is warranted both because of these results and because of a strong rationale.
Acknowledgments
This research was supported by a grant from the Josiah Charles Trent Memorial Foundation Endowment Fund to K.H.W. The authors thank Sarah Wilson for guidance on selection of psychologic questionnaires. Richard Vinesett helped provide the live music for this study.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Hayes SC, Strosahl K, Wilson KG, et al. Measuring experiential avoidance: A preliminary test of a working model. Psychol Rec 2004;54:553–578 [Google Scholar]
- 2.Strauss C, Cavanagh K, Oliver A, Pettman D. Mindfulness-based interventions for people diagnosed with a current episode of an anxiety or depressive disorder: A meta-analysis of randomised controlled trials. PLoS One 2014;9:e96110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang MF, Wen YS, Liu WY, et al. Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer: A meta-analysis. Medicine (Baltimore) 2015;94:e0897-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fjorback LO, Arendt M, Ørnbøl E, et al. Mindfulness‐based stress reduction and mindfulness‐based cognitive therapy: A systematic review of randomized controlled trials. Acta Psychiatr Scand 2011;124:102–119 [DOI] [PubMed] [Google Scholar]
- 5.Winkelman M. Shamanism: A Biopsychosocial Paradigm of Consciousness and Healing, 2nd ed. Santa Barbara, Denver, Oxford: Praeger, 2010 [Google Scholar]
- 6.Vinesett A, Price M, Wilson K. Therapeutic potential of a drum and dance ceremony based on the African Ngoma tradition. J Altern Complement Med 2015;21:460–465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janzen J. Ngoma: Discourses of Healing in Central and Southern Africa. Berkeley, CA: University of California Press, 1992 [Google Scholar]
- 8.van Dijk R, Reis R, Spierenburg M. The Quest for Fruition Through Ngoma: Political Aspects of Healing in Southern Africa. Cape Town, Athens: David Philip, 2000 [Google Scholar]
- 9.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Manag 1977;1:385–401 [Google Scholar]
- 10.Eaton WW, Smith C, Ybarra M, et al. Center for epidemiologic studies depression scale: Review and revision (CESD and CESD-R). In: Maruish M, ed. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment, 3rd ed. Volume 3: Instruments for Adults. Mahwah, NJ: Lawrence Erlbaum, 2004, pp. 363–377 [Google Scholar]
- 11.Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: New outcome measure for primary care. BMJ 1992;305:160–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borkovec T, Nau S. Credibility of analogue therapy rationales. J Behav Therap Exp Psychiat 1972;3:257–260 [Google Scholar]
- 13.Piper WE, Marrache M, Lacroix R, et al. Cohesion as a basic bond in groups. Hum Relat 1983;36:93–108 [Google Scholar]
- 14.Searle S, Casella G, McCulloch G. Variance Components. Hoboken, NJ: John Wiley and Sons, 1992 [Google Scholar]
- 15.Hewson P, Rowold J, Sichler C, Walter W. Are healing ceremonies useful for enhancing quality of life? J Altern Complement Med 2014;20:713–717 [DOI] [PubMed] [Google Scholar]
- 16.Sue DW, Sue D. Counseling the Culturally Diverse. Hoboken, NJ: John Wiley and Sons, 2013 [Google Scholar]
- 17.Stansfield D, Browne AJ. The relevance of indigenous knowledge for nursing curriculum. Int J Nurs Educ Scholarsh 2013;10:143–151 [DOI] [PubMed] [Google Scholar]
- 18.Walsh R. The World of Shamanism: New Views of an Ancient Tradition. Woodbury, MN: Llewellyn Publications, 2007 [Google Scholar]