Abstract
Purpose
Understanding the effectiveness of complex, face‐to‐face health behaviour change interventions requires high‐quality measures to assess fidelity of delivery and engagement. This systematic review aimed to (1) identify the types of measures used to monitor fidelity of delivery of, and engagement with, complex, face‐to‐face health behaviour change interventions and (2) describe the reporting of psychometric and implementation qualities.
Methods
Electronic databases were searched, systematic reviews and reference lists were hand‐searched, and 21 experts were contacted to identify articles. Studies that quantitatively measured fidelity of delivery of, and/or engagement with, a complex, face‐to‐face health behaviour change intervention for adults were included. Data on interventions, measures, and psychometric and implementation qualities were extracted and synthesized using narrative analysis.
Results
Sixty‐six studies were included: 24 measured both fidelity of delivery and engagement, 20 measured fidelity of delivery, and 22 measured engagement. Measures of fidelity of delivery included observation (n = 17; 38.6%), self‐report (n = 15; 34%), quantitatively rated qualitative interviews (n = 1; 2.3%), or multiple measures (n = 11; 25%). Measures of engagement included self‐report (n = 18; 39.1%), intervention records (n = 11; 24%), or multiple measures (n = 17; 37%). Fifty‐one studies (77%) reported at least one psychometric or implementation quality; 49 studies (74.2%) reported at least one psychometric quality, and 17 studies (25.8%) reported at least one implementation quality.
Conclusion
Fewer than half of the reviewed studies measured both fidelity of delivery of, and engagement with complex, face‐to‐face health behaviour change interventions. More studies reported psychometric qualities than implementation qualities. Interpretation of intervention outcomes from fidelity of delivery and engagement measurements may be limited due to a lack of reporting of psychometric and implementation qualities.
Statement of contribution.
What is already known on this subject?
Evidence of fidelity and engagement is needed to understand effectiveness of complex interventions
Evidence of fidelity and engagement are rarely reported
High‐quality measures are needed to measure fidelity and engagement
What does this study add?
Evidence that indicators of quality of measures are reported in some studies
Evidence that psychometric qualities are reported more frequently than implementation qualities
A recommendation for intervention evaluations to report indicators of quality of fidelity and engagement measures
Keywords: fidelity of delivery, engagement, measures, quality, psychometric, implementation, complex intervention, health, behaviour change
Background
Most interventions aimed at changing health behaviours are complex in that they contain multiple components (Campbell et al., 2000; Oakley et al., 2006). The effectiveness of face‐to‐face interventions depends on providers delivering the intervention as intended and participants engaging with the intervention. However, delivering interventions with fidelity of delivery and ensuring that participants engage with interventions are not easy to achieve (Glasziou et al., 2010; Hardeman et al., 2008; Lorencatto, West, Bruguera, & Michie, 2014; Michie et al., 2008). Furthermore, it is more difficult to ensure that complex interventions are delivered as intended and engaged with, than simple interventions (Dusenbury & Hansen, 2004; Greenhalgh et al., 2004).
To understand, and potentially improve, intervention effectiveness, it is necessary to measure the extent to which the intervention is delivered in line with the protocol (‘intervention fidelity’) and engaged with by participants. Although many conceptualizations of engagement have been proposed (Angell, Matthews, Barrenger, Watson, & Draine, 2014), in this review, the term ‘participant engagement’ is used as an umbrella term to encapsulate constructs of fidelity that relate to participants’ engagement with intervention content. This includes whether participants understand the intervention, whether they can perform the skills required by the intervention (‘intervention receipt’), and whether they use these skills in daily life (‘intervention enactment’) (Borrelli, 2011). In doing this, the review makes a clear distinction between providers’ behaviours (fidelity of delivery) and participants’ behaviours (engagement). Both fidelity of delivery and engagement are necessary to understand the effects of the intervention; if effects are not found, this may be due to low fidelity of delivery and/or engagement and is therefore not a test of the potential of the intervention components (‘active ingredients’) to bring about change (Borrelli, 2011; Durlak, 1998; Lichstein, Riedel, & Grieve, 1994).
Fidelity of delivery has been assessed by self‐report measures (Bellg et al., 2004), and by audio‐recording, which is considered to be the gold standard (Bellg et al., 2004; Borrelli, 2011; Lorencatto et al., 2014). Methods used to assess engagement include self‐report measures (Bellg et al., 2004; Burgio et al., 2001; Carroll et al., 2007), observation of skills (Burgio et al., 2001), and homework reviews (Bellg et al., 2004). Systematic reviews of measures used to monitor fidelity of delivery demonstrate that these measures have consistently been used in intervention research, in both educational (Maynard, Peters, Vaughn, & Sarteschi, 2013) and health settings (Rixon et al., 2016). For example, a review of 55 studies found that intervention receipt was mostly measured by assessing understanding and performance of skills (Rixon et al., 2016). Observational measures may provide a more valid representation of what is delivered than self‐report measures (Breitenstein et al., 2010) and avoid social desirability bias (Schinckus, Van den Broucke, Housiaux, & Consortium, 2014). However, observation is likely to require more time and resources (Breitenstein et al., 2010; Schinckus et al., 2014), and it may also change the behaviour of those being observed (McMahon, 1987; as cited in Moncher & Prinz, 1991).
To understand which components have been delivered and engaged with, suitable measures are needed. Researchers suggest that measures should be psychometrically robust, with good reliability and validity (Gearing et al., 2011; Glasgow et al., 2005; Lohr, 2002; Stufflebeam, 2000). Reliability is defined as achieving consistent results in different situations (Roberts, Priest, & Traynor, 2006), and validity is defined as measurement of the construct it aims to measure (Roberts et al., 2006). Previous reviews found that few studies reported information on the reliability or validity of fidelity or engagement methods. A systematic review of fidelity of delivery in after‐school programmes found that no studies reported reliability (Maynard et al., 2013), and a systematic review of intervention receipt in health research found that 26% of studies reported on reliability and validity (Rixon et al., 2016). This makes it difficult for researchers to fully interpret the quality of measures and therefore the results of intervention outcomes. In this review, we use the term ‘psychometric qualities’ to refer to the quality of the measures. Aspects of ‘psychometric qualities’ of measures in the fidelity literature include the following: using multiple, independent researchers to rate fidelity of delivery; calculating inter‐rater agreement of measurements; and randomly selecting data (Bellg et al., 2004; Borrelli, 2011; Breitenstein et al., 2010; Lorencatto, West, Seymour, & Michie, 2013).
It is also necessary to ensure that measures are easy to use in practice and to minimize missing responses, which are common in health care self‐report research (Shrive, Stuart, Quan, & Ghali, 2006). Researchers suggest that practicality and acceptability influence the extent to which measures are used in practice (Glasgow et al., 2005; Holmbeck & Devine, 2009; Lohr, 2002). Practicality is defined as whether the measure can be used despite limited resources (Bowen et al., 2009), for example, being short and easy to use, and reducing participant and provider burden (Glasgow et al., 2005; Lohr, 2002). Acceptability is defined as whether the measure is appropriate for those who will use it (Bowen et al., 2009), for example, by including alternative forms and language adaptations, and by ensuring that measures are easy to interpret (Lohr, 2002). In this review, we use the term ‘implementation qualities’ to refer to descriptions of how the measures were implemented in practice. Aspects of ‘implementation qualities’ of measures in the fidelity literature include time constraints, cost, and reactions to measurements (Breitenstein et al., 2010).
Previous reviews have identified the measures used to monitor fidelity of delivery of after‐school programmes (Maynard et al., 2013), evidence‐informed interventions (Slaughter, Hill, & Snelgrove‐Clarke, 2015), and the measures used to monitor intervention receipt in health care settings (Rixon et al., 2016). Furthermore, researchers have previously outlined some strengths and weaknesses of different measures of fidelity of delivery and engagement (e.g., Borrelli, 2011; Breitenstein et al., 2010; Moncher & Prinz, 1991). To the authors’ knowledge, no systematic reviews have been conducted to identify the measures used to monitor fidelity of delivery and engagement (including intervention receipt and enactment), in complex, face‐to‐face health behaviour change interventions. This review will also extend previous research by describing the reporting of both psychometric and implementation qualities of these measures. Synthesizing the psychometric and implementation qualities of fidelity of delivery and engagement measures is needed to determine the quality of measures and how easy they are to implement. ‘Health’ includes physical, mental, and social well‐being, as recommended by the World Health Organisation (WHO, 2017).
This review aimed to:
Identify the types of measures used to monitor (1) the fidelity of delivery of, and (2) engagement with, complex, face‐to‐face health behaviour change interventions.
Describe these measures as reported in terms of both psychometric and implementation qualities.
Methods
The search and screening strategies were developed using the methods advocated by the Cochrane Collaboration (Higgins & Green, 2011; Lefebvre, Manheimer, & Glanville, 2011). Eligibility criteria for considering studies were specified using the ‘Participants’, ‘Intervention’, and ‘Outcomes’ criteria from PICO (O'Connor, Green, & Higgins, 2011).
Inclusion criteria
Participants: Adults aged 18 and over.
Intervention: Complex, face‐to‐face behaviour change interventions aimed at improving health behaviours. Health is defined as physical, mental, or social well‐being (WHO, 1946; as cited in WHO, 2017). Other modes of intervention delivery, such as digital interventions, may have different issues in relation to fidelity of delivery and engagement; therefore, these were not included in this review.
Outcomes: Studies which described measures to monitor fidelity of delivery and/or engagement and reported outcomes for fidelity of delivery and/or engagement and intervention effectiveness using quantitative measures. Only quantitative studies were included to increase the ability to compare across studies.
Exclusion criteria
Review articles, articles not written in English, or articles not peer‐reviewed
Articles in which the intervention outcome could not be clearly distinguished from the engagement or fidelity of delivery outcome.
Search strategy
Five electronic databases (PubMed, ScienceDirect, PsycINFO, Embase, and CINAHL Plus) were searched from the inception of each database up to November 2015. Implementation Science was searched, and reference lists of relevant known reviews (Carroll et al., 2007; Durlak & DuPre, 2008; Toomey, Currie‐Murphy, Matthews, & Hurley, 2015) were screened to identify additional studies. After the initial search, reference lists of reviews identified from the search (Clement, Ibrahim, Crichton, Wolf, & Rowlands, 2009; Conn, Hafdahl, Brown, & Brown, 2008; Gucciardi, Chan, Manuel, & Sidani, 2013; Reynolds et al., 2014; Smith, Soubhi, Fortin, Hudon, & O'Dowd, 2012), relevant protocols (Gardner et al., 2014), and forward and backward searching of included studies were screened to identify further articles. The articles generated by this search strategy were sent to 21 experts to ask whether they knew of relevant articles that were missing from the search results.
Initial search terms were piloted and refined iteratively with sequential testing to identify false‐positive and false‐negative results and ensure that the search captured all relevant keywords. A subject librarian was consulted in the development of the search terms.
Free and mapped searches (using Medical Subject Heading Terms) were conducted. Boolean operators were used to construct a search incorporating all search terms when combination searches were not possible. Search outputs were filtered for English full texts, peer‐reviewed articles, adult participants and health topics. The final search strategy is in Appendix S1.
To access articles not available through the university library database, the authors were contacted or articles were accessed through library services.
This search strategy was not exhaustive, but was instead used to identify as many papers that measured and reported fidelity of delivery and/or engagement in sufficient depth to provide insight into the measures used.
Data collection and analysis
Study selection
One reviewer conducted the electronic searches and screened the reference lists of relevant articles. All identified titles and abstracts were downloaded and merged using EndNote. Duplicates were removed. Two reviewers independently screened all (1) titles, (2) abstracts, and (3) full texts against inclusion and exclusion criteria. Reviewers met after each stage to determine agreement and resolve discrepancies. Any articles which reviewers were unsure of were retained until data extraction, when more information was available (Higgins & Deeks, 2008). Inter‐rater reliability was assessed using percentage agreement and kappa statistics. Scores from both the initial search screening and additional search screening were combined to calculate agreement scores. For the title screening, researchers achieved 64.9% agreement (n = 802, two missing responses, kappa .49, PABAK .47). For the abstract screening, researchers achieved 68% agreement (n = 425, three missing responses, kappa .36, PABAK .36). For the full‐text screening, researchers achieved 71.8% agreement (n = 266; kappa = .46 and PABAK = .58). The full‐text kappa scores (Cohen, 1960) indicated fair agreement (Orwin, 1994; as cited in Higgins & Deeks, 2008). This might reflect the difficulty identifying relevant articles due to differences in terminology in studies. Information on fidelity of delivery and engagement was often reported in separate articles than those reporting intervention outcomes.
Data extraction
A data extraction form was developed using a combination of standardized forms: Guidelines International Network‐Evidence Tables Working Group intervention template (Guidelines International Network, 2002–2017) and the Oxford Implementation Index (Montgomery, Underhill, Gardner, Operario, & Mayo‐Wilson, 2013). Data on the measures used to monitor fidelity of delivery and engagement and results were extracted, along with any qualities of measures that were reported. Psychometric qualities and implementation qualities were not pre‐specified before data extraction; therefore, any information that was reported in the results and discussion section of the original articles in relation to the quality of the measures was extracted. As a minimum quality check (Centre for Reviews and Dissemination, University of York, 2009), an independent researcher checked 20% of data extraction forms. Minor errors of punctuation were identified; however, no further details were extracted, and therefore, one researcher extracted data from all studies.
Data synthesis
Narrative analysis was used to summarize the fidelity of delivery and engagement measures and the reporting of psychometric and implementation qualities by one researcher. If authors specified the type of engagement that they measured, for example, ‘intervention receipt’ or ‘intervention enactment’, these were reported separately within engagement. One researcher synthesized the information on methods. The extracts from the text that included descriptions of qualities were summarized, and the part of the procedure that the quality related to was recorded. Psychometric qualities included reliability (achieving consistent results in different situations; Roberts et al., 2006) and validity (measures what it aims to measure; Roberts et al., 2006). Implementation qualities included acceptability (appropriate for those who will use it; Bowen et al., 2009), practicality (can be used despite limited resources; Bowen et al., 2009), and cost. Researchers were open to other categories that may have emerged if qualities did not fit into these categories. Due to the heterogeneity of studies, a descriptive rather than quantitative synthesis of data was conducted (Deeks, Higgins, & Altman, 2008; Popay et al., 2006).
Two researchers were involved in the categorization of psychometric and implementation qualities. The first author coded 10% of the qualities and asked an independent researcher to check responses. Disagreements were identified, and both researchers independently coded an additional 10% of qualities. Researchers met after each round to discuss disagreements. This process was repeated, until 80% agreement on the categorization of features was reached, as recommended by Lombard, Snyder‐Duch, and Bracken (2002). After four rounds (40% of qualities were independently coded), reliability was achieved with 80.1% agreement between coders. The first author coded the rest of the qualities, based on discussions with the second researcher. Following this, the second researcher checked a further 10% of the researcher's independent coding and any qualities that the first author was unsure how to code.
Results
After duplicates were removed, 809 records were identified. Sixty‐six articles were included in the analysis (Figure 1).
Figure 1.
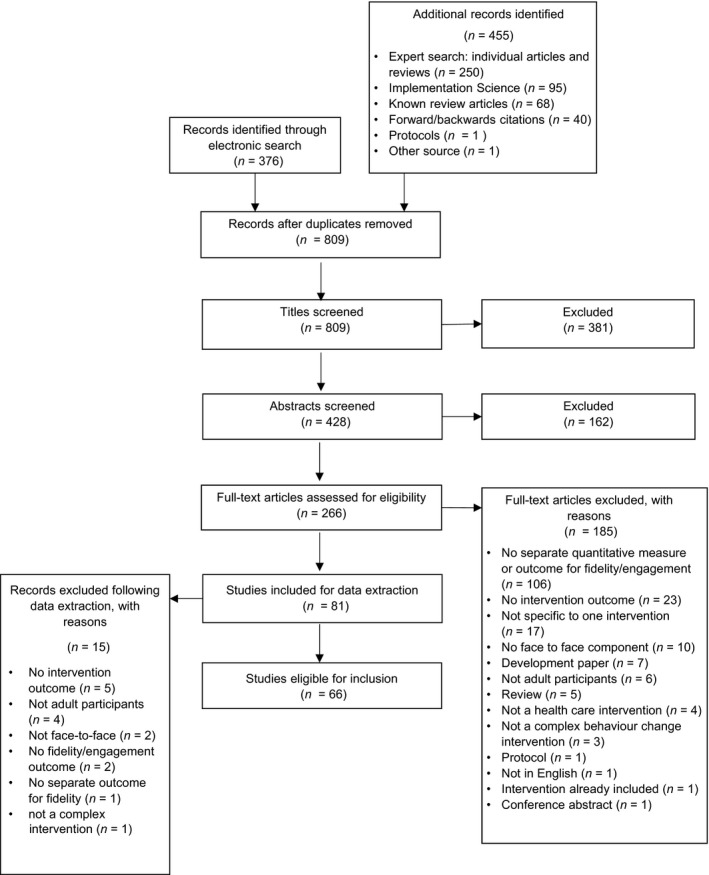
A flow diagram of the paper selection process (based on Moher, Liberati, Tetzlaff, and Altman's (2009) PRISMA flow diagram).
Study characteristics
Sixty‐six studies (100%) were included (for a list of studies and their characteristics, see Appendix S2). All of the included studies described fidelity of delivery and/or engagement measures, in relation to a complex, face‐to‐face health behaviour change intervention. Forty‐six studies (69.7%) were randomized controlled trials and 20 (30.3%) used non‐randomized designs. Settings included medical settings (n = 40; 60.6%), community settings (n = 20; 30.3%), and companies (n = 1; 1.5%). Five studies (7.6%) did not specify their setting. Intervention recipients were patients (n = 31; 47%), members of the public (n = 17; 25.8%), health care professionals and practices (n = 11; 16.7%), caregivers and care recipients (n = 4; 6.1%), and workers (n = 3; 4.5%). Target behaviours included multiple health behaviours (n = 35; 53%), self‐management skills (n = 11; 16.7%), clinician behaviours (n = 10; 15.2%), anxiety‐reducing behaviours (n = 3; 4.5%), work sickness absence (n = 2; 3%), caregiver skills (n = 2; 3%), treatment adherence (n = 1; 1.5%), patient resource use (n = 1; 1,5%), and activities of daily living (n = 1; 1.5%). Interventions were delivered by health care professionals (n = 33; 50%), people trained especially for the intervention (e.g., community mediators and outreach visitors) (n = 11; 16.7%), pharmacists (n = 2; 3%), postgraduate students (n = 2; 3%), and researchers (n = 4; 6%). Fourteen studies (21.2%) did not specify who delivered the intervention.
Measures used to monitor fidelity of delivery and engagement
Of all included studies, 44 (66.7%) assessed fidelity of delivery and 46 (69.7%) assessed engagement. Of these, 24 studies (36.4%) measured both fidelity of delivery and engagement, 20 (30.3%) measured fidelity of delivery only, and 22 (33.3%) measured engagement only (see Appendix S3).
Table 1 provides an overview of the methods, including a summary of what was measured, the measures used, who completed the measures, the sample, analysis method, and the number of studies that used a framework/model and provided definitions for fidelity and engagement. For further details about methods and a summary of results, please see Appendix S4.
Table 1.
A summary of the measures used to monitor fidelity of delivery and engagement
| Fidelity (n = 44; 100%) | Engagement (n = 46, 100%) | |
|---|---|---|
| What was measured? |
|
|
| Type of measures used |
Observational measures (n = 17; 38.6%):
Self‐report measures (n = 15; 34%):
Multiple measures (n = 11; 25%)
Other measures (n = 1; 2.3%)
|
Self‐report measures (n = 18; 39.1%)
Multiple measures (n = 17; 37%):
Intervention records (n = 11; 24%)
|
| More details about measures | Who completed the measures?
|
Who completed the measures?
|
Development of measures
|
Development of measures
|
|
Responses on measures
|
Responses on measures
|
|
| Sample | How many participants were sampled?
|
How many participants were sampled?
|
How were participants sampled?
|
How were participants sampled?
|
|
Which conditions were participants sampled from?
|
Which conditions were participants sampled from?
|
|
| Analysis method |
|
|
| Framework/model |
|
|
| Definitions |
|
|
(R) = receipt; (E) = enactment; (R&E) = receipt and enactment.
What was measured?
The majority of studies reporting measuring fidelity of delivery did so by measuring the delivery of intervention components against the intervention protocol (n = 20; 45.5%), adherence to motivational interviewing techniques (n = 6; 13.6%), and a combination of dose delivered and fidelity (n = 6; 13.6%). For engagement, there were a wide variety of measures, including adherence to target behaviour (n = 7; 15.2%), attendance (n = 7; 15.2%), understanding and use of intervention skills (n = 3; 6.5%), understanding and engagement (n = 2; 4.4%), compliance and attendance (n = 2; 4.4%), adherence to target behaviour and attendance (n = 2; 4.4%), and completion of study visits (n = 2; 4.4%). Please see Table 1 for a full list of what was measured.
Measures
Measures of fidelity of delivery were categorized into observational measures (n = 17; 38.6%), self‐report measures (n = 15; 34%), quantitatively rated qualitative interviews (n = 1; 2.3%), and multiple measures (n = 11; 25%). Of the studies that used multiple measures, six (14%) used at least one type of observational measure and nine (20.5%) used at least one type of self‐report measure. In total, 23 (52%) studies used at least one type of observational measure and 24 (55%) used at least one type of self‐report measure (see Table 1 for details).
Measures of engagement were categorized into self‐report measures (n = 18; 39.1%); intervention records (n = 11; 24%), for example, attendance monitoring; and multiple measures (n = 17, 37%). Of the studies that used multiple measures, 15 (32.6%) used at least one type of self‐report measure. In total, 33 (76.7%) studies used at least one type of self‐report measure (see Table 1 for details). Two studies reported measuring receipt and enactment6,39, and one study reported measuring receipt14 only.
Details of measures, sampling, and analysis
For fidelity of delivery, measures were completed by either the researcher (n = 18; 40.9%), provider (n = 11; 25%), or participant (n = 3; 6.8%); or both the provider and participant (n = 4; 9.1%), provider and researcher (n = 4; 9.1%), and participant and researcher (n = 2; 4.55%). It was not specified who completed the measures in two studies (4.55%).
For engagement, measures were completed by either the participant (n = 14; 30.4%), researcher (n = 13; 28.3%), or provider (n = 4; 8.7%); or both the participant and researcher (n = 6; 13%), provider and participant (n = 3; 6.5%), provider and researcher (n = 3; 6.5%), and the provider, participant, and researcher (n = 3; 6.5%).
The majority of studies (fidelity of delivery, n = 31; 70.45%; engagement, n = 42; 91.3%) did not report whether they developed their own measure or used a previously developed measure. For fidelity of delivery, eight (18.18%) used a previously developed measure and five (11.36%) developed their own measures. For engagement, three (6.5%) studies used previously developed measures and one (2.2%) developed own measures and used measures that were previously developed.
Many studies did not specify the type of scales used to quantify fidelity of delivery (n = 23; 52.3%) or engagement (n = 29; 63%). For fidelity of delivery, 12 studies (27.3%) reported using rating scales (which ranged from 3‐point scales to 10‐point scales), eight (18.2%) reported using dichotomous scales and one (2.3%) used rating scales and dichotomous scales. For engagement, 12 studies (26.1%) reported using rating scales (which ranged from 3‐point scales to 10‐point scales), three (6.5%) reported using dichotomous scales, and two (4.4%) reported using a combination of rating scales and dichotomous scales.
For both fidelity of delivery (n = 23; 52.3%) and engagement (n = 45; 97.8%), many studies did not specify how many participants they sampled. Five (11.4%) measured fidelity of delivery of all participants and 16 (36.4%) measured fidelity of delivery in a subsample of participants. Of those studies that measured fidelity of delivery in a subsample, four reported the number of sessions that they sampled, four reported the number of clinicians/sites data were sampled from, six reported the percentage of sessions that they sampled, and two did not specify how many but reported sampling some but not all participants. One (2.2%) study reported measuring engagement in a subsample of participants.
The sampling strategy used to measure fidelity of delivery included random sampling (n = 8; 18.2%), purposive sampling (n = 3; 6.8%), opportunity sampling (n = 1; 2.3%), stratified sampling (n = 1; 2.3%), self‐selected sampling (n = 1; 2.3%), not specified (n = 25; 56.8%), and not applicable for the studies that measured all participants (n = 5; 11.4%). No studies specified a sampling strategy for measuring engagement.
The majority of studies did not specify whether they measured fidelity of delivery (n = 38; 86.4%) or engagement (n = 35; 76.1%) in all conditions; therefore, it is likely they measured the intervention group only. Four (9.1%) reported measuring fidelity of delivery in all intervention groups, and two (4.5%) reported measuring fidelity of delivery in the intervention group only. Nine (19.6%) reported measuring engagement in all intervention groups, and two (4.3%) reported measuring engagement in the intervention group only.
For fidelity of delivery, 29 studies (65.9%) reported descriptive statistics, 11 (25%) reported descriptive and inferential statistics, and four (9.1%) did not report how they analysed the data. For engagement, 37 studies (80.4%) reported descriptive statistics and nine (19.6%) reported descriptive and inferential statistics.
Across all 66 studies, 13 (19.7%) reported using a fidelity framework.
Reporting of psychometric and implementation qualities
Studies
Of all included studies, 51 (77%) reported at least one psychometric or implementation quality of their measures (38 fidelity of delivery; 86.4%, 23 engagement; 50%).
Forty‐nine studies (74.2%) reported at least one psychometric quality, and 17 studies (25.8%) reported at least one implementation quality (see Table 2 for details).
Table 2.
Number of studies reporting psychometric and implementation qualities, across all studies (N = 66) and by studies reporting fidelity of delivery (N = 44) and engagement (N = 46)
| Psychometric qualities | Implementation qualities | ||||||
|---|---|---|---|---|---|---|---|
| Reported at least one quality | Validity | Reliability | Reported at least one quality | Practicality | Acceptability | Cost | |
| All studies; N (%) | 49 (74.2) | 41 (62) | 34 (52) | 17 (25.8) | 14 (21) | 6 (9) | 2 (3) |
| Fidelity of delivery; N (%) | 37 (84.1) | 31 (70.5) | 29 (65.9) | 12 (27.3) | 11 (25) | 5 (11.4) | 0 (0) |
| Engagement; N (%) | 21 (45.7) | 16 (34.8) | 10 (21.7) | 9 (19.6) | 6 (13.4) | 2 (4.3) | 2 (4.3) |
Psychometric and implementation qualities
In total, 261 (100%) reported qualities were identified (see Table 3 for details). Of these, 215 (82.4%) psychometric qualities were reported, 41 (15.7%) implementation qualities, and five (1.9%) both psychometric and implementation qualities; 213 qualities were reported in relation to fidelity of delivery measures and 58 qualities for engagement measures.
Table 3.
Number of times qualities were reported in total, and for fidelity of delivery and engagement
| Quality | Total number of times (%) | Category | Total number of times | Fidelity of delivery | Engagement |
|---|---|---|---|---|---|
| Psychometric quality | 215 (82.4) | Validity | 129 | 100 | 33 |
| Reliability | 85 | 75 | 14 | ||
| Reliability and validity | 1 | 1 | 0 | ||
| Implementation quality | 41 (15.7) | Practicality | 30 | 25 | 6 |
| Acceptability | 8 | 7 | 1 | ||
| Cost | 2 | 0 | 2 | ||
| Acceptability and practicality | 1 | 1 | 0 | ||
| Psychometric and Implementation quality | 5 (1.9) | Reliability and practicality | 1 | 1 | 0 |
| Validity and practicality | 3 | 2 | 1 | ||
| Validity and acceptability | 1 | 1 | 1 | ||
| Total | 261 (100) | ||||
The fidelity of delivery and engagement columns do not add up to 261 because 10 qualities were reported for both fidelity of delivery and engagement.
The most frequently reported psychometric qualities concerned the use of multiple researchers (n = 21: 3 data collection, 2 data analysis, 1 data entry, 3 develop measures, 11 coding, 1 validate coding frame), the validity of measures (n = 17: 9 valid, 8 not valid), the use of independent researchers (n = 16: 14 used independent researchers, 2 did not use independent researchers), reliability of measures (n = 11: 5 reliable, 6 not reliable), the random selection of data (n = 11: 9 randomly selected data, 2 did not randomly select data), and inter‐rater agreement (n = 9: 3 high inter‐rater agreement, 2 did not report inter‐rater agreement, 2 poor to fair, 1 fair to excellent, 1 no coder drift). Please see Table 4 for a detailed list of all psychometric qualities.
Table 4.
Qualities, category, and number of studies qualities were reported in
| Group of quality | Quality | Category | Number of studies reported in | Fidelity studies | Engagement studies |
|---|---|---|---|---|---|
| Psychometric qualities | |||||
| Use of multiple researchers | Coding | R | 11 | 20,26,27,29,33,34,45,51,58,64 | 47 |
| Data collection | 3 | 6,29,31 | |||
| Develop measures | 3 | 14,26,60 | |||
| Data analysis | 2 | 10,42 | |||
| Data entry | 1 | 26 | |||
| Validate coding frame | 1 | 26 | |||
| Validity of measures | Validated | V | 9 | 21,22,34,48,51 | 4,17,25,51 |
| Not validated | 8 | 2,10,34,35,41,42,50 | 13 | ||
| Use of independent researchers | Used – coding | R | 12 | 20,22,26,27,29,34,38,45,51,55,63,64 | |
| Not used – coding | 1 | 58 | |||
| Used – develop measures | 1 | 14 | |||
| Used – analysis | 1 | 42 | |||
| Not used | V | 1 | 20 | ||
| Measurement of conditions | All conditions (result output) | V | 8 | 7,50 | 4,13,17,18,51,53 |
| All conditions (reported) | 5 | 2,48,51 | 2,3,35 | ||
| Intervention only | 3 | 2,24 | 24,25 | ||
| Reliability of measures | Reliable | R | 6 | 21,22,48 | 4,17,51 |
| Not reliable | 5 | 2,14,23,34,50 | 2,23 | ||
| Random selection of data | Randomly selected | V | 9 | 31,40,51,55,57,58,63,64 | 52 (data entry) |
| Not randomly selected | 2 | 45,48 | |||
| Reporting of inter‐rater agreement | Reported – high | R | 3 | 26,59 | 17 |
| Not reported | 2 | 29,33 | |||
| Reported – poor to fair | 2 | 27,58 | |||
| Reported – fair to excellent | 1 | 58 | |||
| Reported – no coder drift | 1 | 26 | |||
| Coding of sessions | A percentage | V | 7 | 33,45,51,55,57,58,63 | |
| All | 1 | 27 | |||
| Calculated inter‐rater agreement | R | 8 | 20,26,27,29,33,58,59 | 17 | |
| Use of experts | Coding | V | 5 | 10,21,22,36,38 | |
| Develop measures | 1 | 27 | |||
| Not used – coding | 1 | 27 | |||
| Checked % of data input | R | 1 | 10 | ||
| Blinding | Coders | V | 3 | 7,26,48 | |
| Not blinded | 2 | 2 | 52 | ||
| Researchers | 1 | 15 | |||
| Participants | 1 | 2 | |||
| Measurement of content of intervention | Some aspects of intervention | V | 3 | 20,38 | 36,38 |
| All aspects of intervention | 2 | 33,63 | |||
| Problems with scoring criteria | Scoring criteria not sensitive | V | 2 | 20,26 | |
| No success cut‐off point | 1 | 14 | |||
| Dichotomized responses reduce variability | 1 | 25 | |||
| Measures may capture different aspects of fidelity | 1 | 26 | |||
| Standardization of procedure | Script | V | 2 | 34,66 | |
| Data entry | 1 | 52 | |||
| Coding guidelines | 1 | 64 | |||
| Not used standardized procedure | 1 | 33 | |||
| Not used standardized measure | 1 | 52 | |||
| Self‐report bias | V | 4 | 10,26,26,30 | ||
| R | 2 | 5 | 4 | ||
| Sampling | Across all providers | V | 2 | 27,45 | |
| Across all sites | 1 | 10 | |||
| Across all sites (purposively) | 1 | 33 | |||
| Across all participants | 1 | 27 | |||
| Balanced facilitator and gender (purposively) | 1 | 26 | |||
| Audit | Data collection | R | 1 | 6 | |
| Data analysis | 1 | 6 | |||
| Coding | 1 | 20 | 20 | ||
| Data entry | V | 1 | 23 | ||
| Recordings | 1 | 40 | |||
| Missing responses | Missing responses | V | 1 | 15 | |
| Trained researchers | Trained coders | V | 3 | 7,27,58 | |
| Trained researcher (data collection) | 1 | 52 | |||
| Observation effects | V | 4 | 22,26,27,34 | ||
| Use of one researcher | Coding | R | 1 | 38 | |
| Trained observers | 1 | 34 | |||
| Revised coding guidelines | R | 3 | 20,26,48 | ||
| V | 1 | 33 | |||
| Team meetings | R | 4 | 1,6,23,36 | 23 | |
| Recording of sessions | All sessions | V | 2 | 40,55 | |
| % of sessions | 1 | 35 | |||
| Triangulation | Method | V | 2 | 34,42 | |
| Researcher | 1 | 42 | |||
| Problems with analysis plan | Did not control for provider | V | 1 | 36 | |
| Missing responses excluded | 1 | 10 | |||
| Social desirability | V | 3 | 22 | 13,52 | |
| Objective verification | V | 2 | 15,43 | ||
| R | 1 | 12 | |||
| Used coding guidelines | R | 2 | 20,27 | ||
| Analysis consideration – coded missing responses as no adherence | V | 1 | 15 | ||
| Independently validated coding frame | V | 1 | 26 | ||
| Measurement differences – observation and self‐report | V | 1 | 26 | ||
| Measurement period – year after intervention | V | 1 | 25 | ||
| Piloted coding guidelines | V | 1 | 26 | ||
| Practice period before recording | V | 1 | 27 | ||
| Pre‐specified dates for recordings | V | 1 | 27 | ||
| Statistician involved in sampling (stratified) | V | 1 | 10 | ||
| Training before recording may overestimate adherence | V | 1 | 58 | ||
| Piloted measure | V | 1 | 34 | ||
| Provided a reason for inter‐rater agreement | R | 1 | 27 | ||
| Supervision | R | 1 | 58 | ||
| Measures were internally consistent indicating content validity | R+V | 1 | 27 | ||
| Implementation qualities | |||||
| Resource challenges | Time restrictions | P | 4 | 5,20,27,62 | |
| Technical difficulties | P | 3 | 5,5,58 | ||
| Financial restrictions | P | 2 | 5,27 | ||
| Sharing Dictaphones | P | 1 | 45 | ||
| Providers’ attitudes | Dislike paperwork | A | 1 | 10 | |
| Fear of discouraging participants | A | 1 | 27 | ||
| Nerves | A | 1 | 27 | ||
| Report participants behaving differently | A | 1 | 27 | ||
| Positive attitudes | A | 1 | 42 | ||
| Additional work | A | 1 | 62 | ||
| Not enthusiastic | A | 1 | 62 | ||
| Measurement of content of intervention | Telephone calls not assessed due to difficulty | P | 1 | 38 | |
| Measure cannot capture non‐verbal data | P | 1 | 20 | ||
| Problems with documentation | No record of responses | P | 2 | 10,58 | |
| Providers did not document everything | 1 | 10 | |||
| No record of refusals | A+P | 1 | 27 | ||
| Missing responses | Missing responses | P | 1 | 10,10 (different aspects) | |
| Problems with sampling | Low recruitment | P | 1 | 60 | |
| Problems with analysis plan | Analysis not feasible | P | 1 | 10 | |
| Incentives | Incentives used | P | 2 | 15,52 | |
| Incentives required | P | 1 | 62 | ||
| Feedback to providers | P | 2 | 21,27 | ||
| Feedback delay | P | 1 | 38 | ||
| Forgetting to return data | P | 1 | 15 | ||
| Logbook showed that not all steps were applied | P | 1 | 42 | ||
| Paper and digital version of measures given | P | 1 | 5 | ||
| Need simpler coding guidelines to achieve agreement | P | 1 | 27 | ||
| Reviewed fidelity after trial | P | 1 | 45 | ||
| Participants – dislike paperwork | A | 1 | 15 | ||
| Did not do a cost analysis | C | 1 | 13 | ||
| Cost of materials | C | 1 | 37 | ||
| Both psychometric and implementation qualities | |||||
| Problems with scoring criteria | Lack of clarity on items | V+P | 1 | 25 | |
| Missing responses | Missing responses | V+P | 1 | 58 | |
| Use of one researcher | Data collection | R+P | 2 | 5 | 52 |
| Problems with sampling | Selection bias | V+A | 1 | 2 | 2 |
| Not randomly selected | V+P | 1 | 27 | ||
This table is ordered by the number of studies that reported a quality that fits into the ‘group of quality’ column (e.g., ‘use of multiple researchers’). Most frequent → Least frequent. The numbers in this table will not add up to the total number of studies included, as some studies included information on multiple qualities.
R = reliability; V = validity; A = acceptability; P = practicality; C = cost.
The most frequently reported implementation qualities concerned resource challenges (n = 10: 1 sharing Dictaphones, 4 time restrictions, 2 financial restrictions, and 3 technical difficulties) and providers’ attitudes (n = 7: 1 dislike paperwork, 1 fear of discouraging participants, 1 nerves, 1 report participants behaving differently, 1 positive attitudes, 1 additional work) (see Table 4 for a list of all qualities).
Discussion
Key findings
Fewer than half of the reviewed studies measured both fidelity of delivery of and engagement with complex, face‐to‐face health behaviour interventions. Measures covered observation, self‐report, and intervention records. Whilst 73% reported at least one psychometric quality, only 26% reported at least one implementation quality.
How findings relate to previous research
The measures used to measure fidelity of delivery of, and engagement with, complex, face‐to‐face health behaviour change interventions were consistent with previous recommendations of using observational or self‐report measures to monitor fidelity of delivery, and self‐report measures to monitor engagement (Bellg et al., 2004; Borrelli, 2011; Burgio et al., 2001; Carroll et al., 2007; Schinckus et al., 2014). A similar percentage of studies used observational and self‐report measures to measure fidelity of delivery, despite observational measures being recommended as the gold‐standard measure and the reported limitations of self‐report measures (Bellg et al., 2004; Borrelli, 2011; Breitenstein et al., 2010; Lorencatto et al., 2014; Schinckus et al., 2014). Intervention records (e.g., attendance or homework) were also used to measure engagement. Intervention records can be considered an objective measure of receipt (Gearing et al., 2011; Rixon et al., 2016) and participation (Saunders, Evans, & Joshi, 2005). However, these measures are limited by their inability to monitor how much participants understand and use the intervention. Other recommended and potentially more objective measures, for example, asking participants to demonstrate skills (Burgio et al., 2001), were not adopted by any study in this review. Perhaps these findings demonstrate that measures need to be easy to use and acceptable to respondents and researchers in order to be selected for use. This explanation is consistent with previous studies which suggest that observational measures are perceived to be more expensive, time‐consuming and difficult to use (Breitenstein et al., 2010; Schinckus et al., 2014). Many studies used measures of fidelity of delivery and engagement specific to one intervention, and therefore, generalizability is limited (Breitenstein et al., 2010).
This review found that three quarters of studies reported at least one quality of their measures. This finding demonstrates that the reporting of psychometric qualities in the complex, face‐to‐face health behaviour change interventions included in this review, may not be as infrequent as previously suggested in different populations (Baer et al., 2007; Breitenstein et al., 2010; Maynard et al., 2013; Rixon et al., 2016). However, not all studies reported psychometric qualities, and fewer reported implementation qualities, despite the importance of psychometric and implementation qualities (Gearing et al., 2011; Glasgow et al., 2005; Holmbeck & Devine, 2009; Lohr, 2002; Stufflebeam, 2000). The reporting of psychometric and implementation qualities provides information which allows the reader to determine whether the findings are trustworthy and representative. Given this, it is difficult to draw conclusions with high certainty about how well interventions have been delivered or engaged with. This, in turn, makes it difficult to draw conclusions about intervention effectiveness.
The psychometric qualities that were most frequently reported were those recommended by previous research; examples of these are the use of multiple, independent researchers to reliably rate a random percentage of sessions for fidelity of delivery (Bellg et al., 2004; Borrelli, 2011; Lorencatto et al., 2014). However, some qualities which are recommended by research were not frequently reported; an example of this is routine audio‐recording (Gresham, Gansle, & Noell, 1993; Miller & Rollnick, 2014). The implementation qualities that were most frequently reported were those concerning resources (including time constraints, financial constraints, and technical difficulties) and providers’ attitudes towards measures. These findings could explain why missing responses were reported in some of the studies included in this review (Arends et al., 2014; Chesworth et al., 2015; Dubbert, Cooper, Kirchner, Meydrech, & Bilbrew, 2002; Thyrian et al., 2010) and health care research (Shrive et al., 2006). Providers may not return audio‐recordings (Weissman, Rounsaville, & Chevron, 1982) or checklists, if they feel uncomfortable with audio‐recording or if they are overwhelmed with paperwork.
Limitations
The aim of this review was to identify a range of studies that met the criteria and reported fidelity of delivery and/or engagement in enough depth to be able to draw conclusions about the reporting of fidelity of delivery and/or engagement measures. To identify as many studies as possible, a comprehensive search was conducted, which included contacting experts and authors to identify further relevant articles that may have been missed by the search strategy. However, we will not have identified articles that did not report monitoring fidelity of delivery or engagement in titles, abstracts, or keywords. A further reason why relevant articles may have been missed is that many terms are used interchangeably in fidelity research and we may not have captured all of these terms in the search strategy. We only included articles that reported a clear fidelity of delivery or engagement measure or outcome. As is the case with many systematic reviews, the search is inevitably limited to its date cut‐off. However, future use of natural language processing, ontologies, and machine learning (Larsen et al., 2016) will enable more ongoing updating when aggregating review evidence (see www.humanbehaviourchange.org).
The findings from this review consider the reporting of qualities and not the actual quality of measures. The review findings do not consider strengths or weaknesses of these qualities nor how much weighting should be given to each quality when designing fidelity of delivery and engagement measures. This is an area that could be investigated, building on the current review.
Implications
There are three main implications of these review findings for researchers and intervention developers:
The need to fully report details of fidelity of delivery and engagement measures. The findings from this review demonstrated that many studies did not specify details about the sampling or analysis method used in developing measures of fidelity of delivery and or engagement. If this information is not available, evaluation and replication are difficult to achieve.
The need to report both psychometric and implementation qualities for fidelity of delivery and engagement measures. The reporting of psychometric and implementation qualities would be helpful to researchers who are aiming to measure fidelity of delivery or engagement. This information would allow evaluations of what measures and procedures may be feasible.
The need to develop high‐quality measures of fidelity of delivery and engagement that are acceptable and practical to use but also reliable and valid. Both psychometric and implementation qualities of measures are relevant when selecting, developing, and reporting measures.
If implemented, these steps could help to strengthen the quality of fidelity of delivery and engagement data and the interpretation of intervention effectiveness.
Future research
Further research is needed to evaluate the importance and weighting of each quality when designing fidelity of delivery and engagement measures. One way to do this could be to conduct a Delphi study with experts in intervention fidelity and engagement. This systematic method could be used for building a consensus (Hsu & Sandford, 2007) regarding which psychometric and implementation qualities are most important, and which qualities should be given the most weighting when developing and evaluating fidelity of delivery and engagement measures. This information could then to be used to inform the development of measures of fidelity of delivery and engagement that are reliable, valid, acceptable, and practical. Future systematic reviews could explore the qualities of fidelity and engagement measures reported in qualitative studies.
Conclusion
Fewer than half of the reviewed studies measured both fidelity of delivery of and engagement with complex, face‐to‐face health behaviour change interventions. Measures covered observation, self‐report, and intervention records. Whilst 74% reported at least one psychometric quality, only 26% reported at least one implementation quality. Findings suggest that implementation qualities are reported less frequently than psychometric qualities. The findings from this review highlight the need for researchers to report measures of fidelity of delivery and engagement in detail, to report psychometric and implementation qualities, and to develop, use, and report high‐quality measures. This would strengthen the quality of fidelity of delivery and engagement data and the interpretation of intervention effectiveness.
Funding
Holly Walton's PhD is funded by the Economic and Social Research Council (ESRC) Doctoral Training Centre (Grant reference: ES/J500185/1). Ildiko Tombor's post is funded by a programme grant from Cancer Research UK. The funding bodies played no role in designing, conducting, analysing, interpreting or reporting the results of the review.
Conflict of interest
The authors declare no conflict of interests.
Compliance with ethical standards
This research is a review and did not involve research with human participants or animals.
Supporting information
Appendix S1. Search strategy.
Appendix S2. Characteristics of included studies.
Appendix S3. The proportion of studies which measured fidelity of delivery, engagement, or both.
Appendix S4. Details extracted from the papers on fidelity of delivery, and engagement methods and results.
Acknowledgements
Thank you to Jacqui Smith, librarian at University College London, for helping to build and check the search strategy, Olga Perski for her help with screening the identified articles, and Charlotte Stoner for her help with reviewing the data extraction forms and grouping indicators of quality.
References
Note: Included studies marked with *Study number.
- Angell, B. , Matthews, E. , Barrenger, S. , Watson, A. C. , & Draine, J. (2014). Engagement processes in model programs for community reentry from prison for people with serious mental illness. International Journal of Law and Psychiatry, 37, 490–500. https://doi.org/10.1016/j.ijlp.2014.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apter, A. J. , Wang, X. , Bogen, D. K. , Rand, C. S. , McElligott, S. , Polsky, D. , … Have, T.T. (2011). Problem solving to improve adherence and asthma outcomes in urban adults with moderate or severe asthma: A randomized controlled trial. Journal of Allergy and Clinical Immunology, 128, 516–523. e515. https://doi.org/10.1016/j.jaci.2011.05.010*1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arends, I. , Bültmann, U. , Nielsen, K. , van Rhenen, W. , de Boer, M. R. , & van der Klink, J. J. (2014). Process evaluation of a problem solving intervention to prevent recurrent sickness absence in workers with common mental disorders. Social Science and Medicine, 100, 123–132. https://doi.org/10.1016/j.socscimed.2013.10.041*2 [DOI] [PubMed] [Google Scholar]
- Baer, J. S. , Ball, S. A. , Campbell, B. K. , Miele, G. M. , Schoener, E. P. , & Tracy, K. (2007). Training and fidelity monitoring of behavioral interventions in multi‐site addictions research. Drug and Alcohol Dependence, 87, 107–118. https://doi.org/10.1016/j.drugalcdep.2006.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey, W. C. , Richards, J. M. , Brooks, C. M. , Soong, S.‐J. , Windsor, R. A. , & Manzella, B. A. (1990). A randomized trial to improve self‐management practices of adults with asthma. Archives of Internal Medicine, 150, 1664–1668. https://doi.org/10.1001/archinte.1990.00040031664013*4 [PubMed] [Google Scholar]
- Baker, K. R. , Nelson, M. E. , Felson, D. T. , Layne, J. E. , Sarno, R. , & Roubenoff, R. (2001). The efficacy of home based progressive strength training in older adults with knee osteoarthritis: A randomized controlled trial. The Journal of Rheumatology, 28(7), 1655–1665.*3 [PubMed] [Google Scholar]
- Baranowski, T. , & Stables, G. (2000). Process evaluations of the 5‐a‐day projects. Health Education and Behavior, 27(2), 157–166. https://doi.org/10.1177/109019810002700202 [DOI] [PubMed] [Google Scholar]
- Bellg, A. J. , Borrelli, B. , Resnick, B. , Hecht, J. , Minicucci, D. S. , Ory, M. , … Czajkowski, S. (2004). Enhancing treatment fidelity in health behavior change studies: Best practices and recommendations from the NIH Behavior Change Consortium. Health Psychology, 23(5), 443–451. https://doi.org/10.1037/0278-6133.23.5.443 [DOI] [PubMed] [Google Scholar]
- Binkley, C. J. , Johnson, K. W. , Abadi, M. , Thompson, K. , Shamblen, S. R. , Young, L. , & Zaksek, B. (2014). Improving the oral health of residents with intellectual and developmental disabilities: An oral health strategy and pilot study. Evaluation and Program Planning, 47, 54–63. https://doi.org/10.1016/j.evalprogplan.2014.07.003*5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black, K. (2014). Establishing empirically‐informed practice with caregivers: Findings from the CARES program. Journal of Gerontological Social Work, 57, 585–601. https://doi.org/10.1080/01634372.2013.865696*6 [DOI] [PubMed] [Google Scholar]
- Borrelli, B. (2011). The assessment, monitoring, and enhancement of treatment fidelity in public health clinical trials. Journal of Public Health Dentistry, 71(Suppl. 1), S52–S63. https://doi.org/10.1111/j.1752-7325.2011.00233.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen, D. J. , Kreuter, M. , Spring, B. , Cofta‐Woerpel, L. , Linnan, L. , Weiner, D. , … Fernandez, M. (2009). How we design feasibility studies. American Journal of Preventive Medicine, 36(5), 452–457. https://doi.org/10.1016/j.amepre.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breitenstein, S. M. , Gross, D. , Garvey, C. A. , Hill, C. , Fogg, L. , & Resnick, B. (2010). Implementation fidelity in community‐based interventions. Research in Nursing and Health, 33, 164–173. https://doi.org/10.1002/nur.20373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brug, J. , Spikmans, F. , Aartsen, C. , Breedveld, B. , Bes, R. , & Fereira, I. (2007). Training dietitians in basic motivational interviewing skills results in changes in their counseling style and in lower saturated fat intakes in their patients. Journal of Nutrition Education and Behavior, 39(1), 8–12. https://doi.org/10.1016/j.jneb.2006.08.010*7 [DOI] [PubMed] [Google Scholar]
- Burgio, L. , Corcoran, M. , Lichstein, K. L. , Nichols, L. , Czaja, S. , Gallagher‐Thompson, D. , … for the REACH Investigators. (2001). Judging outcomes in psychosocial interventions for dementia caregivers: The problem of treatment implementation. The Gerontologist, 41(4), 481–489. https://doi.org/10.1093/geront/41.4.481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler, C. C. , Simpson, S. A. , Dunstan, F. , Rollnick, S. , Cohen, D. , Gillespie, D. , … Hood, K. (2012). Effectiveness of multifaceted educational programme to reduce antibiotic dispensing in primary care: Practice based randomised controlled trial. BMJ, 344, d8173 https://doi.org/10.1136/bmj.d8173*8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, M. , Fitzpatrick, R. , Haines, A. , Kinmonth, A. L. , Sandercock, P. , Spiegelhalter, D. , & Tyrer, P. (2000). Framework for design and evaluation of complex interventions to improve health. BMJ, 321, 694–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, N. C. , Ritchie, L. D. , Thain, J. , Deans, H. G. , Rawles, J. M. , & Squair, J. L. (1998). Secondary prevention in coronary heart disease: A randomised trial of nurse led clinics in primary care. Heart, 80, 447–452. https://doi.org/10.1136/hrt.80.5.447*9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll, C. , Patterson, M. , Wood, S. , Booth, A. , Rick, J. , & Balain, S. (2007). A conceptual framework for implementation fidelity. Implementation Science, 2(1), 40 https://doi.org/10.1186/1748-5908-2-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centre for Reviews and Dissemination, University of York (2009). Systematic reviews. CRD's guidance for undertaking reviews in healthcare. York: York Publishing Services Ltd. [Google Scholar]
- Chesworth, B. M. , Leathley, M. J. , Thomas, L. H. , Sutton, C. J. , Forshaw, D. , & Watkins, C. L. (2015). Assessing fidelity to treatment delivery in the ICONS (Identifying Continence OptioNs after Stroke) cluster randomised feasibility trial. BMC Medical Research Methodology, 15, 68 https://doi.org/10.1186/s12874-015-0051-9*10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung, K. S.‐L. , Lau, B. H.‐P. , Wong, P. W.‐C. , Leung, A. Y.‐M. , Lou, V. W. , Chan, G. M.‐Y. , & Schulz, R. (2015). Multicomponent intervention on enhancing dementia caregiver well‐being and reducing behavioral problems among Hong Kong Chinese: A translational study based on REACH II. International Journal of Geriatric Psychiatry, 30, 460–469. https://doi.org/10.1002/gps.4160*11 [DOI] [PubMed] [Google Scholar]
- Clement, S. , Ibrahim, S. , Crichton, N. , Wolf, M. , & Rowlands, G. (2009). Complex interventions to improve the health of people with limited literacy: A systematic review. Patient Education and Counseling, 75, 340–351. https://doi.org/10.1016/j.pec.2009.01.008 [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1960). A coefficient of agreement for nominal scales. Educational and Psychological Measurement, 20(1), 37–46. [Google Scholar]
- Conn, V. S. , Hafdahl, A. R. , Brown, S. A. , & Brown, L. M. (2008). Meta‐analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Education and Counseling, 70(2), 157–172. https://doi.org/10.1016/j.pec.2007.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannhauser, T. M. , Cleverley, M. , Whitfield, T. J. , Fletcher, B. , Stevens, T. , & Walker, Z. (2014). A complex multimodal activity intervention to reduce the risk of dementia in mild cognitive impairment‐ThinkingFit: Pilot and feasibility study for a randomized controlled trial. BMC Psychiatry 14, ArtID 129, 14. https://doi.org/10.1186/1471-244x-14-129*12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks, J. J. , Higgins, J. P. T. , & Altman, D. G. (2008). Chapter 9: Analysing data and undertaking meta‐analyses In Higgins J. P. T. & Green S. (Eds.), Cochrane handbook for systematic reviews of interventions, version 5.0.1 [updated September 2008]. The Cochrane Collaboration; Retrieved from https://www.cochrane-handbook.org [Google Scholar]
- DeWalt, D. A. , Malone, R. M. , Bryant, M. E. , Kosnar, M. C. , Corr, K. E. , Rothman, R. L. , … Pignone, M. P. (2006). A heart failure self‐management program for patients of all literacy levels: A randomized, controlled trial ISRCTN11535170. BMC Health Services Research, 6(1), 30 https://doi.org/10.1186/1472-6963-6-30*13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driessen, M. , Proper, K. , Anema, J. , Bongers, P. , & van der Beek, A. (2010). Process evaluation of a participatory ergonomics programme to prevent low back pain and neck pain among workers. Implementation Science, 5(1), 65 https://doi.org/10.1186/1748-5908-5-65*14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubbert, P. M. , Cooper, K. M. , Kirchner, K. A. , Meydrech, E. F. , & Bilbrew, D. (2002). Effects of nurse counseling on walking for exercise in elderly primary care patients. Journals of Gerontology Series a‐Biological Sciences and Medical Sciences, 57A(11), M733–M740. https://doi.org/10.1093/gerona/57.11.M733 *15 [DOI] [PubMed] [Google Scholar]
- Duff, J. , Walker, K. , Omari, A. , Middleton, S. , & McInnes, E. (2013). Educational outreach visits to improve nurses’ use of mechanical venous thromboembolism prevention in hospitalized medical patients. Journal of Vascular Nursing, 31(4), 139–149. https://doi.org/10.1016/j.jvn.2013.04.002*16 [DOI] [PubMed] [Google Scholar]
- Duncan, K. , & Pozehl, B. (2003). Effects of an exercise adherence intervention on outcomes in patients with heart failure. Rehabilitation Nursing: The Official Journal of the Association of Rehabilitation Nurses, 28(4), 117–122. https://doi.org/10.1002/j.2048-7940.2003.tb01728.x*17 [DOI] [PubMed] [Google Scholar]
- Durlak, J. A. (1998). Why program implementation is important. Journal of Prevention & Intervention in the Community, 17(2), 5–18. https://doi.org/10.1300/J005v17n02_02 [Google Scholar]
- Durlak, J. A. , & DuPre, E. P. (2008). Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. American Journal of Community Psychology, 41, 327–350. https://doi.org/10.1007/s10464-008-9165-0 [DOI] [PubMed] [Google Scholar]
- Dusenbury, L. , & Hansen, W. B. (2004). Pursuing the course from research to practice. Prevention Science, 5(1), 55–59. https://doi.org/10.1023/B:PREV.0000013982.20860.19 [DOI] [PubMed] [Google Scholar]
- Ettinger, W. H. , Burns, R. , Messier, S. P. , Applegate, W. , Rejeski, W. J. , Morgan, T. , … Craven, T. (1997). A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: The Fitness Arthritis and Seniors Trial (FAST). JAMA, 277(1), 25–31. https://doi.org/10.1001/jama.1997.03540250033028*18 [PubMed] [Google Scholar]
- Farmer, A. , Wade, A. , Goyder, E. , Yudkin, P. , French, D. , Craven, A. , … Neil, A. (2007). Impact of self‐monitoring of blood glucose in the management of patients with non‐insulin treated diabetes: Open parallel group randomised trial. BMJ, 335, 132 https://doi.org/10.1136/bmj.39247.447431.BE*19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- French, S. D. , Green, S. E. , Francis, J. J. , Buchbinder, R. , O'Connor, D. A. , Grimshaw, J. M. , & Michie, S. (2015). Evaluation of the fidelity of an interactive face‐to‐face educational intervention to improve general practitioner management of back pain. British Medical Journal Open, 5, e007886 https://doi.org/10.1136/bmjopen-2015-007886*20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabbay, R. A. , Añel-Tiangco, R. M. , Dellasega, C. , Mauger, D. T. , Adelman, A. , & Van Horn, D. H. (2013). 糖尿病护士病例管理以及促进改变的动机性会谈(DYNAMIC: 一项为期 2 年的实用随机对照研究 [Diabetes nurse case management and motivational interviewing for change (DYNAMIC): Results of a 2‐year randomized controlled pragmatic trial]. Journal of Diabetes, 5, 349–357. https://doi.org/10.1111/1753-0407.12030*21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner, B. , Thune-Boyle, I. , Iliffe, S. , Fox, K. R. , Jefferis, B. J. , Hamer, M. , … Wardle, J. (2014). ‘On Your Feet to Earn Your Seat’, a habit‐based intervention to reduce sedentary behaviour in older adults: Study protocol for a randomized controlled trial. Trials, 15(1), 368 https://doi.org/10.1186/1745-6215-15-368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gearing, R. E. , El-Bassel, N. , Ghesquiere, A. , Baldwin, S. , Gillies, J. , & Ngeow, E. (2011). Major ingredients of fidelity: A review and scientific guide to improving quality of intervention research implementation. Clinical Psychology Review, 31(1), 79–88. https://doi.org/10.1016/j.cpr.2010.09.007 [DOI] [PubMed] [Google Scholar]
- Glasgow, R. E. , Ory, M. G. , Klesges, L. M. , Cifuentes, M. , Fernald, D. H. , & Green, L. A. (2005). Practical and relevant self‐report measures of patient health behaviors for primary care research. The Annals of Family Medicine, 3, 73–81. https://doi.org/10.1370/afm.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasziou, P. , Chalmers, I. , Altman, D. G. , Bastian, H. , Boutron, I. , Brice, A. , … Williams, J. W. (2010). Taking healthcare interventions from trial to practice. BMJ, 341, 384–387. https://doi.org/10.1136/bmj.c3852 [DOI] [PubMed] [Google Scholar]
- Goyder, E. , Hind, D. , Breckon, J. , Dimairo, M. , Minton, J. , Everson-Hock, E. , … Horspool, K. (2014). A randomised controlled trial and cost‐effectiveness evaluation of ‘booster'interventions to sustain increases in physical activity in middle‐aged adults in deprived urban neighbourhoods. Health Technology Assessment, 18(3), 1–209. https://doi.org/10.3310/hta18130*22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh, T. , Robert, G. , Bate, P. , Kyriakidou, O. , Macfarlane, F. , & Peacock, R. (2004). A systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation. How to spread good ideas, 1–424. [Google Scholar]
- Gresham, F. M. , Gansle, K. A. , & Noell, G. H. (1993). Treatment integrity in applied behaviour analysis with children. Journal of Applied Behaviour Analysis, 26, 257–263. https://doi.org/10.1901/jaba.1993.26-257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin, S. F. , Wilcox, S. , Ory, M. G. , Lattimore, D. , Leviton, L. , Castro, C. , … Rheaume, C. (2010). Results from the Active for Life process evaluation: Program delivery fidelity and adaptations. Health Education Research, 25(2), 325–342. https://doi.org/10.1093/her/cyp017*23 [DOI] [PubMed] [Google Scholar]
- Grubbs, K. M. , Cheney, A. M. , Fortney, J. C. , Edlund, C. , Han, X. , Dubbert, P. , … Sullivan, J. (2015). The role of gender in moderating treatment outcome in collaborative care for anxiety. Psychiatric Services, 66(3), 265–271. https://doi.org/10.1176/appi.ps.201400049*24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gucciardi, E. , Chan, V. W.-S. , Manuel, L. , & Sidani, S. (2013). A systematic literature review of diabetes self‐management education features to improve diabetes education in women of Black African/Caribbean and Hispanic/Latin American ethnicity. Patient Education and Counseling, 92, 235–245. https://doi.org/10.1016/j.pec.2013.03.007 [DOI] [PubMed] [Google Scholar]
- Guidelines International Network (2002. –2017). Template for intervention studies. Retrieved from http://www.g-i-n.net/document-store/working-groups-documents/etwg-documents/template-summarising-intervention-studies.doc/view?searchterm=evidence tables working group
- Hankonen, N. , Sutton, S. , Prevost, A. T. , Simmons, R. K. , Griffin, S. J. , Kinmonth, A. L. , & Hardeman, W. (2014). Which behavior change techniques are associated with changes in physical activity, diet and body mass index in people with recently diagnosed diabetes? Annals of Behavioral Medicine, 49(1), 7–17. https://doi.org/10.1007/s12160-014-9624-9*25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardeman, W. , Michie, S. , Fanshawe, T. , Prevost, A. T. , Mcloughlin, K. , & Kinmonth, A. L. (2008). Fidelity of delivery of a physical activity intervention: Predictors and consequences. Psychology and Health, 23(1), 11–24. https://doi.org/10.1080/08870440701615948*26 [DOI] [PubMed] [Google Scholar]
- Harting, J. , van Assema, P. , van der Molen, H. T. , Ambergen, T. , & de Vries, N. K. (2004). Quality assessment of health counseling: Performance of health advisors in cardiovascular prevention. Patient Education and Counseling, 54(1), 107–118. https://doi.org/10.1016/S0738-3991(03)00194-0*27 [DOI] [PubMed] [Google Scholar]
- Hasson, H. (2010). Systematic evaluation of implementation fidelity of complex interventions in health and social care. Implementation Science, 5(1), 67 https://doi.org/10.1186/1748-5908-5-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermens, R. , Hak, E. , Hulscher, M. , Braspenning, J. , & Grol, R. (2001). Adherence to guidelines on cervical cancer screening in general practice: Programme elements of successful implementation. British Journal of General Practice, 51, 897–903.*28 [PMC free article] [PubMed] [Google Scholar]
- Higgins, J. P. T. , & Deeks, J. J. (2008). Chapter 7: Selecting studies and collecting data In Higgins J. P. T. & Green S. (Eds.), Cochrane handbook for systematic reviews of interventions. Chichester: John Wiley & Sons. [Google Scholar]
- Higgins, J. P. T. , & Green, S. (2011). Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated Mar 2011]. The Cochrane Collaboration; Retrieved from http://handbook.cochrane.org [Google Scholar]
- Holmbeck, G. N. , & Devine, K. A. (2009). Editorial: An author's checklist for measure development and validation manuscripts. Journal of Pediatric Psychology, 34(7), 691–696. https://doi.org/10.1093/jpepsy/jsp046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtrop, J. , Potworowski, G. , Fitzpatrick, L. , Kowalk, A. , & Green, L. (2015). Understanding effective care management implementation in primary care: A macrocognition perspective analysis. Implementation Science, 10(1), 122 https://doi.org/10.1186/s13012-015-0316-z*29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu, C.-C. , & Sandford, B. A. (2007). The Delphi technique: Making sense of consensus. Practical Assessment, Research & Evaluation, 12(10), 1–8. [Google Scholar]
- Hunt, M. K. , Lobb, R. , Delichatsios, H. K. , Stone, C. , Emmons, K. , & Gillman, M. W. (2001). Process evaluation of a clinical preventive nutrition intervention. Preventive Medicine, 33(2), 82–90. https://doi.org/10.1016/S0091-7435(01)80003-7*30 [DOI] [PubMed] [Google Scholar]
- Jansink, R. , Braspenning, J. , Keizer, E. , van der Weijden, T. , Elwyn, G. , & Grol, R. (2013). No identifiable Hb1Ac or lifestyle change after a comprehensive diabetes programme including motivational interviewing: A cluster randomised trial. Scandinavian Journal of Primary Health Care, 31(2), 119–127. https://doi.org/10.3109/02813432.2013.797178*32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keith, R. , Hopp, F. , Subramanian, U. , Wiitala, W. , & Lowery, J. (2010). Fidelity of implementation: Development and testing of a measure. Implementation Science, 5(1), 99 https://doi.org/10.1186/1748-5908-5-99*33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane, C. , Huws-Thomas, M. , Hood, K. , Rollnick, S. , Edwards, K. , & Robling, M. (2005). Measuring adaptations of motivational interviewing: the development and validation of the behavior change counseling index (BECCI). Patient Education and Counseling, 56(2), 166–173. https://doi.org/10.1016/j.pec.2004.01.003 [DOI] [PubMed] [Google Scholar]
- Larsen, K. R. , Michie, S. , Hekler, E. B. , Gibson, B. , Spruijt-Metz, D. , Ahern, D. , … Yi, J. (2016). Behavior change interventions: The potential of ontologies for advancing science and practice. Journal of Behavioral Medicine, 40(1), 6–22. https://doi.org/10.1007/s10865-016-9768-0 [DOI] [PubMed] [Google Scholar]
- Lawrence, W. , Black, C. , Tinati, T. , Cradock, S. , Begum, R. , Jarman, M. , … Barker, M. (2014). ‘Making every contact count’: Evaluation of the impact of an intervention to train health and social care practitioners in skills to support health behaviour change. Journal of Health Psychology, 21(2), 1–14. https://doi.org/10.1177/1359105314523304*34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazovich, D. A. , Curry, S. J. , Beresford, S. A. , Kristal, A. R. , & Wagner, E. H. (2000). Implementing a dietary intervention in primary care practice: A process evaluation. American Journal of Health Promotion, 15(2), 118–125.*35 [DOI] [PubMed] [Google Scholar]
- Lefebvre, C. , Manheimer, E. , & Glanville, J. (2011). Chapter 6: Searching for studies In Higgins J. P. T. & Green S. (Eds.), Cochrane handbook for systematic reviews of interventions, version 5.1.0 (updated March 2011). The Cochrane Collaboration; Retrieved from www.handbook.cochrane.org [Google Scholar]
- Lichstein, K. L. , Riedel, B. W. , & Grieve, R. (1994). Fair tests of clinical trials: A treatment implementation model. Advances in Behaviour Research and Therapy, 16, 1–29. https://doi.org/10.1016/0146-6402(94)90001-9 [Google Scholar]
- Lobb, R. , Gonzalez Suarez, E. , Fay, M. E. , Gutheil, C. M. , Hunt, M. K. , Fletcher, R. H. , & Emmons, K. M. (2004). Implementation of a cancer prevention program for working class, multiethnic populations. Preventive Medicine, 38, 766–776. https://doi.org/10.1016/j.ypmed.2003.12.025*36 [DOI] [PubMed] [Google Scholar]
- Lohr, K. N. (2002). Assessing health status and quality‐of‐life instruments: Attributes and review criteria. Quality of Life Research, 11(3), 193–205. https://doi.org/10.1023/A:1015291021312 [DOI] [PubMed] [Google Scholar]
- Lombard, M. , Snyder-Duch, J. , & Bracken, C. C. (2002). Content analysis in mass communication: Assessment and reporting of intercoder reliability. Human Communication Research, 28(4), 587–604. https://doi.org/10.1111/j.1468-2958.2002.tb00826.x [Google Scholar]
- Lorencatto, F. , West, R. , Bruguera, C. , & Michie, S. (2014). A method for assessing fidelity of delivery of telephone behavioral support for smoking cessation. Journal of Consulting and Clinical Psychology, 82(3), 482–491. https://doi.org/10.1037/a0035149 [DOI] [PubMed] [Google Scholar]
- Lorencatto, F. , West, R. , Seymour, N. , & Michie, S. (2013). Developing a method for specifying the components of behavior change interventions in practice: The example of smoking cessation. Journal of Consulting and Clinical Psychology, 81(3), 528–544. https://doi.org/10.1037/a0032106 [DOI] [PubMed] [Google Scholar]
- Matei, R. , Thuné-Boyle, I. , Hamer, M. , Iliffe, S. , Fox, K. R. , Jefferis, B. J. , & Gardner, B. (2015). Acceptability of a theory‐based sedentary behaviour reduction intervention for older adults (‘On Your Feet to Earn Your Seat’). BMC Public Health, 15(1), 606 https://doi.org/10.1186/s12889-015-1921-0*37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maynard, B. R. , Peters, K. E. , Vaughn, M. G. , & Sarteschi, C. M. (2013). Fidelity in after‐school program intervention research: A systematic review. Research on Social Work Practice, 23(6), 613–623. https://doi.org/10.1177/1049731513491150 [Google Scholar]
- McCarthy, M. M. , Dickson, V. V. , Katz, S. D. , Sciacca, K. , & Chyun, D. A. (2015). Process evaluation of an exercise counseling intervention using motivational interviewing. Applied Nursing Research, 28, 156–162. https://doi.org/10.1016/j.apnr.2014.09.006*38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurry, S. M. , LaFazia, D. M. , Pike, K. C. , Logsdon, R. G. , & Teri, L. (2012). Development and evaluation of a sleep education program for older adults with dementia living in adult family homes. The American Journal of Geriatric Psychiatry, 20(6), 494–504. https://doi.org/10.1097/JGP.0b013e318248ae79*39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGillion, M. H. , Watt-Watson, J. , Stevens, B. , LeFort, S. M. , Coyte, P. , & Graham, A. (2008). Randomized controlled trial of a psychoeducation program for the self‐management of chronic cardiac pain. Journal of Pain and Symptom Management, 36(2), 126–140. https://doi.org/10.1016/j.jpainsymman.2007.09.015*40 [DOI] [PubMed] [Google Scholar]
- McNamara, K. P. , O'Reilly, S. L. , George, J. , Peterson, G. M. , Jackson, S. L. , Duncan, G. , … Dunbar, J. A. (2015). Intervention fidelity for a complex behaviour change intervention in community pharmacy addressing cardiovascular disease risk. Health Education Research, 30(6), 897–909. https://doi.org/10.1093/her/cyv050*41 [DOI] [PubMed] [Google Scholar]
- Metzelthin, S. F. , Daniëls, R. , van Rossum, E. , Cox, K. , Habets, H. , de Witte, L. P. , & Kempen, G. I. J. M. (2013). A nurse‐led interdisciplinary primary care approach to prevent disability among community‐dwelling frail older people: A large‐scale process evaluation. International Journal of Nursing Studies, 50, 1184–1196. https://doi.org/10.1016/j.ijnurstu.2012.12.016*42 [DOI] [PubMed] [Google Scholar]
- Michie, S. , Hardeman, W. , Fanshawe, T. , Prevost, A. T. , Taylor, L. , & Kinmonth, A. L. (2008). Investigating theoretical explanations for behaviour change: The case study of ProActive. Psychology and Health, 23(1), 25–39. https://doi.org/10.1080/08870440701670588 [DOI] [PubMed] [Google Scholar]
- Miller, W. R. , Moyers, T. B. , Ernst, D. , & Amrhein, P. (2003). Manual for the motivational interviewing skill code (MISC). Unpublished manuscript. Albuquerque: Center on Alcoholism, Substance Abuse and Addictions, University of New Mexico. Retrieved from https://casaa.unm.edu/download/misc.pdf
- Miller, W. R. , & Rollnick, S. (2014). The effectiveness and ineffectiveness of complex behavioural interventions: Impact of treatment fidelity. Contemporary Clinical Trials., 37, 234–241. https://doi.org/10.1016/j.cct.2014.01.005 [DOI] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. Annals of Internal Medicine, 151, 264–269. [DOI] [PubMed] [Google Scholar]
- Moncher, F. J. , & Prinz, R. J. (1991). Treatment fidelity in outcome studies. Clinical Psychology Review, 11, 247–266. https://doi.org/10.1016/0272-7358(91)90103-2 [Google Scholar]
- Montgomery, P. , Underhill, K. , Gardner, F. , Operario, D. , & Mayo-Wilson, E. (2013). The Oxford Implementation Index: A new tool for incorporating implementation data into systematic reviews and meta‐analyses. Journal of Clinical Epidemiology, 66, 874–882. https://doi.org/10.1016/j.jclinepi.2013.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oakley, A. , Strange, V. , Bonell, C. , Allen, E. , Stephenson, J. , & Team, R. S. (2006). Health services research: Process evaluation in randomised controlled trials of complex interventions. BMJ. British Medical Journal, 332, 413–416. https://doi.org/10.1136/bmj.332.7538.413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obarzanek, E. , Vollmer, W. M. , Lin, P.-H. , Cooper, L. S. , Young, D. R. , Ard, J. D. , … Appel, L. J. (2007). Effects of individual components of multiple behavior changes: The PREMIER Trial. American Journal of Health Behavior, 31(5), 545–560. https://doi.org/10.5993/ajhb.31.5.10*43 [DOI] [PubMed] [Google Scholar]
- Ockene, I. S. , Tellez, T. L. , Rosal, M. C. , Reed, G. W. , Mordes, J. , Merriam, P. A. , … Ma, Y. (2012). Outcomes of a Latino community‐based intervention for the prevention of diabetes: The Lawrence Latino Diabetes Prevention Project. American Journal of Public Health, 102(2), 336–342. https://doi.org/10.2105/AJPH.2011.300357*44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor, D. , Green, S. , & Higgins, J. P. T. (2011). Chapter 5: Defining the review question and developing criteria for including studies In Higgins J. P. T. & Green S. (Eds.), Cochrane handbook for systematic reviews of interventions. version 5.1.0 (updated March 2011). The Cochrane Collaboration. Retrived from https://www.handbook.cochrane.org. [Google Scholar]
- Olsen, S. , Smith, S. S. , Oei, T. P. , & Douglas, J. (2012). Motivational interviewing (MINT) improves continuous positive airway pressure (CPAP) acceptance and adherence: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 80(1), 151 https://doi.org/10.1037/a0026302*45 [DOI] [PubMed] [Google Scholar]
- Osborn, C. Y. , Amico, K. R. , Cruz, N. , O'Connell, A. A. , Perez-Escamilla, R. , Kalichman, S. C. , … Fisher, J. D. (2010). A brief culturally tailored intervention for Puerto Ricans with type 2 diabetes. Health Education and Behavior, 37(6), 849–862. https://doi.org/10.1177/1090198110366004*46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettman, T. L. , Misan, G. M. , Owen, K. , Warren, K. , Coates, A. M. , Buckley, J. D. , & Howe, P. R. (2008). Self‐management for obesity and cardio‐metabolic fitness: Description and evaluation of the lifestyle modification program of a randomised controlled trial. The International Journal of Behavioral Nutrition and Physical Activity, 5, 53 https://doi.org/10.1186/1479-5868-5-53*47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pill, R. , Stott, N. , Rollnick, S. , & Rees, M. (1998). A randomized controlled trial of an intervention designed to improve the care given in general practice to type II diabetic patients: Patient outcomes and professional ability to change behaviour. Family Practice, 15(3), 229–235. https://doi.org/10.1093/fampra/15.3.229*48 [DOI] [PubMed] [Google Scholar]
- Popay, J. , Roberts, H. , Sowden, A. , Petticrew, M. , Arai, L. , Rodgers, M. , … Duffy, S. (2006). Guidance on the conduct of narrative synthesis in systematic reviews A product from the ESRC methods programme. 1: 92. [Google Scholar]
- Resnick, B. , Inguito, P. , Orwig, D. , Yahiro, J. Y. , Hawkes, W. , Werner, M. , … Magaziner, J. (2005). Treatment fidelity in behavior change research: a case example. Nursing Research, 54(2), 139–143. [DOI] [PubMed] [Google Scholar]
- Reynolds, J. , DiLiberto, D. , Mangham-Jefferies, L. , Ansah, E. , Lal, S. , Mbakilwa, H. , … Chandler, C. (2014). The practice of ‘doing’ evaluation: Lessons learned from nine complex intervention trials in action. Implementation Science, 9(1), 75 https://doi.org/10.1186/1748-5908-9-75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rixon, L. , Baron, J. , McGale, N. , Lorencatto, F. , Francis, J. , & Davies, A. (2016). Methods used to address fidelity of receipt in health intervention research: A citation analysis and systematic review. BMC Health Services Research, 16(1), 663 https://doi.org/10.1186/s12913-016-1904-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts, P. , Priest, H. , & Traynor, M. (2006). Reliability and validity in research. Nursing Standard, 20(44), 41–45. https://doi.org/10.7748/ns2006.07.20.44.41.c6560 [DOI] [PubMed] [Google Scholar]
- Roy-Byrne, P. , Craske, M. G. , Sullivan, G. , Rose, R. D. , Edlund, M. J. , Lang, A. J. , … Stein, M. B. (2010). Delivery of evidence‐based treatment for multiple anxiety disorders in primary care: A randomized controlled trial. JAMA, 303(19), 1921–1928. https://doi.org/10.1001/jama.2010.608*49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders, R. P. , Evans, M. H. , & Joshi, P. (2005). Developing a process‐evaluation plan for assessing health promotion program implementation: A How‐to guide. Health Promotion Practice, 6(2), 134–147. https://doi.org/10.1177/1524839904273387 [DOI] [PubMed] [Google Scholar]
- Saunders, R. P. , Wilcox, S. , Baruth, M. , & Dowda, M. (2014). Process evaluation methods, implementation fidelity results and relationship to physical activity and healthy eating in the Faith, Activity, and Nutrition (FAN) study. Evaluation and Program Planning, 43, 93–102. https://doi.org/10.1016/j.evalprogplan.2013.11.003*50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schinckus, L. , Van den Broucke, S. , Housiaux, M. , & Consortium, D. L. (2014). Assessment of implementation fidelity in diabetes self‐management education programs: A systematic review. Patient Education and Counseling, 96(1), 13–21. https://doi.org/10.1016/j.pec.2014.04.002 [DOI] [PubMed] [Google Scholar]
- Shrive, F. M. , Stuart, H. , Quan, H. , & Ghali, W. A. (2006). Dealing with missing data in a multi‐question depression scale: A comparison of imputation methods. BMC Medical Research Methodology, 6(1), 57 https://doi.org/10.1186/1471-2288-6-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skidmore, E. R. , Dawson, D. R. , Whyte, E. M. , Butters, M. A. , Dew, M. A. , Grattan, E. S. , … Holm, M. B. (2014). Developing complex interventions: Lessons learned from a pilot study examining strategy training in acute stroke rehabilitation. Clinical Rehabilitation, 28(4), 378–387. https://doi.org/10.1177/0269215513502799*51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade, M. , Bird, V. , Clarke, E. , Le Boutillier, C. , McCrone, P. , Macpherson, R. , … Leamy, M. (2015). Supporting recovery in patients with psychosis through care by community‐based adult mental health teams (REFOCUS): A multisite, cluster, randomised, controlled trial. The Lancet Psychiatry, 2, 503–514. https://doi.org/10.1016/S2215-0366(15)00086-3*52 [DOI] [PubMed] [Google Scholar]
- Slaughter, S. E. , Hill, J. N. , & Snelgrove-Clarke, E. (2015). What is the extent and quality of documentation and reporting of fidelity to implementation strategies: A scoping review. Implementation Science, 10(1), 129 https://doi.org/10.1186/s13012-015-0320-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, M. J. , Ackland, L. , O'Loughlin, S. , Young, D. , Pelosi, A. J. , & Morrison, J. (2010). ‘Doing Well’: Description of a complex intervention to improve depression care. Primary Health Care Research and Development, 11, 326–338. https://doi.org/10.1017/S1463423610000228*54 [Google Scholar]
- Smith, D. E. , Heckemeyer, C. M. , Kratt, P. P. , & Mason, D. A. (1997). Motivational interviewing to improve adherence to a behavioral weight‐control program for older obese women with NIDDM – A pilot study. Diabetes Care, 20(1), 52–54. https://doi.org/10.2337/diacare.20.1.52*53 [DOI] [PubMed] [Google Scholar]
- Smith, S. M. , Soubhi, H. , Fortin, M. , Hudon, C. , & O'Dowd, T. (2012). Interventions for improving outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database Systematic Review, 4, Cd006560 https://doi.org/10.1002/14651858.cd006560.pub2 [DOI] [PubMed] [Google Scholar]
- Stanley, M. A. , Calleo, J. , Bush, A. L. , Wilson, N. , Snow, A. L. , Kraus-Schuman, C. , … Kunik, M. E. (2013). The Peaceful Mind program: A pilot test of a cognitive–behavioral therapy–based intervention for anxious patients with Dementia. The American Journal of Geriatric Psychiatry, 21(7), 696–708. https://doi.org/10.1016/j.jagp.2013.01.007*55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stufflebeam, D. L. (2000). Guidelines for developing evaluation checklists: The checklists development checklist (CDC). Kalamazoo, MI: The Evaluation Center. [Google Scholar]
- Suzuki, T. , Shimada, H. , Makizako, H. , Doi, T. , Yoshida, D. , Tsutsumimoto, K. , … Park, H. (2012). Effects of multicomponent exercise on cognitive function in older adults with amnestic mild cognitive impairment: A randomized controlled trial. BMC Neurology, 12(1), 128 https://doi.org/10.1186/1471-2377-12-128*56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thyrian, J. R. , Freyer-Adam, J. , Hannöver, W. , Röske, K. , Mentzel, F. , Kufeld, C. , … Hapke, U. (2007). Adherence to the principles of Motivational Interviewing, clients’ characteristics and behavior outcome in a smoking cessation and relapse prevention trial in women postpartum. Addictive Behaviors, 32, 2297–2303. https://doi.org/10.1016/j.addbeh.2007.01.024*57 [DOI] [PubMed] [Google Scholar]
- Thyrian, J. R. , Freyer-Adam, J. , Hannöver, W. , Röske, K. , Mentzel, F. , Kufeld, C. , … Hapke, U. (2010). Population‐based smoking cessation in women post partum: Adherence to motivational interviewing in relation to client characteristics and behavioural outcomes. Midwifery, 26, 202–210. https://doi.org/10.1016/j.midw.2008.04.004*58 [DOI] [PubMed] [Google Scholar]
- Tomasone, J. , Martin Ginis, K. , Estabrooks, P. , & Domenicucci, L. (2014). ‘Changing Minds’: Determining the effectiveness and key ingredients of an educational intervention to enhance healthcare professionals’ intentions to prescribe physical activity to patients with physical disabilities. Implementation Science, 9(1), 30 https://doi.org/10.1186/1748-5908-9-30*59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toomey, E. , Currie-Murphy, L. , Matthews, J. , & Hurley, D. A. (2015). Implementation fidelity of physiotherapist‐delivered group education and exercise interventions to promote self‐management in people with osteoarthritis and chronic low back pain: A rapid review Part II. Manual Therapy, 20, 2187–2294. https://doi.org/10.1016/j.math.2014.10.012 [DOI] [PubMed] [Google Scholar]
- van de Glind, I. , Heinen, M. , Evers, A. , Wensing, M. , & van Achterberg, T. (2012). Factors influencing the implementation of a lifestyle counseling program in patients with venous leg ulcers: A multiple case study. Implementation Science, 7(1), 104 https://doi.org/10.1186/1748-5908-7-104*60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace, J. I. , Buchner, D. M. , Grothaus, L. , Leveille, S. , Tyll, L. , LaCroix, A. Z. , & Wagner, E. H. (1998). Implementation and effectiveness of a community‐based health promotion program for older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 53A(4), M301–M306. https://doi.org/10.1093/gerona/53A.4.M301*61 [DOI] [PubMed] [Google Scholar]
- Weinberger, M. , Murray, M. D. , Marrero, D. G. , Brewer, N. , Lykens, M. , Harris, L. E. , … Smith, F. (2002). Effectiveness of pharmacist care for patients with reactive airways disease: A randomized controlled trial. JAMA, 288, 1594–1602. https://doi.org/10.1001/jama.288.13.1594*62 [DOI] [PubMed] [Google Scholar]
- Weissman, M. M. , Rounsaville, B. J. , & Chevron, E. (1982). Training psychotherapists to participate in psychotherapy outcome studies. American Journal of Psychiatry, 139, 1442–1446. https://doi.org/10.1176/ajp.139.11.1442 [DOI] [PubMed] [Google Scholar]
- Welch, G. , Zagarins, S. E. , Feinberg, R. G. , & Garb, J. L. (2011). Motivational interviewing delivered by diabetes educators: Does it improve blood glucose control among poorly controlled type 2 diabetes patients? Diabetes Research and Clinical Practice, 91(1), 54–60. https://doi.org/10.1016/j.diabres.2010.09.036*63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- West, D. S. , DiLillo, V. , Bursac, Z. , Gore, S. A. , & Greene, P. G. (2007). Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care, 30, 1081–1087. https://doi.org/10.2337/dc06-1966*64 [DOI] [PubMed] [Google Scholar]
- Wieland, M. L. , Weis, J. A. , Palmer, T. , Goodson, M. , Loth, S. , Omer, F. , … Sia, I. G. (2012). Physical activity and nutrition among immigrant and refugee women: A community‐based participatory research approach. Women's Health Issues, 22, e225–e232. https://doi.org/10.1016/j.whi.2011.10.002*65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windsor, R. , Clark, J. , Cleary, S. , Davis, A. , Thorn, S. , Abroms, L. , & Wedeles, J. (2014). Effectiveness of the Smoking Cessation and Reduction in Pregnancy Treatment (SCRIPT) dissemination project: A science to prenatal care practice partnership. Maternal and Child Health Journal, 18(1), 180–190. https://doi.org/10.1007/s10995-013-1252-7*66 [DOI] [PubMed] [Google Scholar]
- World Health Organisation (2017). Constitution of WHO: principles. Retrieved from http://www.who.int/about/mission/en/
- Yu-Yahiro, J. A. , Resnick, B. , Orwig, D. , Hicks, G. , & Magaziner, J. (2009). Design and implementation of a home‐based exercise program post‐hip fracture: The Baltimore hip studies experience. PM&R, 1, 308–318. https://doi.org/10.1016/j.pmrj.2009.02.008*31 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Search strategy.
Appendix S2. Characteristics of included studies.
Appendix S3. The proportion of studies which measured fidelity of delivery, engagement, or both.
Appendix S4. Details extracted from the papers on fidelity of delivery, and engagement methods and results.


