Abstract
Background
The influence of surgery on olfaction in patients who suffer from chronic rhinosinusitis (CRS) is still not fully understood. Most particularly, the time course of the recovery is poorly studied.
Methods
The prospective study describes the results of the Sniffin' Sticks identification test in 41 subjects before (V1), 2 weeks after (V2), and 6 months after (V3) endonasal sinus surgery (ESS). Influencing factors (gender, revision surgery, nasal polyposis, and initial olfactory score) on the changes of the smell testing were evaluated.
Results
The whole cohort showed a significant improvement in Identification scores, from 8.63 to 10.24 after 2 weeks and to 10.68 after 6 months. Patients with nasal polyps revealed a similar increase in the identification test at V3 (+2.17 compared to +1.89 in those without polyps) but not at V2 (+1.30 compared to 2.00). The initial classification of olfaction was the only significant influencing factor. Patients who showed initially anosmic results improved (+4.87 at V2 and +4.73 at V3), as did patients in the hyposmic group (+0.58 resp. +1.42). Forty‐four percent of the patients reached an improvement with regard to their diagnostic group.
Conclusions
This study of the evaluation of the sense of smell after ESS exhibits an improvement of olfaction already 2 weeks after surgery, which is stable for 6 months. CRSwNP and CRSsNP patients showed similar improvements of olfaction, although the recovery was slower in CRSwNP patients.
Level of Evidence
2b.
Keywords: Sniffin' Sticks, sense of smell, nasal polyps, quality of life, CRS
INTRODUCTION
The intact human sense of smell is an important factor in human quality of life.1 Some examples of the consequences of impaired olfaction are food‐related problems,2 depression,3 and professional issues.4 Chronic rhinosinusitis (CRS), especially, is frequently associated with reduced smell abilities5 and reports describe an incidence of olfactory dysfunction of up to 80% in CRS patients.6 “Reduced smell” is used as a major symptom in guidelines for diagnosis of CRS.7 Patients suffering from CRS can be divided into two groups–CRS with nasal polyps (CRSwNP) and CRS without nasal polyps (CRSsNP)–with the former group showing a higher degree of smell impairment.8 In this aetiology of olfactory dysfunction, treatment options are available (either medical or surgical). If conservative treatment (especially topical steroids or short courses of systemic steroids) does not lead to a sufficient relief of symptoms (eg, rhinorrhea, blocked nose, and reduced olfaction), endonasal sinus surgery (ESS) is another therapeutic option for CRS patients.7 Whereas the positive effect of ESS on patients’ satisfaction and quality of life is well documented,9 its effect on olfaction is still not fully understood. Most studies evaluating changes in olfaction after sinus surgery rely on subjective reports of the patient's sense of smell, rather than any sophisticated testing methods, and therefore have limited validity.10 In those studies that use psychophysical tests to evaluate sense of smell, it is suggested that patients with polyps and anosmia might have a higher likelihood of improved olfaction after ESS than hyposmic patients without polyps.6 In some studies, a positive effect could only be found for initially anosmic patients.11 In other studies, no effect of ESS on olfaction was seen at all.12 Additionally, only a single study reports on a longer post‐operative period.13 A new meta‐analysis of olfactory outcomes after sinus surgery for CRS14 clearly shows a significant and clinically relevant improvement of the sense of smell documented by the used tests (UPSIT, total TDI of Sniffin’ Sticks, and Sniffin’ Sticks Identification Score) in CRSwNP patients and a mixed group of CRSwNP and CRSsNP. Patients with polyps revealed a higher increase, as well as pre‐operatively anosmic patients. In this meta‐analysis, the demand for further studies identifying results in CRSwNP and CRSsNP, hyposmics and anosmics, and the time course of recovery of olfaction is expressed.
Yet in recent publications15, 16 the first evaluation of olfaction after sinus surgery takes place after a time interval of 6 months and it is unclear when the recovery of olfaction starts postoperatively and whether there are differences in the timeline of recovery in CRSwNP and CRSsNP.
The aim of this investigation was to describe the time course of changes of olfaction in patients after sinus surgery for CRS by evaluating olfactory ability using the Sniffin' Sticks 16‐item identification test. Additionally, influencing factors (eg, presence of polyps, CT‐scores) and subjective evaluation were examined.
MATERIALS AND METHODS
Patients
In a prospective trial, patients of both genders over the age of 18 who were scheduled for ESS because of CRS, both with and without polyps, were screened. Primary surgical cases and revision cases were included and all patients had undergone unsuccessful conservative treatment with topical and/or systemic steroids prior the operation. The diagnosis of CRS was established by reference to the patient's history, nasal endoscopy and computed tomography (CT) of the paranasal sinuses according to the European position paper on rhinosinusitis and nasal polyps (EPOS) 2012 criteria.7 The preoperative CT scans of the paranasal sinuses were analyzed and the Lund‐Mackay score was noted.17 Exclusion criteria were single‐sided CRS, cystic fibrosis, immunodeficiency, primary cilia dysfunction, presence of neurodegenerative diseases, liver or renal deficiency, pregnancy, history of head trauma, and concomitant medication with drugs known to affect the sense of smell. All patients used nasal irrigation with saline at least twice a day and were treated with a topical nasal steroid (fluticasone furoate) once a day (27.5 µg), beginning after the surgical intervention and continuing for the entire study period. Courses of systemic steroids were not allowed postoperatively. The Ethics Committee of the Medical Association of Rhineland Palatinate, Germany approved the study (No. 837.475.08 [6472]) and all patients gave written informed consent.
Testing Olfaction
To evaluate the sense of smell, the 16‐item Sniffin’ Sticks identification test was used–a standardized, forced‐choice odor identification test.18 The correct answers were noted and results between 0 and 16 were possible. Normal olfactory function is presumed for scores of 13 and above, hyposmia for scores between 8 and 12, while scores below 8 are considered “functionally anosmic.”19, 20 Olfaction was measured before the surgery, 2 weeks thereafter (14 ± 1 days), and 6 months (24 ± 1 weeks) after the surgical intervention. Additionally, at these time points, the patients were asked to complete the German Adapted Version 20 of the Sino‐Nasal Outcome Test (SNOT‐20 GAV) questionnaire21 and were asked to rate the severity of their problem concerning the sense of smell (from 0 = no problem to 5 = highest impairment).
Statistical Analysis
All analyses were performed using the Statistical Package for the Social Sciences, Version 16.0 software system (SPSS Inc., Chicago, IL). In normally distributed values a T‐test was used for statistical analysis. Mean values and standard deviation were indicated. Confirmative testing was carried out for changes of olfactory scores before and after sinus surgery, therefore a Bonferroni correction was performed for multiple testing and the adapted significance level was set at p < 0.0125. Additionally, a linear regression was used to asses influencing factors (gender, age, type of CRS (without or with nasal polyps), previous surgery, and olfactory category [normosmic, hyposmic, or anosmic]) at baseline on the changes of postoperative olfactory scores. Other analyses were done exploratory and p values are given for descriptive reasons only. Influences of different parameters on olfaction preoperatively were evaluated using the Mann‐Whitney U test.
RESULTS
Fifty‐eight patients who were scheduled for ESS due to CRS were screened. Complete datasets of olfactory test results were available for 41 patients. For most of the missing 17 patients, the results for the Sniffin' Sticks Identification Score were missing for the last visit as patients refused to appear. Nevertheless, the groups of included and non‐included patients did not show relevant differences (for details see Table 1). Of the analyzed patients, 25 were male and 16 were female. The mean age was 49 years. The demographic details are shown in Table 1.
Table 1.
Demographic Data, Results of Sniffin’ Sticks Identification Scores (±SD) and Categories of Olfaction in Patients and Drop Outs Preoperatively (V1), 2 Weeks (V2), and 6 Months (V3) After Sinus Surgery.
| Patient group | Drop outs | |
|---|---|---|
| Total number | 41 | 17 |
| Female | 17 = 42% | 8 = 47% |
| Male | 24 = 58% | 9 = 53% |
| Age range | 21–73 years | 29–70 years |
| Mean age | 48.7 ± 13.2 | 50.7 ± 12.0 |
| Previous sinus operation | 24 = 58.5% | 8 = 47.1% |
| Lund‐Mackay Score ≤ 12 | 11 | 11 |
| Lund‐Mackay Score > 12 | 30 | 6 |
| CRSsNP | 18 | 8 |
| CRSwNP | 23 | 9 |
| Mean Sniffin’ Sticks Identification Score V1 | 8.6 ± 4.2 | 9.6 ± 3.5 (n = 12) |
| Normosmia | 7 = 17.1% | 4 = 33.3% |
| Hyposmia | 19 = 46.4% | 4 = 33.3% |
| Anosmia | 15 = 36.6% | 4 = 33.3% |
| Mean Sniffin’ Sticks Identification Score V2 | 10.2 ± 3.4 | 10.8 ± 3.4 (n = 14) |
| Normosmia | 12 = 29.3% | 4 = 28.6% |
| Hyposmia | 21 = 51.2% | 8 = 57.1% |
| Anosmia | 8 = 19.5% | 2 = 14.3% |
| Mean Sniffin’ Sticks Identification Score V3 | 10.7 ± 3.2 | 9.9 ± 5.2 (n = 7) |
| Normosmia | 15 = 36.6% | 3 = 42.9% |
| Hyposmia | 19 = 46.4% | 2 = 28.6% |
| Anosmia | 7 = 17.1% | 2 = 28.6% |
CRSsNP = chronic rhinosinusitis without nasal polyps; CRSwNP = chronic rhinosinusitis with nasal polyps
Pre‐ and Post‐Operative Olfactory Performance
The mean Sniffin' Sticks Identification score (± standard deviation, SD) for the visit before surgery (V1) was 8.6 ± 4.2. The mean score increased to 10.2 ± 3.4 at the second visit (V2, 2 weeks after surgery) and to 10.7 ± 3.2 at the third visit (V3, 6 months after surgery). The differences were significant for the changes between V1 and V3 (−2.1 ± 3.8, p = 0.001), but not between V1 and V2 (+1.6 ± 4.4, p = 0.023) and V2 and V3 (+0.4 ± 3.0, p = 0.361). Two weeks after surgery, 28 of 41 patients showed an increase of at least 1 point in the Sniffin’ Sticks identification test. Six months after surgery, this was the case in 25 of 41 patients.
Influencing Factors of Olfaction Before Operation
Male patients showed lower Identification scores (7.6 ± 3.8) than female (10.2 ± 4.3), p = 0.02. Patients who had previously undergone sinus surgery (7.7 ± 4.2) showed a reduced identification score as compared to patients for whom this was their first sinus operation (9.9 ± 3.9), p = 0.06. Patients with a Lund‐Mackay score of 13 or more in the CT scan showed a trend towards lower Identification scores (8.0 ± 4.4) than did patients with lower CT‐scores (10.4 ± 2.8), p = 0.16. The same trend towards lower smell test scores was found in the group of CRSwNP (7.7 ± 4.4) as compared to the group of CRSsNP (9.8 ± 3.6), p = 0.11.
Subjective Evaluation of the Sense of Smell
The mean value of patients’ ratings of the severity of disturbance to their sense of smell (from 0 = no problem to 5 = highest impairment) before surgery was 3.35 (±1.62) and decreased to 2.34 (±1.68) after 2 weeks (p = 0.001) and to 1.56 (±1.34) after 6 months (p = 0.013) following surgery. The correlation between self‐ratings and the Sniffin' Sticks results was good at all time points: −0.640 at V1, −0.629 at V2, and −0.646 at V3. The changes in both the identification score and self‐ratings also correlated, with r = −0.398 to −0.507. The subgroups of CRS patients with and without nasal polyposis also showed relevant correlations of subjective and objective measures, except at V1 in the CRSwNP group.
Factors Influencing the Increase of Olfaction Post‐Operatively
After 6 months, patients with nasal polyps showed a similar increase in the identification test (+2.2 ± 4.2, p = 0.02) as compared to those without polyps (+1.9 ± 3.4, p = 0.03). This size of increase was found in the CRSsNP group already after 2 weeks (+2.0 ± 3.5, p = 0.026) but not in the CRSwNP group (+1.3 ± 5.0, p = 0.224) (Fig. 1). In the linear regression model, only the category of olfaction before surgery showed a significant influence of the mean changes of Identification Scores between V1 and V3 (coefficient of 4.09, p < 0.001, confidence interval: 2.53 to 5.66). The detailed results of the regression model are shown in Table 2.
Figure 1.
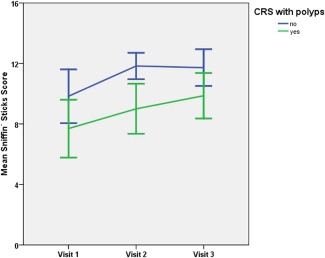
Mean Sniffin’ Sticks score preoperatively (visit 1), 2 weeks (visit 2), and 6 months (visit 3) after surgery ±SD in patients with chronic rhinosinusitis without nasal polyps (blue, n = 18) and chronic rhinosinusitis with nasal polyps (green, n = 23).
Table 2.
Results of the Regression Model of Results of Sniffin' Sticks Identification Scores at V1 (Preoperatively) and V3 (6 Months After Surgery).
| Variables Entered/Removed* | |||
|---|---|---|---|
| Model | Variables Entered | Variables Removed | Method |
| 1 | olfactory category, age, polyps, gender, previous surgery | . | Enter |
| *Dependent Variable: Identification Scores V1 and V3. | |||
| Model Summary | ||||
|---|---|---|---|---|
| Model | R | R Square | Adjusted R Square | Std. Error of the Estimate |
| 1 | 0.679* | 0.461 | 0.384 | 2.98949 |
| *Predictors: (Constant), olfactory category, age, polyps, gender, previous surgery. | ||||
| ANOVA† | ||||||
|---|---|---|---|---|---|---|
| Model | Sum of Squares | df | Mean Square | F | Sig. | |
| 1 | Regression | 267.106 | 5 | 53.421 | 5.978 | 0.000* |
| Residual | 312.797 | 35 | 8.937 | |||
| Total | 579.902 | 40 | ||||
| *Predictors: (Constant), olfactory category, age, polyps, gender, previous surgery. | ||||||
| †Dependent Variable: Identification Scores V1 and V3. | ||||||
| Coefficients* | ||||||||
|---|---|---|---|---|---|---|---|---|
| Unstandardized Coefficients | Standardized Coefficients | 95% Confidence Interval for B | ||||||
| Model | B | Std. Error | Beta | t | Sig. | Lower Bound | Upper Bound | |
| 1 | (Constant) | −11.856 | 2.867 | −4.135 | 0.000 | −17.678 | −6.035 | |
| Previous surgery | 1.368 | 1.187 | 0.179 | 1.152 | 0.257 | −1.043 | 3.778 | |
| Gender | −0.988 | 1.055 | −0.128 | −0.936 | 0.355 | −3.130 | 1.154 | |
| Age | 0.032 | 0.040 | 0.111 | 0.813 | 0.422 | −0.048 | 0.112 | |
| Polyps | 0.116 | 1.083 | 0.015 | 0.107 | 0.915 | −2.082 | 2.315 | |
| Olfactory category | 4.091 | 0.771 | 0.768 | 5.308 | 0.000 | 2.526 | 5.656 | |
*Dependent Variable: Identification Scores V1 and V3.
Patients who had undergone sinus surgery previously showed a lower increase of the Identification score from V1 to V2 (+1.3) as compared to patients who had no previous surgery (+2.1, p = 0.013), but not from V1 to V3 (+2.2, compared to +1.8, p = 0.24).
The preoperative CT‐score (Lund‐Mackay ≤12 vs. >13) did not show differences in the amount of changes of Identification scores at the different time points (2.1 vs. 2.0, between V1 and V3).
Category of Olfaction
If the results of the Identification scores are classified into categories of olfaction (anosmia, hyposmia, and normosmia), 15 patients were anosmic, 19 were hyposmic, and 7 were normosmic preoperatively (V1). Two weeks (V2) after the surgery, 8 subjects were anosmic, 21 were hyposmic, and 12 were normosmic. Six months after surgery (V3), 8 subjects were anosmic, 18 were hyposmic, and 15 were normosmic (Fig. 2). Therefore, 6 months after surgery (V3), 44% of patients reached a better category of olfaction, 46% stayed in the same category, and 10% changed to a lower category as compared to the diagnostic group prior to the surgical intervention (Table 3). In the subgroups with and without nasal polyps, comparable results were seen (43% of CRSsNP patients and 44% of CRSwNP patients reached a higher category, 43% of CRSsNP patients and 50% of CRSwNP patients stayed in the same category, and 13% of CRSsNP patients and 6% of CRSwNP patients decrease to a lower category). Taking both patient groups (CRSsNP and CRSwNP) together, the number of normosmic subjects doubled from V1 to V3, although the absolute number of patients who reached normosmic results after surgery was lower in the CRSwNP group. The amount of hyposmic patients stayed stable and the amount of anosmic individuals decreased from 20% to 10% in the CRSsNP group and from 50% to 30% in CRSwNP patients (Fig. 2).
Figure 2.
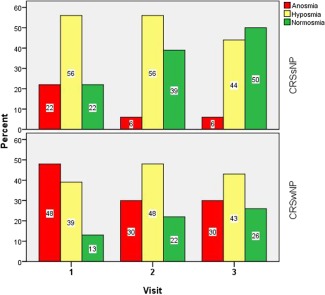
Distribution of the different categories of olfaction (anosmia = red, hyposmia = yellow, and normosmia = green) preoperatively (V1), 2 weeks (V2), and 6 months (V3) after surgery in patients with CRSsNP (n = 18) and CRSwNP (n = 23).
Table 3.
Changes in the Diagnostic Group of the Individual Patients From V1 (Preoperatively) to V3 (6 Months After Surgery).
| 6 Months After Surgery | ||||
|---|---|---|---|---|
| Anosmic | Hyposmic | Normosmic | ||
| Before surgery | Anosmic | 6 | 7 | 2 |
| Hyposmic | 1 | 9 | 9 | |
| Normosmic | 1 | 2 | 4 | |
The improvement of patients’ olfaction is shaded in green (anosmic to hyposmic; anosmic to normosmic; hyposmic to normosmic), an unchanged category is shaded in blue, and a decrease (normosmic to hyposmic; normosmic to anosmic; hyposmic to anosmic) is shaded in red.
Patients who initially showed anosmic results (n = 15) reached a mean increase in the Identification score of 4.9 (±3.5, p < 0.001) points after 2 weeks, which was stable after 6 months (+4.7 ± 3.2, p < 0.001). The patients in the hyposmic group (n = 19) showed an increase of 0.6 ± 2.3 (p = 0.295) points after 2 weeks and 1.4 ± 2.8 (p = 0.039) points after 6 months. The patients who were normosmic preoperatively (n = 7) experienced the following changes: −2.6 ± 5.6 (p = 0.272) points after 2 weeks and −2.0 ± 3.3 (p = 0.162) points after 6 months (Fig. 3). The reductions in subjective ratings were similar (−1.62/−1.06 points at 2 weeks and −2.31/‐2.17 at 6 months) in the initially anosmic and hyposmic groups resp., while the normosmic group underwent a mean decrease of 0.57 after 2 weeks and 0.0 after 6 months.
Figure 3.
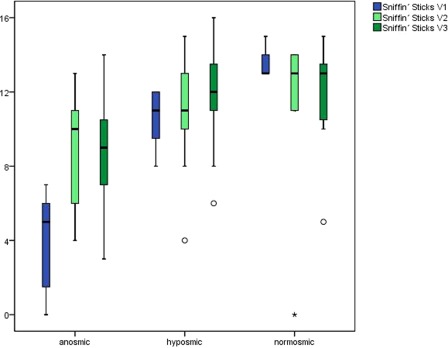
Box plots of changes in Sniffin’ Sticks scores preoperatively (V1, blue), 2 weeks (V2, light green), and 6 months (V3, dark green) after surgery, considering the initial olfactory performance (anosmic, n = 15, hyposmic, n = 19 or normosmic, n = 7). The lines represent the medians; the boxes include 75% of the results; the whiskers include 95% of the results; the circles show outliers.
DISCUSSION
This prospective cohort study shows that, in most patients, after ESS for CRS, a measurable improvement in Sniffin’ Sticks identification of at least 1 point can be achieved just 2 weeks after surgery (68%) which is stable under concomitant treatment with topical steroids for a period of 6 months (61%). This percentage is higher than that described by others,22 although the distribution of CRSwNP and CRSsNP patients is similar in both cohorts, and both the testing method used and the follow‐up period observed were comparable. One explanation could be that, in Pade's study, the preoperative identification score was considerably higher (mean 10.2) than in our cohort (mean 8.6). The change of about 2 points in the Sniffin' Sticks Identification score can be regarded as clinically significant, following the results of Gudziol et al.23 A possible “learning effect” as one reason for improved identification scores does not seems to play an important role, as in the initial presentation of the Sniffin' Sticks test kit,24 such an effect could not been seen over a 4‐month interval. A more recent study did not see significant changes in results when using an extended 32‐item test.25 Additionally, it must be recognized that these studies were done on healthy individuals and the chance of an occurring learning effect is even lower in subjects with impaired olfaction because the tested subject as a matter of course is not told whether his choice during the test was correct or not.
As shown by the linear regression model in our study, the only influencing factor that significantly affects the olfactory improvement is the pre‐operative olfactory category. Other factors like age, gender, previous sinus operations, or polyp status (CRSwNP or CRSsNP) showed no influence here.
When the diagnostic group of olfaction is considered, 44% of patients achieved an improvement in their sense of smell (hyposmic to normosmic; anosmic to hyposmic; anosmic to normosmic), which is similar to the results of a study that showed an improvement rate to a higher class of olfaction in 45% of 29 revision cases.26 Although our study confirmed a trend towards lower values in the smell test preoperatively in patients who had previously undergone sinus surgery, there was no significant difference in the post‐operative improvement on olfaction. Instead, we found a higher improvement rate in CRSwNP patients (66%) than in CRSsNP patients (30%).
The improvement in Identification scores after ESS accompanies a reduction in the subjective ratings of disturbance of the olfactory impairment. The additional information of other tests evaluating olfactory discrimination and threshold (represented by the Sniffin’ Sticks TDI‐Score) would seem to be more appropriate to measure olfaction, but this estimation could not be proved in CRS studies yet.14, 27
The fact that the post‐operative improvement of olfaction can be predicted by the Lund‐Mackay score has been described elsewhere.28 Although we confirmed that the preoperative Identification score was lower in the group with higher CT‐scores (Lund‐Mackay score >12), the improvement rates after 6 months were almost identical in both groups (+2 points) whereas, in the Minwegen study, the patients with Lund‐Mackay scores ≤7 showed a trend towards decreased values (‐0.82 points on the 12‐item Sniffin' Sticks identification test). Even if the same limits in CT‐scores are used, we still see a clear trend towards improved olfactory scores (+3.5 at V3), although only the data of four patients are suitable.
Our study showed lower preoperative and post‐operative scores in patients with CRSwNP as compared to CRSsNP, as previously described.6 The statistical analysis failed to be significant in our study, most likely because the sample size was too low. The post hoc power calculation for the changes of the Sniffin' Sticks Identification Score in our study showed a value of 88% for the differences between V1 and V3, 58% for differences between V1 and V2, and only 7% for differences between V2 and V3. Yet, in our study 6 months after surgery, both groups of patients (CRSsNP and CRSwNP) showed a comparable increase in Identification scores contradictory to other studies.15 Interestingly, there was a notable difference already 2 weeks after surgery, and the CRSwNP patients required a longer time for recovery. This finding could be explained by reference to the fact that the recovery of the olfactory epithelium might take more time in patients with a more severe form of the disease, as which CRSwNP can be regarded. Not only local recovery processes but also an increase in the volume of the olfactory bulb can be observed after sinus surgery has been documented by MRI studies.29
Inconsistently with the results of another trial which used the University of Pennsylvania Smell Identification Test (UPSIT) score to measure olfaction,11 we measured increasing olfactory scores in patients who were preoperatively anosmic and also in initially hyposmic patients. Patients in the anosmic group showed an earlier (already after 2 weeks) and greater increase, which was stable after 6 months. The group of hyposmic subjects showed a remarkable recovery of olfaction after 6 months but the degree of increase was lower. The reason for this finding is not clear. One would assume that a recovery of the olfactory epithelium takes longer in anosmic patients as compared to hyposmic patients. On the other hand, elimination of a mechanical obstruction by polyps of the olfactory cleft would lead to an almost instant effect, which was the case in 75% of the anosmic patients in our cohort. Therefore, it can be concluded that indeed both factors – a local inflammatory disturbance and a mechanical obstruction – are involved in the pathophysiology of impaired olfaction in CRS patients. Although the increase experienced by the initially hyposmic patients was lower and delayed as compared to the anosmic group, it can still be considered as clinically relevant as the reduction in subjective ratings were similar.
The sustained improvement of the sense of smell after sinus surgery under continued topical nasal steroid medication is documented by our findings for a period of up to 6 months. One remarkable study shows positive effects on olfaction even after a follow‐up period of 5 years.13
In some patients, an improvement of olfaction after sinus surgery cannot be achieved and, in fact, in up to 10% of patients a decrease of olfaction after ESS can occur, as corroborated by others studies.22, 30 The reason for this result is still unknown. In our study, a sustained deterioration of the sense of smell 6 months after surgery occurred in 4 of 41 patients. Of these, three patients were initially normosmic and three showed CRSwNP. Interestingly, the subjective rating of the impairment of olfaction was preoperatively high (with scores of between 3 and 4) and showed a decrease after surgery (to scores between 1 and 2). Therefore, we can say that preoperative evaluation of the sense of smell by validated testing is crucial and olfactory impairments after surgery are not necessarily recognized by the individual patient.
CONCLUSION
This prospective study of the evaluation of the sense of smell using an established testing method in a well‐defined population of patients undergoing ESS for CRSwNP and CRSsNP found an improvement of olfaction in both groups already 2 weeks after the surgical procedure. The overall improvement recorded at 6 months after surgery was similar in both groups, although CRSsNP patients showed higher preoperative scores and gained greater post‐operative levels, and the recovery of olfaction was slower in CRSwNP patients. More than 40% of patients showed a clinically relevant improvement of olfaction, regardless of polyposis status. Additionally, the recovery of the sense of smell was possible independently of whether a subject was initially anosmic or hyposmic, with higher recovery rates in initially anosmic subjects.
Conflict of Interest: The authors declare that they have no conflict of interest.
Financial disclosure: None.
BIBLIOGRAPHY
- 1. Philpott CM, Boak D. The impact of olfactory disorders in the United Kingdom. Chemical Senses 2014;39:711–718. [DOI] [PubMed] [Google Scholar]
- 2. Temmel A, Quint C, Schickinger‐Fischer B, Klimek L, Stoller E, Hummel T. Characteristics of olfactory disorders in relation to major causes of olfactory loss. Arch Otolaryngol Head Neck Surg 2002;128:635–641. [DOI] [PubMed] [Google Scholar]
- 3. Deems DA, Doty RL, Settle RG, et al. Smell and taste disorders, a study of 750 patients from the University of Pennsylvania Smell and Taste Center. Arch Otolaryngol Head Neck Surg 1991;117:519–528. [DOI] [PubMed] [Google Scholar]
- 4. Haxel BR, Nisius A, Fruth K, Mann WJ, Muttray A. [Deficits in medical counseling in olfactory dysfunction]. HNO 2012;60:432–438. [DOI] [PubMed] [Google Scholar]
- 5. Rombaux P, Huart C, Levie P, Cingi C, Hummel T. Olfaction in chronic rhinosinusitis. Curr Allergy Asthma Rep 2016;16:41. [DOI] [PubMed] [Google Scholar]
- 6. Rudmik L, Smith TL. Olfactory improvement after endoscopic sinus surgery. Curr Opin Otolaryngol Head Neck Surg 2012;20:29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fokkens WJ, Lund VJ, Mullol J, et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 2012;50:1–12. [DOI] [PubMed] [Google Scholar]
- 8. Litvack JR, Fong K, Mace J, James KE, Smith TL. Predictors of olfactory dysfunction in patients with chronic rhinosinusitis. Laryngoscope 2008;118:2225–2230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smith TL, Litvack JR, Hwang PH, et al. Determinants of outcomes of sinus surgery: a multi‐institutional prospective cohort study. Otolaryngol Head Neck Surg 2010;142:55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Haxel BR, Bertz‐Duffy S, Fruth K, Letzel S, Mann WJ, Muttray A. Comparison of subjective olfaction ratings in patients with and without olfactory disorders. J Laryngol Otol 2012;126:692–697. [DOI] [PubMed] [Google Scholar]
- 11. Litvack JR, Mace JC, Smith TL. Does olfactory function improve after endoscopic sinus surgery? Otolaryngol Head Neck Surg 2009;140:312–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jiang RS, Lu FJ, Liang KL, et al. Olfactory function in patients with chronic rhinosinusitis before and after functional endoscopic sinus surgery. Am J Rhinol 2008;22:445–448. [DOI] [PubMed] [Google Scholar]
- 13. Briner HR, Jones N, Simmen D. Olfaction after endoscopic sinus surgery: long‐term results. Rhinology 2012;50:178–184. [DOI] [PubMed] [Google Scholar]
- 14. Kohli P, Naik AN, Farhood Z, et al. Olfactory outcomes after endoscopic sinus surgery for chronic rhinosinusitis: a meta‐analysis. Otolaryngol Head Neck Surg 2016;155:936–948. [DOI] [PubMed] [Google Scholar]
- 15. Andrews PJ, Poirrier AL, Lund VJ, Choi D. Outcomes in endoscopic sinus surgery: olfaction, nose scale and quality of life in a prospective cohort study. Clin Otolaryngol 2016;41:798–803. [DOI] [PubMed] [Google Scholar]
- 16. Levy JM, Mace JC, Sansoni ER, Soler ZM, Smith TL. Longitudinal improvement and stability of olfactory function in the evaluation of surgical management for chronic rhinosinusitis. Int Forum Allergy Rhinol 2016;6:1188–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lund VJ, Mackay IS. Staging in rhinosinusitus. Rhinology 1993;31:183–184. [PubMed] [Google Scholar]
- 18. Wolfensberger M, Schnieper I, Welge‐Lüssen A. Sniffin' Sticks: a new olfactory test battery. Acta Otolaryngol 2000;120:303–306. [DOI] [PubMed] [Google Scholar]
- 19. Kobal G, Klimek L, Wolfensberger M, et al. Multicenter investigation of 1,036 subjects using a standardized method for the assessment of olfactory function combining tests of odor identification, odor discrimination, and olfactory thresholds. Eur Arch Otorhinolaryngol 2000;257:205–211. [DOI] [PubMed] [Google Scholar]
- 20. Landis BN, Konnerth CG, Hummel T. A study on the frequency of olfactory dysfunction. Laryngoscope 2004;114:1764–1769. [DOI] [PubMed] [Google Scholar]
- 21. Baumann I. [ Validated instruments to measure quality of life in patients with chronic rhinosinusitis]. HNO 2009;57:873–881. [DOI] [PubMed] [Google Scholar]
- 22. Pade J, Hummel T. Olfactory function following nasal surgery. Laryngoscope 2008;118:1260–1264. [DOI] [PubMed] [Google Scholar]
- 23. Gudziol V, Lotsch J, Hahner A, Zahnert T, Hummel T. Clinical significance of results from olfactory testing. Laryngoscope 2006;116:1858–1863. [DOI] [PubMed] [Google Scholar]
- 24. Hummel T, Sekinger B, Wolf SR, Pauli E, Kobal G. ‘Sniffin' sticks': olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses 1997;22:39–52. [DOI] [PubMed] [Google Scholar]
- 25. Haehner A, Mayer AM, Landis BN et al. High test‐retest reliability of the extended version of the “Sniffin' Sticks” test. Chem Senses 2009;34:705–711. [DOI] [PubMed] [Google Scholar]
- 26. Hsu CY, Wang YP, Shen PH, Weitzel EK, Lai JT, Wormald PJ. Objective olfactory outcomes after revision endoscopic sinus surgery. Am J Rhinol Allergy 2013;27:e96–e100. [DOI] [PubMed] [Google Scholar]
- 27. Gudziol V, Michel M, Sonnefeld C, Koschel D, Hummel T. Olfaction and sinonasal symptoms in patients with CRSwNP and AERD and without AERD: a cross‐sectional and longitudinal study. Eur Arch Otorhinolaryngol 2017;274:1487–1493. [DOI] [PubMed] [Google Scholar]
- 28. Minwegen F, Thomas JP, Bernal‐Sprekelsen M, Dazert S, Minovi A. Predictive value of disease severity on self‐reported rating and quantitative measures of olfactory function outcomes after primary endoscopic sinus surgery. A prospective study. Rhinology 2014;52:437–443. [DOI] [PubMed] [Google Scholar]
- 29. Gudziol V, Buschhuter D, Abolmaali N, Gerber J, Rombaux P, Hummel T. Increasing olfactory bulb volume due to treatment of chronic rhinosinusitis–a longitudinal study. Brain 2009;132:3096–3101. [DOI] [PubMed] [Google Scholar]
- 30. Stevens CN, Stevens MH. Quantitative effects of nasal surgery on olfaction. Am J Otolaryngol 1985;6:264–267. [DOI] [PubMed] [Google Scholar]


