Dear Editor,
Endotracheal intubation is an airway management procedure commonly performed under general anaesthesia; it may cause some complications (1). Vocal cord paralysis, which is a rare complication with an incidence of less than 0.1%, may lead to aspiration pneumonia and postoperative mortality and morbidity (2). In this case report, the importance of the early diagnosis of vocal cord paralysis and also of performing preoperative and postoperative endoscopic examinations was emphasised.
A 22-year-old (height: 172 cm, weight: 68 kg) male patient planned to undergo middle ear surgery due to the diagnosis of chronic otitis media. Biochemical parameters, airway assessment and endoscopic examination results of the larynx were normal. Written informed consent was obtained from the patient for performing surgery and administering anaesthesia. After performing ECG, non-invasive blood pressure, pulse oximetry and standard anaesthesia monitoring were done; the premedication was provided with 2 mg iv midazolam. For anaesthesia induction, 150 mg propofol and 70 μg remifentanil (in 1-min) boluses were intravenously administered. A neuromuscular blocker was not used for anaesthesia induction in order to perform neuromonitoring of the facial nerve. After 2 min, the patient was intubated on the first attempt without any problem using an 8.0-mm endotracheal tube (ETT) with a C-MAC® D-BLADE™ video laryngoscope (STORZ®). The cuff was inflated with air, and the cuff volume was adjusted using the classical manual palpation method instead of a manometer. For the maintenance of anaesthesia, total intravenous anaesthesia was administered with an infusion of propofol (6 mg kg−1 h−1) and remifentanil (0.025 μg kg−1 min−1). During left canal wall-down mastoidectomy and tympanoplasty, which lasted for 220 min, the patient’s head was rotated to the right side at a 45-degree angle. At the end of surgery, the patient was extubated. No blood stain was observed on the lips and in the mouth during intubation and extubation.
The patient stated that he had a tickling sensation in his throat and hoarseness for 4 h after extubation and he did not define aspiration for solid and liquid foods. In the fibreoptic endoscopic examination of the larynx, the right vocal cord was evaluated as paramedian, even as fixed and paralytic (Figure 1a). Oral prednisolone therapy (1 mg kg−1 day−1) was initiated with doses decreasing every 5 days for 3 weeks. The results of a control endoscopic examination, which was performed on the 30th day after extubation, were found to be normal (Figure 1b), and the patient showed full recovery.
Figure 1.
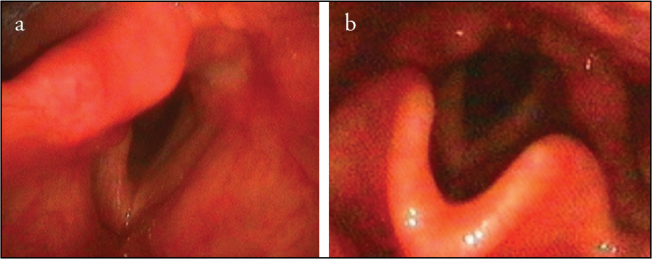
a, b. (a) In the fibreoptic endoscopic examination of the larynx performed at the 4th postoperative hour, the right vocal cord was observed as paramedian, even as fixed; (b) in the control examination performed on the 30th postoperative day, both vocal cords were observed to be moving and symmetrical during phonation.
Some factors can be considered responsible for the pathogenesis of vocal cord paralysis. The vocal cord can be damaged when mechanically compressed by ETTs and laminas of the thyroid cartilage; as a result, vocal cord paralysis can occur. In another mechanism, the cricoid cartilage or vocal cords can be pushed to the oblique position of the neck by the posterior surface of ETT cuffs and neuropraxia can develop due to the compression of the recurrent laryngeal nerve. This condition generally results in temporary nerve paralysis. Moreover, endotracheal intubation with an inappropriate ETT and a high cuff pressure can cause the development of vocal cord paralysis. In cases in which the surgical duration is between 3 h and 6 h, the risk of nerve paralysis increases two-fold (3). In our case, the duration of intubation was more than 3 h and the rotation of the head to the right side can probably explain recurrent nerve paralysis. In addition, we aimed to regress the oedema and inflammation on the recurrent laryngeal nerve by providing oral steroid therapy at decreasing doses.
If hoarseness and serious respiratory distress develop after endotracheal intubation, vocal cord paralysis should be remembered to avoid possible complications.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – H.T., U.K., M.C.G., Ü.A.; Resources – H.T.; Data Collection and/or Processing – M.C.G.; Analysis and/or Interpretation – Ü.A.; Literature Search – U.K.; Writing Manuscript – H.T.; Critical Review – M.C.G.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Fauzdar S, Kraus J, Papageorge M. Vocal cord paralysis following orthognathic surgery intubation. Ann Maxillofac Surg. 2011;1:166–8. doi: 10.4103/2231-0746.92785. https://doi.org/10.4103/2231-0746.92785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shin YH, An DA, Choi WJ, Kim YH. Unilateral vocal cord paralysis following a short period of endotracheal intubation anesthesia. Korean J Anesthesiol. 2013;65:357–8. doi: 10.4097/kjae.2013.65.4.357. https://doi.org/10.4097/kjae.2013.65.4.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benumof JL. Airway Management: Principles and Practice. St Louis: Mosby; 1996. p. 868. [Google Scholar]


