Abstract
Introduction
Vasectomy is the simplest, safest, and most effective form of definitive fertility control in men [1]. Vasectomy is used for 10% of contraception worldwide but only for 2% in Germany [2]. The aim of this study was to investigate the impact of vasectomy on the sexual satisfaction of sterilized men and their partners.
Material and methods
Vasectomized men and their partners were surveyed by means of the IIEF (International Index for Erectile Function) and the FSFI (Female Sexual Function Index) questionnaires. A total of 294 couples were surveyed; 90 men answered the IIEF, and 74 women answered the FSFI. The results of the questionnaires were compared to a historical comparison group. The men were also surveyed with a not validated questionnaire, which was returned by 95 men. The two-sample t-test for independent samples, the chi-squared test, and the Wilcoxon-Mann-Whitney test were carried out.
Results
The vasectomized men had significantly better results than the healthy historical comparison group in the IIEF domains of erectile function, orgasm, sexual desire, and intercourse satisfaction. For the female partners of the sterilized men, there were almost no significant differences in any questions of the FSFI in comparison to the control group. A significant difference was observed only in the domain ‘arousal’.
Conclusions
Vasectomy does not have a negative impact on the sexual satisfaction of the affected couples. In fact, sexual satisfaction improved for the sterilized men, while the satisfaction of the women was not reduced by the vasectomy.
Keywords: vasectomy, sexual satisfaction, IIEF, FSF
INTRODUCTION
Vasectomy, the use of condoms, periodic abstinence, and coitus interruptus are the only possibilities for contraception that are in the hands of men. Vasectomy is the simplest and most reliable method of fertility control [1]. Currently, sterilization of men is substantially less accepted in Germany than in other parts of the world. Vasectomy is used in ca. 10% of men worldwide but only in 2% of men in Germany [2]. In recent years, we have observed a clear increase in the acceptance of vasectomy and a rise of the number of sterilizations performed.
The most important aspect of patient informing is that the men are conscious of the definitiveness of the procedure. Up to 5–10% of men, and even up to 20% in one large study [3], later regret their decision for sterilization. The cause of this regret is usually a consequence of the high rate of divorce/separation today, so these men then have a new partner, who then has a yearning to have children. Within 10 years after the procedure, ca. 2% of the men have undergone a refertilization. Having no children and a younger age are risk factors in regards to the desire for refertilization [4].
A frequently expressed apprehension of men considering vasectomy and their partners is the concern that their sexlife could be significantly changed. Sterilization of men has no noticeable influence on the volume of ejaculate. About 95% of ejaculate is produced by the prostate and the vesiculae. A study on 204 vasectomized men showed that the ejaculation volume after a vasectomy was only 0.3 ml smaller than before the operation [5]. During the patient informing visit, many patients ask about the influence of the sterilization on erectile function and sexual satisfaction. Their female partners often play a decisive role in the decision-making for vasectomy and also in the informing in regards to possible negative effects on sexuality.
The aim of this study was to survey operated men and also their female partners about the influence of the vasectomy on their sexual satisfaction.
MATERIAL AND METHODS
In order to investigate the influence of vasectomy on the sexual satisfaction of the couples, the Female Sexual Function Index (FSFI) [6] and the International Index of Erectile Function (IIEF) [6] were used. The IIEF consists of 15 questions. These questions are about the effects that erection problems have on sexual life. All these questions refer to the past four weeks. The FSFI consists of 19 questions that relate to the sexual feelings and reactions of the woman during the previous four weeks.
We surveyed men with the IIEF and their female partners with the FSFI who were vasectomized in the Frankfurt Vasectomy Center from August 2012 until January 2015. Two very experienced surgeons carried out the surgical procedures.
The sterilizations were carried out using the no-scalpel technique, since this has a lower rate of complications in regards to pain, inflammation, and bleeding [7].
Since the data collection was retrospective and anonymous, ethics approval was not required, according to the stipulations of the responsible ethics commission of the Frankfurt State Chamber of Physicians.
A total of 294 couples were surveyed. The results of the questionnaires were compared with the healthy control groups of the studies by Rosen et al. for the validation of the FSFI or IIEF [6, 8]. The control groups can be compared with our groups under investigation, since both cases concerned patients without known erectile or sexual dysfunction. The erectile and sexual function was determined in both groups by self-assessment using IIEF or FSFI, respectively.
In addition to the two validated questionnaires (IIEF and FSFI), the men were surveyed with an unofficial questionnaire that we developed. This questionnaire recorded, above all, the influence of the vasectomy on various aspects of sexual life.
The postoperative questionnaire after vasectomy can be found in Supplement 1.
The two-sample t-test for independent samples, the chi-squared test, and the Wilcoxon-Mann-Whitney test were used.
RESULTS
The IIEF was completed by 90 of the vasectomized patients we surveyed.
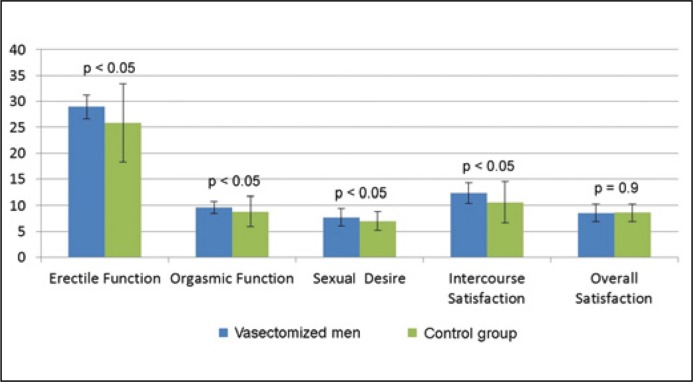
The sterilization had taken place between 3 months and 2.5 years prior. In four of the five domains of the IIEF, the vasectomized men had a significantly higher score than the healthy historical control group. There was no significant difference except in the domain, ‘General Satisfaction’ (p = 0.9) (Table 1, Figure 1).
Table 1.
Comparison of IIEF of vasectomized men and control group [6]
| Domain | Vasectomized men (n = 90) | Control group (n = 109) | p-value |
|---|---|---|---|
| Erectile function | 28.92 ±2.27 | 25.8 ±7.6 | 0.0002262 |
| Orgasmic function | 9.66 ±1.15 | 8.8 ±2.9 | 0.0088053 |
| Sexual desire | 7.73 ±1.64 | 7.0 ±1.8 | 0.0034167 |
| Intercourse satisfaction | 12.29 ±1.94 | 10.6 ±3.9 | 0.0002367 |
| Overall satisfaction | 8.57 ±1.71 | 8.6 ±1.7 | 0.9017779 |
Figure 1.
Comparison of IIEF of vasectomized men and control group.
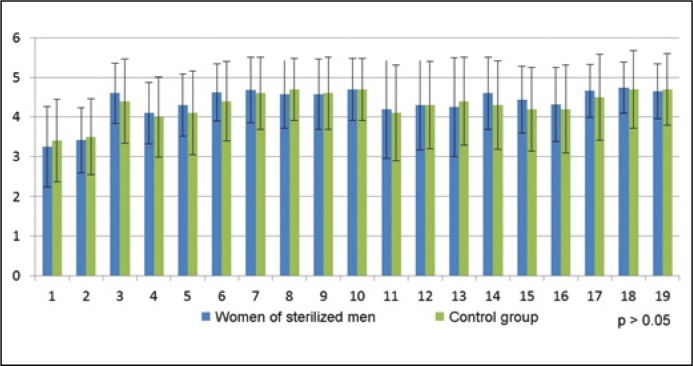
Seventy-four female partners of the men vasectomized in our center completed the FSFI. In comparison with the healthy control population from the literature, there was a p-value greater than 0.05 for each question, so there were no significant differences between women with a vasectomized partner and the healthy control group for any of the questions (Table 2, Figure 2).
Table 2.
Comparison of FSFI questions of women of sterilized men and control group [5]
| Question | Women of sterilized men (n = 74) | Control group (n = 129) | p-value |
|---|---|---|---|
| 1 | 3.25 ±1.01 | 3.4 ±1.04 | 0.3187836 |
| 2 | 3.41 ±0.83 | 3.5 ±0.96 | 0.5007267 |
| 3 | 4.6 ±0.76 | 4.4 ±1.06 | 0.15548 |
| 4 | 4.1 ±0.78 | 4.0 ±1.01 | 0.4632205 |
| 5 | 4.3 ±0.78 | 4.1 ±1.06 | 0.15795825 |
| 6 | 4.62 ±0.72 | 4.4 ±1.01 | 0.1008844 |
| 7 | 4.68 ±0.83 | 4.6 ±0.91 | 0.5345489 |
| 8 | 4.57 ±0.86 | 4.7 ±0.79 | 0.2759911 |
| 9 | 4.57 ±0.89 | 4.6 ±0.92 | 0.8212242 |
| 10 | 4.7 ±0.79 | 4.7 ±0.79 | 1 |
| 11 | 4.19 ±1.24 | 4.1 ±1.21 | 0.6137781 |
| 12 | 4.3 ±1.13 | 4.3 ±1.11 | 1 |
| 13 | 4.25 ±1.25 | 4.4 ±1.11 | 0.3774207 |
| 14 | 4.6 ±0.92 | 4.3 ±1.12 | 0.0518514 |
| 15 | 4.44 ±0.85 | 4.2 ±1.06 | 0.0976154 |
| 16 | 4.32 ±0.94 | 4.2 ±1.11 | 0.4347584 |
| 17 | 4.66 ±0.67 | 4.5 ±1.09 | 0.2539257 |
| 18 | 4.74 ±0.65 | 4.7 ±0.98 | 0.7541456 |
| 19 | 4.65 ±0.69 | 4.7 ±0.91 | 0.6824334 |
Figure 2.
Comparison of FSFI questions of women of sterilized men and control group.
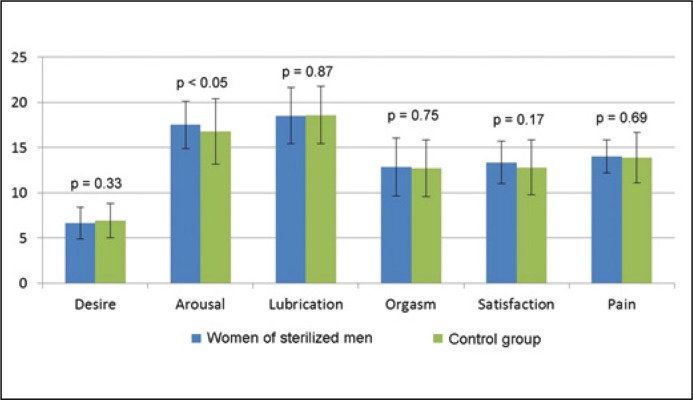
Also in the six domains, the mean scores of the women with vasectomized partners diverged only slightly from those of the control population. In five of the six domains, there was no significant difference between the two groups. A significant difference was observed only in the domain ‘Arousal’ (Table 3, Figure 3).
Table 3.
Comparison of FSFI domains of women of sterilized men and control group [5]
| Domain | Women of sterilized men (n = 74) | Control group (n = 129) | p-value |
|---|---|---|---|
| Desire | 6.64 ±1.74 | 6.9 ±1.89 | 0.3329079 |
| Arousal | 17.51 ±2.62 | 16.8 ±3.62 | 0.0023549 |
| Lubrication | 18.53 ±3.12 | 18.6 ±3.17 | 0.8791063 |
| Orgasm | 12.85 ±3.21 | 12.7 ±3.16 | 0.7465425 |
| Satisfaction | 13.36 ±2.37 | 12.8 ±3.03 | 0.1730101 |
| Pain | 14.04 ±1.82 | 13.9 ±2.79 | 0.6993024 |
Figure 3.
Comparison of FSFI domains of women of sterilized men and control group.
Ninety-five men answered our own questionnaire. In this questionnaire, 37.9% of the vasectomized men stated that their sexual life had improved after the surgical procedure. The reason for this was that contraception was no longer needed. Both independence from condoms as well as independence from hormonal contraception of the partner were referred to here. According to the men, this led to a more spontaneous, relaxed, and freer sexual life.
A 95% confidence interval was calculated for the categories, ‘sexual life improved’ and ‘sexual life unchanged’. For ‘sexual life improved’, the lower limit was 27% and the upper limit was 48%. In other words, this means that if the vasectomy was performed again, at least 27% would report that they were more satisfied with their sexual life than before. For the category ‘sexual life unchanged’, the limits were between 52% and 73%. Therefore, with a probability of 95%, vasectomy has no negative impact on sexual life whatsoever on at least half of the men.
More frequent sexual intercourse after vasectomy was reported by 12.4% of the men; the frequency was unchanged in 83.1%.
The question as to how the men would rate their maximum discomfort in the first week after vasectomy was answered by 22.8% with ‘hardly any pain’. None of the patients indicated a value of 9 or 10 (unbearable pain) on a scale of 1–10.
68.4% of the patients had no bothersome symptoms after vasectomy while 31.6% still felt the effects of vasectomy. These were for example a 'strange sensation' or changes in orgasm.
92.6% of patients had the same partner at the time of the survey as at the time of vasectomy, 7.4% had a new partner.
Regarding the question of the frequency of sexual intercourse, 15.9% reported having one to two times per month of sexual intercourse. 22.7% of patients had sex more than eight times per month. The other frequencies were relatively evenly distributed.
97.7% of patients would undergo vasectomy again, only 2.27% of patients would not opt for vasectomy in the future.
In a two-group comparison, it was tested whether the women of the men who reported a better sexual life than before the vasectomy had a higher FSFI score than the women of the men whose sexual life had not changed. The Wilcoxon-Mann-Whitney test was used for this with the two group variables, ‘sexual life improved’ and ‘sexual life unchanged’. A significant difference between the two groups could not be found in any of the domains. The subjective perception of the men that sexual life had improved was not confirmed by the women in this study.
DISCUSSION
Vasectomy is the most reliable and also the best method of contraception, under the decisive precondition that the family planning of the man is definitively finished [9]. The complication rate is low in the hands of an experienced surgeon [10]. The effects of vasectomy on the sexual life, the mindset of the patients and their female partners has already been described in a few studies [11, 12]. Since the influence of vasectomy on sexual satisfaction depends also on the experience of the surgeon, the aim of this study was to investigate this issue in a sample that was operated in a specialized high-volume center.
One concern that is often voiced in the preoperative consultation is the question of a potential negative influence of vasectomy on sexuality. Based on our results, we were able to show that the sexual satisfaction of the female partners is not influenced negatively by the sterilization of the man and the satisfaction of the operated man is even improved. Vasectomy of men therefore does not appear to negatively influence the sexual life of their female partners.
This insight is an important piece of information for the preoperative consultation, in order to be able to soundly answer these questions. The reason for the positive development of male sexual satisfaction is presumably the absence of anxiety of unwanted pregnancies.
In order to investigate the influence of vasectomy on the sexual satisfaction of the couples, it is of course in dispensible to compare the postoperative data with a preoperative sample. Since only the questionnaires of the already operated men were available in this retrospective study, we compared these data with a historical sample. These control groups were the healthy comparison groups consisting of test persons of North America and Western Europe from the publications by Rosen et al. on the description of the IIEF and the FSFI [6, 8]. The retrospective design of our study is certainly the most important limitation of this work. It would have been better to survey the same couples preoperatively and postoperatively. However, such data were not available, so we decided to make a comparison with a historical sample. A subsequent study with a comparison of the postoperative data to the preoperative data of the same couples is currently underway.
About 30% of the surveyed couples sent back the questionnaires. As with all questionnaire-based data, there might exist a certain selection bias, since it is entirely possible that mostly satisfied couple sent back the questionnaires. In that case, there would be a distortion of the results, if predominantly the couples whose sexual satisfaction deteriorated after the vasectomy did not send back the questionnaires.
Furthermore, there was the problem that, although we sent each patient three questionnaires (the IIEF, the FISI, and the unofficial questionnaire we developed), sometimes not all three questionnaires were answered, and among the answered questionnaires, not all of them were filled out completely, resulting possibly in selection bias. Therefore it is conceivable that satisfied men answered the questionnaire but their possibly unsatisfied female partners did not. Specifically, in this study, the questionnaire we developed was answered the most often, followed by the IIEF, and least often the FSFI. In addition, it is conceivable that the partners did not answer the questionnaire in an honest way because their partners were able to read the answers.
Vasectomy is a safe and very reliable method of contraception. This method of contraception is clearly less accepted in Germany than in other countries, such as in the USA. The recognition that the sterilization of men does not have a negative influence on the sexual satisfaction of the couples concerned could have a positive effect on the acceptance of vasectomy.
CONCLUSIONS
Vasectomy is a safe method of contraception and in cases of completed family planning it could be the method of first choice. The fear that sexual satisfaction could be reduced by the procedure is unfounded. In this study, we were able to show that the sexual satisfaction of men improved and that that of the women did not diminish.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
For this type of study formal consent is not required.
Compliance with Ethical Standards.
Supplement 1
Postoperative questionnaire after vasectomy
How long does your vasectomy date back to?
How would you rate your maximum discomfort in the first week after vasectomy? Please indicate the severity of pain on a scale of 1 to 10. (1 = hardly pain, 10 = unbearable pain).
At present, are you still having problems after vasectomy? If so, please specify.
Do you still have the same partner as at the time of vasectomy?
Has your sexual life changed since vasectomy? If so, how?
How often do you have sex per month?
Has the frequency of sexual intercourse changed after vasectomy? If so, please specify.
If any, what is the most significant change in your life attributable to vasectomy?
If you had to make the decision again, would you undergo vasectomy once again?
References
- 1.Dohle GR, Diemer T, Kopa Z, Krausz C, Giwercman A, Jungwirth A. European Association of Urology Working Group on Male Infertility European Association of Urology guidelines on vasectomy. Eur Urol. 2012;61:159–163. doi: 10.1016/j.eururo.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization 1991 Noticeboard Vasectomy and cancer. Lancet. 1991;338:1586. [Google Scholar]
- 3.Sharma V, Le BV, Sheth KR, Zargaroff S, Dupree JM, Cashy J, Brannigan RE. Vasectomy demographics and postvasectomy desire for future children: results from a contemporary national survey. Fertil Steril. 2013;99:1880–1885. doi: 10.1016/j.fertnstert.2013.02.032. [DOI] [PubMed] [Google Scholar]
- 4.Holman CD, Wisniewski ZS, Semmens JB, Rouse IL, Bass AJ. Population-based outcomes after 28.246 in-hospital vasectomies and 1.902 vasovasostomies in western Australia. BJU Int. 2000;86:1043–1049. doi: 10.1046/j.1464-410x.2000.00977.x. [DOI] [PubMed] [Google Scholar]
- 5.Leader AJ, Axelrad SD, Frankowski R, Mumford ST. Complications of 2.711 vasectomies. J Urol. 1974;111:365–369. doi: 10.1016/s0022-5347(17)59967-x. [DOI] [PubMed] [Google Scholar]
- 6.Rosen R, Brown C, Heiman J, et al. Female Sexual Function Index. J Sex Marital Ther. 2000;26:191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- 7.Cook LA, Pun A, Gallo MF, Lopez LM, Van Vliet HA. Scalpel versus no-scalpel incision for vasectomy. Cochrane Database Syst Rev. 2014;30:CD004112. doi: 10.1002/14651858.CD004112.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Rosen RC, Riley A, Wagner G, et al. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–830. doi: 10.1016/s0090-4295(97)00238-0. [DOI] [PubMed] [Google Scholar]
- 9.Zini A, Grantmyre J, Chan P. CUA guideline: Vasectomy. Can Urol Assoc J. 2016;10:E274–278. doi: 10.5489/cuaj.4017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lowe G. Optimizing outcomes in vasectomy: how to ensure sterility and prevent complications. Transl Androl Urol. 2016;5:176–180. doi: 10.21037/tau.2016.03.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohamad Al-Ali B, Shamloul R, Ramsauer J, et al. The effect of vasectomy on the sexual life of couples. J Sex Med. 2014;11:2239–2242. doi: 10.1111/jsm.12567. [DOI] [PubMed] [Google Scholar]
- 12.Smith A, Lyons A, Ferris J, Richters J, Pitts M, Shelley J. Are sexual problems more common in men who have had a vasectomy? A population-based study of Australian men. J Sex Med. 2010;7(2 Pt 1):736–742. doi: 10.1111/j.1743-6109.2009.01565.x. [DOI] [PubMed] [Google Scholar]