Abstract
Introduction
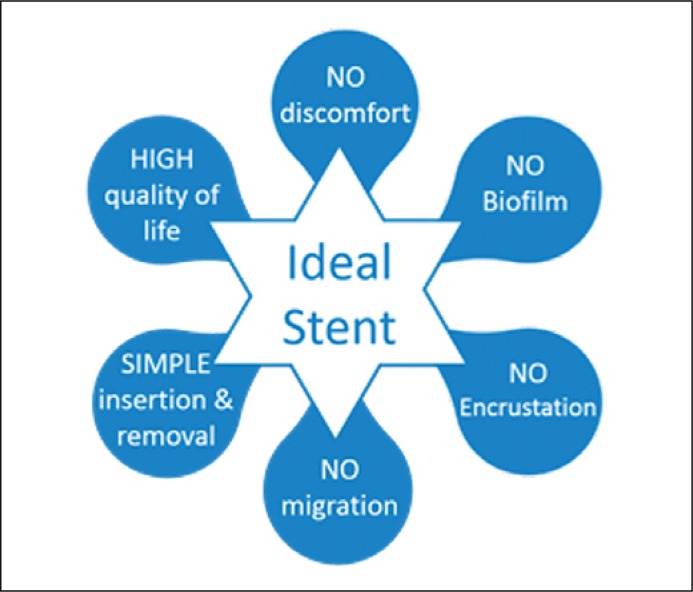
An ideal stent would offer simple insertion and removal with no discomfort and/or migration, it would have no biofilm formation or encrustation and would also maintain the patient's quality of life.
Material and methods
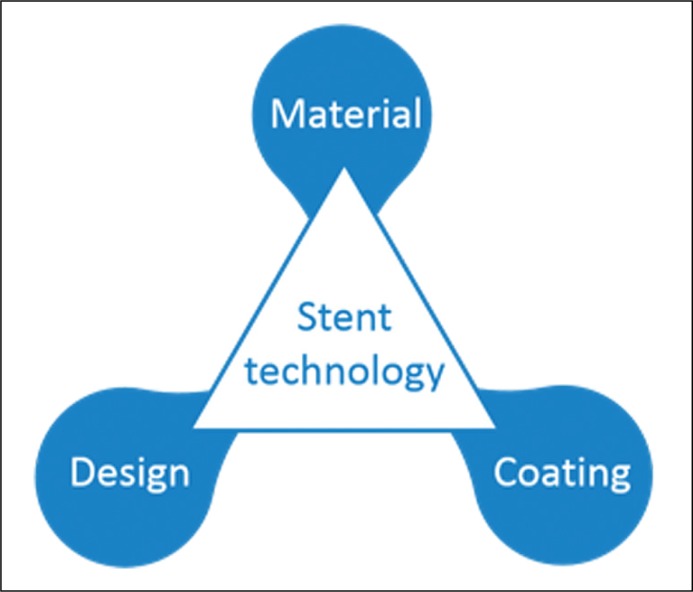
In this mini-review, we outlined the engineering developments related to stent material, design and coating.
Results
There have been a wide variety of in-vitro, model-based, animal-based and clinical studies using a range of commercial and non-commercial stents. Ureteric stents have evolved since their first usage with a wider range of stent design, material and coating available for laboratory and clinical use.
Conclusions
While engineering innovations have led to the evolution of stents, more work needs to be done to address the issues relating to stent encrustation and biofilm formation.
Keywords: engineering, ureter, stent, design, material, coating
INTRODUCTION
Ureteral stents are deployed to overcome intrinsic or extrinsic causes of upper urinary tract obstruction, thus aiding the drainage of urine from kidneys to the bladder [1, 2]. They are often related to the treatment of kidney stone disease (KSD) and with a rising incidence and a lifetime prevalence of KSD at 14%, the use of stents is going to increase further [3]. Since their first use, stents have been prone to mechanical, physico-chemical and biological failures, such as encrustation and biofilm formation [5, 6].
An ideal stent would offer simple insertion and removal without discomfort, would not result in migration upon deployment, and would resist biofilm formation or encrustations. A stent with these characteristics would not compromise a patient's quality of life (Figure 1). While a number of changes have taken place regarding the size and the length of a stent, in this mini-review we will outline the engineering developments relating to stent material, design and surface coating (Figure 2).
Figure 1.
Characteristics of an ideal stent.
Figure 2.
Factors affecting stent technology.
MATERIAL AND METHODS
To engineer an ideal ureteric stent, developments are required on three key technology areas: the constitutive material of the stent, its surface properties, and the stent architecture (Figure 2). In the following sections, we will provide an overview of recent innovations in these areas.
Stent material
There are three main classes of materials that are employed to fabricate ureteric stents: metals, polymers and bio-degradable/bio-absorbable materials [7–14] (Table 1). Polymeric stents are more favored due to their biologically inert properties in comparison to metal stents. They typically comprise of thermoplastic, thermoset elastomers and other proprietary materials, which are mostly silicone-based [1, 2, 3]. Bio- degradable/bio-absorbable stents are more recent, and have been shown to reduce the requirement for secondary procedures (i.e. stent removal). The time taken for the stent to be absorbed depends on the material type and potential surface coatings [4]. Dual durometer stents consist of a material that transitions from hard proximally to soft distally, with the purpose of decreasing bladder irritation [5].
Table 1.
Summary of the most commonly used materials for ureteral stents to date
| Innovations in material | Key comments by manufacturer or reported in a scientific publication | Commercial example | |
|---|---|---|---|
| Polymeric | Silicone | Highly biocompatible when compared to other materials [2] | FLUORO-4™ (Bard®, USA) |
| Polyurethane | High drainage performance and High epithelial erosion [2, 10] | Bardex® (Bard®, USA) | |
| Silitek™ | High tensile strength, weak coil retention, high incident rate of edema [11] | (Medical Engineering©, Argentina) | |
| Percuflex™ | Cost effective, efficient urine drainage and coil retention, low coil and tensile strength [1] | (Boston® Scientific, USA) | |
| C-Flex® | Lower surface friction allowing less particle adhesion, lower mechanical strength compared to polyurethane and PureFlex™ [1] | (Cook© Medical, USA) | |
| Dual Durometer | Minimizes bladder irritation [8] | (Bioteq©, Taiwan) | |
| Metal | MP35N alloy, a composite of non- magnetic nickel-cobalt- chromium-molybdenum | Metallic double pigtail stent that possesses a high tensile strength and resistance to corrosion [7] | Resonance® Metallic ureteral stent (Cook Medical, Bloomington, IN, USA) |
| Nickel Titanium (Nitinol) | Soft and strong, not indicated for patients with functional stenosis or stone formation [7] | Memokath 051 ureteral stent (PNN© medical, Denmark) | |
| Stainless steel | Simplicity of fabrication, removal may be complex [5, 7] | Wall stent (Boston® Scientific, USA) | |
| Biodegradable | Reduction of secondary procedures [4, 9] | Uriprene (Poly-Med Inc., USA) | |
Metallic stents were first introduced by Gort et al., and gained popularity due to their resistance against deformation caused by extrinsic/intrinsic strictures [6, 7, 8].
Table 1 summarizes the commonly used materials for ureteral stents, as well as a few commercial examples [1, 2, 4, 6, 8–12].
Stent coating
Coatings are evolutions in ureteric stents that allow a decrease in friction, resulting in easier stent passage over a guidewire [13]. Moreover, they can potentially help reducing formation of biofilms and encrustations [6]. Coatings have also the potential for reducing inflammation caused by the release of ions from metal stents [3]. Specific coatings may also be employed for drug eluting purposes [14].
Notably, reduced surface adhesion and friction from coatings has been associated with increased stent lifetime and has improved the patient's quality of life. Table 2 summarizes the stent coatings that are commonly used or have been researched [15–26].
Table 2.
Summary of the most commonly used coatings for ureteral stents to date
| Innovations in material | Key comments by manufacturer or reported in a scientific publication | Commercial example or method of reported study |
|---|---|---|
| Heparin (a blood thinner) | Prevention of biofilm and encrustation [20] | In-vivo human patient |
| Polyvinylpyrrolidone (PVP) | Provides a non-adhesive surface due to its lubricant properties and water-solubility [14] | In-vitro study |
| Antibiotic | Bacterial uropathogens growth prevention, antimicrobial properties, drug elution [19] | In-vivo study on rat model |
| Carbon (diamond- like) | Decreasing biofilm formation and encrustation [15] | In-vivo study human patient |
| Hyaluronic acid | Prevention of growth and nucleation of salts, decreasing protein surface assimilation [22] | In-vitro study on rat model |
| Triclosan | Uropathogens and bacterial growth prevention, FDA concern on the potential for causing bacterial resistance [18] | In-vivo studies e.g. Triumph™ (Boston® Scientific, USA) |
| Silver | In comparison to ordinary stent, silver-coated stents appear to perform better in preventing biofilm formation; however, prolonged usage of these coatings can potentially cause argyria [23] | In-vitro study ‘plant infection model’ |
| Gendine | Biofilm and ureteric infection prevention [23] | In-vivo study on rabbit |
| Chitosan | Biofilm prevention, especially a derivation with polymethylmethacrylate (PMMA) [16, 25] | In-vitro study |
| Salicylic acid | Salicylic acid release, due to the hydrolysation of the salicyl acrylate polymer coating in aqueous environment, prevents biofilm formation [17, 24] | In-vitro study |
| Hydrogel | High water solubility properties provide a thin layer of water that potentially prevents the creation of conditioning film and biofilm However, there are variable results regarding the level of effectiveness of this coating [21] |
In-vitro (in human urine) study |
Stent design
Stent design, on the other hand, is one of the areas that have experienced many scientific trials and associated modifications globally [10, 27]. While stent design changes have allowed the double-J structure as a default for almost all stents, its main rationale was to avoid migration of these stents once placed successfully.
Similar stent modifications have also happened with regard to the stent drainage, such as side holes along with other novelties such as spiral stents, mesh stents, stents with variations in tail designs and the method of removal of these stents. A future research area relates to the fluidic aspects of stent drainage, which may become more important with in-vitro research data suggesting that it can govern encrustation and biofilm formation [28]. Table 3 summarizes the various designs and provides examples of their representing stents on the market [9–36].
Table 3.
Summary of most commonly used designs for ureteral stents to date
| Innovations in design | Key comments by manufacturer or reported in a scientific publication | Commercial example or method of reported study |
|---|---|---|
| Double-J | Decreasing migration of stent both proximally and distally. This design is employed in most of the ureteral stents currently on the market [28] | In-vivo human patient |
| Double-J 3D | Believed to provide a better proximal and distal retention | Silicon Figure Four (SFF) (Bard®, USA) |
| Loop | Believed to provide a 69% volume reduction in the amount of material inside bladder, and better patient comfort | Polaris™ Loop ureteral stent (Boston® Scientific, USA) |
| Mesh | Less frequency of upper urinary tract inflammation, but more difficult to place compared to standard unmeshed ureteral stents [34] | In-vivo study on pig model |
| Expandable | This design is believed to provide a higher intra-luminal flow, and ease of insertion and retrieval | Allium® Ureteral Stent (Allium Medical Solutions®, Israel) |
| Magnetic- tip | Allowing more effective retrieval due to the presence of magnetic material (stainless steel bead) at the distal end of the stent | Magnetic Black- Star (Urovision, Germany) |
| String | The extraction string is designed to be attached to the stent to facilitate removal [35] | In-vivo human patient study |
| Coil- Reinforced | It allows efficient drainage because of the larger lumen, it reduces kinking and buckling, and has high compressive resistance [36] | Silhouette® stent (Applied Medical, USA) |
| Basket | Its ability to widen laterally upon an activation force improves passageway for small stones and stops bigger stones’ migration through ureter | Ureteral Stone Sweeper® (Fossa® Medical, USA) |
| Spiral Cut | This type includes having the standard solid lumen of the ureteral stent at the distal and proximal region and spiral cut lumen through the rest of the stent. The stent is claimed to result in fewer upper tract symptoms [30] | In-vivo pig model study |
| Linearly Expandable | A design in which the stent has got spiral wire spring sandwiched between inner and outer lining of the stent wall to maintain urine flow in the presence of an obstruction [32] | In-vitro study |
| Helical | Side holes that emerge from the main body of the stent, direct the flow into the lumen thanks to the hole projecting out of the stent lumen and therefore potentially results in potrntially better drainage of the urine and passage of small stones [33] | In-silico study |
| Grooved | Specifically designed for patients treated with lithotripsy, enabling stone fragments to travel efficiently along the ureter [29, 31] | Towers Peripheral Ureteral Stent (Cook® Medical, USA) |
CONCLUSIONS
Stents have evolved over the last century with a wide variety of available materials, coatings and designs. An ideal stent still remains a panacea, but potential solutions would lie in further engineering evolutions in an era of widespread and increasing clinical use of ureteric stents.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Mardis HK, Kroeger RM, Morton JJ, Donovan JM. Comparative evaluation of materials used for internal ureteral stents. J Endourol. 1993;7:105–115. doi: 10.1089/end.1993.7.105. [DOI] [PubMed] [Google Scholar]
- 2.Hofmann R, Hartung R. Ureteral stents - materials and new forms. World J Urol. 1989;7:154–157. [Google Scholar]
- 3.Abrams HL. Abrams' angiography: interventional radiology: Lippincott Williams & Wilkins. 2006. [Google Scholar]
- 4.Barros AA, Oliveira C, Lima E, Duarte ARC, Reis RL. Gelatin-based biodegradable ureteral stents with enhanced mechanical properties. Applied Materials Today. 2016;5:9–18. https://doi.org/10.1016/j.apmt.2016.07.006. [Google Scholar]
- 5.Al-Aown A, Kyriazis I, Kallidonis P, et al. Ureteral stents: new ideas, new designs. Ther Adv Urol. 2010;2:85–92. doi: 10.1177/1756287210370699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Denstedt J, Atala A. Biomaterials and tissue engineering in urology: Elsevier. 2009. [Google Scholar]
- 7.Kulkarni R. Metallic stents in the management of ureteric strictures. Indian J Urol. 2014;30:65–72. doi: 10.4103/0970-1591.124210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beiko DT, Knudsen BE, Denstedt JD. Advances in ureteral stent design. J Endourol. 2003;17:195–199. doi: 10.1089/089277903765444294. [DOI] [PubMed] [Google Scholar]
- 9.Chew BH, Lange D, Paterson RF, et al. Next generation biodegradable ureteral stent in a yucatan pig model. J Urol. 2010;183:765–771. doi: 10.1016/j.juro.2009.09.073. [DOI] [PubMed] [Google Scholar]
- 10.Lamba NM, Woodhouse KA, Cooper SL. Polyurethanes in biomedical applications: CRC press. 1997. [Google Scholar]
- 11.Marx M, Bettmann MA, Bridge S, Brodsky G, Boxt LM, Richie JP. The effects of various indwelling ureteral catheter materials on the normal canine ureter. J Urol. 1988;139:180–185. doi: 10.1016/s0022-5347(17)42349-4. [DOI] [PubMed] [Google Scholar]
- 12.Lange D, Chew BH. Update on ureteral stent technology. Ther Adv Urol. 2009;1:143–148. doi: 10.1177/1756287209341306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ma X, Wu T, Robich MP. Drug-eluting stent coatings. Interv Cardiol. 2012;4:73–83. [Google Scholar]
- 14.Lo J, Lange D, Chew B. Ureteral stents and Foley catheters-associated urinary tract infections: the role of coatings and materials in infection prevention. Antibiotics (Basel). 2014;3:87–97. doi: 10.3390/antibiotics3010087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laube N, Kleinen L, Bradenahl J, Meissner A. Diamond-like carbon coatings on ureteral stents - a new strategy for decreasing the formation of crystalline bacterial biofilms? J Urol. 2007;177:1923–1927. doi: 10.1016/j.juro.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 16.Peng Z-X, Wang L, Du L, Guo S-R, Wang X-Q, Tang T-T. Adjustment of the antibacterial activity and biocompatibility of hydroxypropyltrimethyl ammonium chloride chitosan by varying the degree of substitution of quaternary ammonium. Carbohyd Polym. 2010;81:275–283. [Google Scholar]
- 17.Bryers JD, Jarvis RA, Lebo J, Prudencio A, Kyriakides TR, Uhrich K. Biodegradation of pol y(anhydride-esters) into non-steroidal anti-inflammatory drugs and their effect on Pseudomonas aeruginosa biofilms in vitro and on the foreign-body response in vivo. Biomaterials. 2006;27:5039–5048. doi: 10.1016/j.biomaterials.2006.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wignall GR, Goneau LW, Chew BH, Denstedt JD, Cadieux PA. The effects of triclosan on uropathogen susceptibility to clinically relevant antibiotics. J Endourol. 2008;22:2349–2356. doi: 10.1089/end.2008.9705. [DOI] [PubMed] [Google Scholar]
- 19.Minardi D, Cirioni O, Ghiselli R, et al. Efficacy of tigecycline and rifampin alone and in combination against enterococcus faecalis biofilm infection in a rat model of ureteral stent. J Surg Res. 2012;176:1–6. doi: 10.1016/j.jss.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 20.Cauda F, Cauda V, Fiori C, Onida B, Garrone E. Heparin coating on ureteral Double J stents prevents encrustations: an in vivo case study. J Endourol. 2008;22:465–472. doi: 10.1089/end.2007.0218. [DOI] [PubMed] [Google Scholar]
- 21.Desgrandchamps F, Moulinier F, Daudon M, Teillac P, LeDuc A. An in vitro comparison of urease- induced encrustation of JJ stents in human urine. Br J Urol. 1997;79:24–27. doi: 10.1046/j.1464-410x.1997.02775.x. [DOI] [PubMed] [Google Scholar]
- 22.Choong SKS, Wood S, Whitfield HN. A model to quantify encrustation on ureteric stents, urethral catheters and polymers intended for urological use. BJU Int. 2000;86:414–421. doi: 10.1046/j.1464-410x.2000.00861.x. [DOI] [PubMed] [Google Scholar]
- 23.Dave RN, Joshi HM, Venugopalan VP. Novel biocatalytic polymer-based antimicrobial coatings as potential ureteral biomaterial: preparation and in vitro performance evaluation. Antimicrob Agents Chemother. 2011;55:845–853. doi: 10.1128/AAC.00477-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nowatzki PJ, Koepsel RR, Stoodley P, et al. Salicylic acid-releasing polyurethane acrylate polymers as anti-biofilm urological catheter coatings. Acta Biomater. 2012;8:1869–1880. doi: 10.1016/j.actbio.2012.01.032. [DOI] [PubMed] [Google Scholar]
- 25.Tan H, Peng Z, Li Q, Xu X, Guo S, Tang T. The use of quaternised chitosan-loaded PMMA to inhibit biofilm formation and downregulate the virulence-associated gene expression of antibiotic-resistant staphylococcus. Biomaterials. 2012;33:365–377. doi: 10.1016/j.biomaterials.2011.09.084. [DOI] [PubMed] [Google Scholar]
- 26.Rao NP, Preminger GM, Kavanagh JP. Urinary tract stone disease: Springer Science & Business Media. 2011. [Google Scholar]
- 27.Clavica F, Zhao XF, ElMahdy M, Drake MJ, Zhang XL, Carugo D. Investigating the flow dynamics in the obstructed and stented ureter by means of a biomimetic artificial model. Plos One. 2014;9:e87433. doi: 10.1371/journal.pone.0087433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Finney RP. Experience with new double j ureteral catheter stent. J Urol. 1978;120:678–681. doi: 10.1016/s0022-5347(17)57326-7. [DOI] [PubMed] [Google Scholar]
- 29.Finney RP. Google Patents. 1981. Externally grooved ureteral stent. [Google Scholar]
- 30.Mucksavage P, Pick D, Haydel D, et al. An in vivo evaluation of a novel spiral cut flexible ureteral stent. Urology. 2012;79:733–737. doi: 10.1016/j.urology.2011.10.062. [DOI] [PubMed] [Google Scholar]
- 31.Skolnick ML. Real-time Ultrasound Imaging in the Abdomen. New York, NY: Springer New York; 1981. Intra- and Extraluminal Fluid; pp. 191–212. [Google Scholar]
- 32.Gellman BN. Google Patents. 2010. Linearly Expandable Ureteral Stent. [Google Scholar]
- 33.Tong JCK, Sparrow EM, Abraham JP. Numerical simulation of the urine flow in a stented ureter. J Biomech Eng. 2007;129:187–192. doi: 10.1115/1.2472381. [DOI] [PubMed] [Google Scholar]
- 34.Chew BH, Lange D. Ureteral stent symptoms and associated infections: a biomaterials perspective. Nat Rev Urol. 2009;6:440–448. doi: 10.1038/nrurol.2009.124. [DOI] [PubMed] [Google Scholar]
- 35.Oliver R, Wells H, Traxer O, et al. Ureteric stents on extraction strings: a systematic review of literature. Urolithiasis. 2016 Jun 20; doi: 10.1007/s00240-016-0898-1. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pedro RN, Hendlin K, Kriedberg C, Monga M. Wire-based ureteral stents: impact on tensile strength and compression. Urology. 2007;70:1057–1059. doi: 10.1016/j.urology.2007.08.007. [DOI] [PubMed] [Google Scholar]