Abstract
Introduction
This study examined feasibility of a place-based community health worker (CHW) and health advocate (HA) initiative in five public housing developments selected for high chronic disease burden and described early outcomes.
Methods
This intervention was informed by a mixed-method needs assessment performed December 2014–January 2015 (representative telephone survey, n=1,663; six focus groups, n=55). Evaluation design was a non-randomized, controlled quasi-experiment. Intake and 3-month follow-up data were collected February–December 2015 (follow-up response rate, 93%) on 224 intervention and 176 comparison participants, and analyzed in 2016. All participants self-reported diagnoses of hypertension, diabetes, or asthma. The intervention consisted of chronic disease self-management and goal setting through six individual CHW-led health coaching sessions, instrumental support, and facilitated access to insurance/clinical care navigation from community-based HAs. Feasibility measures included CHW service satisfaction and successful goal setting. Preliminary outcomes included clinical measures (blood pressure, BMI); disease management behaviors and self-efficacy; and preventive behaviors (physical activity).
Results
At the 3-month follow-up, nearly all intervention participants reported high satisfaction with their CHW (90%) and HA (76%). Intervention participants showed significant improvements in self-reported physical activity (p=0.005) and, among hypertensive participants, self-reported routine blood pressure self-monitoring (p=0.013) compared with comparison participants. No improvements were observed in self-efficacy or clinical measures at the 3-month follow-up.
Conclusions
Housing-based initiatives involving CHW and HA teams are acceptable to public housing residents and can be effectively implemented to achieve rapid improvements in physical activity and chronic disease self-management. At 3-month assessment, additional time and efforts are required to improve clinical outcomes.
Introduction
Place-based initiatives are a potentially effective approach to reduce health disparities among residents living in underserved neighborhoods.1 Community health workers (CHWs) and health advocates (HAs) can play a role in advancing community health.2 CHWs are health professionals who provide healthcare support and have a close understanding of communities they serve through shared ethnicity, culture, language, and life experiences.3 HAs provide health insurance enrollment and post-enrollment healthcare navigational assistance.4 In limited settings, CHWs have been deployed in public housing to address specific health needs, support health promotion, or build social capital.5–8 None have been launched with municipal funds.
In January 2015, a partnership among a city health agency, housing authority, community-based organizations, and academic partners was launched to address the health of residents in East Harlem, New York City, a neighborhood with high rates of obesity, diabetes, and barriers to health care.9 This publicly financed initiative, the Harlem Health Advocacy Partnership, was guided by a health equity framework10 and offered CHW services to housing residents to manage chronic diseases and set health goals, as well as insurance navigational assistance by a team of HAs to help residents find, understand, and use affordable/low-cost health insurance and health care, and review plan options. This study aimed to demonstrate feasibility and examine preliminary effectiveness.
Methods
Study Design
Intervention design and protocol was developed between June 2014 and January 2015 through meetings between partner institutions and interactions with public housing resident leaders. Participants were recruited from five public housing developments representing 12,720 residents; developments were selected for high hemoglobin A1c levels per health surveillance data.11 Intervention inclusion criteria were age ≥ 18 years; self-reported diagnosis of hypertension, diabetes, or asthma; fluency in English or Spanish; and participation consent.
The intervention was informed by a mixed-method needs assessment performed by academic partners from December 2014 to January 2015 (random sample telephone survey, n=1,663; six focus groups, n=55) among residents living in selected housing developments, as well as in five nearby developments with comparable demographic/health status make-up (comparison community). Needs assessment details have been published elsewhere as a report to policymakers and stakeholders.11
Intervention evaluation design was a non-randomized, controlled quasi-experiment. Most intervention and all comparison participants were recruited from the needs-assessment telephone survey if they reported hypertension, diabetes, or asthma diagnoses and expressed interest; additional recruitment of intervention participants occurred via local health fairs and outreach. Intake and 3-month follow-up data collection by academic partners occurred February–December 2015; a brief in-person questionnaire and biometric assessment of blood pressure, height, and weight were administered at each time point. All participants received a $20 cash incentive for completing follow-up survey.
CHWs were recruited from targeted housing residences and broader East Harlem community, hired by a local community- based organization, and trained in CHW core competencies, health education, goal setting, and in facilitating linkages to care by referring to HAs employed by another local community-based organization expert in health insurance enrollment and access to care issues. The CHW intervention included six or more educational/instrumental support visits, as well as referral to HAs as needed. CHW and HAs were trained separately on respective competencies but jointly on Harlem Health Advocacy Partnership protocol/referral processes. HA support was available to both intervention and comparison communities.
Measures
At each visit, blood pressure was measured three times and averaged for analyses. Self-reported physical activity, general mental health status, self-perceived chronic disease management, healthcare access, self-efficacy, and quality of life were assessed at each time point.
Statistical Analysis
Group differences in demographics, health insurance, and general health characteristics were compared using chi-square tests. Between-group differences in changes in outcome measures from baseline to follow-up were assessed using mixed models for continuous outcomes and generalized estimating equations for categorical outcomes. Each model included time (baseline, follow up); group (intervention, comparison); and their interaction term. Models adjusted for baseline age to account for older average age among intervention participants and conducted using SAS, version 9.2, or Stata, version 12. Analyses were conducted in 2016.
Results
Needs assessment survey results confirmed no statistically significant differences in aggregate demographics, health insurance status/type, self-reported health, or health behaviors between residents in intervention and comparison developments (Appendix, available online). Prevalence of targeted health conditions (hypertension, diabetes, and asthma) was also similar.
Despite comparable aggregate demographic/health status profiles between residents in intervention and comparison developments, participants who enrolled into the intervention were significantly older than those enrolled in the comparison group (Figure 1). A greater proportion of intervention participants self-reported a hypertension diagnosis (87% vs 71%, p=0.001) and being diagnosed with all three reported conditions (18% vs 11%, p=0.056), but a lower proportion reported having diagnosed asthma (38% vs 50%, p=0.045). The intervention group experienced greater attrition (11%) between baseline and follow-up than the comparison group (3%), with a total response rate of 93%. Analyses were based on 199 intervention and 171 comparison participants with follow-up information, adjusting for between-group age differences.
Figure 1.
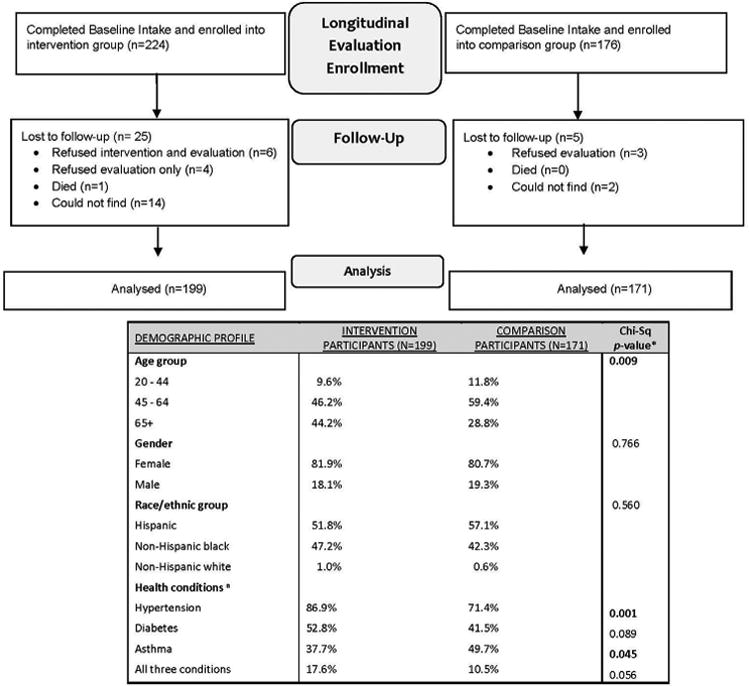
Participant CONSORT diagram for longitudinal evaluation of HHAP intervention, East Harlem, New York City, 2015.
Note: Boldface indicates statistical significance (p<0.05).
aHealth conditions are adjusted for age. HHAP, Harlem Health Advocacy Partnership.
Nearly all (90%) intervention participants reported high satisfaction with their CHW and most (76%) established personal goals at follow-up. Measured clinical outcomes did not improve in intervention versus comparison participants over time (Table 1). At follow-up, however, intervention participants reported greater improvements in physical activity than comparison participants (p=0.005), and those with hypertension reported greater improvements in self-monitoring of blood pressure (p=0.013). Intervention participants were also more likely to receive help from an HA in solving health insurance problems (p=0.019, not shown). Of those receiving HA support, 97% found services helpful. Compared with comparison participants, intervention participants were more likely to report at follow-up having changed their health insurance or insurance status (11% vs 4%, p=0.009), and to report having changed their personal doctor (14% vs 6%, p=0.024). Open-ended responses confirmed high satisfaction with the program (Appendix, available online).
Table 1. Behavioral and Clinical Outcomes at Baseline and at 3-Month Follow-Up, Intervention Versus Comparison Group: East Harlem, New York City, 2015.
| Intervention group (n=199) | Comparison group (n=171) | Estimated between-group difference | ||||||
|---|---|---|---|---|---|---|---|---|
| Outcome | Baseline | 3-month FU | p-value | Baseline | 3-month FU | p-value | Difference (95% CI) | p-value |
| Measured clinical outcomes, M (SD) | ||||||||
| Systolic blood pressure (SBP) | 132.8 (21.3) | 133.0 (22.1) | 0.866 | 128.8 (20.8) | 124.3 (19.4) | 0.004 | 3.79(-0.14, 7.72) | 0.059 |
| Diastolic blood pressure (DBP) | 82.6 (12.3) | 83.9 (13.7) | 0.274 | 82.4 (12.3) | 81.1 (12.5) | 0.106 | 2.32(-0.05, 4.69) | 0.055 |
| BMI | 33.5 (7.8) | 33.7 (8.2) | 0.415 | 34.3 (8.6) | 34.1 (8.2) | 0.102 | 0.39(-0.05, 0.82) | 0.082 |
| Self-reported behaviors, M (SD) | ||||||||
| Average number of days of physical activity, past 2 weeks | 4.6 (5.1) | 6.6 (5.8) | <0.001 | 5.7 (5.6) | 5.9 (5.6) | 0.840 | 1.90(0.58, 3.23) | 0.005 |
| General health | ||||||||
| % reporting mental health status as “Excellent,” “Very good,” or “Good” | 56.7 | 69.0 | 0.025 | 70.0 | 66.5 | 0.972 | 0.12(-0.10, 0.34) | 0.303 |
| Hypertension management | ||||||||
| % reporting they are managing their hypertension well | 80.5 | 88.8 | 0.019 | 85.1 | 86.7 | 0.781 | 0.07(-0.03, 0.17) | 0.149 |
| % with diagnosed hypertension at baseline who routinely measure their own blood pressure | 45.6 | 60.7 | 0.001 | 44.3 | 43.8 | 0.897 | 0.15(0.03, 0.26) | 0.013 |
| Diabetes management | ||||||||
| % reporting they are managing their diabetes well | 65.7 | 80.0 | 0.011 | 75.0 | 84.5 | 0.073 | 0.05(-0.09, 0.18) | 0.504 |
| % with diagnosed diabetes at baseline who routinely measure their glycemic levels | 74.0 | 72.1 | 0.662 | 63.2 | 59.2 | 0.561 | 0.02(-0.12, 0.16) | 0.819 |
| Asthma management | ||||||||
| % reporting they are managing their asthma well | 87.5 | 79.7 | 0.151 | 85.0 | 82.4 | 0.589 | -0.05(-0.19, 0.09) | 0.491 |
Note: Boldface indicates statistical significance (p<0.05). Absolute difference is shown for blood pressure, BMI, and average days of physical activity in the estimated between-group difference column. Difference in % improved is shown for percentage-based outcomes.
FU, follow-up.
Discussion
This evaluation of a publicly funded, place-based CHW initiative found using locally recruited CHWs and facilitated referrals to HAs to be well received by low-income housing residents and effective at rapidly improving services navigation, self-reported physical activity, and self-management behaviors. Findings are consistent with literature suggesting that CHW programs generally achieve positive outcomes for chronic disease prevention and self-management when supportive relationships with patients are developed,7,12,13 and high satisfaction levels and risk reduction can be achieved when programs established in public housing settings use residents as workers.5,6 In early intervention months, it was challenging to improve clinical outcomes. Other studies have documented challenges in improving clinical outcomes, depending heavily on integration with clinical services, dose, and intervention standardization.14,15
Limitations
Findings should be interpreted while being mindful of key limitations. First, this was a controlled quasi-experiment; participants in treatment and control groups were not randomly selected. Intervention participants were older and in worse health than comparison participants, reducing the effectiveness of the comparison proxy group. Second, sample size limited the statistical power to detect differences.
Conclusions
These findings demonstrate the feasibility of a municipal health department leading a place-based CHW/HA intervention targeting multiple chronic conditions using public funds, catalyzed by multisector partnerships. Findings also stress the importance of collective monitoring of early results, which, for this project, has yielded increased attention to building formal clinical integration mechanisms and improved documentation of intervention fidelity. Such innovative models inform and align with Medicaid Expansion and other policy efforts designed to more effectively link communities to care.
Supplementary Material
Acknowledgments
This publication is a product of the Prevention Research Centers Program at the Centers for Disease Control and Prevention. The findings and conclusions in this publication are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the National Institute on Minority Health and Health Disparities.
We would like to acknowledge the following individuals for their contribution to the design and implementation of the Harlem Health Advocacy Partnership intervention and evaluation: Margaret Baker Ryerson, Albert Tovar, Gabriel Martinez, Vanessa Jimenez, Najuma Abdullah, Violeta Alvarado, Noah Amuzu, Kevin Anderson, Sonia Angell, Eugene Averkiou, Sindia Avila, Michelene Blum, LaShawn Brown-Dudley, Thomas Can- nell, Lauren Carey, Matthew Caron, Shadi Chamany, Georges Compagnon, Iris Cooney, Brigitte Cousins, Nneka Lundy De La Cruz, Cynthia Curry, Sheila Desai, Cadine DeSouza, Khady Diaby, Katherine Earle, Noel Mayindo, Ayman El Mohandes, Folake Eniola, Anne-Marie Flatley, Aline Da Fonseca, Martin Frankel, Marc Gourevitch, Cynthia Greaves, Fangtao He, Diana Herrera, Yong Hwang, Amber Levanon-Seligson, Maritza Martinez, Yaxkyn Mejia, Chris Palmedo, Lara Rabiee, Adam Ramos, Jerome Richardson, Jesica Rodriguez-Lopez, Nerisusan Rosario, Charlene Ryan, Crystal Sacaridiz, Tara Smith, Jamil Soriano, Cassiopia Toner, Diane Vasquez, and Sterling Walker.
We would like to acknowledge all other staff in the New York City Health Department not mentioned here who have contributed to the Harlem Health Advocacy Partnership project, in particular, for vision and leadership from Commissioner Dr. Mary T. Bassett and Executive Deputy Commissioner Dr. Oxiris Barbot and the work of the Department’s Center for Health Equity and Harlem District Public Health Office staff. We would also like to thank New York City Housing Authority’s executive staff, resident leaders, borough Property Management staff, and Community Operations staff for their support, and the many active residents and community leaders who participate in the intervention and evaluation. Last, a special thank-you to the Baruch College Survey Research team for careful execution of the telephone survey.
The efforts of Drs. Thorpe, Trinh-Shevrin, and Islam and Ms. Lopez and Riley are supported in part by the Centers for Disease Control and Prevention (CDC) Grant U48DP001904. Trinh- Shevrin, Islam, and Riley are also supported in part by the NIH National Institute on Minority Health and Health Disparities Grant P60MD000538 and NIH National Center for the Advancement of Translational Science Grant UL1TR000038.
Footnotes
This article is part of a supplement issue titled Prevention Research Centers Program – 30th Anniversary: Translating Applied Public Health Research into Policy and Practice.
No financial disclosures were reported by the authors of this paper.
Supplemental Material: Supplemental materials associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.amepre.2016.08.034.
References
- 1.Shmedley B, Amaro H. Advancing the science and practice of placed- based intervention. Am J Public Health. 2016;106(2):197. http://dx.doi.org/10.2105/AJPH.2015.303043. [Google Scholar]
- 2.CDC. A policy and systems-level approach. CDC; [Accessed February 2016]. Addressing CDC chronic disease through community health workers. www.cdc.gov/dhdsp/docs/chw_brief.pdf. Published April 2015. [Google Scholar]
- 3.American Public Health Association. APHA Policy Brief. American Public Health Association; [Accessed February 2016]. Support for community health workers to increase health access and to reduce health inequities. http://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/09/14/19/support-for-community-health-workers-to-increase-health-access-and-to-reduce-health-inequities. Published 2009. [Google Scholar]
- 4.de Jung T, Tracy C, Benjamin ER. Connecting consumers to coverage: the role of navigators and consumer assistance programs in implementing health reform in New York. NYS Health Foundation; [Accessed March 2016]. http://nyshealthfoundation.org/uploads/resources/navigators-consumer-assi-stance-programs-september-2011.pdf. Published September 2011. [Google Scholar]
- 5.Slater JS, Ha CN, McGovern P, et al. A randomized community trial to increase mammography utilization among low-income women living in public housing. Prev Med. 1998;27(6):862–870. doi: 10.1006/pmed.1998.0370. http://dx.doi.org/10.1006/pmed.1998.0370. [DOI] [PubMed] [Google Scholar]
- 6.Andrews JO, Tingen MS, Jarriel SC, et al. Application of a CBPR framework to inform a multi-level tobacco cessation intervention in public housing neighborhoods. Am J Community Psychol. 2012;50(1-2):129–140. doi: 10.1007/s10464-011-9482-6. http://dx.doi.org/10.1007/s10464-011-9482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brownstein JN, Chowdhury FM, Norris SL, et al. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med. 2007;32(5):435–447. doi: 10.1016/j.amepre.2007.01.011. http://dx.doi.org/10.1016/j.amepre.2007.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Quintiliani LM, DeBiasse MA, Branco JM, Bhosrekar SG, Rorie JA, Bowen DJ. Enhancing physical and social environments to reduce obesity among public housing residents; rationale, trial design, and baseline data for the Healthy Families study. Contemp Clin Trials. 2014;39(2):201–210. doi: 10.1016/j.cct.2014.08.005. http://dx.doi.org/10.1016/j.cct.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 9.King L, Hinterland K, Dragan KL, et al. Community Health Profiles 2015, Manhattan Community District 11: East Harlem. 2015;11(59):1–16. [Google Scholar]
- 10.Center for Health Equity. NYC Department of Health and Mental Hygiene. [Accessed July 2016]; www1.nyc.gov/site/doh/health/neighborhood-health/center-for-health-equity.page. Published 2016.
- 11.Feinberg A, Seidl L, Levanon Seligson A, et al. Launching a neighborhood-based community health worker initiative: Harlem Health Advocacy Partner (HHAP) Community Needs Assessment. [Accessed August 2016];A joint report by the NYU-CUNY Prevention Research Center, New York City Department of Health and Mental Hygiene, New York City Housing Authority, and Community Service Society. www1.nyc.gov/assets/doh/downloads/pdf/dpho/neighborhood-based-chw-ilnitiative.pdf. Published December 2015.
- 12.Costa EF, Guerra PH, Santos TI, Florindo AA. Systematic review of physical activity promotion by community health workers. Prev Med. 2015;81:114–121. doi: 10.1016/j.ypmed.2015.08.007. http://dx.doi.org/10.1016Aj.ypmed.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Viswanathan M, Kraschnewski J, Nishikawa B, et al. Outcomes of community health worker interventions. Evid Rep Technol Assess. 2009;181:1–144. [PMC free article] [PubMed] [Google Scholar]
- 14.Smalls BL, Walker RJ, Bonilha HS, Campbell JA, Egede LE. Community interventions to improve glycemic control in African Americans with type 2 diabetes: a systemic review. Glob J Health Sci. 2015;7(5):171–182. doi: 10.5539/gjhs.v7n5p171. http://dx.doi.org/10.5539/gjhs.v7n5p171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Verhagen I, Steunenberg B, de Wit NJ, Ros WJ. Community health worker interventions to improve access to health care services for older adults from ethnic minorities: a systematic review. BMC Health Serv Res. 2014;13(14):497. doi: 10.1186/s12913-014-0497-1. http://dx.doi.org/10.1186/s12913-014-0497-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


