Abstract
Objectives
Suboptimal hearing aid use extorts significant social, health, and economic costs. The aims of this study were to (1) test the novel hypothesis that the threat associated with being diagnosed with hearing loss could be ameliorated with a self‐affirmation manipulation and (2) gauge the feasibility of deploying the manipulation in routine clinical practice.
Design
Parallel groups randomized controlled trial with 10‐week follow‐up.
Method
Fifty people, newly prescribed with a hearing aid, completed either a questionnaire that included a brief self‐affirming exercise or an identical questionnaire with no self‐affirming exercise. The main outcome measure was derived from data logging automatically stored by the hearing aid. Perceived threat (‘anxiety about ageing’), behavioural intention, and self‐efficacy were measured as potential mediators.
Results
Objectively measured hours of daily hearing aid use were marginally higher in the intervention group compared with the control group (between‐group difference = 1.94 hr, 95%CI = −1.24, 5.12, d = 0.43). At follow‐up, participants in the intervention group were significantly less anxious about ageing and more accepting of older people than were participants in the control group (between‐group difference = 0.75, 95%CI = 0.26, 1.22, d = 0.87). There was no statistically significant effect of the intervention on behavioural intention or self‐efficacy.
Conclusions
Although not statistically significant, the magnitude of the effect of the intervention on hearing aid use (d = 0.43) suggests that it would be worthwhile working towards a fully powered randomized controlled trial. The ability to reduce anxieties about ageing with this brief intervention could have far‐reaching benefits for multiple patient and general population groups.
Statement of contribution.
What is already known on this subject?
Hearing impairment is more disabling than diabetes, yet hearing aid use is suboptimal.
Anxieties about ageing may undermine hearing aid use.
What does this study add?
The study tests a brief theory‐based psychological intervention to reduce anxiety about ageing and promote hearing aid use.
Results show that the brief psychological intervention reduced anxiety and marginally increased objective hearing aid use.
Further work is required to identify other situations in which anxieties about ageing undermine behaviour change efforts.
The very brief, flexible nature of the intervention means it could be adapted and deployed in numerous other health care settings.
Keywords: self‐affirmation, hearing aid use, audiology, behaviour change, intervention, hearing aid prescription, ageing
Background
Hearing loss is the most common sensory deficit and the second leading cause of long‐term disability (WHO, 2002). Hearing loss can be managed effectively, and approximately 1.68 m people have been tested and fitted with hearing aids via the National Health Service (NHS) at a cost of £294 (one ear) or £388 (both ears, Campbell, 2015). However, it is estimated that 30% of people who own hearing aids do not wear them regularly (Action on Hearing Loss, 2014) meaning that the NHS incurs significant wastage. A recent Cochrane review (Barker, Mackenzie, Elliott, Jones, & de Lusignan, 2016) examined 37 randomized controlled trials of interventions to improve hearing aid use, but found no evidence that hearing aid use could be improved either through self‐management support, changing how the service was provided, or a combination of the two. Barker et al. (2016) attributed these null findings to the poor methodological quality of the studies included in the review and concluded that new studies employing better‐quality methodologies are needed to improve hearing aid use. One key limitation of the studies included in Barker et al.'s (2016) systematic review is that none made explicit use of behaviour change theory to design the interventions aimed at improving hearing aid use. Explicit use of theory is one means by which behaviour change interventions can be optimized (Michie & Prestwich, 2010). This study took the novel approach of hypothesizing that suboptimal hearing aid use is driven by anxieties about ageing that can be ameliorated by encouraging people to self‐affirm. The principal aims of the study were to (1) assess the feasibility of delivering and (2) estimate the likely effect of a self‐affirmation‐based intervention on hearing aid use.
Barriers to hearing aid use
It is clear that suboptimal hearing aid use is a multifactorial problem, but that many of the solutions require that patients engage with services, from initial assessments of hearing to solving technical problems with assistive hearing devices (McCormack & Fortnum, 2013). However, there are potentially powerful psychological barriers to engaging fully with hearing services, and it is notable that Barker et al. (2016) found that interventions designed to reconfigure hearing health services (e.g., reorganizing the scheduling of care) were not effective in improving hearing aid use. One factor that might explain both lack of engagement with services and reluctance to wear hearing aids is the stigma associated with hearing aid use. For example, patients in one prototypical study (Dawes, Maslin, & Munro, 2014) described how they resisted using hearing aids because they were an unwanted symbol of old age (e.g., ‘I wanted to still be a young man’, p. 866) and it is notable that 70% of people over the age of 70 years have hearing loss compared with 40% of people aged over 50 (Action on Hearing Loss, 2014). Thus, the psychological threat associated with using hearing aids could act as a substantial barrier to optimal hearing aid use.
Self‐affirmation theory
Self‐affirmation theory (Steele, 1988) offers one possible approach to overcoming threats to the self that might arise as a result of needing a hearing aid. According to self‐affirmation theory (Steele, 1988), people sustain their subjective well‐being by maintaining a positive, moral, and adaptive self‐image. A threat to this subjective well‐being targeted at any domain of the self (e.g., ageing) leads people to protect their global sense of self, which means bolstering their self‐image in a domain other than that under direct threat. Being asked to wear a hearing aid may be one such threat to a person's sense of self, which might lead people to preserve this sense of self by compensating in other domains, including not engaging with services or neglecting to use a hearing aid as advised. However, if a person's self‐image can be bolstered (affirmed) in a domain that is important to them (e.g., being kind), thereby preserving self‐integrity, they should be less likely to respond defensively and so be more likely to engage with services (Steele, 1988). Accumulated empirical evidence demonstrates that affirming the self consistently leads to significant improvements in health behaviours, including reducing alcohol consumption (Armitage, Rowe, Arden, & Harris, 2014) and increasing adherence to medication (Wileman et al., 2014). More recently, Armitage (2016) showed that a self‐affirmation manipulation was able to protect women's subjective well‐being from global societal threats associated with ageing and it is plausible that the specific threat from a hearing aid prescription might similarly be ameliorated.
Limitations of previous studies
Like Coulson, Ferguson, Henshaw, and Heffernan's (2016) review of applications of health psychology theories to audiological outcomes, we were unable to locate studies that had applied self‐affirmation theory to the problem of hearing aid uptake. However, consistent with Coulson et al.'s (2016) thesis, we argue that the limitations in research designs and sampling common to many studies of the effects of self‐affirmation on behaviour change can be addressed through insights from audiology research. First, in the typical self‐affirmation study, changes in behaviour are assessed using self‐reports (Armitage, Rowe, et al., 2014) or proxy biomedical measures (Wileman et al., 2014). This is potentially problematic because it is not clear whether these measures truly assess behaviour change. Given that objective data on hearing aid use are generated automatically by hearing aids and routinely gathered by hearing care professionals (although rarely used), audiological research offers a unique opportunity to gather objective behavioural data. A second limitation concerns sampling: The majority of self‐affirmation research is conducted on student populations, and it would be valuable to see whether research findings extend beyond this narrow sampling (Epton, Harris, Kane, van Koningsbruggen, & Sheeran, 2015). Given that most hearing loss is age‐related (e.g., Cruickshanks et al., 2003), hearing aid use represents an opportunity to test health psychology approaches in an older population.
A third limitation with previous research is that, thus far, the mediating mechanisms proposed by Steele (1988) have been discovered only sporadically (Epton et al., 2015). For example, although Wileman et al. (2014) hypothesized that self‐affirming would reduce renal patients’ defensiveness and hence make them more open to a persuasive message, there was no evidence that the observed significant effects on serum phosphate levels (a biomarker for medication adherence) were mediated through changes in perceived threat or motivation. However, as noted by Epton et al. (2015), the ways in which perceived threat and motivation have been operationalized have been variable in terms of reliability and validity. This study therefore employed measures with established reliability and validity to operationalize perceived threat as ‘anxiety about ageing’ (Lasher & Faulkender, 1993) and motivation as behavioural intention and self‐efficacy, which are considered the proximal determinants of behaviour in Ajzen's (1991) theory of planned behaviour and have been shown consistently to have medium–large associations with behaviour (e.g., Armitage & Conner, 2001).
This study uses a parallel group randomized controlled design to test the novel hypothesis that self‐affirmation can reduce people's anxieties about ageing that accompany hearing aid use (Dawes et al., 2014), thereby increasing motivation and ultimately improving hearing aid use. Using a parallel group randomized controlled design allows us to infer causal relationships between self‐affirming and any observed behaviour change. Careful observation of recruitment and retention rates will help us to gauge the feasibility of our approach and decide whether to pursue a fully powered randomized controlled trial in the future.
Method
Participants
Participants were recruited from an audiology department in a single NHS hospital in the north of England. Patients who were new to the service were invited to participate in a study about their beliefs about wearing hearing aids. No incentive to participate was offered, and all hearing aids and aftercare appointments were provided free of charge consistent with standard NHS practice. Only adults aged over 18 years who had never used a hearing aid before were included. The exclusion criteria were as follows: severe or profound hearing impairment, any condition that required a medical opinion including otalgia (‘earache’); unilateral, bothersome, or pulsatile tinnitus (noises in ears and/or head); asymmetrical hearing loss of unknown origin; or any dementia or cognitive deficits that would affect the individual's capacity to consent.
Ethical approval for this study was sought using the Integrated Research Application System and was granted by London (Camden and Islington), reference number 14/LO/1681. Patients provided informed consent and were told that they were free to choose whether or not to participate and that they could withdraw themselves or their data at any time without consequence. Participants were told that the study was designed to assess motivation with respect to wearing hearing aids and anxiety about ageing.
Design
The design was mixed, consisting of between‐ and within‐participants factors. The between‐participants factor was condition: Participants were randomized either to an intervention group (n = 25) or a control group (n = 25) on the basis of blind random draws from a hat. The within‐participants factor was the 10‐week time interval between pre‐fitting and follow‐up, consistent with the standard care pathway. The main outcome measure was objective hearing aid use.
Materials
Self‐affirmation manipulation
Self‐affirmation has been induced in three main ways and so a workshop with 12 patient and public involvement representatives was conducted to assess acceptability. Participants were presented with an accessible description of self‐affirmation theory, summaries of relevant studies, and examples of three different types of self‐affirmation activity (writing an essay about important values, elaborating on past acts of kindness through a questionnaire, and being asked to write one of four self‐affirming statements). Participants were invited to comment on the acceptability and appropriateness of the self‐affirmation activities for use in a patient questionnaire. Participants were positive about the approach and unanimous that writing out one of four self‐affirming statements was the most acceptable.
Thus, self‐affirmation was induced at baseline using an established manipulation (Armitage, Harris, & Arden, 2011; Armitage, Rowe, et al., 2014) that was embedded at the end of the research questionnaires. An annotated version of the intervention questionnaire is included in the Supporting Information. Participants were first presented with the stem ‘If I feel threatened or anxious, then I will…’ and were then presented with one of four options with which to complete the sentence (‘…think about the things I value about myself’, ‘…remember things that I have succeeded in’, ‘…think about what I stand for’, and ‘…think about the things that are important to me’). Following these options were three blank lines on which to write one of the four self‐affirming sentences. To encourage participants to write the self‐affirming sentence out in full, they were prompted with ‘If…’ at the beginning of the first blank line. Participants in the control condition completed the same questionnaire as participants in the intervention group described below, but without this self‐affirmation manipulation.
Measures
Motivation to use hearing aid(s) was operationalized as behavioural intention and self‐efficacy, which were measured before the self‐affirmation manipulation, and at 10‐week follow‐up. All measures were assessed at baseline and follow‐up on 7‐point (+1 to +7) Likert‐type scales. Behavioural intention was measured using three items (e.g., ‘I intend to wear my hearing aid as advised definitely do not‐definitely do’). Internal reliability was high at both baseline, α = .72, and follow‐up, α = .76. Self‐efficacy was measured with three items, including ‘How confident are you that you will be able to wear your hearing aid as advised? not very confident‐very confident’. Cronbach's α indicated high internal reliability at baseline, α = .72, and at follow‐up, α = .89.
Lasher and Faulkender's (1993) anxiety about ageing scale was used to operationalize people's perceived threat concerning ageing. The four subscales tap ‘fear of old people’, ‘psychological concerns’, ‘physical appearance’, and ‘fear of losses’, which consist of five items each. However, piloting demonstrated that the full 20‐item scale was unlikely to be completed by the target population, and so the scale was abbreviated using the three highest‐loading items on each of the subscales according to Lasher and Faulkender's (1993) principal components analysis. Descriptions of the items and their psychometric properties are provided in Table 1. All anxiety about ageing items were assessed on strongly disagree (+1)–strongly agree (+7) scales; lower scores on the scale denote greater anxiety and lower acceptance of ageing.
Table 1.
Rotated factor matrix for principal components analysis of Anxiety about ageing items
| Items | Factor Loadings | |||
|---|---|---|---|---|
| ‘Fear of old people’ | ‘Positive ageing’ | Factor 3 | Factor 4 | |
| Anxiety about ageing 1: ‘friends will be gone’ | .38 | −.37 | .17 | .53 |
| Anxiety about ageing 2: ‘enjoy being around old people’ | .80 | .16 | .19 | .01 |
| Anxiety about ageing 3: ‘feel good about life’ | .28 | .65 | −.04 | −.15 |
| Anxiety about ageing 4: ‘do things for myself’ | .22 | .74 | −.30 | .09 |
| Anxiety about ageing 5: ‘enjoy talking with old people’ | .81 | .22 | −.05 | .02 |
| Anxiety about ageing 6: ‘see grey hairs’ | .19 | −.02 | .76 | .05 |
| Anxiety about ageing 7: ‘someone else making decisions for me’ | .30 | .09 | .70 | .20 |
| Anxiety about ageing 8: ‘feel good about myself’ | .39 | .34 | .07 | .62 |
| Anxiety about ageing 9: ‘looking old’ | −.07 | .69 | .47 | .13 |
| Anxiety about ageing 10: ‘worry about my health’ | .12 | .24 | −.17 | .80 |
| Anxiety about ageing 11: ‘doesn't bother me’ | .27 | .57 | .54 | −.27 |
| Anxiety about ageing 12: ‘enjoy doing things for old people’ | .67 | .06 | −.10 | .03 |
| Cronbach's α | .76 | .68 | .50 | .35 |
| Percent variance explained | 26.56 | 16.63 | 12.09 | 9.62 |
Values in bold indicate the items that were used in each of the ‘anxiety about ageing’ subscales.
Data on hours of daily hearing aid use were generated automatically by the hearing aid(s) and downloaded at participants’ regular standard 10‐week follow‐up appointments. Objective hearing aid use data are collected routinely, but are not used in practice. Asking participants to state how many hours per day on average they had been using their hearing aid(s) served as a measure of subjective hearing aid use.
Procedure
Potential participants, identified from the new patient assessment clinic lists, were contacted by telephone for permission to send out information regarding the study. If verbal consent was given, then potential participants were sent information about the study by mail prior to their hearing assessment appointment. At the assessment appointment, potential participants were screened to see whether they fit the inclusion/exclusion criteria and to obtain written consent for the study. Once participants had signed the consent form following their assessment appointment, they were assigned to a condition by being given the next questionnaire from a pile that had been pre‐randomized by the researcher, which they completed immediately and alone. The only difference between the intervention and control conditions was the material that appeared on the last page of the questionnaire, namely the self‐affirmation manipulation. This meant that the person randomizing the questionnaires, the hearing care professionals, and the participants were all blind with respect to condition. Although the means of randomization could have been improved (e.g., through the use of opaque envelopes), the procedures were designed to be as close to routine practice as possible without significant additional burden on hearing care professionals or patients.
Following completion of the questionnaires, participants had their hearing aid fitted. To further minimize bias, audiologists performing the fitting appointments were not aware as to which group the participant was assigned. As per standard NHS procedures, decisions over unilateral or bilateral fittings, volume controls, programmes, and mould (customized or slim‐tube) fittings were jointly decided by the audiologist and the participant. All participants were prescribed and fitted with the Spirit Zest manufactured by Oticon (SmØrum, Denmark). The NHS purchases around 800,000 hearing aids every year, and the Spirit Zest was one of the most popular hearing aids at the time of the study. This model was available outside of the NHS where it was known as the Vigo Pro. This hearing aid was an eight‐channel behind‐the‐ear device, and the software allowed the gain to be modified at eight centre frequencies (0.25, 0.5, 1, 1.5, 2, 3, 4, and 6 kHz). The compression has an attack time ranging between 15 and 20 ms and a release time ranging between 200 and 400 ms.
Ten weeks post‐fitting, patients returned to the clinics for their standard routine follow‐up appointments. At follow‐up, participants completed questionnaires that included measures that were identical to the baseline measures of motivation and anxieties about ageing. Additionally, participants at follow‐up were asked to report how many hours they thought they had worn their hearing aid each day. Data were also downloaded from participants’ hearing aids to check for usage.
All equipments used for the assessment, fitting, and follow‐up appointments were carried out as per British Society of Audiology‐recommended procedures, and the appointments were conducted in accordance with national practice guidelines and are typical of audiology departments across the country. This ensured that all participants were receiving an equal high‐quality standard of care.
Sample size
According to Epton et al.'s (2015) meta‐analysis of self‐affirmation‐based interventions, the average weighted mean effect on behaviour was d = 0.32. G‐power software (Faul, Erdfelder, Lang, & Buchner, 2007) was used to calculate the required sample size. As the principal analyses required a one‐tailed t‐test, and assuming statistical power of 0.95 and an error probability of 0.05, the total required sample size for a fully powered randomized controlled trial was estimated to be N = 426. There are several views on the sample size required for a pilot study: Connelly (2008) suggests that pilots should aim to recruit 10% of the sample size required for the full study, Isaac and Michael (1995) recommend 10–30 participants, and Julious (2005) advocates 12 participants per arm. We therefore aimed to recruit a total of 50 participants to allow for attrition.
Data analysis
Principal components analysis with varimax rotation was used to assess the psychometric properties of the anxiety about ageing scale (Table 1). The effect of self‐affirmation on hearing aid use was tested using independent‐samples t‐tests. The effect of the manipulation on motivation and anxiety was tested initially using a series of mixed ANOVAs. Condition (control vs. intervention) was the between‐participants factor, and time (baseline vs. follow‐up) was the within‐persons factor. Significant interactions were decomposed by (1) between‐participants ANCOVAs controlling for baseline values and (2) within‐participants ANOVAs run separately for the intervention and control groups. Follow‐up data were missing completely at random, χ2(4) = 6.37, p = .17, and so where possible, the analyses were subject to intention to treat with the baseline observation carried forward.
Results
Feasibility
Three hundred and ninety‐one potential participants were identified from the new patient assessment clinic lists, of whom 374 gave verbal consent by telephone and were sent information about the study by mail prior to their hearing assessment appointment (Figure 1). At the assessment appointment, 324 potential participants were screened out, largely because they already had a hearing aid, n = 173; required immediate treatment, n = 38; or did not attend, n = 25. Acceptability of the approach we took is evidenced by there being just 15 of 324 (4.63%) participants who declined to take part (Figure 1). The baseline sample consisted of 25 men and 25 women aged between 40 and 90 years (M = 59.92, SD = 12.89) who were randomly allocated to the intervention (n = 25) or control (n = 25) condition (Table 2). There were 13 women (52%) in the intervention group and 12 women (48%) in the control group. Seventeen participants did not attend their 10‐week follow‐up appointment and so were lost to follow‐up (Figure 1).
Figure 1.
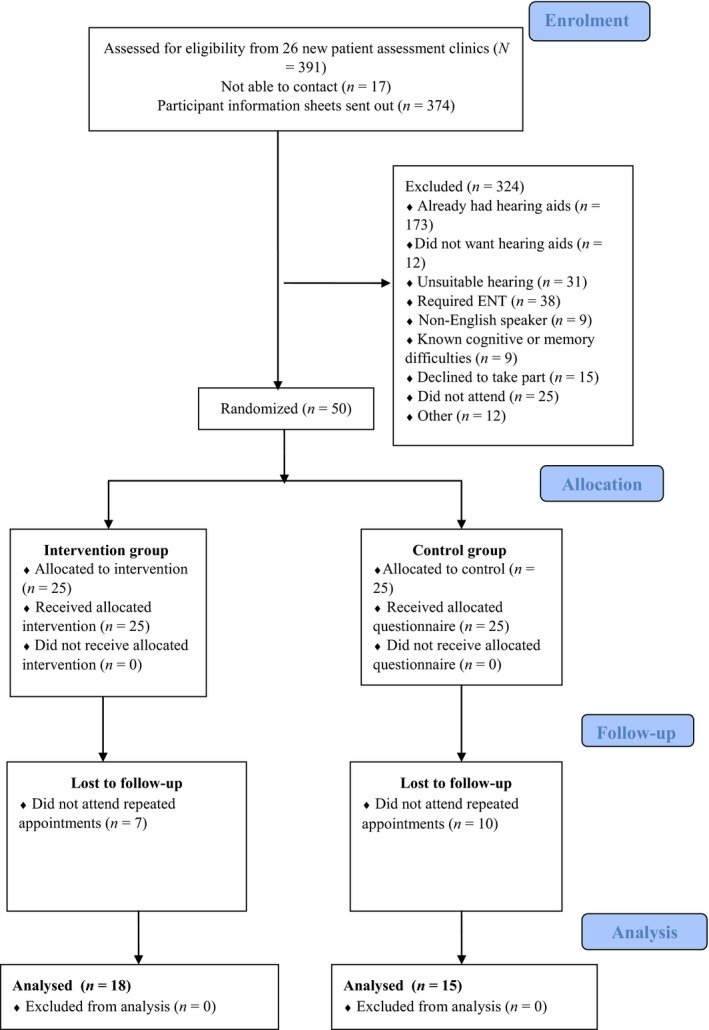
CONSORT diagram showing flow of participants through the trial. [Colour figure can be viewed at wileyonlinelibrary.com]
Table 2.
Baseline characteristics of the sample and effects of the intervention at follow‐up on motivation, anxiety about ageing, and hearing aid use
| Dependent variables | Baseline | Follow‐up | 95%CI | p | d | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Age (years) | |||||||
| Control | 67.44 | 13.51 | – | – | – | – | |
| Intervention | 71.60 | 12.15 | – | – | |||
| Hearing loss (best ear average 500–4,000 Hz) | |||||||
| Control | 34.85 | 8.97 | – | – | – | – | |
| Intervention | 36.90 | 9.73 | – | – | |||
| Behavioural intention | |||||||
| Control | 6.53 | 0.82 | 6.37 | 1.16 | .30 | .29 | |
| Intervention | 6.40 | 0.84 | 6.41 | 0.82 | |||
| Between‐group difference | 0.17 | −0.16, 0.51 | |||||
| Self‐efficacy | |||||||
| Control | 6.40 | 0.73 | 6.15 | 1.13 | .79 | .09 | |
| Intervention | 6.19 | 0.92 | 6.01 | 1.43 | |||
| Between‐group difference | −0.06 | −0.67, 0.55 | |||||
| Anxiety about ageing 1: ‘Fear of old people’ | |||||||
| Control | 5.33 | 1.31 | 4.90 | 1.43 | <.01 | .87 | |
| Intervention | 5.15 | 1.48 | 5.51 | 1.24 | |||
| Between‐group difference | 0.75 | 0.26, 1.23 | |||||
| Anxiety about ageing 2: ‘positive ageing’ | |||||||
| Control | 5.74 | 1.13 | 5.76 | 1.05 | .33 | .29 | |
| Intervention | 5.50 | 1.26 | 5.76 | 1.05 | |||
| Between‐group difference | 0.15 | −0.27, 0.57 | |||||
| Self‐reported hearing aid use (hr/day) | |||||||
| Control | – | – | 8.33 | 4.82 | .46 | .04 | |
| Intervention | – | – | 8.50 | 3.99 | |||
| Between‐group difference | 0.17 | −3.29, 2.96 | |||||
| Objective hearing aid use (hr/day) | |||||||
| Control | – | – | 6.32 | 4.64 | .11 | .43 | |
| Intervention | – | – | 8.26 | 4.31 | |||
| Between‐group difference | 1.94 | −1.24, 5.12 | |||||
Hearing aid use was measured post‐intervention only and so values are based on n = 15 participants in the control group and n = 18 participants in the intervention group at follow‐up; p‐values and d‐values are based on independent t‐tests. All other measures were taken at baseline and follow‐up using intention to treat (last observation carried forward); p‐values and d‐values are based on the interaction between condition and time computed following mixed ANOVAs. Mean values are ‘raw’ and unadjusted for baseline covariates except for between‐group differences and 95%CI, which adjust for baseline values. Lower scores on the anxiety about ageing scales denote greater anxiety and less acceptance of ageing.
Psychometric evaluation of principal measures
The principal components analysis of the anxiety about ageing scale items produced four factors according to Velicer's minimum average partial test, all of which had eigenvalues >1, and accounted for 68.94% of the variance (Table 1). The first factor included three items such as ‘I enjoy being around old people’, which mapped onto one of the subscales reported in Lasher and Faulkender's (1993) original study and concomitantly was labelled ‘fear of old people’ (Cronbach's α = .76). The second factor consisted of four items, including ‘I expect to feel good about life when I am old’, which was labelled ‘positive ageing’ (Cronbach's α = .68). The third and fourth factors consisted of two items each, but weak internal reliability (Cronbach's αs = .50 and .35) meant that these items were not considered further. Scrutiny of the zero‐order correlation between the ‘fear of old people’ and ‘positive ageing’ subscales revealed adequate discriminant validity (r = .37, p < .01). Lower scores on the scales denote greater anxiety and lower acceptance of ageing.
Effects of the manipulation
According to both subjective and objective hearing aid use data, participants in the intervention condition wore their hearing aids for longer than those in the control group (Table 2). Although these differences were not statistically significant, t subjective(31) = 0.11, p = .46; t objective(31) = 1.24, p = .11, it is notable that, objectively, participants in the intervention group wore their hearing aids for almost 2 hrs longer than those in the control group (Table 2) and that this effect approached what Cohen (1992) would describe as a ‘medium‐sized’ effect, d = 0.43.
The effects of the manipulation on behavioural intention, self‐efficacy, anxiety about ageing 1 (fear of old people), and anxiety about ageing 2 (positive ageing) were tested initially using a series of mixed ANCOVAs, but the only statistically significant effects were observed for anxiety about ageing 1 (fear of old people). Given the high baseline levels of behavioural intention (M = 6.47, SD = 0.82) and self‐efficacy (M = 6.29, SD = 0.83) as measured on +1 to +7 scales, it is perhaps unsurprising that these were unaffected by the manipulation. The following analyses therefore focus on anxiety about ageing 1 (fear of old people).
There was a significant interaction between condition and time for anxiety about ageing 1 (fear of old people), F(1, 48) = 9.34, p < .01, = .16, d = 0.87. Between‐participants ANCOVA controlling for baseline anxiety about ageing 1 (fear of old people) showed significant differences in anxiety about ageing 1 (fear of old people) between conditions at follow‐up, F(1, 50) = 9.53, p < .01, = .17, d = 0.90 (Table 2). Thus, participants in the experimental group experienced significantly lower anxiety about ageing 1 (fear of old people) at follow‐up. Within‐persons ANOVAs showed that the decreases in anxiety about ageing 1 (fear of old people) across time in the experimental group were non‐significant, F(1, 24) = 3.21, p = .09, = .12, d = 0.74, but that the increases in anxiety about ageing 1 (fear of old people) in the control group were significant, F(1, 24) = 6.94, p = .01, = .22, d = 1.06.
Discussion
Summary
This is the first study to have applied the concept of self‐affirmation to improve use of hearing aids. At the same time as addressing this important public health issue, we were also able to address limitations in a self‐affirmation literature that relies on self‐reports or proxy biomedical measures, student samples, and has yet to identify a consistent mediator of the effects of self‐affirming on behaviour change. The principal findings were that, despite being a pilot study trial, there was a trend for objectively measured hearing aid use to be higher in the intervention group than in the control group and that self‐affirming statistically significantly reduced patients’ anxieties about ageing. The following discussion considers the practical and theoretical implications of the findings.
Future trial
The present study was designed as a pilot study to see whether self‐affirming might improve hearing aid use among people having hearing aids fitted for the first time. Although the sample was not of sufficient size to be able to detect statistically significant effects, the effects favoured the intervention group, who wore their hearing aids for almost 2 hrs per day longer than people in the control group (M = 8.26, SD = 4.31 vs. M = 6.32, SD = 4.64). Moreover, the size of the effect (d = 0.43) was stronger than that found in a recent meta‐analysis of self‐affirmation‐based intervention studies (d = 0.32, Epton et al., 2015). The implication is that it would be valuable to carry out further feasibility testing and piloting prior to proceeding to a fully powered randomized controlled trial. Two issues in particular are worthy of further investigation. First, procedures for identifying potential participants were inefficient: The majority of the people who were approached initially did not meet our inclusion criteria because they already had hearing aids. Given that the present study demonstrated strong effects in terms of reducing anxiety about ageing, it would be valuable to try and recruit all attendees at clinics to see whether hearing aid use can also be optimized among people who already have a hearing aid. Second, 17 of 50 (34.0%) participants did not attend their routine 10‐week appointment and so were lost to follow‐up. Concurrent with the issue of wastage in the NHS through lack of hearing aid use (e.g., Action on Hearing Loss, 2014), non‐attendance at appointments extorts a cost from the NHS and it would be valuable to design interventions to maximize attendance at hearing aid appointments.
Implications for intervention
The present findings provide insight into the kinds of strategies that might not work in increasing hearing aid use. For example, it is notable that patients reported feeling highly motivated and very confident in their ability to use hearing aids as advised, with the majority of participants scoring maximum on both the behavioural intention and self‐efficacy scales. This is perhaps unsurprising given that all participants had recognized a hearing deficit, arranged a hearing assessment appointment, subsequently attended the appointment, and agreed to participate in the research. However, such high pre‐existing levels of motivation help to explain why previous intervention studies have typically found null effects (Barker et al., 2016). Typically, the studies in Barker et al.'s (2016) systematic review focused on boosting people's motivation to wear hearing aids, yet based on the current evidence, it does not seem that motivation is likely to be a problem for this population, at least at the 10‐week stage that currently constitutes the last routine contact with hearing care professionals. The implication is that future intervention efforts might best be focused on ensuring motivation is translated into action (e.g., by targeting volitional processes, see Gollwitzer, 1999), rather than on educating and motivating people. One possible avenue might be to develop a hearing aid use ‘volitional help sheet’ (Armitage, 2008). Volitional help sheets are tools that help people to form implementation intentions that help translate people's intentions into action and have been tested successfully in clinical settings, including emergency rooms (Armitage, Rahim, Rowe, & O'Connor, 2016) and commercial weight loss programmes (Armitage, Norman, Noor, Alganem, & Arden, 2014), but not yet in relation to hearing aid use. The advantage of volitional help sheets in relation to clinical practice is that they can be completed in fewer than five minutes and do not require input from a health care professional.
One key strategy for intervention might be to address ways in which patients’ anxieties about ageing might be ameliorated. Anxiety about ageing increased in the control group and decreased in the intervention group, although the effect in the control group was stronger. Consistent with Steele's (1988) theorizing, it suggests that self‐affirming serves a protective function and that, without intervention, the process of assessment and fitting for a hearing aid is perceived as threatening to patients (see also Armitage, 2016). Further research is needed to see what, in addition to self‐affirmation, could be done to reduce the threat perceived by patients. The findings also offer the intriguing possibility that combining self‐affirming statements with public health messages could increase help‐seeking and uptake of hearing assessments in the broader populace. Armitage and Arden (2016) tested this approach and showed that pairing a self‐affirming statement with the standard information on the labels of wine bottles significantly reduced subsequent alcohol consumption relative to a condition in which participants were exposed to wine bottles with standard labels only.
Limitations
Although the present study takes the literatures on increasing hearing aid adherence and self‐affirmation theory forward in important respects, it is important to highlight some limitations. First, as a pilot study, the present sample was not of sufficient size to be able to detect statistically significant effects and it is not clear how representative the current sample was. Nevertheless, it is notable that the size of the present effect (d = 0.43) is stronger than that found in a recent meta‐analysis of self‐affirmation‐based intervention studies (d = 0.32, Epton et al., 2015). Second, we were unable to replicate the factor structure of Lasher and Faulkender's (1993) anxiety about ageing measure and it would be valuable to test the observed effects with an alternative measure of anxiety about ageing. It is notable that other authors have similarly been unable to replicate Lasher and Faulkender's (1993) original factor structure (e.g., Rivera‐Ledesma, Lena, Rangel, & Sanchez‐Sosa, 2007). Nevertheless, the ability to reduce anxiety about ageing with this brief intervention could have far‐reaching benefits for people beyond the domain of hearing loss. Further research is required to identify additional interactions with health services that trigger anxieties about ageing, and whether self‐affirming in these contexts can similarly help to promote behaviour change.
Conclusion
This is the first study to have applied the concept of self‐affirmation to improve use of hearing aids. At the same time as addressing this important public health issue, we were also able to address limitations in a self‐affirmation literature that relies on self‐reports or proxy biomedical measures, student samples, and has yet to identify a consistent mediator of the effects of self‐affirming on behaviour change. This pilot study suggests that, subject to further feasibility testing and piloting, it might be valuable to proceed to a fully powered randomized controlled trial into the use of self‐affirmation to improve use of hearing aids, and provides insight into the likely effect size, recruitment, and attrition rates. At the same time, we were able to extend the self‐affirmation literature into a novel domain (hearing aid use) and to show that self‐affirmation not only can change objectively measured behaviour but may work by reducing anxiety.
Supporting information
Data S1. Personal Views and Opinions Questionnaire.
Acknowledgements
The authors declare no conflict of interests. This research was funded by Central Manchester University Hospitals NHS Foundation Trust, Trust Charitable Funds (Central Manchester University Hospitals NHS Foundation Trust Charity), and facilitated by the NIHR Manchester Biomedical Research Centre and the NIHR Greater Manchester: Clinical Research Network. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research, or the Department of Health. We would like to thank the audiologists at University Hospitals of South Manchester NHS Foundation Trust, Withington Community Hospital, United Kingdom, for their support in conducting this research, and Charlotte Garrett and Rebecca Hays for their help conducting the patient and public involvement workshop.
References
- Action on Hearing Loss . (2014). Statistics. Retrieved from https://www.actiononhearingloss.org.uk/your-hearing/about-deafness-and-hearing-loss/statistics.aspx
- Ajzen, I. (1991). The theory of planned behaviour. Organizational Behavior and Human Decision Processes, 50, 179–211. [Google Scholar]
- Armitage, C. J. (2008). A volitional help sheet to encourage smoking cessation: A randomized exploratory trial. Health Psychology, 27, 557–566. https://doi.org/10.1037/0278-6133.27.5.557 [DOI] [PubMed] [Google Scholar]
- Armitage, C. J. (2016). A brief psychological intervention to protect subjective well‐being in a community sample. Quality of Life Research, 25, 385–391. https://doi.org/10.1007/s11136-015-1076-6 [DOI] [PubMed] [Google Scholar]
- Armitage, C. J. , & Arden, M. A. (2016). Enhancing the effectiveness of alcohol warning labels with a self‐affirming implementation intention. Health Psychology, 35, 1159–1163. https://doi.org/10.1037/hea0000376 [DOI] [PubMed] [Google Scholar]
- Armitage, C. J. , & Conner, M. (2001). Efficacy of the theory of planned behaviour: A meta‐analytic review. British Journal of Social Psychology, 40, 471–499. https://doi.org/10.1348/014466601164939 [DOI] [PubMed] [Google Scholar]
- Armitage, C. J. , Harris, P. R. , & Arden, M. A. (2011). Evidence that self‐affirmation reduces alcohol consumption: Randomized exploratory trial with a new, brief means of self‐affirming. Health Psychology, 30, 633–641. https://doi.org/10.1037/a0023738 [DOI] [PubMed] [Google Scholar]
- Armitage, C. J. , Norman, P. , Noor, M. , Alganem, S. , & Arden, M. A. (2014). Evidence that a very brief psychological intervention boosts weight loss in a weight loss program. Behavior Therapy, 45, 700–707. https://doi.org/10.1016/j.beth.2014.04.001 [DOI] [PubMed] [Google Scholar]
- Armitage, C. J. , Rahim, W. A. , Rowe, R. , & O'Connor, R. C. (2016). An exploratory randomised trial of a simple, brief psychological intervention to reduce subsequent suicidal ideation and behaviour in patients admitted to hospital for self‐harm. British Journal of Psychiatry, 208, 470–476. https://doi.org/10.1192/bjp.bp.114.162495 [DOI] [PubMed] [Google Scholar]
- Armitage, C. J. , Rowe, R. , Arden, M. A. , & Harris, P. R. (2014). A brief psychological intervention that reduces adolescent alcohol consumption. Journal of Consulting and Clinical Psychology, 82, 546–550. https://doi.org/10.1037/a0035802 [DOI] [PubMed] [Google Scholar]
- Barker, F. , Mackenzie, E. , Elliott, L. , Jones, S. , & de Lusignan, S. (2016). Interventions to improve hearing aid use in adult auditory rehabilitation. Cochrane Database of Systematic Reviews, 7 Article no. CD010342. https://doi.org/10.1002/14651858.cd010342.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, D. (2015, January 3). NHS accursed of “cruel” rationing of hearing aids. The Observer Retrieved from https://www.theguardian.com/society/2015/jan/03/hearing-aids-supply-cuts-nhs-depression-dementia
- Cohen, J. (1992). A power primer. Psychological Bulletin, 112, 155–159. https://doi.org/10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Connelly, L. M. (2008). Pilot studies. Medsurg Nursing: Official Journal of the Academy of Medical‐Surgical Nurses, 17, 411–412. [PubMed] [Google Scholar]
- Coulson, N. S. , Ferguson, M. , Henshaw, H. , & Heffernan, E. (2016). Applying theories of health behaviour and change to hearing health research: Time for a new approach. International Journal of Audiology, 55(Suppl. 3), S99–S104. https://doi.org/10.3109/14992027.2016.1161851 [DOI] [PubMed] [Google Scholar]
- Cruickshanks, K. J. , Tweed, T. S. , Wiley, T. L. , Klein, B. E. K. , Klein, R. , Chappell, R. , … Dalton, D. S. (2003). The 5‐year incidence and progression of hearing loss – The Epidemiology of Hearing Loss Study. Archives of Otolaryngology‐Head and Neck Surgery, 129, 1041–1046. https://doi.org/10.1001/archotol.129.10.1041 [DOI] [PubMed] [Google Scholar]
- Dawes, P. , Maslin, M. , & Munro, K. J. (2014). ‘Getting used to’ hearing aids from the perspective of adult hearing‐aid users. International Journal of Audiology, 53, 861–870. https://doi.org/10.3109/14992027.2014.938782 [DOI] [PubMed] [Google Scholar]
- Epton, T. , Harris, P. R. , Kane, R. , van Koningsbruggen, G. M. , & Sheeran, P. (2015). The impact of self‐affirmation on health behavior change: A meta‐analysis. Health Psychology, 34, 187–196. https://doi.org/10.1037/hea0000116 [DOI] [PubMed] [Google Scholar]
- Faul, F. , Erdfelder, E. , Lang, A. G. , & Buchner, A. (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. https://doi.org/10.3758/BF03193146 [DOI] [PubMed] [Google Scholar]
- Gollwitzer, P. M. (1999). Implementation intentions – Strong effects of simple plans. American Psychologist, 54, 493–503. https://doi.org/10.1037//0003-066X.54.7.493 [Google Scholar]
- Isaac, S. , & Michael, W. B. (1995). Handbook in research and evaluation. San Diego, CA: Educational and Industrial Testing Services. [Google Scholar]
- Julious, S. A. (2005). Sample size of 12 per group rule of thumb for a pilot study. Pharmaceutical Statistics, 4, 287–291. https://doi.org/10.1002/pst.185 [Google Scholar]
- Lasher, K. P. , & Faulkender, P. J. (1993). Measurement of aging anxiety – development of the anxiety about aging scale. International Journal of Aging and Human Development, 37, 247–259. https://doi.org/10.2190/1u69-9au2-v6lh-9y1l [DOI] [PubMed] [Google Scholar]
- McCormack, A. , & Fortnum, H. (2013). Why do people fitted with hearing aids not wear them? International Journal of Audiology, 52, 360–368. https://doi.org/10.3109/14992027.2013.769066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie, S. , & Prestwich, A. (2010). Are interventions theory‐based? Development of a theory coding scheme. Health Psychology, 29, 1–8. https://doi.org/10.1037/a0016939 [DOI] [PubMed] [Google Scholar]
- Rivera‐Ledesma, A. , Lena, M. M. L. , Rangel, A. L. G. C. , & Sanchez‐Sosa, J. J. (2007). Lasher and Faulkender. Anxiety about ageing scale: Psychometric properties on Mexican elderly. Salud Mental, 30, 55–61. [Google Scholar]
- Steele, C. M. (1988). The psychology of self‐affirmation: Sustaining the integrity of the self In Berkowitz L. (Ed.), Advances in experimental social psychology (Vol. 21, pp. 261–302). New York, NY: Academic Press. [Google Scholar]
- WHO . (2002). Facts about deafness. Retrieved from https://www.who.int/pbd/deafness/facts/en/
- Wileman, V. , Farrington, K. , Chilcot, J. , Norton, S. , Wellsted, D. M. , Almond, M. , … Armitage, C. J. (2014). Evidence that self‐affirmation improves phosphate control in hemodialysis patients: A pilot cluster randomized controlled trial. Annals of Behavioral Medicine, 48, 275–281. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Personal Views and Opinions Questionnaire.


