Abstract
Objectives
Loneliness is a biopsychosocial determinant of health and contributes to physical and psychological chronic illnesses, functional decline, and mortality in older adults. This paper presents the results of the first randomized trial of LISTEN, which is a new cognitive behavioral intervention for loneliness, on loneliness, neuroimmunological stress response, psychosocial functioning, quality of life, and measures of physical health.
Methods
The effectiveness of LISTEN was evaluated in a sample population comprising 27 lonely, chronically ill, older adults living in Appalachia. Participants were randomized into LISTEN or educational attention control groups. Outcome measures included salivary cortisol and DHEA, interleukin-6, interleukin-2, depressive symptoms, loneliness, perceived social support, functional ability, quality of life, fasting glucose, blood pressure, and body mass index.
Results
At 12 weeks after the last intervention session, participants of the LISTEN group reported reduced loneliness (p = 0.03), enhanced overall social support (p = 0.05), and decreased systolic blood pressure (p = 0.02). The attention control group reported decreased functional ability (p = 0.10) and reduced quality of life (p = 0.13).
Conclusions
LISTEN can effectively diminish loneliness and decrease the systolic blood pressure in community-dwelling, chronically ill, older adults. Results indicate that this population, if left with untreated loneliness, may experience functional impairment over a period as short as 4 months. Further studies on LISTEN are needed with larger samples, in varied populations, and over longer periods of time to assess the long-term effects of diminishing loneliness in multiple chronic conditions.
Keywords: Loneliness, LISTEN, Older adults
1. Introduction
The prevalence rates of loneliness have been reported to be 35% in U.S. adults aged 45 years and above [1], 27.9% in older adults in Jerusalem [2], 31.5% in Australian older adults, and up to 78% in Chinese older adults [3,4]. Researchers have consistently suggested that diminishing loneliness can improve overall health [5]. Loneliness is recognized as a bio-psychosocial determinant of health [6] in older adult populations worldwide. Loneliness is associated with the activation of the hypothalamic-pituitary-adrenocortical (HPA) axis [7], which elicits a physiological response [8] that contributes to the dysregulation of inflammatory [9], neuroendocrine [10], and immune systems [11]. Through this mechanism, loneliness may contribute to poor control of chronic conditions, including hypertension [12,13] and metabolic problems, such as obesity [14]. In addition, loneliness is linked to multiple behavioral health problems, including anxiety [15], depression [16], substance abuse [1], and suicidal tendency [17]. Over half (56%) of adults in the USA with anxiety have reported loneliness [1]. Loneliness contributes to depression [11,18]; hence, diminishing loneliness can help prevent depression [16], thereby decreasing expenses in healthcare systems [19].
At present, healthcare providers do not have access to a recommended clinically effective treatment for loneliness. Interventions for loneliness have ranged from overemphasis on social reintegration [20–24] to individual cognitive therapies, such as mindfulness [25]. No single intervention has been determined as effective for diminishing loneliness and its negative health outcomes across age groups or populations. One recent meta-analysis of interventions suggested that effectiveness may be enhanced if interventions targeted common thought process errors that occur with loneliness [26], such as automatic thinking [27] or fears and phobias [28]. In response to this body of knowledge, we developed LISTEN, a novel intervention for loneliness. The initial development, feasibility, and acceptability of LISTEN have been published [29,30].
This initial study on LISTEN was conducted in West Virginia, a state located entirely in Appalachia. The Appalachian region is a known area of health disparity [31]. A disproportionate segment of the region’s population is rural [32], impoverished, lowly educated, and physically ill, all of which are linked to poor mental health outcomes [33]. Therefore, more adults in Appalachia may be suffering from loneliness [15] or untreated depression [34]. The rural nature of Appalachia coupled with the lack of public transportation may limit social contacts. In spite of the stereotypical view of Appalachians living rurally with close extended family, other forms of social support may be more important than family proximity in predicting mental health outcomes [35]. Particularly for women, emotional support from friends has been reported to enhance affect [36]. Knowing that adults living rurally may experience a chronic condition with a sense of quiet pride [37] makes it even more important that healthcare providers proactively assess and address problems such as loneliness and depression.
Findings from preliminary qualitative studies on lonely older women living in Appalachia encouraged the development of LISTEN [29]. Lonely older women suffering from chronic illness and living in Appalachia reported that their experience of loneliness is related to negative emotions including fear, anger, and worry. They reported that loneliness can lead to loss of function or independence [38]. Conversely, these women reported positive emotions such as joy when the feeling of loneliness is absent. Participants of the qualitative studies on loneliness in Appalachia reported that staying busy and going out were important to the management of loneliness [38]. This paper presents the effectiveness of LISTEN, an intervention designed to target impaired cognitive processes associated with loneliness, on the psychosocial and physiological measures in a sample of lonely, chronically ill adults living in the communities of Appalachia.
1.1. Theoretical framework for study
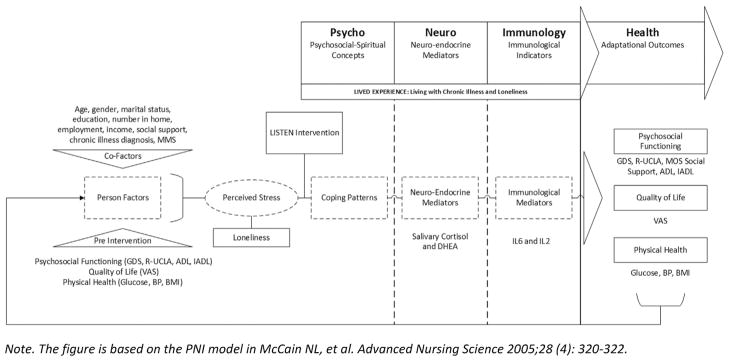
A psychoneuroimmunology (PNI) paradigm serves as a theoretical framework for the study design [39]. This paradigm enhances understanding about how the experience of a psychosocial stressor may lead to other physical or behavioral health problems through the physiological response to the stressor. The framework specifically considers how the perception of stress in the presence of existing coping can lead to neuroimmunological responses that affect functional ability, quality of life, and illness progression over time. Fig. 1 illustrates the study variables in the model of the PNI paradigm. For the purposes of this study, the research team posited that by diminishing loneliness, participants would experience a diminished physiological response to the stressor of loneliness and then achieve improved health.
Fig. 1.
Study variables illustrated in the psychoneuroimmunology paradigm.
2. Study design, setting, subjects, and methods
2.1. Design, aims, and ethical considerations
The study design was a prospective, longitudinal, randomized controlled trial with two groups: LISTEN intervention group and attention control group. The two following aims were accomplished by studying a sample of lonely, rural, and chronically ill adults: (1) to evaluate the relative effectiveness of LISTEN for decreasing loneliness and neuroimmunological stress response; and (2) to evaluate the relative effectiveness of LISTEN in improving psychosocial functioning, quality of life, and physical health. The two aims presented two corresponding research questions, as follows. 1) What are the differences between the LISTEN group and the attention control group in morning rise in salivary cortisol, DHEA levels, interleukin (IL)-6, and IL-2? 2) What are the differences between the LISTEN group and the attention control group in terms of depression, loneliness, social support, functional ability, quality of life, glucose, blood pressure, and body mass index (BMI)? Before the study commenced, a letter of approval was obtained from the West Virginia University Institutional Review Board.
2.2. Setting
The setting for enrollment in the study was the Clark Sleeth Family Medicine Center, which is a primary care center located in the Health Sciences Center of West Virginia University in North Central West Virginia. Approximately 5600 geriatric outpatients are in this clinic annually. The setting for the delivery of the LISTEN and attention control group sessions was a private room in the Health Sciences Center. This room is accessible to persons with disabilities and can facilitate audio and video recording.
2.3. Subjects
The study established a sampling goal of 30 participants, and the enrollment closed when 27 older adults completed the study. This limitation was necessary because the study required three to five participants to hold concurrent group sessions. Therefore, the subjects for the study were 27 older adults (24 females) with mean age of 75 years old [(SD 7.50), age range: 65–89 years old]. The majority of participants lived alone (70.4%), and the remainder lived with either a spouse or daughter. Table 1 presents the baseline sociodemographic characteristics (pre-intervention Co-Factors in the PNI model) for both groups. To participate in the study, potential participants should meet the following inclusion criteria. 1) All patients should be 65 years of age or older. 2) They must have a minimum loneliness score of 40 on the revised 20-item UCLA Loneliness scale [40]. 3) Participants should be living in the community. 4) They have been diagnosed with at least one chronic illness. 5) Each participant must have voluntarily signed an informed consent form prior to enrollment. Participants were excluded on the basis of the following criteria. 1) Potential participants who had lost their spouse within the last 2 years were excluded to control for grief reaction. 2) Those who had cognitive impairment with scores less than 23 on the Folstein mini-mental status exam did not participate. 3) Those with institutional living were excluded. 4) Those with significant psychiatric or developmental problems that prevented their ability to independently answer survey questions were also excluded.
Table 1.
Baseline characteristics of randomized participants.
| Variable | LISTEN group (N = 15) | AC group (N = 12) | Difference statistic |
|---|---|---|---|
| Age [mean years (SD)] | 74.93 (7.39) | 75.21 (7.97) | t = 0.9, p = 0.93 |
| Gender | χ2 = 2.70, p = 0.10 | ||
| Male | 3 | 0 | |
| Female | 12 | 12 | |
| Marital status | χ2 = 0.49, p = 0.78 | ||
| Married, spouse in home | 4 | 4 | |
| Separated, divorced, never married | 7 | 4 | |
| Widowed | 4 | 4 | |
| Highest education completed | χ2 = 1.02, p = 0.79 | ||
| High school or less | 3 | 4 | |
| Some college | 3 | 2 | |
| Undergraduate degree | 6 | 3 | |
| Graduate degree | 3 | 3 | |
| Household Income ($/year) | χ2 = 2.37, p = 0.31 | ||
| Less than $20,000 | 4 | 6 | |
| $20,001 to $40,000 | 8 | 3 | |
| Over $40,000 | 3 | 3 | |
| Number of people living in home [mean (SD)] | 1.36 (0.75) | 1.50 (0.80) | t = 0.47, p = 0.64 |
| Employment status | χ2 = 1.49, p = 0.48 | ||
| Retired and not working | 12 | 8 | |
| Working part-time | 3 | 3 | |
| Working full-time | 0 | 1 | |
| Total Katz basic ADLs [mean (SD)] | 6.5 (0.9) | 6.4 (1.2) | t = −0.13, p = 0.90 |
| Total Katz instrumental ADLs [mean (SD)] | 13.2 (3.2) | 13.2 (3.2) | t = −0.01, p = 0.99 |
| Total chronic illnesses [mean (SD)] | 2.9 (0.38) | 2.6 (1.6) | t = −0.47, p = 0.64 |
| Loneliness score [mean (SD)] | 47.0 (6.5) | 51.8 (9.5) | t = 1.53, p = 0.14 |
Note. AC = attention control, SD = standard deviation, total values may not be exactly 100% because of estimation.
Note. Chi-Square test for gender was performed only for a 2 × 2 table because no males were randomized to the control group.
The t and chi-square symbols were italicized to indicate the statistical test and the N was italicized as it is an abbreviation for sample size of each group.
2.4. Study procedures
Participants were recruited through advertisement in a family primary care center, which was university based and serves as a multi-county area of rural and small urban communities. The study team also placed advertisements in local and regional newspapers. Potential participants contacted the clinic via phone to volunteer. Prior to enrollment, all potential participants completed a screening to assess for meeting the basic inclusion and exclusion criteria. Participants were then scheduled for the initial enrollment meeting, in which they were first given the opportunity to read all informed consent forms and ask questions. After the participants signed consent to participate, baseline enrollment data were collected, and the participants were randomized into either LISTEN group or educational attention control group. Both groups (three to five participants at a time) met weekly for a total of five times (2 h each time). Reminder letters and phone calls were used for the weekly group sessions. After completing the fifth session, the participants answered survey questions by phone at 1 and 6 weeks after the last group session and attended a face-to-face meeting at 12 weeks post-intervention for final data collection.
2.5. Study comparators
2.5.1. LISTEN: the intervention
LISTEN was developed using the Medical Research Council framework for complex intervention development [41]. The development process of LISTEN, including information about the underlying theoretical frameworks, has been previously published [29] along with the initial feasibility and acceptability evaluation data [30]. The psychophysiological links between loneliness and chronic illness made it logical to propose an intervention that targeted this stress mechanism by encouraging rethinking the experience of loneliness to enhancing meaning and facilitate moving forward. LISTEN is delivered sequentially and weekly, in five 2 h sessions. The content of the sessions was derived from the health and social science literature on loneliness, and the sessions are designed to be sequential, focusing first on belonging, then relationships, role in community, loneliness as a health challenge, and meaning of loneliness. Participants begin each session with writing; during weeks 1–4, the participants complete unique homework assignments relevant to the content for the upcoming week.
2.5.2. Attention control group
The attention control group met weekly for 2 h time periods each week for a total of 5 weeks. This group received educational information about aging, including contents on Common Physical Changes with Aging, Eating for Health, Aging and Health, Stroke Prevention, and Preventive Care. The attention control group educational sessions were scripted; hence, the content was the same for each small group.
2.6. Fidelity to the intervention
The LISTEN and attention control groups met on the same days, at the same time, and in similar location and room settings; both groups were given the same break with the same refreshments. The LISTEN and attention control groups had separate trained interventionists to prevent contamination of the intervention. Prior to the intervention study, all team members were trained to understand the study protocol, which was reviewed prior to enrollment of each cohort of patients. All intervention and control group sessions were audio and video recorded to assess for fidelity to LISTEN and to assess for potential contamination in the attention control group. Recordings were reviewed by the study team after each session to monitor the fidelity to LISTEN.
2.7. Instruments and measures
2.7.1. Neuroimmunological stress
Salivary cortisol, DHEA, IL-6, and IL-2 levels were measured at enrollment and at 12 weeks after the final intervention session as indicators of physiological stress response, inflammation, and immunity. The Adrenocortex Stress Profile Kit was used as a measure of salivary cortisol. Saliva was collected from the participants at four different time points in a 24 h period, and the study team then transported the saliva samples to the University Medical Laboratories, where the samples were sent out for analysis to Genova Diagnostics [42]. The Adrenocortex Stress Profile evaluates cortisol and DHEA levels, both of which are linked to anti-inflammatory response and stress resistance. IL-6 and IL-2 were determined from the blood samples processed at the University Medical Laboratories [43].
2.7.2. Psychosocial functioning
Depression was measured using the five-item Geriatric Depression Scale (GDS) [44]. The current scale was reported as comparable to prior versions of GDS in both reliability and validity in populations of older adults. Loneliness was measured using the revised UCLA Loneliness Scale [40]. The scale consists of 20 items with several items reverse scored, and the possible total scores range from 20 to 80. This scale has been reported as reliable and valid in varied populations [45]. Loneliness was assessed at enrollment and at 1, 6, and 12 weeks after the last intervention session. Social support was measured using the MOS Social Support Scale. This scale includes subscales of tangible support, emotional support, and affective support and has been widely used to assess social support in varied populations [46]. Functional ability was assessed using the Katz ADL and IADL instruments [47]. The Katz Activities of Daily Living instruments have been used widely in populations of older adults to assess basic and instrumental functional ability. All measures of psychosocial functioning were collected at enrollment and at 12 weeks after the last intervention session.
2.7.3. Quality of life
The quality of life was measured using a visual analog scale ranging from 0 to 10. This scale has been reported as highly correlating with other measures of quality of life [48]. The quality of life was assessed at enrollment and at 1, 6, and 12 weeks after the last intervention session.
2.7.4. Physical health measures
Blood pressure was measured by a trained registered nurse using an appropriately calibrated sphygmomanometer. Fasting glucose was measured after the participants fasted for at least 8 h. The fasting glucose level was measured by a trained registered nurse using an appropriately calibrated glucometer. BMI was calculated using the measures of height and weight taken in the family medicine center by using a calibrated scale and height measure. Physical measures were collected at enrollment and at 12 weeks after the last intervention session.
3. Statistical analyses
Data were analyzed using Statistical Package for the Social Sciences 23.0. Methods for analysis included a comprehensive descriptive analysis of all study variables, followed by bivariate analysis for significant relationships among the study variables. Mean comparisons were conducted using a repeated-measures analysis of variance for the main study outcome variables while controlling for baseline depressive symptoms. The level of statistical significance was set at p < 0.05. Loneliness and quality of life were the only two variables collected at four time points. For these two variables, Mauchly’s test was performed to assess the effect size within subjects.
4. Results
The LISTEN and attention control groups did not differ significantly on any of the baseline demographic characteristics (Table 1). Table 2 provides the mean comparisons between baseline measures and those at 12 weeks after the last intervention session for outcome variables measured alone at these time points.
Table 2.
Mean comparisons for outcome variables measured at enrollment and 12 weeks post-intervention.
| Outcome | Group | Baseline
|
12 Weeks post
|
F | p | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Morning rise in salivary cortisol | LISTEN | 0.58 | 0.45 | 0.46 | 0.68 | 3.65 | *0.07 |
| Control | 0.55 | 0.34 | 0.34 | 0.23 | |||
| DHEA | LISTEN | 76.48 | 51.22 | 39.30 | 42.05 | 0.76 | 0.39 |
| Control | 82.82 | 46.49 | 61.73 | 64.52 | |||
| IL-6 | LISTEN | 6.25 | 12.19 | 9.62 | 17.91 | 0.38 | 0.54 |
| Control | 0.99 | 7.24 | 7.66 | 16.6 | |||
| IL-2 | LISTEN | 2.25 | 0.59 | 2.06 | 0.39 | 0.277 | 0.60 |
| Control | 2.34 | 0.43 | 2.64 | 0.69 | |||
| Depression (GDS) | LISTEN | 1.96 | 1.34 | .852 | 1.06 | 3.779 | 0.13 |
| Control | 1.79 | 1.42 | 1.81 | 1.79 | |||
| MOS total social support | LISTEN | 59.13 | 15.9 | 64.98 | 12.49 | 3.99 | *0.05 |
| Control | 56.36 | 19.07 | 52.36 | 16.42 | |||
| Emotional support subscale | LISTEN | 22.47 | 7.29 | 24.57 | 7.12 | 2.31 | 0.14 |
| Control | 20.75 | 8.66 | 22.42 | 5.93 | |||
| Tangible support subscale | LISTEN | 12.33 | 5.31 | 14.38 | 4.00 | 7.01 | **0.01 |
| Control | 12.82 | 5.05 | 10.36 | 5.27 | |||
| Affectionate support subscale | LISTEN | 10.60 | 3.31 | 11.93 | 2.22 | 1.21 | 0.28 |
| Control | 9.67 | 4.07 | 9.75 | 4.63 | |||
| Positive social interaction subscale | LISTEN | 10.47 | 3.33 | 10.58 | 2.36 | 0.31 | 0.58 |
| Control | 9.17 | 4.30 | 8.67 | 3.05 | |||
| Basic ADL | LISTEN | 6.47 | 0.91 | 6.49 | 0.91 | 0.92 | 0.35 |
| Control | 6.42 | 1.16 | 6.08 | 0.29 | |||
| Instrumental ADL | LISTEN | 13.20 | 3.19 | 12.73 | 2.31 | 2.92 | 0.10 |
| Control | 13.45 | 3.29 | 12.36 | 3.35 | |||
| Fasting glucose | LISTEN | 111.8 | 48.77 | 112.08 | 19.24 | 0.43 | 0.51 |
| Control | 108.7 | 36.24 | 118.80 | 60.40 | |||
| Systolic blood pressure | LISTEN | 137.63 | 14.41 | 126.93 | 13.62 | 6.43 | *0.02 |
| Control | 132.67 | 20.84 | 130.00 | 18.33 | |||
| Diastolic blood pressure | LISTEN | 77.98 | 8.18 | 75.00 | 9.03 | 1.92 | 0.18 |
| Control | 77.33 | 11.95 | 74.58 | 9.13 | |||
| Body mass index | LISTEN | 29.94 | 7.93 | 29.52 | 7.97 | 2.61 | 0.12 |
| Control | 30.67 | 5.91 | 29.53 | 7.97 | |||
Note. Variables are presented in order of presentation in the PNI model (Fig. 1).
= p ≤ .05,
= p ≤ .01. GDS is the 5-item Geriatric Depression Scale.
4.1. Neuroimmunological stress
Morning rise in salivary cortisol changed over the course of the study. Both LISTEN and control group means decreased between enrollment and 12 weeks post-intervention. DHEA, IL-6, and IL-2 were not significant, but both the LISTEN and control groups decreased in morning rise in cortisol and DHEA over the course of the study. In addition, mean levels of IL-6 increased for both groups. The groups were not equal at baseline on IL-6. This finding may be attributed to the different experiences of chronic illnesses, including rheumatoid arthritis, and this result may have skewed the Il-6 data. However, even when controlling for the chronic illness diagnoses, the IL-6 values were not significantly different from baseline to 12 weeks post-intervention. The mean levels of IL-2 decreased for the LISTEN group and increased for the attention control group, but the difference was not significant.
4.2. Psychosocial functioning and quality of life
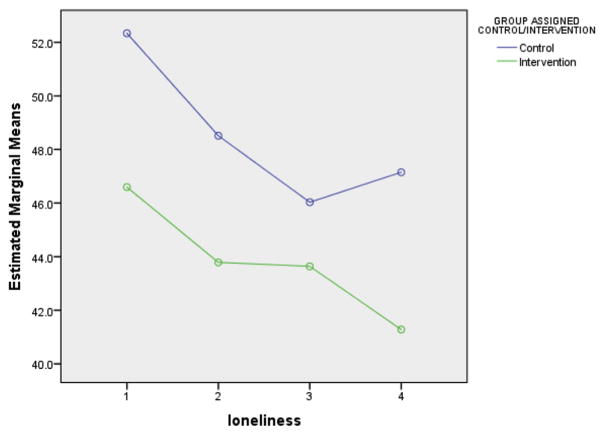
Twelve weeks after the last intervention session, the LISTEN group presented reduced depressive symptoms, and this finding was clinically relevant but not statistically significant. At completion of the study, the LISTEN group demonstrated significantly less loneliness (p = 0.018) than that of the attention control group. Loneliness and quality of life were assessed at four time points, and the mean comparisons for these variables are presented in Table 3. When loneliness was compared at all four time points for within-subjects effect and while controlling for baseline depressive symptoms, Mauchly’s W was 0.725 (p = 0.198). Assuming sphericity, the Epsilonb Greenhouse–Geisser value was 0.859, and the four means were not equal [F (3, 72) = 3.060, p = 0.034]. Fig. 2 illustrates the mean loneliness scores at each time point; as shown in the figure, the loneliness in the LISTEN group continued to decline, whereas the attention control group achieved mean loneliness scores that trended upward between 6 and 12 weeks after the last session.
Table 3.
Mean comparisons for loneliness and quality of life.
| Outcome | Group | Baseline
|
1 Week post
|
6 Weeks post
|
12 Weeks post
|
F | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||||
| Loneliness (R–UCLA) | LISTEN | 46.00 | 5.33 | 43.57 | 5.89 | 43.79 | 7.18 | 41.19 | 5.83 | 4.142 | *0.02 |
| Control | 51.79 | 9.55 | 48.08 | 10.47 | 45.42 | 11.43 | 47.79 | 8.39 | |||
| Quality of life (VAS) | LISTEN | 7.07 | 1.94 | 7.33 | 1.59 | 7.26 | 1.98 | 7.90 | 1.49 | 1.168 | 0.13 |
| Control | 7.41 | 1.91 | 6.33 | 2.10 | 6.79 | 3.08 | 6.96 | 1.98 | |||
Note. R-UCLA is the revised 20-item UCLA Loneliness Scale (scores range from 20 to 80). VAS is the Visual Analog Scale for Quality of Life (scores range from 0 to 10).
= p < 0.05.
Fig. 2.
Changes in mean loneliness scores from baseline to 12 weeks post intervention.
The mean quality-of-life scores are also presented in Table 3. As shown in the table, the quality of life increased slightly for the LISTEN group and decreased slightly for the attention control group, but the changes were not significant. The total social support scores changed with mean scores for the LISTEN group increasing significantly (p = 0.05). The subscale with the greatest change was the tangible support subscale, in which the control group reported less support, whereas the LISTEN group reported more support (p = 0.01). The LISTEN group reported maintenance of basic functional ability, whereas the attention control group reported a slight decline in function.
4.3. Physical health measures
The LISTEN group demonstrated clinically relevant changes in fasting glucose, but these changes were not statistically significant. The mean fasting glucose levels increased in both groups at baseline. The LISTEN group achieved <1 mg/dl change in mean fasting glucose, whereas the control group, who received lectures on healthy diet, yielded a mean increase of 10.1 mg/dl in mean fasting glucose. The changes in systolic blood pressure were statistically significant (p = 0.018) with mean systolic blood pressures in the LISTEN group dropping below 130, which is a clinically relevant finding in an older adult sample. The mean diastolic blood pressure and BMI did not differ significantly between the groups after intervention.
5. Discussion
This study employed a randomized controlled trial design to identify LISTEN as a potential intervention for diminishing loneliness and the poor health outcomes associated with loneliness in chronically ill, lonely, older adults. Prior reviews of interventions and one meta-analysis of interventions [26] suggested that the most successful intervention for loneliness would be one that specifically targets the cognitive mis-perceptions or thinking errors that occur during loneliness.
This study is the first to employ LISTEN as a potential method to reduce feelings of loneliness. LISTEN is the first group intervention designed to bring lonely people together to offer their narrative of loneliness in a therapeutic environment and in a sequenced way, aiming to facilitate cognitive restructuring. The structure of this intervention facilitates a change in cognitive perspective; hence, one can view loneliness as an experience that can be challenged with individualized actions.
The findings of this study will provide additional information about the relationship between loneliness and depressive symptoms. Primarily, participants of the LISTEN group reported diminished depressive symptoms; this result is significant, given the links between depression and negative health outcomes, which recently included sensory impairments and suicide [49,50]. The findings emphasize that untreated loneliness can lead to an increase in depressive symptoms in a relatively short period of time. Previous literature reported that loneliness and depression are separate unique constructs [51]; loneliness is predictive of depression [16], and this relationship is not reciprocal. Our findings indicating that untreated lonely persons may report increased depressive symptoms over a period of only 4 months emphasize the need for proactive assessment and treatment of loneliness. Considering that depression is negatively associated with poor chronic illness outcomes [15], depression should be prevented if possible. Research has posited that treating loneliness prior to the development of depressive symptoms can significantly reduce such symptoms, thereby greatly saving expenses on the healthcare system [52].
An extensive literature on loneliness and social support has detailed how people who perceive social support to be low may experience loneliness. Particularly in older adult populations worldwide, lonely older adults have reported social isolation [53], lack of meaningful connection [54], or diminished social networks [55]. Our findings indicating that participants of LISTEN perceived overall enhanced social support were unexpected because participating in LISTEN did not provide any enhancement of tangible support. The structure of LISTEN may have contributed to this change because participants of LISTEN reported that they were beginning to take actions against loneliness by seeking tangible means of support, joining exercise courses, and joining community organizations. These actions occurred after gaining the opportunity to cognitively process their experience of loneliness.
LISTEN integrates the key concepts from narrative therapy and cognitive behavioral therapy to offer the participants the opportunity to share a narrative of their personal experience of loneliness. Narrative therapy has been used to diminish depressive symptoms, and recent studies have concluded that both narrative therapy and cognitive behavioral therapy can result in diminished depressive symptoms [56]. Being able to share one’s experience of loneliness and live the vicarious experience of another who is lonely may have changed the perception of social support [57] for participants of the LISTEN group.
Two national data analyses have identified loneliness as a predictive factor of functional decline and mortality in older adult samples [58,59]. The current literature links loneliness to the decline of both physical and cognitive functions [60]. Considering that the LISTEN group maintained physical functional ability, the diminishing loneliness may result in behavioral changes that can facilitate maintenance of function. Given that the untreated group diminished slightly in both basic and instrumental activities of daily living, the importance of taking on loneliness as a complex health phenomenon is highlighted. Longitudinal studies on LISTEN are needed to further determine whether diminishing loneliness in chronically ill, lonely, older adults can result in any regained functional ability. Lonely older adults may lose function because of their self-isolating behavior or lack of activity. Therefore, with the right support or intervention, intrinsic motivation can be altered and may lead to increased activity.
The findings related to salivary cortisol, DHEA, IL-6, and IL-2 are exploratory and have created more questions. The diminished rise in salivary cortisol in the control group may indicate underlying chronic stress response and flattening of the cortisol rhythm [8]. Given that the present study had the inclusion criterion of a minimum UCLA loneliness score of 40, all the study participants were at least moderately lonely and were likely to demonstrate a slightly flattened cortisol rhythm at study enrollment. Although the loneliness of the LISTEN participants decreased significantly, the mean scores at 12 weeks were still not indicative of the overall absence of loneliness. In addition, the participants presented multiple chronic conditions, including rheumatoid arthritis, which may have skewed the IL6 results [61]. Recent studies indicate that lonely older adults showed increased cytokine production compared with non-lonely persons; this finding suggests a proinflammatory response [62].
The findings related to physical health measures are consistent with the literature indicating that loneliness is linked to hypertension [63] through the physiological stress response [9]. Changes in systolic blood pressure were clinically significant because the mean systolic blood pressure of the LISTEN group decreased within the guidelines for management of hypertension for older adults [64]. This finding is very important because patients seen clinically and are above this goal are frequently prescribed with higher doses of new antihypertensive medication, which can lead to other adverse reactions. Previous studies indicated that loneliness can increase blood pressure over long periods of time [65], and this effect is very problematic given the relationship between high blood pressure, cardiovascular illness, and stroke. Thus, diminishing the physiological stress response to loneliness can prevent hypertension. One of the potential downstream effects is the prevention of stroke or secondary stroke. Our preliminary studies on loneliness of ischemic stroke survivors in Appalachia indicate that loneliness is a prevalent problem for stroke survivors, and this feeling is linked to multiple domains in this population [66].
5.1. Limitations
The main limitation of this study is the relatively small homogeneous sample. The majority of female sample limits true generalizability of the findings to older men in Appalachia. The participants were all community dwelling; hence, the findings cannot be generalized to older adults living in long-term care or other assisted living settings. Moreover, the participants were not assessed for being native to Appalachia. Given that Appalachian women identify strongly with their kin, this factor is also a limitation. Assessing for birthplace in future studies will be important; consequently, logical inferences can be made regarding loneliness and Appalachian culture.
5.2. Planning for future research
Future steps will be multifaceted and will comprehensively evaluate the potential use of LISTEN as a therapeutic strategy for loneliness in varied populations. The study team is currently evaluating the feasibility and acceptability of LISTEN as a therapy for loneliness in survivors of ischemic stroke (funded by WVCTSI NIGM, U54GM104942). Additional studies on the significance of the changes in IL-6 and IL-2 are needed to further determine how the treatment of loneliness can affect inflammatory or immune changes that may in turn influence chronic conditions. The planned subsequent steps include seeking funding to conduct large-scale longitudinal trials of LISTEN to appropriately assess the long-term health and health system benefits of diminishing loneliness. Future trials are being designed to report on the resources needed to deliver LISTEN, as well as the potential scalability, replicability, and costs of such delivery. In summary, LISTEN can effectively diminish loneliness and reduce systolic blood pressure, with increased self-reported social support compared with the attention control group. The importance of sharing experiences of loneliness and gaining the opportunity to find out how others are coping with loneliness was described by the participants as the most significant part of their participation in LISTEN. Study participants noted that being open to listening to how others coped with loneliness led to the adoption of new behavior after completing the study.
References
- 1.Wilson C, Moulton B. Loneliness among older adults: a national survey of adults 45+ Washington, DC 20049: AARP; 2010. [Google Scholar]
- 2.Stessman J, Rottenberg Y, Shimshilashvili I, Ein-Mor E, Jacobs JM. Loneliness, health, and longevity. J Gerontol A Biol Sci Med Sci. 2014;69(6):744–50. doi: 10.1093/gerona/glt147. [DOI] [PubMed] [Google Scholar]
- 3.Wang G, Zhang X, Wang K, Li Y, Shen Q, Ge X, et al. Loneliness among the rural older people in Anhui, China: prevalence and associated factors. Int J Geriatr Psychiatry. 2011;26(11):1162–8. doi: 10.1002/gps.2656. [DOI] [PubMed] [Google Scholar]
- 4.Yang KM, Victor CR. The prevalence of and risk factors for loneliness among older people in China. Ageing Soc. 2008;28(3):305–27. [Google Scholar]
- 5.Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness, clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238–49. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Currie C. Social determinants of health and well-being among young people: Health Behaviour in School-Aged Children (HBSC) study: international report from 2009/2010 survey. Copenhagen: World Health Organization Regional Office for Europe; 2012. [Google Scholar]
- 7.Hawkley LC, Cole SW, Capitanio JP, Norman GJ, Cacioppo JT. Effects of social isolation on glucocorticoid regulation in social mammals. Horm Behav. 2012;62(3):314–23. doi: 10.1016/j.yhbeh.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doane LD, Adam EK. Loneliness and cortisol: momentary, day-to-day, and trait associations. Psychoneuroendocrinology. 2010;35(3):430–41. doi: 10.1016/j.psyneuen.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29(5):593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- 10.Hackett RA, Hamer M, Endrighi R, Brydon L, Steptoe A. Loneliness and stress-related inflammatory and neuroendocrine responses in older men and women. Psychoneuroendocrinology. 2012;37(11):1801–9. doi: 10.1016/j.psyneuen.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 11.Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, et al. Pain, depression, and fatigue: loneliness as a longitudinal risk factor. Health Psychol. 2014;33(9):948–57. doi: 10.1037/a0034012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Momtaz YA, Hamid TA, Yusoff S, Ibrahim R, Chai ST, Yahaya N, et al. Loneliness as a risk factor for hypertension in later life. J Aging Health. 2012;24(4):696–710. doi: 10.1177/0898264311431305. [DOI] [PubMed] [Google Scholar]
- 13.Thurston RC, Kubzansky LD. Women, loneliness, and incident coronary heart disease. Psychosom Med. 2009;71(8):836–42. doi: 10.1097/PSY.0b013e3181b40efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright A, Pritchard ME. An examination of the relation of gender, mass media influence, and loneliness to disordered eating among college students. Eat Weight Disord. 2009;14(2–3):E144–7. doi: 10.1007/BF03327813. [DOI] [PubMed] [Google Scholar]
- 15.Theeke LA, Mallow J. Original research: loneliness and quality of life in chronically ill rural older adults. Am J Nurs. 2013;113(9):28–37. doi: 10.1097/01.NAJ.0000434169.53750.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging. 2006;21(1):140–51. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- 17.Lamis DA, Ballard ED, Patel AB. Loneliness and suicidal ideation in drug-using college students. Suicide Life Threat Behav. 2014;44(6):629–40. doi: 10.1111/sltb.12095. [DOI] [PubMed] [Google Scholar]
- 18.Theeke LA, Goins RT, Moore J, Campbell H. Loneliness, depression, social support, and quality of life in older chronically ill Appalachians. J Psychol. 2012;146(1–2):155–71. doi: 10.1080/00223980.2011.609571. [DOI] [PubMed] [Google Scholar]
- 19.Berto P, D’Ilario D, Ruffo P, Virgilio RD, Rizzo F. Depression: cost-of-illness studies in the international literature, a review. J Ment Health Policy Econ. 2000;3(1):3–10. doi: 10.1002/1099-176x(200003)3:1<3::aid-mhp68>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 20.van den Elzen AJ, Fokkema CM. Home visits to the elderly in Leiden: an investigation into the effect on loneliness. Tijdschr Gerontol Geriatr. 2006;37(4):142–6. [PubMed] [Google Scholar]
- 21.Fokkema CM, van Tilburg TG. Loneliness interventions among older adults: sense or nonsense? Tijdschr Gerontol Geriatr. 2007;38(4):185–203. [PubMed] [Google Scholar]
- 22.Hartke RJ, King RB. Telephone group intervention for older stroke caregivers. Top Stroke Rehabil. 2003;9(4):65–81. doi: 10.1310/RX0A-6E2Y-BU8J-W0VL. [DOI] [PubMed] [Google Scholar]
- 23.Martina CM, Stevens NL. Breaking the cycle of loneliness? Psychological effects of a friendship enrichment program for older women. Aging Ment Health. 2006;10(5):467–75. doi: 10.1080/13607860600637893. [DOI] [PubMed] [Google Scholar]
- 24.Shapira N, Barak A, Gal I. Promoting older adults’ well-being through internet training and use. Aging Ment Health. 2007;11(5):477–84. doi: 10.1080/13607860601086546. [DOI] [PubMed] [Google Scholar]
- 25.Creswell JD, Irwin MR, Burklund LJ, Lieberman MD, Arevalo JM, Ma J, et al. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: a small randomized controlled trial. Brain Behav Immun. 2012;26(7):1095–101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15(3):219–66. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheng ST. Loneliness-distress and physician utilization in well-elderly females. J Comm Psych. 1992;20(1):43–56. [Google Scholar]
- 28.Meltzer H, Bebbington P, Dennis MS, Jenkins R, McManus S, Brugha TS. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2012;48(1):5–13. doi: 10.1007/s00127-012-0515-8. [DOI] [PubMed] [Google Scholar]
- 29.Theeke LA, Mallow JA. The development of LISTEN: a novel intervention for loneliness. Open J Nurs. 2015;5(2):136–43. doi: 10.4236/ojn.2015.52016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Theeke LA, Mallow JA, Barnes ER, Theeke E. The feasibility and acceptability of LISTEN for Loneliness. Open J Nurs. 2015;5(5):416–25. doi: 10.4236/ojn.2015.55045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGarvey E, Leon-Verdin M, Killos L, Guterbock T, Cohn W. Health disparities between Appalachian and non- Appalachian counties in Virginia. J Community Health Nurs. 2011;36(3):348–56. doi: 10.1007/s10900-010-9315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haaga J. The aging of Appalachia: demographic and socioeconomic change in Appalachia. Washington, DC: 2004. [Google Scholar]
- 33.Halverson JA, Ma L, Harner EJ. An analysis of disparities in health status and access to care in the appalachian region. Washington, DC: Appalachian Regional Commission; 2004. [accessed 02.08.16]. www.prb.org/pdf04/householdsfamiliesappalachi.pdf. [Google Scholar]
- 34.Friedman B, Conwell Y, Delavan RL. Correlates of late-life major depression: a comparison of urban and rural primary care patients. Am J Geriatr Psychiatry. 2007;15(1):28–41. doi: 10.1097/01.JGP.0000224732.74767.ad. [DOI] [PubMed] [Google Scholar]
- 35.McCulloch The relationship of family proximity and social support to the mental health of older rural adults: the Appalachian Context. J Aging Stud. 1985;9(1):17. [Google Scholar]
- 36.Patrick JH, Cottrell LE, Barnes KA. Gender, emotional support, and well-being among rural elderly. Sex Roles. 2001;45(1):15–29. [Google Scholar]
- 37.Davis RA, Magilvy J. Quiet pride: the experience of chronic illness by rural older adults. J Nurs Scholarsh. 2000;32(4):385–90. doi: 10.1111/j.1547-5069.2000.00385.x. [DOI] [PubMed] [Google Scholar]
- 38.Theeke LA, Mallow J, Gianni C, Legg K, Glass C. The experience of older women living with loneliness and chronic conditions in Appalachia. Rural Ment Health. 2015;39(2):61–72. doi: 10.1037/rmh0000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCain NL, Gray DP, Walter JM, Robins J. Implementing a comprehensive approach to the study of health dynamics using the Psychoneuroimmunology paradigm. ANS Adv Nurs Sci. 2005;28(4):320–32. doi: 10.1097/00012272-200510000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39(3):472–80. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- 41.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. Int J Nurs Stud. 2013;50(5):587–92. doi: 10.1016/j.ijnurstu.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 42.Genova Diagnostics G. [accessed 15.03.16];Adrenocortex stress profile. Available at: https://www.gdx.net/core/one-page-test-descriptions/Adrenocortex-Test-Description.pdf.
- 43.WVU Medicine. University Medical Laboratories; [accessed 15.03.16]. Available at: http://wvumedicine.org/health-professionals/services-for-healthcare-professionals/ [Google Scholar]
- 44.Rinaldi P, Mecocci P, Benedetti C, Ercolani S, Bregnocchi M, Menculini G, et al. Validation of the five-item geriatric depression scale in elderly subjects in three different settings. J Am Geriatr Soc. 2003;51(5):694–8. doi: 10.1034/j.1600-0579.2003.00216.x. [DOI] [PubMed] [Google Scholar]
- 45.Russell DW. UCLA loneliness scale (version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 46.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 47.Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970;10(1):20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 48.de Boer AGE, van Lanschot JJB, Stalmeier PFM, van Sandick JW, Hulscher BF, de Haes JCJ, et al. Is the single-item visual analogue scale as valid, reliable and responsive as multi-item scales in measuring quality of life. Qual Life Res. 2004;13(2):311–20. doi: 10.1023/B:QURE.0000018499.64574.1f. [DOI] [PubMed] [Google Scholar]
- 49.Sivam A, Wroblewski KE, Alkorta-Aranburu G, Barnes LL, Wilson RS, Bennett DA, et al. Olfactory dysfunction in older adults is associated with feelings of depression and loneliness. Chem Senses. 2016;41(4):293–9. doi: 10.1093/chemse/bjv088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mezuk B, Rock A, Lohman MC, Choi M. Suicide risk in long-term care facilities: a systematic review. Int J Geriatr Psychiatry. 2014;29(12):1198–211. doi: 10.1002/gps.4142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago health, aging, and social relations study. Psychol Aging. 2010;25(2):453–63. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.VanderWeele TJ, Hawkley LC, Thisted RA, Cacioppo JT. A marginal structural model analysis for loneliness: implications for intervention trials and clinical practice. J Consult Clin Psychol. 2011;79(2):225–35. doi: 10.1037/a0022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saito T, Kai I, Takizawa A. Effects of a program to prevent social isolation on loneliness, depression, and subjective well-being of older adults: a randomized trial among older migrants in Japan. Arch Gerontol Geriatr. 2012;55(3):539–47. doi: 10.1016/j.archger.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 54.Smith JM. Portraits of loneliness: emerging themes among community-dwelling older adults. J Psychosoc Nurs Ment Health Serv. 2012;50(4):34–9. doi: 10.3928/02793695-20120306-04. [DOI] [PubMed] [Google Scholar]
- 55.Fokkema T, De Jong Gierveld J, Dykstra PA. Cross-national differences in older adult loneliness. J Psychol. 2012;146(1–2):201–28. doi: 10.1080/00223980.2011.631612. [DOI] [PubMed] [Google Scholar]
- 56.Lopes RT, Goncalves MM, Machado PP, Sinai D, Bento T, Salgado J. Narrative therapy vs. cognitive-behavioral therapy for moderate depression: empirical evidence from a controlled clinical trial. Psychother Res. 2014;24(6):662–74. doi: 10.1080/10503307.2013.874052. [DOI] [PubMed] [Google Scholar]
- 57.Holm AL, Severinsson E. Surviving depressive ill-health: a qualitative systematic review of older persons’ narratives. Nurs Health Sci. 2014;16(1):131–40. doi: 10.1111/nhs.12071. [DOI] [PubMed] [Google Scholar]
- 58.Luo Y, Hawkley LC, Waite LJ, Cacioppo JT. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74(6):907–14. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172(14):1078–83. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Donovan NJ, Wu Q, Rentz DM, Sperling RA, Marshall GA, Glymour MM. Loneliness, depression and cognitive function in older U.S. adults. Int J Geriatr Psychiatry. 2016 doi: 10.1002/gps.4495. http://dx.doi.org/10.1002/gps.4495. [DOI] [PMC free article] [PubMed]
- 61.Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, Atkinson C, Malarkey WB, Glaser R. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. PNAS. 2003;100(15):9090–5. doi: 10.1073/pnas.1531903100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jaremka LM, Fagundes CP, Peng J, Bennett JM, Glaser R, Malarkey WB, et al. Loneliness promotes inflammation during acute stress. Psychol Sci. 2013;24(7):1089–97. doi: 10.1177/0956797612464059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hawkey LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21(1):152–64. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- 64.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint national committee (jnc 8) JAMA. 2014;311(5):507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 65.Hawkley LC, Thisted RA, Masi CM, Cacioppo JT. Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol Aging. 2010;25(1):132–41. doi: 10.1037/a0017805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Theeke LA, Horstman P, Mallow B, Culp AM, Lucke-Wold A, Domico J, et al. Quality of life and loneliness in stroke survivors living in Appalachia. J Neurosci Nurs. 2014;46(6):E3–15. doi: 10.1097/JNN.0000000000000097. [DOI] [PMC free article] [PubMed] [Google Scholar]