Abstract
Objective
We examined data from a prospective study of risk factors that increase vulnerability or resilience, exacerbate distress, or foster recovery to determine whether risk factors accurately predict which individuals will later have high posttraumatic (PT) symptom levels and whether brief measures of risk factors also accurately predict later symptom elevations.
Method
Using data from 129 adults exposed to traumatic injury of self or a loved one, we conducted receiver operating characteristic (ROC) analyses of 14 risk factors assessed by full-length measures, determined optimal cutoff scores and calculated predictive performance for the nine that were most predictive. For five risk factors, we identified sets of items that accounted for 90% of variance in total scores and calculated predictive performance for sets of brief risk measures.
Results
A set of nine risk factors assessed by full measures identified 89% of those who later had elevated PT symptoms (sensitivity) and 78% of those who did not (specificity). A set of four brief risk factor measures assessed soon after injury identified 86% of those who later had elevated PT symptoms and 72% of those who did not.
Conclusions
Use of sets of brief risk factor measures shows promise of accurate prediction of PT psychological disorder and probable PTSD or depression. Replication of predictive accuracy is needed in a new and larger sample.
1. Introduction
Each year, as many as one million Americans may develop posttraumatic stress disorder (PTSD) or depression after sudden illness or injury. According to the most recent available national hospital survey data from 2011, there were over 5 million hospitalizations for sudden illnesses and injuries requiring very urgent treatment (< 15 minutes) [1]. In one large-scale study that assessed hospitalized trauma patients 12 months after the injury, over 20% were found to have PTSD and/or depression [2]. PTSD can be debilitating for individuals [2, 3] and place a burden on families and society due to impaired occupational and daily functioning [2, 4–6], lost productivity, chronic medical problems [7, 8], disability [3, 9, 10], and increases in suicidality [11], violence [12], and criminal behavior [13]. Predictive screening after traumatic illness or injury for risk of later PTSD or depression could facilitate early intervention to prevent or reduce the severity of disorder, but accurate prediction has proved elusive.
Currently, hospitals in the U.S. do not routinely screen patients treated in trauma or emergency departments to identify those at risk for later PTSD or other mental health (MH) problems, although early screening for PTSD and depression following injury has been recommended by the American College of Surgeons’ Committee on Trauma [14]. In addition, the American Red Cross has begun collecting data on a set of pre-trauma and time-of-trauma risk factors in populations exposed to disasters, but the predictive performance of the triage tool used has not been studied. [15] Screening to detect current symptoms (as opposed to predicting future PTSD symptoms), is not as helpful, because early responses to trauma do not predict who will develop MH problems to a degree of accuracy that is clinically useful [16]. Most people exposed to traumatic events do have some symptoms in the days following the event and recover fairly quickly, but some do not. And some of those who are initially asymptomatic develop MH problems over time [17]. Dozens of studies have measured risk factors for PTSD [18, 19], but, typically, the risk factors are not assessed prospectively and do not capture enough variance in PTSD to make accurate predictions about individuals.
A recent review examined seven PTSD predictive screening tools and noted that for all but one, analyses to select items and analyses to test “performance” were conducted on the same data [20]. Selecting items that are highly related to the outcome yields a set of items that has the strongest possible relation to the outcome in the sample studied, but that set may not be as strongly related to the outcome in a new sample. A few other risk screening tools have been published, but they cannot be used for early predictive screening because they include variables that are typically not available until weeks or months after the event [21–25]. None of these screening tools have been given within days of an event and accurately differentiated between those who developed disorder and those who did not [21–25]. Screening tools have also been developed to identify those who currently have PTSD, but those are not designed to prospectively predict PTSD at a future time point [26, 27].
The only predictive screening tool that has had its performance examined in different data than was used to develop it is the Posttraumatic Adjustment Scale (PAS), which was developed and tested in Australia [28]. Performance of the PAS in a U.S. sample has not been reported, and differences between the populations seem likely to affect the screening tool’s accuracy for predicting PTSD in the U.S. In the Australian patients, the relative importance of risk factors to predict PTSD was different than observed in U.S. patients [28, 29]. In the Australian data, 52% of the variance in PTSD was accounted for by 5 factors: 1. acute stress symptoms, 2. prior social support, 3. pre-injury emotional and trauma history, 4. expectations about ability to cope with post-trauma life stress, and 5. trauma appraisals and post-trauma pain [28]. In contrast, in a U.S. sample that we have reported on previously, the risk factors that were most strongly related to PTSD were post-trauma life stress and negative thinking [29]. It is possible that universal coverage of medical care costs in Australia and the availability of financial support to Australians disabled by injuries explain some of these differences.
Two studies have examined the capacity of data mining methods or machine learning to predict long-term PTSD symptom levels. A large study of World Health Organization survey data from 24 countries (N = 126,096) used data mining methods to categorize the PTSD risk level of trauma exposures in a subsample of individuals who reported exposure to one or more traumas (N = 42,634). Exposure events were categorized into PTSD risk levels based on retrospective data on trauma exposure type, socio-demographics, and reported prior history of trauma exposure and mental disorder. While the study models performed well in classifying traumatic events that were associated with the vast majority of cases of PTSD, performance to predict PTSD in individuals was not reported [30]. Two reports on analyses of data from a study of Israeli patients analyzed the capacity of algorithms based on a wide range of predictors assessed by telephone 6 to 14 days post-trauma to predict a non-remitting PTSD symptom trajectory over 15 months. The algorithms provided fair overall predictive accuracy (AUC = .75) but did not allow accurate prediction for individuals [31, 32]. While these data mining studies show promise for predicting long-term PTSD symptoms, none demonstrated the capacity to predict short-term symptom elevation at the level of the individual, which could permit preventive intervention. Use of data from electronic medical records (EMRs) to screen for risk would also require overcoming major obstacles to implementation in the U.S., including lack of EMR systems in many settings and the high degree of effort and cost involved in introducing new elements into existing EMR systems.
To accurately predict mental health problems at the level of the individual after exposure to traumatic events, it is necessary to assess variables that account for a great deal of variance in outcomes. In a longitudinal study of risk and resilience to traumatic events, we studied fourteen variables that are hypothesized to increase vulnerability or resilience to traumatic stress or to impede or foster recovery. A model including these 14 risk factors accounted for 72% of the variance in posttraumatic (PT) symptoms (including symptoms of PTSD, depression, negative thinking, and dissociation) two months after trauma [29]. We studied these four categories of symptoms, because they are consistent with the DSM-5 diagnostic criteria for PTSD, allow dimensional measurement of symptoms, and are all strongly associated with exposure to traumatic stress [33–36].
The purpose of the current study was to determine whether the risk factors we assessed could accurately identify those who would later have high levels of PT symptoms and those who would not. Given the impracticality and high burden to patients of screening using full-length measures, we also investigated the performance of sets of briefer risk factor measures. We first conducted analyses to examine whether some of the risk factors we studied could be accurately assessed using fewer items and whether a smaller number of risk factors assessed by fewer items could accurately identify individuals who would later have high PT symptoms and those who would not. We also calculated the performance of risk factors that were measured soon after the traumatic injury. Analyses to determine the performance of Acute Stress Disorder symptoms to predict PT symptoms was also conducted to provide information about the relative performance of early symptoms alone to predict later symptoms. Since prior research has shown that prevalence of PTSD is elevated in some racial/ethnic minority groups [37, 38], it is important that any risk screening tool accurately predicts risk for these groups. Accordingly, we conducted a separate analysis of the performance of risk factors to accurately predict PT symptoms in the subset of participants who self-identified as members of racial or ethnic minority groups. Lastly, in order to provide information about performance of brief risk factors to predict whether participants would meet familiar diagnostic criteria, we also conducted a subset of the analyses to predict the outcome of probable diagnosis of PTSD or depression.
2. Materials and methods
2.1 Setting and participants
Participants were 147 trauma-exposed adults who were recruited to participate in a study of factors that influence responses to traumatic stress [29] and a study of an intensive ambulatory data collection method [39]. Participants had been treated in a Level I trauma center and hospitalized for a severe injury (54%) or had loved ones treated and hospitalized for life-threatening injuries (46%). Patients’ injuries were due to motor vehicle crashes, including motorcycle crashes, biking accidents, and pedestrians hit by cars (36%); accidental injuries at home or work (15%); and physical assault (3%). Women comprised 58% of the sample and 31% reported minority racial/ethnic identities, including 15% who self-identified as Hispanic, 8% who self-identified as Asian or Pacific Islander, 7% who reported two or more racial/ethnic identities, and 4% who self-identified as African-American. In this sample, 24% of the injured patients and 22% of the family members appeared to meet DSM-IV diagnostic criteria for PTSD two months post-trauma.
2.2 Measures
Detailed descriptions of the measures are provided in an earlier report [29] and in the online Supplementary File for this article. The risk factor variables assessed, measures used, and the number of items in each measure are listed in Table 1. Childhood home life was assessed with a single item inquiring “How was your home life growing up?” (very happy, pleasant, OK, mixed, unhappy) Pre-trauma home life was assessed with a single item inquiring “How is your home life now?” (very happy, pleasant, OK, mixed, unhappy). Trauma Severity was the sum of ratings of how “terrible” and “out of control” the event seemed (not at all, a little, some, much, very much). To assess mental health two months after the injury, we used measures of PTSD symptoms (Screen for Posttraumatic Stress Symptoms [40]), depression (short form of the Beck Depression Inventory – Short Form [BDI-SF] [41]), and dissociation (Dissociative Symptoms Scale [42]). Given that negative thoughts about self, others, and the world are now included in the DSM-5 diagnostic criteria for PTSD [43], we also assessed negative thinking two months post-trauma with 18 items from the Posttraumatic Cognitions Inventory (PTCI) [44].
Table 1.
Fourteen Risk Factors and Measures to Assess Them
| Variable | Measure | Number of Items |
Area Under Curve for Full Measure |
|---|---|---|---|
|
| |||
| Childhood Home Life | Childhood Home Life | 1 | .72 |
|
| |||
| Past Traumatic Events | Trauma History Screen [34] | 16 | .73 |
|
| |||
| Age at First Trauma | Age at First Trauma | 1 | .75 |
|
| |||
| Prior Psychopathology | Millon Clinical Multiaxial Inventory III [51] | 175 | .79 |
|
| |||
| Acute Stress Symptoms | Screen for Posttraumatic Stress Scale [40] | 17 | .82 |
| Dissociative Symptoms Scale [42] | 20 | ||
|
| |||
| Negative Thoughts | Posttraumatic Cognitions Inventory [44] | 18 | .95 |
|
| |||
| Post-trauma Life Stress | Perceived Stress Scale [52] | 10 | .89 |
|
| |||
| Early Social Support | Social Support Survey [53] | 19 | .71 |
|
| |||
| Early Social Constraints | Social Constraints Scale [54] | 15 | .72 |
|
| |||
| Pre-trauma Home Life | Pre-trauma Home Life Question | 1 | .69 |
|
| |||
| Past High Magnitude Stressors | Trauma History Screen [34] | 16 | .68 |
|
| |||
| Trauma Severity | Trauma Severity Score | 2 | .66 |
|
| |||
| Parental Dysfunction | Parental Dysfunction Score | 4 | .63 |
|
| |||
| Years of Education | Years of Education | 1 | .59 |
As in our prior publication [29], the primary outcome in this study was an index of posttraumatic psychological disorder derived from scores on measures of symptoms of PTSD (SPTSS), depression (BDI-SF), negative thinking (PTCI), and dissociation (DSS) collected two months post-trauma. This index was thought to best represent the DSM-5 diagnostic criteria for PTSD and allow dimensional measurement of symptoms. Scores on the measures of PTSD, depression, negative thinking, and dissociation were highly correlated (r = .69 to r = .83), and principal components analysis of these four symptom categories identified one posttraumatic symptoms factor (PT symptoms) that accounted for 82% of variance in scores [29]. The primary outcome for analysis was the PT symptoms factor score.
In order to conduct analyses of the performance of risk factors to predict probable to diagnoses, SPTSS scores and BDI-SF scores were used to categorize participants as having probable PTSD and/or probable depression when assessed two months after the traumatic injury. SPTSS scores of 20 or higher were used to categorize subjects as positive for PTSD based on strong concurrent validity with the diagnosis of PTSD from structured interviews [40, 45] and on analysis of data from a subsample of 40 participants in the current study who were administered the Clinician-Administered PTSD Scale (CAPS) [46]. BDI-SF scores of 10 or higher were used to categorize subjects as positive for depression based on a study of hospitalized medical patients showing high sensitivity (1.0) and high specificity (.83) of scores of 10 or higher in predicting a diagnosis of depression determined by a structured interview. [47]
2.3 Procedures
Admitted patients were identified via hospital electronic records and approached in their hospital rooms between one and fourteen days after injury. Family members were approached in the patient’s room or in waiting areas. For each traumatic injury event, only a single patient or family member was enrolled. After obtaining informed consent, participants completed all measures listed in Table 1 with the following exceptions. The measures of social support and social constraints were completed one week after enrollment and again two months after the traumatic injury. Only data from the first administration are included in the analyses reported here. Two months post-trauma, participants completed the measures of post-trauma life stress, PTSD symptoms, depression, dissociation, and negative thinking for a second time.
2.3 Data analysis methods
The measures of social support, social constraints, and post-trauma life stress were added to the study mid-way through, which resulted in missing data for social support and social constraints from 53% of participants and missing data for post-trauma life stress for 45% of participants. Data were also missing for 13% of participants for psychopathology, 11% for acute stress, and 2 to 5% for all other variables. Consideration of the reasons for most of the missing data (measures not included in the study at that time) and analysis of patterns of missingness led us to consider the data to be missing Completely at Random. Multiple imputation was conducted to generate five complete datasets. Predictive analyses were conducted on pooled statistical values from the five imputed datasets in the subsample of 129 for whom follow-up assessments were available.
Receiver Operating Characteristic (ROC) analyses were conducted on the 14 risk factors shown in Table 1 to select the most predictive risk factors to include in further analyses. The value for classifying PT symptoms status as elevated was the PT symptom factor score value associated with a score of 45 or higher on the CAPS [46, 48], which was administered to a subset of 40 participants. Selection of risk factors to include in further analyses was based on Area Under the Curve (AUC) values of .70 or higher to predict PT symptom status. ROC analyses for the full measures were also used to determine optimal cut points to classify participants as positive on each risk factor.
To create brief risk measures for Negative Thoughts, Post-trauma Life Stress, Post-trauma Social Support, Post-trauma Social Constraints, and Acute Stress Symptoms, forward regression analyses were conducted on all available data for risk factors (N = 147) to identify items that accounted for 90% of the variance in total measure scores. ROC analyses were used to determine cut-points for presence of each risk. Brief risk factors were not created for Past Traumatic Events, Age at First Traumatic Event, and Psychopathology, because measurement of these risk factors requires a large number of items. There was no need to create a brief measure of Childhood Home Life, because only one item was used to assess this risk factor.
3. Results
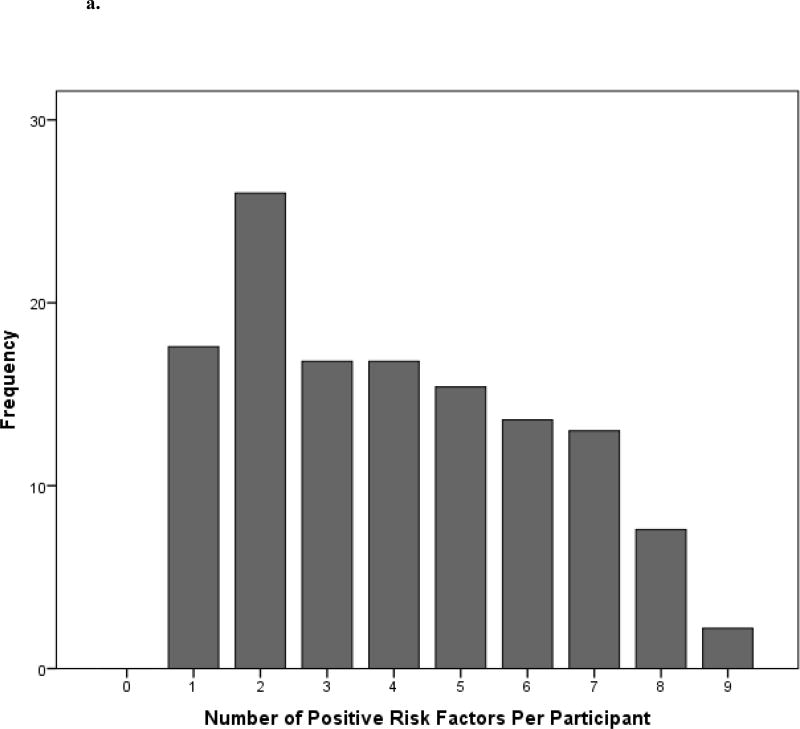
Of 147 enrolled participants for whom baseline data were available, 129 (88%) completed follow-up assessments. Table 1 shows all 14 risk factors and their AUC values. Nine risk factors met our criterion of an AUC of .70 or higher to predict PT symptom status and were included in further analyses. Figure 1a shows the per participant number of positive risks of the nine risk factors assessed by full measures. The mean number of positive risk factors per participant was 4.0 (median = 4). Table 2 shows the performance of a risk count of 5 or more risks assessed by full measures to classify elevation in PT symptoms assessed two months post-trauma. Also shown in Table 2 is the performance of Acute Stress Disorder symptoms (assessed using full measures of PTSD and dissociation) to predict later PT elevation status.
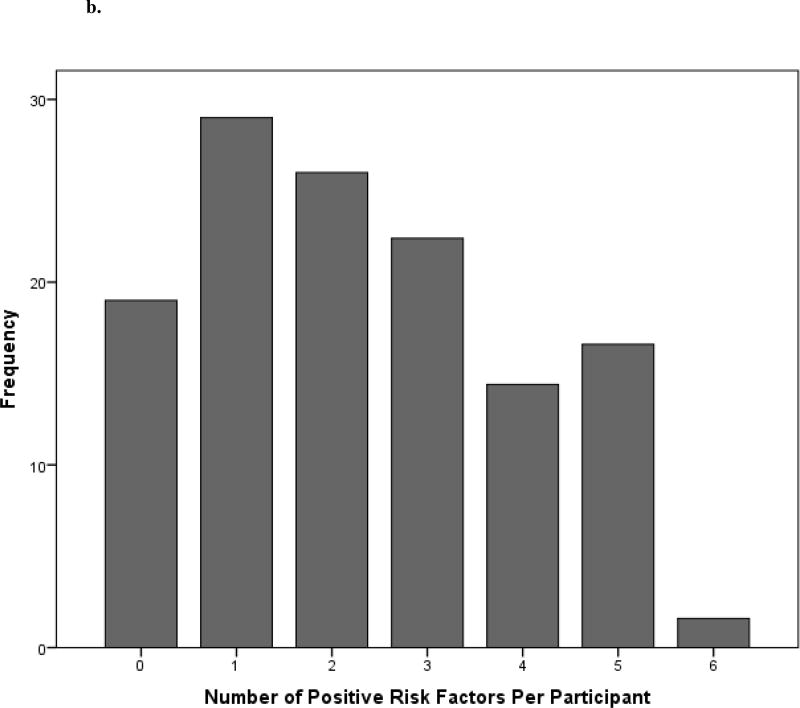
Figure 1.
a. Frequency distribution of positive risk factors per participant assessed by nine full risk factor measures.
b. Frequency distribution of positive risk factors per participant assessed by six brief risk factor measures.
Table 2.
Classification Performance of Full Risk Factor Measures
| Risks Assessed (Cut point for Positive Classification) | Positive Classification Rule |
AUC | % Correctly classified |
SE | SP |
|---|---|---|---|---|---|
|
| |||||
| Childhood Home Life (score of 2 or higher) | 5 or more risks | .92 | 81% | .89 | .78 |
| Past Traumatic Events (3 or more) | |||||
| Age at First Trauma (21 or older) | |||||
| Prior Psychopathology (score of −.40 or higher) | |||||
| Acute Stress Symptoms (score of 23 or higher) | |||||
| Negative Thoughts (score of 13 or higher) | |||||
| Post-trauma Life Stress (score of 20 or higher) | |||||
| Post-Trauma Social Support (score of 3.65 or higher) | |||||
| Post-Trauma Social Constraints (score of 28 or higher) | |||||
|
| |||||
| Acute Stress (score of 23 or higher) | Score of 23 or higher | .81 | 70% | .79 | .67 |
Note: SE = sensitivity, SP = specificity
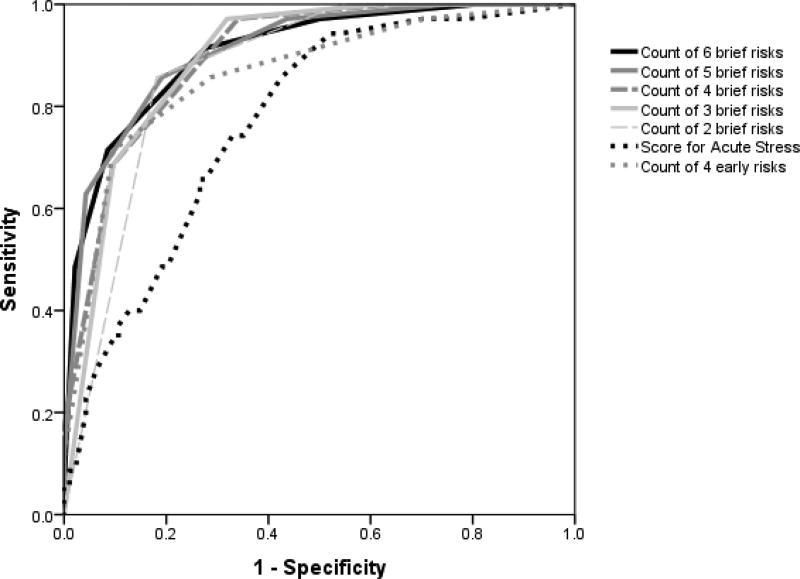
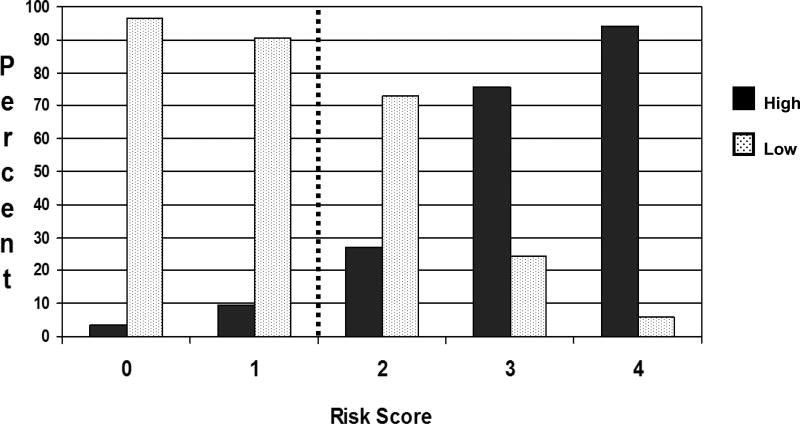
Correlations between brief and full risk measures ranged from .91 to .97. Figure 1b shows the per participant number of “positive” risk factors assessed by six brief measures. The mean number positive per participant was 2.3 (median = 2). Table 3 shows the performance of six, five, four, three, and two risk factors to correctly classify participants for PT elevation. Also shown in Table 3 is the performance of four variables that were assessed prospectively soon after the event and the performance of Acute Stress Disorder symptoms to predict PT elevation at two months post-trauma. Lastly, Table 3 shows the performance of the four risk factors assessed soon after trauma to predict later PT elevation in the 37 participants who self-identified as members of one or more racial or ethnic minority group. Figure 2 shows the ROC curves for analyses presented in Table 3. Figure 3 shows the percent of participants who later had high and low PTPD by risk score with a cutoff of 2 or more risks marked.
Table 3.
Classification Performance of Brief Risk Factor Measure Sets to Predict PT Symptoms
| Risks Assessed (items per risk) | Number of Items |
Positive Classification Rule |
AUC | % Correctly classified |
SE | SP |
|---|---|---|---|---|---|---|
|
| ||||||
| Negative Thoughts (6) | 21 | 3 or more risks | .90 | 80% | .91 | .75 |
| Post-trauma Life Stress (2) | ||||||
| Post-Trauma Social Constraints (3) | ||||||
| Post-Trauma Social Support (3) | ||||||
| Acute Stress Symptoms (6) | ||||||
| Childhood Home Life (1) | ||||||
|
| ||||||
| Negative Thoughts | 20 | 3 or more risks | .91 | 84% | .85 | .83 |
| Post-trauma Life Stress | ||||||
| Post-Trauma Social Constraints | ||||||
| Post-Trauma Social Support | ||||||
| Acute Stress Symptoms | ||||||
|
| ||||||
| Negative Thoughts | 14 | 2 or more risks | .90 | 76% | .97 | .68 |
| Post-trauma Life Stress | ||||||
| Post-Trauma Social Constraints | ||||||
| Post-Trauma Social Support | ||||||
|
| ||||||
| Negative Thoughts | 11 | 2 or more risks | .89 | 77% | .97 | .70 |
| Post-trauma Life Stress | ||||||
| Post-Trauma Social Constraints | ||||||
|
| ||||||
| Negative Thoughts | 8 | one risk | .87 | 82% | .88 | .80 |
| Post-trauma Life Stress | ||||||
|
| ||||||
| Acute Stress (PTSD and dissociation items that account for 90% of variance in total Acute Stress score) | 6 | 5 or more risks | .78 | 70% | .72 | .69 |
|
| ||||||
| Four Prospective Risks: | 18 | 2 or more risks | .91 | 76% | .86 | .72 |
| Negative Thoughts | ||||||
| Post-Trauma Social Constraints | ||||||
| Post-Trauma Social Support | ||||||
| Acute Stress Symptoms | ||||||
|
| ||||||
| Four Prospective Risks for Racial/Ethnic Minority Subjects: | 18 | 2 or more risks | .82 | 78% | .78 | .78 |
| Negative Thoughts | ||||||
| Post-Trauma Social Constraints | ||||||
| Post-Trauma Social Support | ||||||
| Acute Stress Symptoms | ||||||
Note: Brief risk measures contain the same specific items for all analyses reported.
Figure 2.
Receiver Operating Characteristic Curves for Brief Risk Measure Sets
Figure 3.
Percent of Participants with Elevated PTPD by Risk Score for Four Prospectively Assessed Risk Factors
Table 4 shows results of analyses to examine performance of risk factors to predict probable diagnoses of PTSD and/or depression.
Table 4.
Classification Performance of Brief Risk Factor Measure Sets to Predict Probable PTSD or Depression
| Risks Assessed (items per risk) | Number of Items |
Positive Classification Rule |
AUC | % Correctly classified |
SE | SP |
|---|---|---|---|---|---|---|
|
| ||||||
| Negative Thoughts (6) | 21 | 3 or more risks | .89 | 80% | .90 | .77 |
| Post-trauma Life Stress (2) | ||||||
| Post-Trauma Social Constraints (3) | ||||||
| Post-Trauma Social Support (3) | ||||||
| Acute Stress Symptoms (6) | ||||||
| Childhood Home Life (1) | ||||||
|
| ||||||
| Four Measures Collected Early: | 18 | 2 or more risks | .86 | 76% | .85 | .73 |
| Negative Thoughts | ||||||
| Post-Trauma Social Constraints | ||||||
| Post-Trauma Social Support | ||||||
| Acute Stress Symptoms | ||||||
|
| ||||||
| Four Measures Collected Early for Racial/Ethnic Minority Subjects: | 18 | 2 or more risks | .80 | 75% | .76 | .75 |
| Negative Thoughts | ||||||
| Post-Trauma Social Constraints | ||||||
| Post-Trauma Social Support | ||||||
| Acute Stress Symptoms | ||||||
Note: Brief risk measures contain the same specific items for all analyses reported.
Discussion
The analyses conducted indicate that the set of risk factors we studied shows promise of accurate prediction of elevation in post-traumatic symptoms at the level of the individual. Accurate prediction was also possible with small sets of brief measures and for individuals who self-identify as ethnic minorities. Sets of full and brief risk factor measures yielded higher sensitivities and specificities than acute stress symptoms alone.
The findings of sensitivities to predict PT symptom elevation and probable PTSD and/or depression ranging from .85 to .97 and specificities ranging from .68 and .83 indicate strong predictive performances for risk factor counts that compare favorably to the performance of the PAS to predict PTSD (SE = .82, SP = .84) and a major depressive episode (SE = .72, SP = .75) in an Australian sample [28]. The two studies assessed many of the same risk factors, but the only variable included in our sets of brief risk factor measures and the PAS was acute stress symptoms. This may be the result of different methods for selecting the most predictive risks. PAS items were selected based on results of exploratory and confirmatory factor analysis of a large pool of items that measured the risk factors. The PAS excluded items loading onto multiple risk factors and included two items to measure each of five risk factors. In contrast, we selected risk factors based on our theoretical model, then sought to reduce the number of items required to assess each risk factor, and used two to six items to measure most risk factors.
Strengths of this study include the theoretical basis for selection of risk factors, the prospective measurement of most risk factors, and selection of items based on total measure scores rather than relationships to the outcome to be predicted. An important limitation to the study was that one highly predictive risk factor (post-trauma life stress) was measured retrospectively at the same time as the outcome. While expected life stress could be measured soon after trauma, that variable may not be as highly predictive as the variable measured retrospectively. It is important to note, however, that the predictive performance was also strong of a set of four brief measures that were all collected soon after the trauma (SE = .86; SP = .72).
Additional limitations were that some risk factors were measured with as few as one item, and some variables that are thought to increase resilient responses to traumatic stress, such as emotion regulation capacity [49] and attachment security [50], were not included in the study. Further research is needed to replicate (i.e., cross-validate) these results in a larger sample and to validate the screening tool in a variety of racial and ethnic minority groups. Such a study should include only risks that can be measured soon after a traumatic event and should include diagnostic interviews of PTSD and depression to assess outcomes. An accurate and cross-validated predictive screening tool would be a valuable addition to available clinical tools to care for those exposed to traumatic events.
Supplementary Material
Acknowledgments
Support for this research was provided by a grant from the National Institute of Mental Health to Eve Carlson (R21MH69876). The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ambulatory and Hospital Care Statistics Branch. National Hospital Ambulatory Medical Care Survey. Washington, DC: National Center for Health Statistics; 2011. [Google Scholar]
- 2.Zatzick DF, Jurkovich GJ, Rivara F, Wang J, Fan M-Y, Joesch J, et al. A national U.S. study of posttraumatic stress disorder, depression, and work and functional outcomes after hospitalization for traumatic injury. Annals of Surgery. 2008;248:429–437. doi: 10.1097/SLA.0b013e318185a6b8. [DOI] [PubMed] [Google Scholar]
- 3.O'Donnell ML, Varker T, Holmes AC, Ellen S, Wade D, Creamer M, et al. Disability after injury: The cumulative burden of physical and mental health. J Clin Psychiatry. 2013;74:e137–e143. doi: 10.4088/JCP.12m08011. [DOI] [PubMed] [Google Scholar]
- 4.Smith M, Schnurr P, Rosenheck R. Employment outcomes and ptsd symptom severity. Ment Health Serv Res. 2005;7:89–101. doi: 10.1007/s11020-005-3780-2. [DOI] [PubMed] [Google Scholar]
- 5.Westphal M, Olfson M, Gameroff MJ, Wickramaratne P, Pilowsky DJ, Neugebauer R, et al. Functional impairment in adults with past posttraumatic stress disorder: Findings from primary care. Depression and Anxiety. 2011;28:686–695. doi: 10.1002/da.20842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Druss BG, Hwang I, Petukhova M, Sampson NA, Wang PS, Kessler RC. Impairment in role functioning in mental and chronic medical disorders in the United States: results from the National Comorbidity Survey Replication. Molecular Psychiatry. 2009;14:728–737. doi: 10.1038/mp.2008.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott KM, Koenen KC, Aguilar-Gaxiola S, Alonso J, Angermeyer MC, Benjet C, et al. Associations between lifetime traumatic events and subsequent chronic physical conditions: A cross-national, cross-sectional study. PLoS ONE. 2013;8:e80573. doi: 10.1371/journal.pone.0080573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sledjeski EM, Speisman B, Dierker LC. Does number of lifetime traumas explain the relationship between PTSD and chronic medical conditions? Answers from the National Comorbidity Survey-Replication (NCS-R) Journal of Behavioral Medicine. 2008;31:341–349. doi: 10.1007/s10865-008-9158-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sareen J, Cox BJ, Stein MB, Afifi TO, Fleet C, Asmundson GJG. Physical and Mental Comorbidity, Disability, and Suicidal Behavior Associated With Posttraumatic Stress Disorder in a Large Community Sample. Psychosomatic Medicine. 2007;69:242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- 10.Bryant RA, O'Donnell ML, Creamer M, McFarlane AC, Clark CR, Silove D. The psychiatric sequelae of traumatic injury. American Journal of Psychiatry. 2010;167:312–320. doi: 10.1176/appi.ajp.2009.09050617. [DOI] [PubMed] [Google Scholar]
- 11.Tarrier N, Gregg L. Suicide risk in civilian PTSD patients: predictors of suicidal ideation, planning and attempts. Social Psychiatry and Psychiatric Epidemiology. 2004;39:655–661. doi: 10.1007/s00127-004-0799-4. [DOI] [PubMed] [Google Scholar]
- 12.Elbogen EB, Johnson SC, Wagner HR, Sullivan C, Taft CT, Beckham JC. Violent behaviour and post-traumatic stress disorder in US Iraq and Afghanistan veterans. The British Journal of Psychiatry. 2014;204:368–375. doi: 10.1192/bjp.bp.113.134627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eitle D, Turner RJ. Traumatic victimization, and other stressful life events exposure to community violence and young adult crime: The effects of witnessing violence. Journal of Research in Crime and Delinquency. 2002;39:214–237. [Google Scholar]
- 14.American College of Surgeons Committee on Trauma. Resources for optimal care of the injured patient 2014. American College of Surgeons; 2014. [Google Scholar]
- 15.Schreiber MD, Yin R, Omaish M, Broderick JE. Snapshot from Superstorm Sandy: American Red Cross mental health risk surveillance in lower New York state. Annals of Emergency Medicine. 2014;64 doi: 10.1016/j.annemergmed.2013.11.009. [DOI] [PubMed] [Google Scholar]
- 16.Bryant RA. Acute stress disorder as a predictor of posttraumatic stress disorder: A systematic review. J Clin Psychiatry. 2011;72:233–239. doi: 10.4088/JCP.09r05072blu. [DOI] [PubMed] [Google Scholar]
- 17.Cardeña E, Carlson E. Acute stress disorder revisited. Annual Review of Clinical Psychology. 2011:245–267. doi: 10.1146/annurev-clinpsy-032210-104502. [DOI] [PubMed] [Google Scholar]
- 18.Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748–66. doi: 10.1037//0022-006x.68.5.748. [DOI] [PubMed] [Google Scholar]
- 19.Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- 20.Becker-Nehring K, Becker A-K, Bengel J. Screeningfragebögen zu Risiko- und Schutzfaktoren für Traumafolgestörungen – Ein systematischer Review (Screening questionnaires for protective and risk factors following traumatic events - a systematic review) Zeitschrift für Psychiatrie, Psychologie und Psychotherapie. 2014;62:153–163. [Google Scholar]
- 21.Mason S, Farrow TF, Fawbert D, Smith R, Bath PA, Hunter M, et al. The development of a clinically useful tool for predicting the development of psychological disorder following injury. Br J Clin Psychol. 2009;48:31–45. doi: 10.1348/014466508X344799. [DOI] [PubMed] [Google Scholar]
- 22.Russo J, Katon W, Zatzick D. The development of a population-based automated screening procedure for PTSD in acutely injured hospitalized trauma survivors. General Hospital Psychiatry. 2013;35:485–491. doi: 10.1016/j.genhosppsych.2013.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boscarino JA, Kirchner HL, Hoffman SN, Sartorious MS, Adams RE, Figley CR. A brief screening tool for assessing psychological trauma in clinical practice: Development and validation of the New York PTSD Risk Score. General Hospital Psychiatry. 2011;33:489–500. doi: 10.1016/j.genhosppsych.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boscarino JA, Kirchner HL, Hoffman SN, Sartorious MS, Adams RE, Figley CR. Predicting future PTSD using a Modified New York PTSD Risk Score: Implications for patient screening and management. General Hospital Psychiatry. 2012;33:489–500. [Google Scholar]
- 25.Mouthann J, Sijbrandij M, Reitsma JB, Gersons BP, Olff M. Comparing screening instruments to predict posttraumatic stress disorder. PLOS One. 2014 doi: 10.1371/journal.pone.0097183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brewin CR, Fuchkan N, Huntley Z, Scragg P. Diagnostic accuracy of the trauma screening questionnaire after the 2005 London bombings. Journal of Traumatic Stress. 2010;23:393–398. doi: 10.1002/jts.20529. [DOI] [PubMed] [Google Scholar]
- 27.Kok T, de Haan HA, van der velden HJW, van der Meer M, Najavits LM, de Jong CAJ. Validation of two screening instruments for PTSD in Dutch substance use disorder inpatients. Addictive Behaviors. 2013;38:1726–1731. doi: 10.1016/j.addbeh.2012.10.011. [DOI] [PubMed] [Google Scholar]
- 28.O'Donnell ML, Creamer MC, Parslow R, Elliott P, Holmes AC, Ellen S, et al. A predictive screening index for posttraumatic stress disorder and depression following traumatic injury. J Consult Clin Psychol. 2008;76:923–32. doi: 10.1037/a0012918. [DOI] [PubMed] [Google Scholar]
- 29.Carlson EB, Palmieri PA, Dalenberg CJ, Macia KS, Spain DA. Contributions of risk and protective factors to prediction of posttraumatic psychological disorder after traumatic injury. Comprehensive Psychiatry. doi: 10.1016/j.comppsych.2016.04.022. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Rose S, Koenen KC, Karam EG, Stang PE, Stein DJ, et al. How well can post-traumatic stress disorder be predicted from pre-trauma risk factors? An exploratory study in the WHO World Mental Health Surveys. World Psychiatry. 2014;13:265–274. doi: 10.1002/wps.20150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galatzer-Levy IR, Karstoft KI, Statnikov A, Shalev AY. Quantitative forecasting of PTSD from early trauma responses: a Machine Learning application. J Psychiatr Res. 2014;59:68–76. doi: 10.1016/j.jpsychires.2014.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karstoft K-I, Galatzer-Levy IR, Statnikov A, Li Z, Shalev AY Members of the Jerusalem Trauma and Outreach Prevention Study Group. Bridging a translational gap: using machine learning to improve the prediction of PTSD. BMC Psychiatry. 2015;15:30. doi: 10.1186/s12888-015-0399-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carlson EB, Dalenberg CJ, McDade-Montez E. Dissociation in Posttraumatic Stress Disorder Part I: Definitions and review of research. Psychological Trauma. 2012;4:479–489. [Google Scholar]
- 34.Carlson EB, Smith S, Palmieri P, Dalenberg C, Ruzek JI, Kimerling R, et al. Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment. 2011;23:463–477. doi: 10.1037/a0022294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ehring T, Ehlers A, Glucksman E. Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. J Consult Clin Psychol. 2008;76:219–230. doi: 10.1037/0022-006X.76.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Donnell ML, Elliott P, Creamer M, Wolfgang B. The role of posttraumatic appraisal in the development and maintenance of posttraumatic stress disorder. Journal of Traumatic Stress. 2007;20:173–182. doi: 10.1002/jts.20198. [DOI] [PubMed] [Google Scholar]
- 37.Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine. 2011;41:71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alegría M, Fortuna LR, Lin JY, Norris FH, Gao S, Takeuchi DT, et al. Prevalence, risk, and correlates of posttraumatic stress disorder across ethnic and racial minority groups in the United States. Medical Care. 2013;51:1114–1123. doi: 10.1097/MLR.0000000000000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Carlson EB, Field NP, Ruzek JI, Bryant RA, Dalenberg CJ, Keane TM, et al. Advantages and psychometric validation of proximal intensive assessments of patient reported outcomes collected in daily life. Quality of Life Research. 2016;25:507–516. doi: 10.1007/s11136-015-1170-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carlson EB. Psychometric study of a brief screen for PTSD: Assessing the impact of multiple traumatic events. Assessment. 2001;8:431–441. doi: 10.1177/107319110100800408. [DOI] [PubMed] [Google Scholar]
- 41.Beck AT, Steer RA. Task Force for the Handbook of Psychiatric Measures, editor Handbook of psychiatric measures. Washington, DC: American Psychiatric Association; 2000. Beck Depression Inventory; pp. 519–522. [Google Scholar]
- 42.Carlson EB, Waelde LC, Palmieri PA, Macia KS, Smith SR, McDade-Montez E. Development and validation of the Dissociative Symptoms Scale. Assessment. doi: 10.1177/1073191116645904. In press. [DOI] [PubMed] [Google Scholar]
- 43.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5) Washington, DC: Author; 2013. [Google Scholar]
- 44.Foa EB, Ehlers A, Clark DM, Tolin DF, Orsillo SM. The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment. 1999;11:303–314. [Google Scholar]
- 45.Caspi Y, Carlson EB, Klein E. Validation of a screening instrument for posttraumatic stress disorder in a community sample of Bedouin men serving in the Israeli Defense Forces. Journal of Traumatic Stress. 2007;20:517–527. doi: 10.1002/jts.20237. [DOI] [PubMed] [Google Scholar]
- 46.Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. [Google Scholar]
- 47.Furlanetto LM, Mendlowicz MV, Romildo Bueno J. The validity of the Beck Depression Inventory-Short Form as a screening and diagnostic instrument for moderate and severe depression in medical inpatients. Journal of Affective Disorders. 2005;86:87–91. doi: 10.1016/j.jad.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 48.Weathers FW, Keane TM, Davidson JRT. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- 49.Ehring T, Quack D. Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy. 2010;41:587–598. doi: 10.1016/j.beth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 50.Stovall-McClough KC, Cloitre M. Unresolved attachment, PTSD, and dissociation in women with childhood abuse histories. J Consult Clin Psychol. 2006;74:219–228. doi: 10.1037/0022-006X.74.2.219. [DOI] [PubMed] [Google Scholar]
- 51.Millon T. Millon Clinical Multiaxial Inventory III Manual. Minneapolis, MN: National Computer Systems; 1994. [Google Scholar]
- 52.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–96. [PubMed] [Google Scholar]
- 53.Sherbourne CD, Stewart AL. The MOS Social Support Survey. Social Science and Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 54.Lepore SJ, Helgeson VS. Social constraints, intrusive thoughts, and mental health after prostate cancer. Journal of Social & Clinical Psychology. 1998;17:89–106. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.