Abstract
Objective
To examine the role of provider communication about psychosocial causes of abdominal pain and recommendations for psychosocial intervention during a gastroenterology clinic visit in predicting families’ causal beliefs and perceptions of treatment acceptability.
Method
Participants were 57 children with a diagnosed or suspected abdominal pain-related functional gastrointestinal disorder (FGID) presenting for an outpatient gastroenterology follow-up visit and their accompanying parent. Children and parents completed questionnaires assessing child anxiety and abdominal pain severity, recall of provider communication about causes of abdominal pain and recommendations for intervention, their own causal beliefs about pain, and perceived acceptability of cognitive behavioral therapy (CBT) and standard medical treatment (SMT) after reading descriptions of each treatment. Providers completed a questionnaire assessing their perceptions and communication about the causes of the child’s abdominal pain and perceived acceptability of CBT.
Results
Provider communication about psychosocial causes and interventions was reported infrequently by parents, children, and providers. Parents rated psychosocial causes for abdominal pain as less likely than physical causes, and children and parents rated CBT as less acceptable than SMT. Parents’ recall of provider communication about psychosocial causes was associated with their own causal beliefs about pain and their perceived acceptability of CBT. Children’s and parents’ recall of provider recommendations for psychosocial intervention was associated with their perceived acceptability of CBT.
Conclusion
Results highlight the importance of provider communication about psychosocial contributors to abdominal pain and psychosocial interventions for children with FGIDs. Medical and mental health providers can partner to deliver care to children with FGIDs using a biopsychosocial approach.
Abdominal pain-related functional gastrointestinal disorders (FGID), which include irritable bowel syndrome, functional dyspepsia, abdominal migraine, and functional abdominal pain syndrome, are characterized by problems in bowel function not explained by identifiable structural or biochemical abnormalities. FGIDs can have a substantial negative impact on quality of life, including school attendance/engagement, peer relationships, and participation in extracurricular activities.1 The cause of FGIDs is likely multifactorial, including physiological and psychosocial factors and their interactions. Children with FGIDs have high rates of psychosocial difficulties, with some studies estimating the rate of anxiety disorders in this patient population to be as high as 65% to 85%2,3 as compared to less than 10% in community samples.4 Conversely, FGID symptoms have been reported in 30% to 70% of children with anxiety disorders3,5 as compared to 6% to 25% of children from the general population.6
Medical providers working with this patient population often provide education about FGIDs and reassurance of their nonserious nature, recommendations for dietary changes, and medications for symptom relief. However, these interventions alone may not be sufficient for effective management of FGIDs.1 Cognitive behavioral therapy (CBT) has received strong empirical support for the treatment of anxiety disorders in children and adolescents.7 Recent studies also provide support for CBT interventions targeting both pain and anxiety for children with comorbid anxiety disorders and functional gastrointestinal symptoms.8,9 Interdisciplinary treatment teams consisting of both medical and mental health providers are becoming increasingly common for the management of FGIDs.10
Parents are gatekeepers of their children’s health care. Parental beliefs about the nature and causes of somatic symptoms and the acceptability of various forms of intervention, including psychosocial interventions such as CBT, are important in determining which treatments a child will receive.11 Child beliefs about the nature of their symptoms and the acceptability of interventions are also important because they may predict whether a child will receive and benefit from treatment.12,13 Claar and Walker examined beliefs about physical and psychosocial causes of, and remedies for, abdominal pain among 153 mothers of children presenting to a pediatric gastroenterology clinic.14 Before the initial medical evaluation, approximately half of the mothers endorsed the child “being nervous, worried, or tense” as a probable cause of abdominal pain and “knowing how to relax and not get worried or tense” as a probable remedy. However, only 18% endorsed “counseling” as a probable remedy before the medical evaluation, and among those whose child’s unexplained abdominal pain had improved 1 year later, only 5% endorsed “counseling” as a remedy that probably contributed to this improvement. Maternal perceptions of CBT or other empirically supported psychological interventions for pain were not specifically assessed. Claar and Scharff examined parents’ and children’s perceptions of pain treatments among 297 families presenting to a multidisciplinary tertiary pain clinic and found that the parents most often endorsed “learning to cope with pain” as the treatment that would be beneficial if children’s pain continued, but only 2% reported having pursued psychotherapy.15 Limited understanding of the ways in which certain forms of psychotherapy can be helpful in promoting coping and anxiety management strategies for children with chronic pain may be contributing to low levels of mental health treatment in addition to other barriers such as perceived stigma or limited access to mental health professionals with training and experience in pediatric chronic pain interventions.
Multiple factors, including symptom severity/duration and past treatment experiences, are associated with parental beliefs about the causes of and treatments for various forms of child symptoms.11,16,17 Crushell et al contacted the parents of children admitted to the hospital for recurrent abdominal pain within the past several years and found that the parents who reported continued abdominal pain were more likely to attribute the pain to physical causes and less likely to perceive a joint pediatric and psychiatric approach to the treatment of their child in the hospital as helpful when compared to the parents of children whose abdominal pain had been resolved.16 The extent to which medical providers discuss the potential role of psychosocial factors in the causes and maintenance of abdominal pain and recommend psychosocial interventions during the clinic visit may additionally influence parent and child beliefs.18,19 Although these family-provider discussions have been emphasized in the literature describing integrated care models in pediatric gastroenterology10,20 and have been examined in relation to maternal distress and satisfaction with the provider,19 empirical investigations of how they may impact parent and child beliefs about the causes and treatments of abdominal pain are lacking. It is also important to differentiate between discussions reported by a provider or observer versus what the family heard and recalled, as research suggests that these are not interchangeable, with the latter being a stronger predictor of outcomes.21
This study aimed to examine the role of provider communication about psychosocial causes of abdominal pain and recommendations for psychosocial intervention during a gastroenterology clinic visit in predicting families’ causal beliefs and perceptions of treatment acceptability. This study addressed the following questions: (1) How often do parents and children recall provider communication about potential psychosocial causes and treatments for abdominal pain during the gastroenterology clinic visit? (2) How do parents rate the likelihood of psychosocial versus physical causes for the child’s abdominal pain? (3) How do parents and children rate the acceptability of CBT versus standard medical treatment (SMT) for the child’s abdominal pain? and (4) Does parent and child recall of provider communication about psychosocial causes and treatments predict their own causal beliefs and perceived acceptability of CBT? Based on previous literature,14,15 we hypothesized that parents would perceive that psychosocial factors are at least as likely as physical factors to cause the child’s abdominal pain but that parents and children would rate CBT to be less acceptable than SMT as an intervention for abdominal pain. We further hypothesized that families who recalled the provider discussing potential psychosocial causes of pain and psychosocial interventions would rate psychosocial causes as more likely and CBT as more acceptable than those families who did not recall these discussions.
METHODS
Participants
Participants were 57 children between the ages of 7 and 17 with a diagnosed or suspected abdominal pain-related functional gastrointestinal disorder (FGID) presenting for follow-up at an outpatient gastroenterology clinic in a pediatric hospital. The parent who accompanied the child to the clinic also participated in the study. All child participants previously completed an initial medical evaluation to inform diagnosis as part of standard care. Children were considered eligible for the study if an abdominal pain-related FGID was previously diagnosed by the gastroenterology provider or if the provider previously documented in the medical record that the abdominal pain was likely functional in nature, followed by test results (e.g., complete blood count, erythrocyte sedimentation rate, C-reactive protein, liver function tests, abdominal x-rays, and upper gastrointestinal series/small bowel follow-through) ruling out anatomic or pathologic causes of pain. Children who had not experienced recent abdominal pain (i.e., less than 1 episode per month for the last 3 months) were excluded. Children and parents who did not speak and read English fluently were also excluded.
Procedures
Eligible families were approached by a research assistant on arrival to the clinic to discuss study participation. Parents and children who provided informed consent/assent were each given a packet of questionnaires to complete before the clinic visit (i.e., demographics, child anxiety, and abdominal pain severity). A second packet of questionnaires was provided to parents and children (aged 12 and older) immediately following the clinic visit, as responses to these questionnaires were directly related or potentially impacted by the content of the clinic visit (i.e., recall of provider communication, perceived causes of abdominal pain, and perceived acceptability of cognitive behavioral therapy [CBT] and standard medical treatment [SMT]). Children under the age of 12 self-reported anxiety and abdominal pain severity, but did not complete the second packet of questionnaires assessing recall of provider communication and perceived treatment acceptability, as the concepts of the causes of pain and treatment acceptability may be difficult to fully grasp before the development of abstract reasoning skills.22 Families were compensated with a $35 gift card to a national retailer on completion of the study. Providers (physicians and advanced practice nurses) were also asked to complete a brief questionnaire regarding the nature of the child’s abdominal pain and communication during the clinic visit within 24 hours. Select clinical characteristics were extracted from the electronic medical record (e.g., number of previous gastroenterology clinic visits, hospitalizations, or emergency department visits because of abdominal pain). This study was reviewed and approved by the Nemours Institutional Review Board. At the time that this study was initiated, psychology services were available through the hospital’s behavioral health division but were not yet integrated into the gastroenterology clinic.
Measures
Background Information
Information about sociodemographic characteristics and treatment history were gathered through a background questionnaire completed by the parent.
Child Anxiety Symptoms
The Spence Children’s Anxiety Scale (SCAS)23,24 measured the frequency of child anxiety symptoms on a 4-point scale ranging from 0 (never) to 3 (always). Both child-and parent-report versions of the SCAS were used for this study. The SCAS has demonstrated convergent and divergent validity, excellent internal consistency (α =.89–.93), and adequate retest reliability (r =.60–.63).23,24
Child Abdominal Pain
The Abdominal Pain Index (API)25 measured the frequency, duration, and intensity of abdominal pain during the previous 2 weeks. Both child-and parent-report versions of the API were used for this study. Scores on each of the 5 items are standardized using Z scores and summed to produce an overall score. The API has good to excellent internal consistency (α =.80–.93) and evidence of concurrent validity.25,26
Recall of Provider Communications
Parents and children (aged 12 and older) responded to 2 open-ended questions assessing recall of provider communications and recommendations: (1) What has your (child’s) gastroenterologist told you about the likely causes of your (child’s) abdominal pain? and (2) What has your (child’s) gastroenterologist recommended as possible treatments or remedies for your (child’s) abdominal pain? A member of the research team (E.S.) classified responses regarding causes of abdominal pain as including or excluding information about FGIDs and psychosocial factors (e.g., stress, anxiety, and nerves) and responses regarding treatments for abdominal pain as including or excluding information about medication, dietary changes, and psychosocial intervention (e.g., counseling, psychology consultation, and stress management).
Perceived Causes of Abdominal Pain
The Inventory of Causes for Abdominal Pain (ICAP)14 assessed parents’ perceptions of likely causes for the child’s abdominal pain. ICAP lists 10 physical (e.g., virus or disease and food allergies) and 10 psychosocial (e.g., stress and using sickness to get out of doing things) potential causes of abdominal pain, generated in consultation with medical and mental health professionals experienced in both functional and organic gastrointestinal disorders.14 Parents indicated whether each potential cause likely contributes to the child’s pain on a 3-point scale ranging from 0 (probably no) to 2 (probably yes). Responses were examined individually by item and were also summed to yield 2 total scores for physical and psychosocial causes. Since there is no corresponding questionnaire for child respondents, ICAP was completed by parents only.
Treatment Acceptability
Parents and children (aged 12 and older) read one-page descriptions of CBT and SMT. Each description first introduced the rationale and goals of the treatment, type of professional providing the treatment, frequency and duration of appointments, and typical costs, followed by 2 paragraphs describing specific treatment components. For example, the CBT description emphasized learning to cope with anxiety and associated gastrointestinal symptoms (stomach pain and diarrhea), gradually facing situations that result in anxiety, and continuing daily activities even when gastrointestinal symptoms are present, and it was developed in consultation with psychologists who specialize in the cognitive behavioral treatment of child anxiety. The SMT description emphasized medication and dietary changes, and it was developed in consultation with gastroenterologists at the pediatric hospital where the study took place.
After reading each treatment description, parents and children rated the acceptability of the treatment (e.g., reasonableness, effectiveness, side effects, time, cost, and willingness) for the child’s abdominal pain using the Treatment Acceptability Rating Form–Revised (TARF-R).27 Seventeen items were rated on a 7-point scale and are summed to yield a total score. The TARF-R had excellent internal consistency (α =.92) and established construct validity.27,28 Minor modifications were made to the wording of several items to increase their applicability to children with abdominal pain and their parents.
Provider Questionnaire
The child’s gastroenterology provider was asked to complete a 3-item questionnaire within 24 hours of the clinic visit. Providers were first asked to indicate the degree to which they thought the cause of the abdominal pain was organic versus psychosocial in nature by placing an X on a line that spans between entirely organic and entirely psychosocial. For scoring, the 3.5-inch line was divided into 7 equally spaced segments and the segment where the X was placed constituted a score between 1 (entirely organic) and 7 (entirely psychosocial). Providers were then asked to indicate what they told the family about the likely cause(s) of the child’s abdominal pain by checking one or more response options spanning both organic and psychosocial causes. Finally, they were asked to read a brief description of CBT (as described above) and to indicate how acceptable/effective they thought CBT would be in treating the child’s presenting problems on a scale from 1 (not at all) to 7 (very).
Statistical Analyses
Descriptive analyses (frequency counts and percentages) were conducted to examine parent and child recall of provider communication about causes of abdominal pain and recommendations for intervention. Parent perceptions regarding psychosocial versus physical causes for the child’s abdominal pain and parent and child perceptions of the acceptability of CBT versus SMT were examined with repeated measures analysis of variance. The relationships of provider communication about psychosocial causes of abdominal pain and recommendations for psychosocial intervention to the family’s causal beliefs and perceptions of treatment acceptability were examined with analysis of covariance, controlling for anxiety severity and a history of mental health treatment.
RESULTS
Sample Characteristics
Eighty-four families were approached regarding participation in the study. Seventeen were deemed to be ineligible (11 had not experienced recent abdominal pain, 3 were non–English speaking, and 3 were not accompanied by a parent/legal guardian) and 10 declined participation, resulting in a sample of 57 families. Irritable bowel syndrome was diagnosed or suspected for 28 participants, functional abdominal pain syndrome for 15 participants, functional dyspepsia for 2 participants, and unspecified functional gastrointestinal disorder (FGID) (gastrointestinal symptoms suspected to be functional in nature without documentation of a specific FGID diagnosis) for the remaining 12 participants. Two-thirds (N =38) of child participants were aged 12 or older (mean age: 13.9 ± 3.1), 63% (N =36) were female, 86% (N =49) were non-Hispanic white, and 77% (N =44) lived with both parents. Eighty-two percent (N =47) of parent participants were biological or adoptive mothers, 53% (N =30) had at least a college degree, and 70% (N =40; 5% missing data) reported an annual household income of $80,000 or greater. See Table 1 for anxiety and abdominal pain severity and treatment history. Participants did not differ from those who were approached and eligible but declined participation with regard to child gender, race, or number of previous gastroenterology clinic visits. However, participants were older than nonparticipants (participant age: 13.9 ± 3.1; nonparticipant age: 11.9 ± 2.2; p =.03). Since only children aged 12 and older completed the second packet of questionnaires, full child-report data were available for 38 families. Forty-five of the 57 provider questionnaires were completed and returned (79%).
Table 1.
Clinical Characteristics (N =57)
| Clinical Symptoms | Child Report
|
Parent Report
|
||
|---|---|---|---|---|
| Frequency (%) | Mean ± SD | Frequency (%) | Mean ± SD | |
| Abdominal Pain Indexa | ||||
| Frequency ≥ 3 d/wk | 40 (70.2) | 37 (64.9) | ||
| Duration ≥ 1 hr | 27 (47.4) | 38 (66.7) | ||
| Typical Intensity ≥5b | 41 (71.9) | 42 (73.7) | ||
| SCAS Total Scorec | ||||
| Boys aged 7–11 | 23.3 ± 14.8 | 13.3 ± 7.8 | ||
| Boys aged 12–17 | 23.0 ± 14.1 | 13.8 ± 11.5 | ||
| Girls aged 7–11 | 31.1 ± 17.2 | 21.5 ± 10.0 | ||
| Girls aged 12–17 | 29.6 ± 13.9 | 15.9 ± 10.1 | ||
|
| ||||
| Treatment History | Frequency (%) | |||
|
| ||||
| Previous GI clinic visits | ||||
| 1 | 30 (52.6) | |||
| 2–4 | 17 (29.8) | |||
| ≥5 | 10 (17.6) | |||
| Previous ED visit for AP | 15 (26.3) | |||
| Previous hospitalization for AP | 5 (8.8) | |||
| Previous visit with MHP for AP | 14 (24.6) | |||
| Previous visit with MHP for any reason | 19 (33.3) | |||
SCAS, Spence Children’s Anxiety Scale; GI, gastroenterology; ED, emergency department; AP, abdominal pain; MHP, mental health professional.
Responses to items 1, 3, and 4 on the Abdominal Pain Index.
Scale ranged from 1 to 10.
Possible range of SCAS total score is 0 to 114.
Provider Communication During Clinic Visit
Communication About Causes of Pain
Approximately half of parents and children recalled the provider communicating that an FGID may be a cause of abdominal pain (parents: 49.1%; N =28; children: 50%, N =19) (Fig. 1). However, only 19.3% (N =11) of parents and 21.1% (N =8) of children recalled the provider communicating that any specific psychosocial factors may be a cause of pain. Providers reported that they communicated that an FGID may be a cause of abdominal pain in 77.3% (N =34) of cases and that specific psychosocial factors may be a cause of pain in 36.4% (N =16) of cases. With regard to communication about psychosocial factors that may be a cause of pain, the provider-report was significantly correlated with parent recall (r =.45, p =.002), but parent and child recall were not significantly correlated with one another (r =.25, p =.12).
Figure 1.
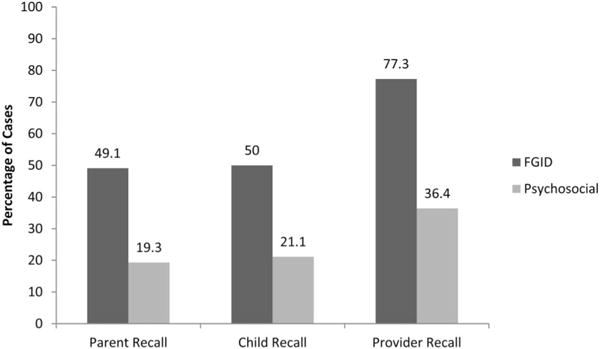
Recall of provider communication about causes of pain. FGID, abdominal pain-related functional gastrointestinal disorder.
When asked the degree to which they thought that the cause of the child’s abdominal pain was organic versus psychosocial in nature, providers reported that the pain was entirely or almost entirely psychosocial (i.e., a score of 6 or greater on a 7-point scale) in 30.2% (N =13) of cases (Fig. 2). However, psychosocial factors were perceived by providers to contribute to the child’s pain at a level similar to organic factors (i.e., a score between 3 and 5) in an additional 53.5% (N =23) of cases.
Figure 2.
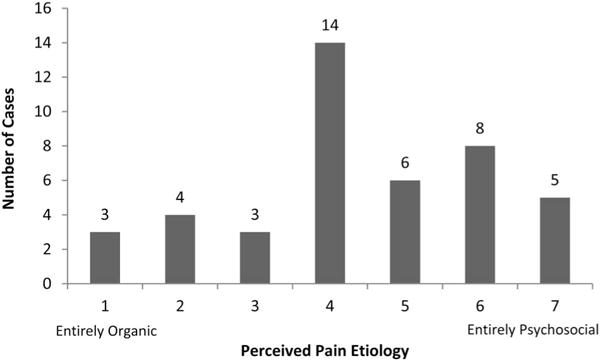
Providers’ perceptions regarding cause of pain. Providers placed an X on a 3.5-inch line that spanned between entirely organic and entirely psychosocial. Responses were scored by dividing the line into 7 equally spaced segments ranging from 1 (entirely organic) to 7 (entirely psychosocial).
Recommendations for Intervention
Less than 20% of parents and children recalled the provider recommending psychosocial intervention (parents: 19.3%, N =11; children: 15.8%, N =6). In contrast, more than three-quarters of parents and children recalled the provider recommending medication (parents: 78.9%, N =45; children: 78.9%, N =30) and one-third recalled the provider recommending dietary changes (parents: 33.3%, N =19; children: 34.2%, N =13). Parent and child recall of recommendations for psychosocial intervention (r =.35, p =.03) and medication (r =.71, p <.001) were significantly correlated, whereas the correlation between parent and child recall of recommendations for dietary changes (r =.30, p =.07) approached significance. Providers reported that they thought cognitive behavioral therapy (CBT) was likely to be acceptable/effective in treating the child’s presenting problems (i.e., a score of 6 or above on a 7-point scale) in 53.3% (N =24) of cases (Fig. 3).
Figure 3.
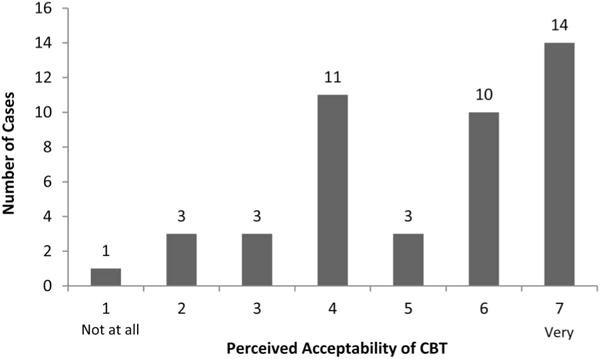
Providers’ perceptions regarding acceptability of cognitive behavioral therapy (CBT). Providers reported their perceived acceptability of CBT on a 7-point Likert scale ranging from 1 (Not at all acceptable/effective) to 7 (Very acceptable/effective).
Parents’ Causal Beliefs About Abdominal Pain
The 3 most frequently endorsed causes of abdominal pain (rated by parents as “probably yes”) were physical in nature: “stomach producing too much acid or gas” (28.1%), “constipation” (24.6%), and “sensitive or nervous stomach” (22.8%). The most frequently endorsed psychosocial causes were: “nervous, worried, and tense” (21.1%), “stress” (17.5%) and “putting too much pressure on himself/herself” (14.0%). In general, parents rated psychosocial causes for the child’s abdominal pain as less likely than physical causes (Inventory of Causes for Abdominal Pain [ICAP] Psychosocial Total: 4.0 ± 3.9; ICAP Physical Total: 6.0 ± 2.9; p <.001). Perceived probability of psychosocial causes was positively associated with non-Hispanic white race (t[55] =2.22, p =.03), parent-reported child anxiety severity (r =.52, p <.001), and history of at least 1 mental health visit because of abdominal pain (t[16] =2.25, p =.04) or for any reason (t[55] =3.68, p =.001) and was negatively associated with history of hospitalization for abdominal pain (t[55] =2.09, p =.04). Parents’ recall of provider communication about psychosocial causes predicted their perceptions about the probability of psychosocial causes for pain (t[11] =2.96, p =.01), which remained significant after controlling for parent-reported anxiety severity and history of previous mental health visit (F[1,53] =7.63, p =.01).
Parents’ and Children’s Perceived Acceptability of Cognitive Behavioral Therapy
Parents and children rated CBT (parents: 76.1 ± 20.9; children: 71.6 ± 16.5) as less acceptable than standard medical treatment (SMT) (parents: 92.8 ± 13.7; children: 87.7 ± 12.9) (ps <.001). Only 17.9% of parents (N =10) and 17.1% of children (N =6) rated CBT as more acceptable than SMT, whereas 78.6% of parents (N =44) and 77.1% of children (N =27) rated SMT as more acceptable.
Parents’ perceived acceptability of CBT was positively associated with a history of at least 1 previous mental health visit because of abdominal pain (t[47] =4.04, p <.001) or for any reason (t[54] =4.26, p <.001), and living in a 2-parent household (t[54] =2.41, p =.02). Parents’ recall of provider communication about psychosocial causes (t[28] =2.19, p =.04) and parents’ recall of provider recommendations regarding psychosocial intervention (t[46] =3.69, p =.001) predicted their perceived acceptability of CBT. However, these relationships were no longer significant after controlling for parent-reported anxiety severity and history of previous mental health visit.
Children’s perceived acceptability of CBT was not associated with sociodemographic variables, anxiety severity, previous treatment history, or recall of provider communication about psychosocial causes. However, children’s recall of provider recommendations regarding psychosocial intervention predicted their perceived acceptability of CBT (t[8] =2.89, p =.02).
DISCUSSION
In a sample of children with a diagnosed or suspected abdominal pain-related functional gastrointestinal disorder (FGID) and their parents, recall of provider communication about psychosocial causes of abdominal pain and recommendations for psychosocial intervention predicted causal beliefs and perceived acceptability of cognitive behavioral therapy (CBT). Although the importance of provider communication about psychosocial factors relating to abdominal pain has been previously emphasized,10,19,20 this is, to our knowledge, the first study evaluating the potential impact of such communication on families’ causal beliefs and perceptions of treatment acceptability. The results of this study have implications for clinical practice and medical training focused on communicating with families about psychosocial issues, an area of need recognized by the American Academy of Pediatrics.18
Despite its demonstrated importance, provider communication about psychosocial causes and interventions was reported infrequently by parents, children, and providers. This is surprising in light of providers’ perceptions that psychosocial factors frequently contributed to the child’s pain at a similar or greater level than organic factors and that CBT was likely to be very acceptable and effective in treating the child’s presenting problems in approximately half of cases. Lack of comfort or confidence in discussing potential psychosocial causes of somatic symptoms may prevent medical providers from initiating such discussions.18,20 In addition, medical providers may not be familiar with mental health professionals who specialize in the treatment of children with comorbid emotional and health concerns to whom they could refer, further preventing communication about psychosocial intervention. Providers may be more likely to discuss psychosocial factors and make referrals to mental health professionals in the context of integrated medical-psychological care and when they have direct, frequent contact with one or more mental health providers.10,20 Even when it is not feasible for a mental health provider to be integrated in a clinic, collaboration between medical and mental health providers can be encouraged through joint participation in rounds and educational programming.
The association between provider communication and parents’ perceived acceptability of CBT diminished after accounting for parent-reported child anxiety severity and history of at least 1 previous mental health visit. It may be that parents who had concerns about the child’s anxiety and previously pursued mental health services were more likely to initiate discussion regarding psychosocial factors with the provider or to recall these discussions after the clinic visit. Although some parents may initiate discussion about psychosocial concerns with the child’s medical provider, research suggests that many refrain from bringing up such concerns because of the belief that medical providers are focused only on the physical aspects of the child’s abdominal pain,17 highlighting the importance of providers initiating these discussions when appropriate. Interestingly, the only variable associated with children’s perceived acceptability of CBT was whether the child recalled that the provider recommended psychosocial intervention. This finding underscores the importance of providers communicating directly with children about causes and interventions rather than focusing solely on parents18 because children’s perceptions are likely impacted by these communications and have been found to predict whether a child will receive and benefit from treatment.12,13
Parents in the present study endorsed symptoms of child anxiety and psychosocial causes of abdominal pain less frequently than previously reported.2,14 Unlike the Claar and Walker study in which families were enrolled before the initial medical evaluation and additional follow-up with gastroenterology was not a requirement for study participation, families in the present study were enrolled during a follow-up visit to gastroenterology and almost half had attended 2 or more previous visits. Parents who bring their child for follow-up at a gastroenterology clinic even after test results rule out anatomic and pathologic abnormalities may have more fears about the child’s abdominal pain and may continue to look for an organic cause as compared with those families who do not pursue follow-up.16,29 Two-thirds of parents in the present study reported that the child continued to experience abdominal pain 3 or more days per week and three-quarters reported a moderate to severe level of pain intensity, as compared to 89% of parents in the Claar and Walker study who reported that the child’s abdominal pain had improved within the year after study entry. Crushell et al evaluated the beliefs of parents whose children were admitted to the hospital for recurrent abdominal pain within the past several years and, consistent with the present study, found that parents who reported continued abdominal pain tended to attribute the pain to physical causes and generally did not perceive a joint pediatric and psychiatric approach to the treatment of their child in the hospital to be helpful.16 In the case of persistent abdominal pain, the extent to which psychosocial causes and interventions are discussed during the gastroenterology clinic visit may be of utmost importance.
This study has several limitations, including its small sample size. Since FGID symptoms tend to wax and wane, appointment cancellations and no-shows were quite common and negatively impacted recruitment. It is possible that additional associations were not detected because of type II error. Children with a suspected but not yet diagnosed FGID were included in this study and some may have gone on to receive a different diagnosis based on future test results. However, restricting inclusion to only those with a diagnosed FGID would have limited generalizability for most children presenting to gastroenterology with recurrent abdominal pain. The study sample was predominantly non-Hispanic white and middle class, consistent with the demographics of patients presenting with FGIDs to this gastroenterology clinic and with previous research suggesting that non-Hispanic white individuals may have higher rates of diagnosed FGIDs as compared to ethnic minorities.30 In addition, the treatment descriptions were estimated at an 11th-grade reading level. Future studies are needed to examine these constructs among families from diverse backgrounds using tools appropriate for a wide range of education levels. The cross-sectional design precludes conclusions regarding causality. Families who perceive a higher likelihood of psychosocial causes and acceptability of CBT may be more likely to recall provider communications consistent with their beliefs. Finally, psychology was in the process of being integrated into the gastroenterology service as the last several participants completed the study. Although no differences were detected between these and previous participants with regard to perceived likelihood of psychosocial causes and perceived acceptability of CBT, small sample sizes preclude more sophisticated time-based analyses. Some study results may not generalize to gastroenterology clinics in which the integration between medical and mental health providers has been long established because the availability and accessibility of mental health professionals trained in empirically supported interventions for children with abdominal pain likely impacts both provider and family perceptions of treatment acceptability.
This study provides evidence for the importance of family-provider discussions about potential psychosocial causes of abdominal pain and psychosocial interventions, and it complements recent articles on integrated care models in pediatric gastroenterology.10,20 Future research involving ethnically and culturally diverse families is needed, given the impact of ethnicity and culture on family-provider communication.18 Future studies should also examine family-provider communication about abdominal pain through direct observation and coding of clinic visit interactions. This methodology could be used to examine how and by whom the discussion was initiated, ways in which recommendations were delivered, nonverbal communication, and factors contributing to inconsistencies in what the provider reported having communicated and what children and parents recall. Although providers may believe that they are sharing information about the role of psychosocial factors for pain, the intended message may not be clear to all family members, as demonstrated in the present study by the relatively weak association between what parents and children recalled from the same clinic visit discussion. This information could have important clinical implications for how to communicate effectively with families about psychosocial aspects of pain, with the ultimate goal of incorporating such discussions into the routine care of children with FGIDs.
Acknowledgments
This study was funded by a Nemours Biomedical Research Grant (16-02966-002). E. Sood’s work on this project was also supported by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health under grant number U54-GM104941 (PI: Binder-Macleod).
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Banez GA, Cunningham CL. Abdominal pain-related gastrointestinal disorders: irritable bowel syndrome and Inflammatory bowel disease. In: Roberts MC, Steele RG, editors. Handbook of Pediatric Psychology. 4th. New York, NY: Guilford; 2009. pp. 403–419. [Google Scholar]
- 2.Campo JV, Bridge J, Ehmann M, et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics. 2004;113:817–824. doi: 10.1542/peds.113.4.817. [DOI] [PubMed] [Google Scholar]
- 3.Dufton LM, Dunn MJ, Compas BE. Anxiety and somatic complaints in children with recurrent abdominal pain and anxiety disorders. J Pediatr Psychol. 2009;34:176–186. doi: 10.1093/jpepsy/jsn064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Costello EJ, Mustillo S, Erkanli A, et al. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 5.Waters AM, Schilpzand E, Bell C, et al. Functional gastrointestinal symptoms in children with anxiety disorders. J Abnorm Child Psychol. 2013;41:151–163. doi: 10.1007/s10802-012-9657-0. [DOI] [PubMed] [Google Scholar]
- 6.Hyams JS, Burke G, Davis PM, et al. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J Pediatr. 1996;129:220–226. doi: 10.1016/s0022-3476(96)70246-9. [DOI] [PubMed] [Google Scholar]
- 7.Walkup JT, Albano AM, Piacentini J, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008;359:2753–2766. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sieberg CB, Flannery-Schroeder E, Plante W. Children with co-morbid recurrent abdominal pain and anxiety disorders: results from a multiple-baseline intervention study. J Child Health Care. 2011;15:126–139. doi: 10.1177/1367493511401640. [DOI] [PubMed] [Google Scholar]
- 9.Warner CM, Colognori D, Kim RE, et al. Cognitive-behavioral treatment of persistent functional somatic complaints and pediatric anxiety: an initial controlled trial. Depress Anxiety. 2011;28:551–559. doi: 10.1002/da.20821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moser NL, Plante WA, LeLeiko NS, et al. Integrating behavioral health services into pediatric gastroenterology: a model of an integrated health care program. Clin Pract Pediatr Psychol. 2014;2:1–12. [Google Scholar]
- 11.Simons LE, Logan DE, Chastain L, et al. Engagement in multidisciplinary interventions for pediatric chronic pain: parental expectations, barriers, and child outcomes. Clin J Pain. 2010;26:291–299. doi: 10.1097/AJP.0b013e3181cf59fb. [DOI] [PubMed] [Google Scholar]
- 12.Bussing R, Zima BT, Mason DM, et al. Receiving treatment for attention deficit/hyperactivity disorder: do adolescents’ perspectives matter? J Adolesc Health. 2011;49:7–14. doi: 10.1016/j.jadohealth.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guite JW, Kim S, Chen CP, et al. Pain beliefs and readiness to change among adolescents with chronic musculoskeletal pain and their parents before an initial pain clinic evaluation. Clin J Pain. 2014;30:27–35. doi: 10.1097/AJP.0b013e31828518e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Claar RL, Walker LS. Maternal attributions for the causes and remedies of their children’s abdominal pain. J Pediatr Psychol. 1999;24:345–354. doi: 10.1093/jpepsy/24.4.345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Claar RL, Scharff L. Parent and child perceptions of chronic pain treatments. Child Health Care. 2007;36:285–301. [Google Scholar]
- 16.Crushell E, Rowland M, Doherty M, et al. Importance of parental conceptual model of illness in severe recurrent abdominal pain. Pediatrics. 2003;112:1368–1372. doi: 10.1542/peds.112.6.1368. [DOI] [PubMed] [Google Scholar]
- 17.Smart S, Cottrell D. Going to the doctors: the views of mothers of children with recurrent abdominal pain. Child Care Health Dev. 2005;31:265–273. doi: 10.1111/j.1365-2214.2005.00506.x. [DOI] [PubMed] [Google Scholar]
- 18.Levetown M. Communicating with children and families: from everyday interactions to skill in conveying distressing information. Pediatrics. 2008;121:e1441–e1460. doi: 10.1542/peds.2008-0565. [DOI] [PubMed] [Google Scholar]
- 19.Williams SE, Smith CA, Bruehl SP, et al. Medical evaluation of children with chronic abdominal pain: impact of diagnosis, physician practice orientation, and maternal trait anxiety on mothers’ responses to the evaluation. Pain. 2009;146:283–292. doi: 10.1016/j.pain.2009.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hommel KA. Psychosocial and behavioral issues in children and adolescents with IBD: clinical implications. Gastroenterol Hepatol. 2013;9:189–191. [PMC free article] [PubMed] [Google Scholar]
- 21.Beckett MK, Elliott MN, Richardson A, et al. Outpatient satisfaction: the role of nominal versus perceived communication. Health Serv Res. 2009;44:1735–1749. doi: 10.1111/j.1475-6773.2009.01001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marini Z, Case R. The development of abstract reasoning about the physical and social world. Child Dev. 2008;65:147–159. [Google Scholar]
- 23.Spence SH, Barrett PM, Turner CM. Psychometric properties of the Spence Children’s Anxiety Scale with young adolescents. J Anxiety Disord. 2003;17:605–625. doi: 10.1016/s0887-6185(02)00236-0. [DOI] [PubMed] [Google Scholar]
- 24.Nauta MH, Scholing A, Rapee RM, et al. A parent-report measure of children’s anxiety: psychometric properties and comparison with child-report in a clinic and normal sample. Behav Res Ther. 2004;42:813–839. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- 25.Walker LS, Smith CA, Garber J, et al. Development and validation of the pain response inventory for children. Psychol Assess. 1997;9:392–405. [Google Scholar]
- 26.Kaminsky L, Robertson M, Dewey D. Psychological correlates of depression in children with recurrent abdominal pain. J Pediatr Psychol. 2006;31:956–966. doi: 10.1093/jpepsy/jsj103. [DOI] [PubMed] [Google Scholar]
- 27.Reimers TM, Wacker DP, Cooper LJ, et al. Acceptability of behavioral treatments for children: analog and naturalistic evaluations by parents. Sch Psychol Rev. 1992;21:628–643. [Google Scholar]
- 28.Reimers TM, Wacker DP, Cooper LJ. Evaluation of the acceptability of treatments for their children’s behavioral difficulties: ratings by parents receiving services in an outpatient clinic. Child Fam Behav Ther. 1991;13:53–71. [Google Scholar]
- 29.Venepalli NK, Van Tilburg MA, Whitehead WE. Recurrent abdominal pain: what determines medical consulting behavior? Dig Dis Sci. 2006;51:192–201. doi: 10.1007/s10620-006-3107-1. [DOI] [PubMed] [Google Scholar]
- 30.Sandler RS. Epidemiology of irritable bowel syndrome in the United States. Gastroenterology. 1990;99:409–415. doi: 10.1016/0016-5085(90)91023-y. [DOI] [PubMed] [Google Scholar]


