Abstract
Objectives
HIV pre‐exposure prophylaxis (PrEP) is not approved in Switzerland and therefore must be paid for by the users themselves. We conducted a survey to find out whether men who have sex with men (MSM) in Switzerland are already taking PrEP, or are considering using it, and whether it is being taken under medical supervision or not.
Methods
Grindr® is a geosocial networking app for MSM. Between 5 and 24 January 2017, users of the app who were located in Switzerland by a global positioning system (GPS) were asked to participate in a ten‐question survey on PrEP use.
Results
Of the 2455 people who took part in the survey, 1893 were included in the analysis. Eighty‐two participants (4.3%) reported that they were currently taking PrEP, 64 of whom (78%) said that they were under medical supervision. Seven PrEP users (9%) declared that they had not taken an HIV test within the previous 12 months. Nine hundred and forty‐four (49.9%) were considering taking PrEP in the next 6 months, and 1474 (77.9%) were considering taking it at some point in the future.
Conclusions
In an online survey carried out among sexually active MSM in Switzerland, only a minority of the individuals approached responded that they were currently using PrEP. However, the majority of participants were considering taking PrEP in the future. We identified a substantial proportion of PrEP users taking PrEP outside a medical setting. Hence, a national programme facilitating access to medical care and providing PrEP is urgently needed.
Keywords: men who have sex with men, pre‐exposure prophylaxis, social media, Switzerland
Introduction
HIV pre‐exposure prophylaxis (PrEP) refers to using antiretroviral medication to prevent HIV infection. Large trials have shown high efficacy of continuous 1, 2 or intermittent 3 PrEP use of tenofovir disoproxil fumarate/emtricitabine (TDF/FTC; Truvada®) in high‐risk populations. PrEP was approved by the food and drug administration (FDA) of the USA in 2012. Since then, PrEP has become available under different conditions in many other countries.
In Switzerland, prevention strategies have led to a stabilization of the HIV epidemic in the past decade 4. However, there are still a considerable number of newly detected HIV infections every year. Men who have sex with men (MSM) are the most affected group, contributing almost half of all new HIV diagnoses, indicating that a subgroup of MSM has not been reached by existing prevention strategies. In this context, PrEP may be an effective tool complementing the available HIV prevention strategies. TDF/FTC is not approved for PrEP use in Switzerland. However, the Federal Commission for Sexual Health published recommendations on how to monitor individuals taking PrEP and supports its use for people at high risk for becoming infected with HIV 5.
Yet, it is unclear how many individuals are taking PrEP in Switzerland or are considering it. Data from social media and the European Center for Disease Control (ECDC) European PrEP surveys (www.eatg.org) suggest that there are a considerable number of people in Switzerland already using generic TDF/FTC bought through online pharmacies without any professional medical supervision. These individuals are at risk of developing drug‐related complications such as resistance 6 and side effects. Furthermore, in cases where condoms are not used, contracting other sexually transmitted infections (STIs) is more likely 7.
In order to collect data on the number of individuals already taking PrEP in Switzerland, and to assess the acceptance of PrEP among sexually active MSM in Switzerland, we conducted an online survey on the MSM networking app Grindr® (Grindr LLC, Los Angeles, California, USA). The aim of the survey was to evaluate the need in the MSM community for a national PrEP programme as well as the actual and potential numbers of PrEP users in Switzerland.
Methods
Design
Grindr® is a geosocial networking application for smartphones and tablets, designed to help MSM to meet other men in their area via geolocation. It runs with iOS and Android. With over 6.5 million active users every month, according to statistics provided by the company Grindr LLC, Grindr® is the most popular mobile app for the MSM community in the world. Between 5 and 24 January 2017, users of the Grindr® app who were located in Switzerland by a global positioning system (GPS) were asked to participate in the survey. The question appeared in the three national languages spoken in Switzerland, i.e. German, French and Italian, and additionally in English on alternating days. To ensure anonymity, the survey appeared on an independent website (www.surveymonkey.com). The user could choose between these four languages. Once the participants had completed the survey, a cookie prevented them from participating again from the same electronic device. To achieve a high response rate, we kept the survey as short as possible, with the estimated time needed for a participant to complete the survey being 1 min. For questions 2, 3, 6, 7 and 8, answers from all participants were included irrespective of whether an answer was given or not. Questions 4 and 5 were only taken into account in cases where question 3 was answered positively. We offered access to information about PrEP in all four languages and provided addresses of HIV specialists in Switzerland to the participants. The questionnaire is provided in Figure 1.
Figure 1.
The survey questionnaire. PrEP, pre‐exposure prophylaxis.
Data analysis
Data analysis was performed in r (version 3.3.0 The R Foundation for Statistical Computing, Vieanna, Austria). The impact of age and language on the answers to questions 2−8 of the questionnaire was assessed using logistic regression.
Consent and ethics
The responsible ethics committee approved the survey in a letter dated 28 November 2016. No informed consent or study protocol was required as the data were collected anonymously.
Results
A total of 2455 men took part in the survey, of whom 1911 answered at least one question about PrEP, while the remaining 544 participants stopped immediately after they had chosen a language. Eighteen participants said in a comment that they were already HIV positive and were excluded from the analysis. Support was provided for these people in the survey. Ultimately, 1893 participants were included in the analysis. The median age of the participants was 35.9 years [first quartile (Q1) = 28; third quartile (Q3) = 43]. The youngest participant was 18 years old, and the oldest was 74 years old. Of note, the Grindr® terms of service disallow the use of the app by persons under the age of 18 years. Figure 2 shows the answers given by the participants.
Figure 2.
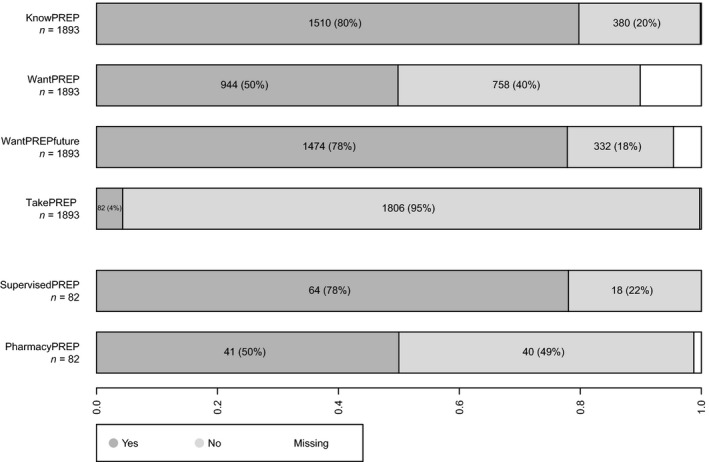
Answers to the survey questions. KnowPrEP, “Have you heard of PrEP before? The daily medication that prevents HIV?”; WantPrEP, “If you are not currently taking PrEP, do you consider to use PrEP in the next 6 months?”; WantPrEPfuture, “If you are not currently taking PrEP, are you interested in taking it or learning more?”; TakePrEP, “Are you taking PrEP now?”; SupervisedPrEP, “If you are taking PrEP now, do you take it under the control of a doctor/medical care provider?”; PharmacyPrEP, “If you are taking PrEP now, where do you buy it?”
Of 1893 participants, 1510 (79.8%) had heard about PrEP before and 82 (4.3%) reported current PrEP use. Italian‐speaking respondents were significantly less likely [odds ratio (OR) 0.21; P < 0.001] and French‐speaking participants slightly less likely (OR: 0.67; P = 0.018) to have heard about PrEP than their German‐speaking counterparts. No significant difference was seen between German‐ and English‐speaking participants regarding this question (OR: 0.84; P = 0.4). Moreover, Italian‐speaking respondents reported taking PrEP significantly less often (OR: 0.29; P = 0.005) compared with the German‐speaking participants, with no significant difference between the other two languages and German (English: OR: 0.99; P = 0.98; French: OR: 1.01; P = 0.96).
Of the 82 PrEP users, 41 (50%) reported buying PrEP in pharmacies, while the other half said that they ordered PrEP on the internet. Only 64 (78%) of the 82 PrEP users were taking PrEP under the supervision of a medical care provider and seven (9%) PrEP users stated that they had not performed an HIV test within the previous 12 months. Of all 1893 participants, 575 (30.4%) answered that their last HIV test was performed more than 12 months ago.
Of all interviewees, 944 (49.9%) were interested in taking PrEP within the next 6 months. Of those, participants in all age groups under 50 years old more often answered this question positively compared with those aged 50 years and older (<20 years: OR: 1.2; P = 0.02; 20–29 years: OR: 1.15; P = 0.001; 30–39 years: OR: 1.16; P < 0.001; 40–49 years: OR: 1.07; P = 0.1). Moreover, 1474 (77.9%) of the participants reported being interested in taking PrEP at some point in the future.
Participants could opt to answer the question “Is there anything else you would like to tell us?” in a comment. Of the 227 comments given by the participants, we observed five main topics: (1) the high cost of PrEP in Switzerland (30 comments); (2) the need for better information about PrEP (30 comments); (3) moral concerns (21 comments); (4) concerns about the potential increase of other STIs in the context of PrEP (21 comments); and (5) concerns about side effects (20 comments).
Discussion
In an online survey among MSM in Switzerland on PrEP use, we found that a high proportion of MSM were considering taking PrEP. We identified a substantial proportion of PrEP users taking PrEP without the recommended medical monitoring 5.
For Switzerland, very few data on current PrEP users exist. The Swiss PrEP Acceptance Study (www.prepstudy.ch), conducted between 1 November 2014 and 29 February 2016, had 556 participants. In this survey, 39% of the participants had considered taking PrEP and 6% had experience with the use of antiretrovirals as PrEP or as postexposure prophylaxis (PEP). Our finding that only a small fraction of the MSM in Switzerland used PrEP correlates with these results; however, twice that number of people were considering beginning to take PrEP in our survey. The ECDC PrEP survey in collaboration with the MSM dating app Hornet (www.eatg.org) was conducted between 23 and 25 April 2016 and had a high response rate (9152) across Europe. However, only 2% of the interviewees came from Switzerland. In the Hornet survey, 10% of the participants were using PrEP and approximately one‐third were considering using it in the next 6 months. However, in this survey many participants came from France and the UK, where PrEP was available in the framework of clinical trials at that time.
By using the dating app Grindr® and by keeping the effort required by participants to a minimum, we obtained more representative data for sexually active MSM in Switzerland than the previous two surveys produced. We found that a larger number of MSM were interested in taking PrEP in the future, and were therefore candidates to participate in any PrEP service programme that may be implemented in Switzerland. Moreover, we identified a substantial number of PrEP users taking PrEP without medical supervision, and thus at risk of developing drug‐related complications. The data obtained in our survey will help to estimate the influence of PrEP on the public health sector, and to develop an infrastructure to ensure access to medical care for people using PrEP.
Our study has some limitations. Firstly, the participants were only users of the Grindr® app. It is therefore unclear if the survey is fully representative of the entire sexually active MSM population in Switzerland. Secondly, the only sociodemographic data we collected were the age and language of the participant, because we wanted to limit the survey to ten questions. Finally, people who were not permanent residents of Switzerland could have participated in the survey and might have influenced the results.
The fact that people use PrEP without medical supervision is of great concern and has manifold implications. There has been an increase in the rate of other STIs such as syphilis, gonorrhoea and chlamydia, especially among MSM, world‐wide (www.bag.admin.ch and www.cdc.gov/std/stats15). PrEP is discussed as one reason for the rising epidemic of these STIs 7, because follow‐up studies from regions where PrEP is available show a decrease of condom use, although PrEP is recommended in combination with condoms 8. Consequently, a national PrEP programme with regular STI testing might also lead to a reduction of these STIs. Particularly alarming is the fact that there are people who use PrEP but do not undergo regular HIV testing. In addition to the problem of contracting HIV as a result of insufficient adherence to the medication 1, 2, 3, there are also a few case reports of break‐through HIV infections in people who had been highly adherent to the daily intake of PrEP 6. HIV‐positive individuals are at high risk of developing drug resistance if they continue taking PrEP.
More frequent HIV testing should be performed among people using PrEP and also among those who do not use PrEP if we really want to achieve the Joint United Nations Programme on HIV/AIDS (UNAIDS) target 90‐90‐90 model by 2020 9. Almost one‐third of the participants in our survey had not take an HIV test in the previous 12 months. This is in line with a recent publication by Kohler and colleagues on the current test‐and‐treat cascade in Switzerland 10. They showed that Switzerland reached the UNAIDS target of treating almost every patient identified with a new HIV infection and achieving an undetectable viral load, but needs to do better in the first 90. The HIV prevention strategy in Switzerland must be reassessed as regards how to reach people at risk of becoming HIV infected and motivate them to take regular HIV tests. In combination with test‐and‐treat and other existing strategies, PrEP can be used as a new tool in the fight against the HIV epidemic. The dramatic decline of new HIV diagnoses in San Francisco 11 and London 12 has been linked to the high rate of PrEP users in these regions. However, causation has not been demonstrated as these findings are influenced by many other factors.
The use of social media was extremely useful to reach the target population in this survey and further collaboration in the prevention strategy should be considered. Our results emphasize the urgent need to build up a comprehensive PrEP service in Switzerland, and to offer targeted prevention measures to MSM. To study the influence of PrEP on the incidence of new HIV diagnoses, the Swiss HIV Cohort Study could serve as a proof‐of‐concept tool to combine prevention strategies such as PrEP and treatment as prevention with existing HIV networks. If all existing resources can be used, an end to the HIV epidemic may be in sight.
Author contributions
BH, JHQ and JF planned the survey and formulated the questions. JQ implemented the questions in surveymonkey and advertised it on Grindr. KK performed the statistical analysis. BH and KK drafted the manuscript. All authors reviewed the manuscript critically and approved the final version before submitting it for publication.
Acknowledgements
We wish to thank all Grindr users who participated in the survey and Grindr LLC who made this survey possible. Many thanks to Charlotte Berlièr, Carsten Depmeier, Simon Froehling and Murray Gaylard for their help and special thanks to Benjamin Christopher Robinson for the inspiration for the study.
References
- 1. McCormack S, Dunn DT, Desai M, et al Pre‐exposure prophylaxis to prevent the acquisition of HIV‐1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open‐label randomised trial. Lancet 2016; 387: 53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grant RM, Lama JR, Anderson PL, et al Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010; 363: 2587–2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Molina JM, Capitant C, Spire B, et al On‐demand preexposure prophylaxis in men at high risk for HIV‐1 infection. N Engl J Med 2015; 373: 2237–2246. [DOI] [PubMed] [Google Scholar]
- 4. Bundesamt für Gesundheilt . HIV, syphilis, gonorrhoe und chlamydose in der Schweiz im jahr 2015: eine epidemiologische übersicht. BAG‐Bulletin 2016; 46: 24. [Google Scholar]
- 5. Bundesamt für Gesundheit . Empfehlung der Eidgenössischen Kommission für sexuelle Gesundheit (EKSG) zur HIV‐Prä‐Expositionsprophylaxe (PrEP) in der Schweiz. BAG‐Bulletin 2016; 4: 3. [Google Scholar]
- 6. Knox DC, Anderson PL, Harrigan PR, Tan DH. Multidrug‐resistant HIV‐1 infection despite preexposure prophylaxis. N Engl J Med 2017; 376: 501–502. [DOI] [PubMed] [Google Scholar]
- 7. Dubourg G, Raoult D. The challenges of preexposure prophylaxis for bacterial sexually transmitted infections. Clin Microbiol Infect 2016; 22: 753–756. [DOI] [PubMed] [Google Scholar]
- 8. Alaei K, Paynter CA, Juan SC, Alaei A. Using PrEP, losing condoms? PrEP promotion may undermine safe sex. AIDS 2016; 3(18): 2753–2756. [DOI] [PubMed] [Google Scholar]
- 9. McMahon JH, Medland N. 90‐90‐90: how do we get there? Lancet HIV 2014; 1: e10–e11. [DOI] [PubMed] [Google Scholar]
- 10. Kohler P, Schmidt AJ, Cavassini M, et al The HIV care cascade in Switzerland: reaching the UNAIDS/WHO targets for patients diagnosed with HIV. AIDS 2015; 29: 2509–2515. [DOI] [PubMed] [Google Scholar]
- 11. Garcia B et al HIV Epidemiology Annual Report 2015, San Francisco. 2016.
- 12. Nwokolo N, Whitlock G, McOwan A. Not just PrEP: other reasons for London's HIV decline. The lancet HIV 2017; 4(4): e153 [DOI] [PubMed] [Google Scholar]


