Abstract
Study Objectives:
Community-based research indicates that Black preschoolers tend to have more bedtime difficulties and are at higher risk for obstructive sleep apnea (OSA) compared to White preschoolers. This study examined differences in sleep patterns and problems by race among a clinical sample of Black and White preschoolers at an outpatient sleep clinic.
Methods:
Data were collected from electronic medical records for 125 children ages 2–5 years (mean = 3.37 years, 64.0% White, 36.0% Black; 59.2% male) presenting at a pediatric sleep clinic in an academic medical center. Neighborhood income data were based on ZIP codes entered into the United States Census Bureau's American Fact Finder.
Results:
Black patients (51.1%) were significantly more likely than White patients (20.0%) to bed-share with a caregiver (χ2 = 12.99, P ≤ .001). There were no other significant differences in presenting sleep patterns (bed/wake times, sleep onset latency, naps, night awakenings, or sleep opportunity). Logistic regressions showed that White patients were more likely to present with difficulty falling/staying asleep and receive an insomnia diagnosis, and Black patients were more likely to present with OSA-related concerns and receive a diagnosis of suspected OSA, even when controlling for relevant sociodemographic covariates.
Conclusions:
In contrast to community-based research, Black and White children showed similar sleep patterns. However, there were differences by race in referral questions and diagnoses. Findings suggest the need to consider caregiver perceptions and other sociocultural factors that may contribute to differential rates of presentation for sleep services, as well as potential health disparities in this regard.
Citation:
Williamson AA, Rubens SL, Patrick KE, Moore M, Mindell JA. Differences in sleep patterns and problems by race in a clinical sample of black and white preschoolers. J Clin Sleep Med. 2017;13(11):1281–1288.
Keywords: clinical services, insomnia, obstructive sleep apnea, preschoolers, race, sleep
INTRODUCTION
Although sleep problems affect 20% to 30% of infants, pre-schoolers, and kindergarteners,1,2 recent research indicates that young children from non-White racial/ethnic backgrounds are at increased risk of experiencing sleep difficulties compared to non-Hispanic/Latino White youth (hereafter the term “White” will be used to reference non-Hispanic/Latino White racial/ ethnic background). Specifically, studies comparing Black and White children have found that racial/ethnic background is a significant predictor of variation in preschoolers' sleep regularity, duration, and quality.3–5 Community-based studies have shown that Black preschoolers are more likely than their White peers to exhibit symptoms of behavioral sleep disturbances, such as increased bedtime resistance, longer sleep onset latency, and shorter total sleep duration.5–8 Aspects of sleep routines and the sleep environment also differ by race, with Black children showing later bedtimes and decreased likelihood of following a regular bedtime routine,5,6,8,9 as well as higher rates of parent-child bed-sharing.10,11 Later bedtimes and less regular bedtime routines have been associated with increased child sleep disturbances,2,12,13 and research on the effect of bed-sharing on child sleep is mixed.11 Some families may choose to bed-share due to cultural preferences or economic constraints (eg, overcrowded housing; limited household size or bed availability) and not necessarily in response to a child sleep problem.11
BRIEF SUMMARY
Current Knowledge/Study Rationale: Community-based research indicates that Black preschoolers exhibit more behavioral sleep problems and are at higher risk for obstructive sleep apnea (OSA) compared to White children. Little is known about differential rates of sleep disorders by race among young children who present for clinical services at outpatient pediatric sleep centers.
Study Impact: Despite few significant differences in sleep patterns, White patients were significantly more likely to present for sleep services for insomnia-related concerns, and Black children were significantly more likely to present for OSA-related concerns, even when controlling for relevant covariates. Study findings represent a first step in examining potential health disparities in referrals for and engagement in pediatric sleep services, particularly for behavioral sleep concerns.
Many of these differences in behavioral sleep patterns by race remain even when accounting for socioeconomic factors that have been independently associated with variation in child sleep,5,14,15 including household income and parental education. For instance, in a community sample of young children, socioeconomic status (SES) and Black racial background were independently associated with sleep difficulties, with Black children showing later bedtimes, shorter sleep durations, and increased daytime sleepiness relative to their White counterparts.8 Similarly, in a large sample of 3-year-old children, Black children were less likely to have regular bedtimes and bedtime routines compared to White children, even while controlling for maternal education.5
Black racial background has also been associated with an increased risk for symptoms of obstructive sleep apnea (OSA), including snoring and sleep-disordered breathing.16–20 The difference in pediatric OSA symptoms by race remains when controlling for lower SES and other factors associated with risk for OSA, such as obesity.16,18,20 For example, one study of a community sample of children ages 2 to 6 years found that Black children were 2.5 times more likely to snore than White children, adjusting for parental education, household income, and child body mass index (BMI).17 Another study of 1,010 low-SES pre-schoolers showed that relative to White children, Black children were more likely to exhibit sleep-disordered breathing, based on parent report of snoring, among other symptoms.20
To date, studies investigating differences by race in sleep patterns and problems among preschoolers have primarily used community-based rather than clinically referred samples. In addition, previous research has focused on symptoms of sleep problems rather than on rates of clinical diagnoses. As such, little is known about the differential rates of sleep disorders among young children who are referred to and present for clinical services at outpatient pediatric sleep centers. Although a previous study using a subset of the sample in the current study found differences by race in sleep problems and diagnostic impressions in a clinically referred sample of children ages newborn to 21 years,21 research focused specifically on preschool-aged children in this regard is lacking. The identification and treatment of sleep problems is especially important during early childhood given the increased neural plasticity and rapid growth that occurs during this developmental period.22,23 In addition, untreated early childhood sleep problems tend to persist over time24,25 and are associated with deficits in neurocognitive and emotional-behavioral functioning,26–29 thereby increasing risk for poor school readiness30,31: a key early childhood milestone.
Examining both sleep patterns and sleep problems by race in a sample of clinically referred children is also important in the context of the larger research on pediatric health disparities, which shows that non-White youth, as well as those of lower SES, are less likely than their White and higher SES peers to be referred to and/or present for specialty health care services.32,33 However, whether a similar pattern of health disparities exists in the area of pediatric sleep services for young children is relatively unknown. Characterizing differences in sleep patterns and problems by race among clinically referred preschoolers is a critical first step in understanding whether there is a need for targeted interventions aimed at reducing health disparities in early childhood pediatric sleep problems.
The purpose of this study was to examine differences by race in sleep patterns and problems among Black and White children ages 2 to 5 years presenting for an initial consultation at an outpatient pediatric sleep clinic. Using data drawn from electronic medical records (EMRs), we first compared Black and White preschoolers on parent-reported sleep patterns, including sleep location, bed and wake times, sleep onset latency, night awakenings, naps, and caffeine consumption. We then examined differences by race in presenting problems and subsequent provisional diagnostic impressions provided by pediatric sleep medicine providers.
METHODS
Participants
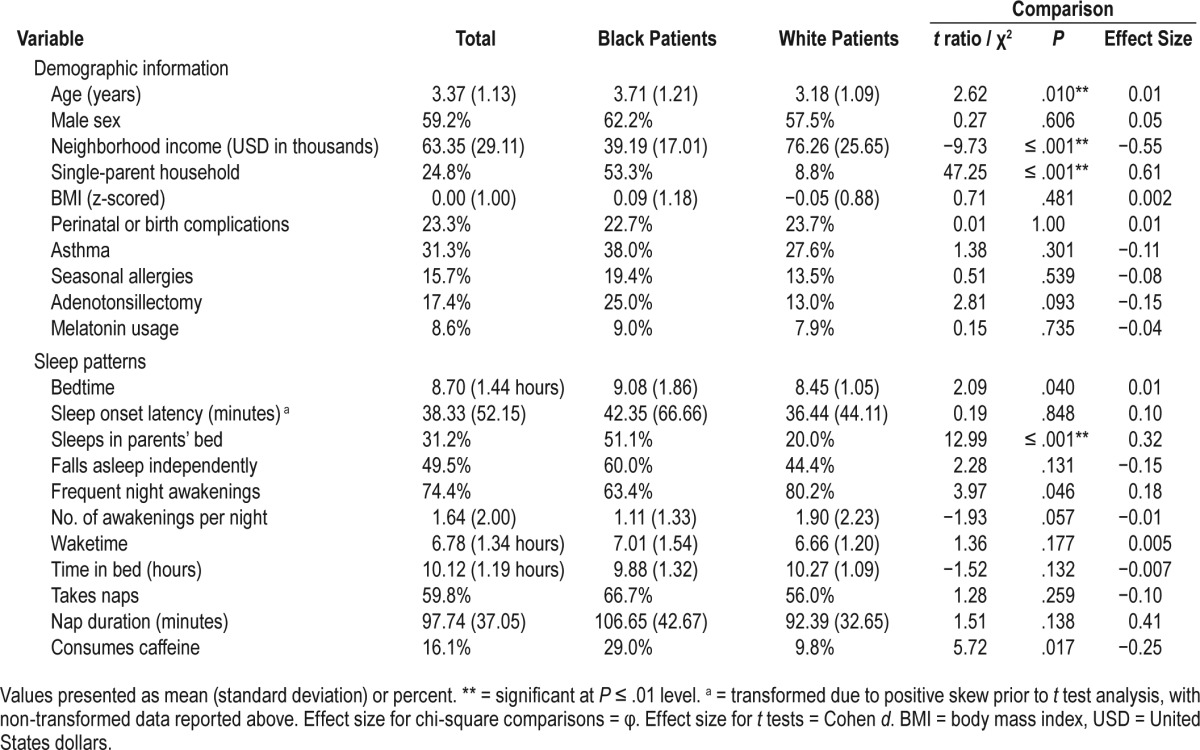
Participants were drawn from a database of 543 consecutive patients ages newborn to 21 years who presented for an initial outpatient sleep consultation at a large urban academic medical center. We conducted a retrospective review of EMRs for these patients, who were seen between August 2013 and April 2014 at either the main center's pediatric sleep clinic or at one of the two suburban satellite clinics. For the purposes of the current study, we selected children 2 to 5 years of age who identified as being of Black or White racial/ethnic background, given that our study aims were specific to these demographic groups. The final sample included 125 children (n = 80, 64.0% White; n = 45, 36.0% Black) with a mean age of 3.37 years (standard deviation = 1.13 years). Additional demographic information is reported in Table 1.
Table 1.
Demographic information, sleep patterns, and comparisons by racial background.
Procedure
Consistent with the current standard of care at the pediatric sleep center, patients are seen by an interdisciplinary pediatric sleep team. During the initial sleep consultation, a member of the team administers semistructured interview questions and records patient and/or caregiver responses in a note within the child's EMR. The semistructured intake interview is guided by a template in the EMR note. All patients and their caregivers are seen by at least one attending sleep physician. Patients also typically see other members of the interdisciplinary sleep clinic team during the visit, such as sleep medicine fellows, medical residents, behavioral sleep psychologists, doctoral-level psychology interns or graduate students, nurse practitioners, and respiratory therapists.
Which members of the sleep team see a particular patient depends on the reason for the visit. For instance, at intake, patients with a caregiver-identified or physician-suspected behavioral sleep concern are seen by a behavioral sleep psychologist or trainee if one of these providers is available, whereas patients presenting for follow-up OSA treatment often see a respiratory therapist for management of continuous positive airway pressure treatment. All patients in the current sample were seen by one of seven different attending sleep physicians. A total of 50.4% of patients in the current sample were seen by one of four behavioral sleep psychologists or one of seven doctoral-level psychology interns or graduate students supervised by one of the behavioral sleep psychologists.
EMR review procedures included abstracting race, ethnicity, sex, body mass index (BMI), and ZIP code data from the demographic section of the EMR, and abstracting data on presenting sleep patterns, referral question, and diagnostic impressions given to patients at the end of the visit from the initial sleep consultation note. Sleep pattern variables included sleep location (ie, whether the child sleeps in bed with a parent and whether the child falls asleep independently), patient bedtime, sleep onset latency, number of night awakenings, wake time, incidence and duration of daytime naps, and caffeine consumption. We calculated time in bed (ie, sleep opportunity) using bedtime and wake time. We also abstracted medical information, including whether the patient had a history of adenotonsillectomy, as this surgery is the first-line treatment for OSA34 and thus could affect whether children presented with OSA-related concerns. Other relevant medical information abstracted from the consultation note included risk factors for OSA16 (ie, perinatal/birth complications and history of asthma or seasonal allergies) and current use of melatonin as a sleep aid. Of note, the attending physician recorded birth or perinatal complications using a dichotomous drop-down (yes/no) field in the clinical note, and specific information about the nature of these complications (eg, prematurity, low birth weight) was not available. The patient median neighborhood income variable was generated by entering EMR ZIP codes into the American Community Survey.35 Additional details about coding variables have been described elsewhere.9,21
Sleep patterns and referral questions are based on caregiver and/or patient report, whereas diagnostic impressions were provided by the attending sleep medicine physician. Diagnoses provided at the end of the visit are considered to be provisional “impressions,” as diagnoses such as OSA require further assessment and confirmation via subsequent overnight polysomnography. An insomnia diagnosis was considered only if the caregiver and/or family members reported the sleep habits to be problematic.36 For the current study, we limited our examination to the most prevalent presenting referral questions and diagnostic impressions in our sample, which were presenting concerns related to difficulty falling/staying asleep and OSA (eg, snoring, labored breathing), and diagnostic impressions of insomnia (behavioral insomnia of childhood; psychophysiological insomnia; or insomnia secondary to an underlying medical or neurodevelopmental condition) or suspected OSA.
Five trained researchers reviewed and coded all EMRs of new sleep patients during the designated 9-month period. Disagreements or questions related to coding that were raised by coders during the coding phase were discussed until a consensus was reached. Following the completion of this phase, we conducted reliability coding for 20% of the coded data. Reliability calculations for each of the coding categories indicated adequate reliability, with kappa coefficients ranging from 0.80 to 1.00 across categories. All study data were collected and managed using REDCap37 electronic data capture tools hosted at the academic medical center. The academic medical center's Institutional Review Board approved this study.
Analyses
All analyses were completed using Statistical Package for the Social Sciences (SPSS) Version 23 Software (IBM Corp, Armonk, New York, United States). Variables were examined for normality. Sleep onset latency was transformed due to positive skew. Frequency of night awakenings, which was originally coded on a 3-point scale (never, sometimes, often) was recoded to reflect a dichotomous rating (0 = never, 1 = sometimes or often). BMI was z-scored.
To examine differences between Black and White children in demographic information and sleep patterns, we computed t tests for continuous variables and chi-square tests for categorical variables. We set a conservative alpha level of .01 for t tests and chi-square analyses, due to the number of comparisons.
To examine differences in referral question and diagnostic impressions, we conducted logistic regressions with the referral outcomes of difficulty falling/staying asleep and OSA, and the diagnostic impression outcomes of insomnia disorder and suspected OSA (pending further assessment via polysomnography). These models regressed the dichotomously coded referral question or diagnostic impression on racial background (Black versus White) and demographic covariates, including child age, sex, z-scored BMI and neighborhood income. We also entered whether patients shared a bed with a caregiver as a covariate into both insomnia and OSA-related models. For insomnia concerns, bed-sharing with a caregiver may be in response to child difficulty falling or staying asleep, due to environmental constraints, or due to cultural preferences.11 For OSA-related concerns, families who bed-share may be more aware of whether or not a child exhibits OSA symptoms, such as snoring. We additionally entered in previous adenoid or tonsil removal surgery as a covariate in OSA-related models, given that this surgery is the first-line treatment for pediatric OSA in the context of adenoid or tonsillar hypertrophy.34 Alpha level for logistic regressions was set at .05.
RESULTS
Differences in Demographic Information and Presenting Sleep Patterns
Few statistically significant differences emerged between Black and White patients in demographic information and presenting sleep patterns (Table 1). There were no significant differences by race for child BMI, prevalence of birth/perinatal complications, or history of asthma or allergies. Rates of melatonin usage also did not differ significantly by race. Black patients had a significantly lower median neighborhood income level compared to White patients (approximately $39,000 for Black patients and $76,000 for White patients, t = −9.73, P ≤ .001, d = −0.55). In addition, Black patients (53.3%) were significantly more likely than White patients (8.8%) to live in a single-parent versus a two-parent or other type of household (eg, relative care), χ2 (1) = 47.25, P < .001, φ = 0.61. Black patients were slightly older (3.71 years) than White patients (3.18 years) when presenting to clinic (t = 2.62, P = .010, d = 0.01), although this effect was small.
With regard to presenting sleep patterns, the only significant finding was that Black patients were more likely than White patients to sleep in a bed shared with a caregiver (51.1% for Black patients and 20.0% for White patients, χ2 (1) = 12.99, P < .001, φ = 0.32). Among children who did bed-share, 50.0% of Black patients fell asleep independently, compared to 1.5% of White patients, χ2 (1) = 3.63, P = .057, φ = −0.37. Regard -less of where they slept, overall 60.0% of Black patients fell asleep independently at bedtime compared to 44.4% of White patients, χ2 (1) = 2.28, P = .131, φ = −0.15.
Differences in Insomnia and OSA-Related Presenting Concerns
Overall, 61 patients (48.8%) presented with concerns related to insomnia (difficulty falling or staying asleep) and 70 (56.0%) presented with OSA-related concerns, such as snoring or difficulty breathing during sleep. Fifteen patients (12.0%) presented with both insomnia and OSA-related concerns. Logistic regression examining differences by race in insomnia-related presenting concerns while controlling for child age, sex, income, BMI, and parent-child bed-sharing showed that White patients (62.5%) were significantly more likely than Black patients (24.4%) to present with difficulties related to insomnia (odds ratio [OR] = 3.23, 95% confidence interval, or CI [1.05, 9.81], P = .041). Excluding parent-child bed-sharing from these models did not change the pattern of significance for the results reported here. By contrast, logistic regression with the covariates of child age, sex, income, BMI, and adenotonsillectomy status showed that Black patients (77.8%) were 4.16 times as likely as White patients (43.8%) to present with OSA-related concerns (OR = 0.24, 95% CI [0.08, 0.76], P = .015). None of the covariates included in two models were significantly associated with the likelihood of insomnia- or OSA-related presenting concerns.
Differences in Insomnia and OSA Diagnostic Impressions
A total of 46 patients (36.8%) were given a diagnosis of insomnia disorder (behavioral insomnia of childhood [82.6%]; psychophysiological insomnia [2.2%]; or insomnia secondary to an underlying medical or neurodevelopmental condition subtypes [15.2%]). Seventy-eight patients (62.4%) were given a diagnosis of suspected OSA. Twenty patients (16%) were given a diagnosis of both insomnia and suspected OSA. When differences by race in diagnostic impressions were examined in the context of logistic regressions controlling for covariates, analyses showed that White patients (48.8%) were significantly more likely than Black patients (15.6%) to receive a diagnosis of insomnia disorder (OR = 3.96, 95% CI [1.73, 13.39], P = .027). Excluding parent-child bed-sharing from these models did not change the pattern of significance for the results reported here. Similar to the aforementioned pattern with regard to referral questions, Black patients (80.0%) were significantly more likely than White patients (52.5%) to receive a diagnosis of suspected OSA (OR = 0.26, 95% CI [0.08, 0.90], P = .033). No covariates were significantly associated with the likelihood of an insomnia or suspected OSA diagnosis in either model.
DISCUSSION
This study examined whether findings from community-based research on differences in preschoolers' sleep patterns and problems by race were replicated in a sample of Black and White preschoolers presenting to an outpatient pediatric sleep clinic. Study findings provide preliminary information about possible sociocultural differences in perceptions about child sleep problems, as well as potential race-related health disparities in presentation to specialty care services for pediatric sleep concerns, especially for behavioral sleep disorders. More broadly, there appears to be a health disparity in patients presenting to the main hospital's sleep clinic, where most patients were seen. Whereas the sleep clinic population was more likely to be White and to reside in higher-income neighborhoods, patients seen in the primary care sites in the communities surrounding the main hospital's sleep clinic are predominantly Black (75%) and of lower SES (over 50% living at or below the poverty line; 77% receiving medical assistance).38
Few differences were seen in demographic data or sleep patterns by racial background. Black children were slightly older at their initial consultation compared to White children. Although the magnitude of this difference was small, this finding points to a potential disparity in the age at which children may be identified by a primary care or other provider and referred to a specialty clinic for sleep problems. Black youth in this sample also were more likely to live in a single-parent household, and resided in neighborhoods with a lower income on average than White youth. Surprisingly, we did not find effects of neighborhood income when this variable was included as a covariate in logistic regression models related to presenting sleep concerns and subsequent diagnostic impressions, despite data on health disparities32,33 and increased OSA and behavioral sleep concerns5,8,14,15,18 for socioeconomically disadvantaged populations. However, as described further in the next paragraphs, our measure of SES is limited by the use of a single indicator, which could have affected our results.
The only significant difference in sleep patterns across race was that Black children were more likely than White children to share a bed with a caregiver as opposed to sleeping independently in another location. This is both consistent with community-based research6,10 and potentially attributable to sociocultural factors that were not measured in the current study.6,39 For instance, Salm Ward and Doering39 have described a socioecological model for differences in mother-infant bed-sharing practices by race that contains multiple contributing sociocultural factors at the infant, maternal, familial, community, and societal level. Such a model has yet to be examined in the context of bed-sharing beyond infancy; however, sociocultural factors at multiple ecological levels likely contribute to differences by race in bed-sharing for pre-schoolers in both clinical and nonclinical samples. These factors also likely play different roles in predicting bed-sharing practices based on whether bed-sharing occurs as a response to a child sleep problem, due to economic constraints, as an intentional practice, or perhaps as a combination of these reasons.11 Bed-sharing could also be due to current or past medical concerns.11,40 Black and White children in this sample did not significantly differ in their rates of perinatal or birth complications, allergies, or asthma; however, other medical conditions more likely to be associated with bed sharing (epilepsy, sickle cell anemia)40,41 were not studied. Future research should consider differences in such medical conditions and their association with bed sharing.
As bed-sharing practices were not associated with an increased likelihood of insomnia in our sample, and Black children who shared a bed were more likely than White children who shared a bed to fall asleep independently, this practice may reflect different parental ideologies and childhood experiences.11 In addition, family composition and household size could play a role, given that in this sample, Black children were both more likely to bed-share and more likely to live in single-parent households. It could be that bed-sharing with a child is considered to be more problematic in two-parent households for reasons related to one or both parents' sleep preferences or needs, although this has yet to be examined empirically. Further research that examines bed-sharing beyond infancy is necessary to better understand this practice, as well as how this practice may relate to parents' perceptions of child sleep needs and problems, and decision to seek pediatric sleep treatment.11
Although no other sleep patterns measured in this study differed significantly by race, certain patterns were still notable. The slightly later bedtimes and longer nap duration for Black children in this sample converge with previous research drawn from community-based samples.3,5–8 It may be that these results did not significantly differ from patterns of White children due to the nature of the clinically referred sample. It was striking that 16.1% of all children in our sample had reportedly consumed caffeine. Caffeine is a known sleep disruptor,42,43 and the American Academy of Pediatrics recommends against any caffeine consumption during childhood and adolescence.44 By contrast, 8.6% of patients overall had a history of melatonin use, with no difference in prevalence by race. Melatonin has been used for sleep onset-related issues, particularly in children with neurodevelopmental delays; however, behavioral approaches remain the first-line treatment for pediatric insomnia.45 These findings highlight the need for increased efforts at disseminating healthy sleep recommendations and information about behavioral sleep treatment approaches for caregivers of preschoolers even before they are seen in a specialty sleep clinic.
Black preschoolers in this sample were more likely to present for OSA-related concerns. This was the case even when controlling for neighborhood income, BMI, and adenotonsillectomy, factors that have previously been associated with OSA in young children.18,34 This finding parallels previous research showing increased OSA symptoms (ie, snoring and sleep-disordered breathing) among Black children relative to White children.18–20 Seasonal allergies and asthma have been shown to increase risk for OSA16; however, rates of these risk factors did not differ by race in this sample. Goldstein et al.17 note several genetic factors that may increase predisposition for rates of OSA in specific racial/ethnic groups, including differences in craniofacial anatomy, neuromuscular tone, and fat distribution. Identifying these genetic factors, and how they may interact with environmental effects to produce OSA onset in early childhood is especially important given the broad developmental risks that OSA poses to young children.26,27,34
Further, despite Black preschoolers having sleep patterns similar to those of White children in this sample, a greater proportion of White children presented for difficulty falling/ staying asleep concerns and were given a diagnosis of pediatric insomnia. This difference was present even when we controlled for caregiver-child bed-sharing. Unmeasured socio-cultural factors likely affected these racial differences in presenting sleep concerns and diagnostic impressions, and in the rate of presentation to a specialty care clinic for pediatric sleep problems.32 Such sociocultural factors could include caregivers' sleep-related cognitions and behaviors, which appear to emerge in infancy46 and have been linked to subsequent objectively measured preschool sleep quality.47 Given that caregiver report is typically the basis for determining the symptoms and functional effect of insomnia disorder in young children,36,46 it could be that caregivers of White preschoolers in the current sample perceived their child's sleep habits as more problematic or difficult to manage compared with caregivers of Black children6 or that they were more willing to share concerns with providers.
White caregivers may also have different expectations for child sleep relative to caregivers of other sociocultural backgrounds. Several studies using community-based samples have investigated differences in caregiver perceptions of preschool sleep problems by race/ethnicity within the United States6,7 and internationally,4,48 with mixed results. Within the United States, one study found that White mothers reported greater concerns than Black mothers about their child having difficulty falling asleep, regardless of mother-child sleeping arrangements.6 Patrick, Millet, and Mindell7 found that although Black caregivers rated their preschoolers as having increased bedtime resistance and rated themselves as feeling less confident in managing their child's sleep problems, Black and White caregivers did not differ on ratings of their child's sleep as problematic. Additional research on multiple dimensions of caregiver perceptions of sleep, including healthy versus problematic sleep behaviors, expectations for child sleep patterns and problems, and sleep-related parenting self-efficacy is needed in clinical and non-clinical samples. Such data will serve to illuminate how these factors may contribute to differences by race in behavioral sleep problem identification and treatment-seeking behaviors. Research examining sources of sleep clinic referrals and factors related to families following through on a referral to a specialty sleep clinic, including barriers to accessing care (eg, transportation, childcare difficulties, shift work), is also warranted to better understand potential health disparities in this regard, and to inform assessment and interventions to address the needs of diverse families.
Study results should be considered in the context of several limitations. As these data are based on information that is care-giver reported and then physician documented, future research with clinical samples would benefit from the use of standardized, caregiver-reported sleep questionnaires as well as objective sleep measures, such as actigraphy, to assess child sleep patterns and polysomnography to confirm OSA diagnoses. In addition, and as noted previously, a direct assessment of care-giver perceptions about multiple aspects of sleep in early childhood (ie, importance of sleep, healthy versus problematic sleep habits, self-efficacy in managing child medical and behavioral sleep problems), as well as other sociocultural variables that affect these perceptions and child sleep habits, are needed to better understand variation by race in rates of sleep patterns and problems within a larger socioecological framework.39,46 The family history of sleep problems was not accessible in this dataset, and should be examined in research on sociodemo-graphic differences in treatment-seeking behaviors for child sleep problems. A family history of sleep difficulties could affect caregiver knowledge of and sensitivity to child OSA or insomnia-related sleep concerns, and may influence willingness to seek treatment.
Multiple indicators of socioeconomic background, including household income, caregiver education and employment, and caregiver health literacy should also be examined in future studies of differences by race in the sleep of clinically referred young children. Especially as socioeconomic factors have been found to interact in complex ways with both caregiver racial/ ethnic background and sleep-related caregiver behaviors to predict child sleep patterns and problems,7,14 an examination of these factors using multiple measures is needed in research that examines sleep problems in clinical samples, as well as potential disparities in pediatric sleep services. Future research studies on this topic should include multiple points of assessment prior to the initial sleep consultation, such as at the point of sleep problem identification and/or at referral to a specialty sleep clinic, as well as following the initial consultation, to assess diagnostic confirmation of OSA, treatment adherence for insomnia and OSA, and related follow-up care. In addition, information about whether families were referred by a medical or other provider, or were self-referred, and whether this information varies by sociodemographic factors should be collected in future studies. More information about variation by race according to the child sleep environment, including aspects of sleep health, such as whether the child fell asleep using electronics, could also identify important targets of preventive interventions. Collectively, this research is an important next step in examining potential disparities by race and other sociodemographic factors in the continuum of health services for pediatric sleep problems.
Although additional research is needed, this study has provided initial information about differences by race in sleep patterns and problems among a sample of clinically-referred Black and White children. In light of research on the deleterious effects of untreated pediatric insomnia and OSA on broad early childhood development, and neurocognitive and emotional-behavioral functioning in particular,26–29 it is important to examine where potential sleep problem identification and treatment gaps and disparities may occur for sociodemographically diverse young children. In particular, this study's findings underscore the need to consider caregiver perceptions and other sociocultural variables that may contribute to differential rates of presentation for pediatric sleep services. Additionally, future research is needed in order to identify whether there are racial/ethnic and socioeconomic disparities in the identification of sleep problems in primary care settings, referral to sleep clinics, and follow through on these referrals in order to understand and address barriers to accessing this care.
DISCLOSURE STATEMENT
This study was conducted at Children's Hospital of Philadelphia. All authors have seen and approved this manuscript. The authors have indicated no financial conflicts of interest. Ariel A. Williamson was supported during this study by a postdoctoral fellowship T32HL007953-17 from the National Heart, Lung, and Blood Institute.
ABBREVIATIONS
- BMI
body mass index
- CI
confidence interval
- EMR
electronic medical record
- OR
odds ratio
- OSA
obstructive sleep apnea
- REDCap
Research Electronic Data Capture
- SES
socioeconomic status
- SPSS
Statistical Package for the Social Sciences
- USD
United States dollars
REFERENCES
- 1.Hiscock H, Canterford L, Ukoumunne OC, Wake M. Adverse associations of sleep problems in Australian preschoolers: national population study. Pediatrics. 2007;119(1):86–93. doi: 10.1542/peds.2006-1757. [DOI] [PubMed] [Google Scholar]
- 2.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10(7):771–779. doi: 10.1016/j.sleep.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Crosby B, LeBourgeois MK, Harsh J. Racial differences in reported napping and nocturnal sleep in 2-to 8-year-old children. Pediatrics. 2005;115(Supplement 1):225–232. doi: 10.1542/peds.2004-0815D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mindell JA, Sadeh A, Kwon R, Goh DY. Cross-cultural differences in the sleep of preschool children. Sleep Med. 2013;14(12):1283–1289. doi: 10.1016/j.sleep.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 5.Hale L, Berger LM, LeBourgeois MK, Brooks-Gunn J. Social and demographic predictors of preschoolers' bedtime routines. J Dev Behav Pediatr. 2009;30(5):394–402. doi: 10.1097/DBP.0b013e3181ba0e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Milan S, Snow S, Belay S. The context of preschool children's sleep: racial/ethnic differences in sleep locations, routines, and concerns. J Family Psychol. 2007;21(1):20–28. doi: 10.1037/0893-3200.21.1.20. [DOI] [PubMed] [Google Scholar]
- 7.Patrick KE, Millet G, Mindell JA. Sleep differences by race in preschool children: the roles of parenting behaviors and socioeconomic status. Behav Sleep Med. 2016;14(5):467–479. doi: 10.1080/15402002.2015.1017101. [DOI] [PubMed] [Google Scholar]
- 8.Crabtree VM, Korhonen JB, Montgomery-Downs HE, Jones VF, O'Brien LM, Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Med. 2005;6(4):319–324. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 9.Williamson AA, Patrick KE, Rubens SL, Moore M, Mindell JA. Pediatric sleep disorders in an outpatient sleep clinic: clinical presentation and needs of children with neurodevelopmental conditions. Clin Pract Pediatr Psychol. 2016;4(2):188–199. [Google Scholar]
- 10.Barajas RG, Martin A, Brooks-Gunn J, Hale L. Mother-child bed-sharing in toddlerhood and cognitive and behavioral outcomes. Pediatrics. 2011;128(2):e339–e347. doi: 10.1542/peds.2010-3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mileva-Seitz V, Bakersmans-Kraneburg M, Battaini C, Luijk M. Parent-child bed-sharing: The good, the bad, and the burden of evidence. Sleep Med Rev. 2017;32:4–27. doi: 10.1016/j.smrv.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 12.Henderson JA, Jordan SS. Development and preliminary evaluation of the Bedtime Routines Questionnaire. J Psychopathol Behav Assess. 2010;32(2):271–280. [Google Scholar]
- 13.Mindell JA, Li AM, Sadeh A, Kwon R, Goh DY. Bedtime routines for young children: a dose-dependent association with sleep outcomes. Sleep. 2015;38(5):717–722. doi: 10.5665/sleep.4662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Sheikh M, Bagley EJ, Keiley M, Elmore-Staton L, Chen E, Buckhalt JA. Economic adversity and children's sleep problems: Multiple indicators and moderation of effects. Health Psychol. 2013;32(8):849–859. doi: 10.1037/a0030413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jarrin DC, McGrath JJ, Quon EC. Objective and subjective socioeconomic gradients exist for sleep in children and adolescents. Health Psychol. 2014;33(3):301–305. doi: 10.1037/a0032924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children: associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med. 1999;159(5):1527–1532. doi: 10.1164/ajrccm.159.5.9809079. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein NA, Abramowitz T, Weedon J, Koliskor B, Turner S, Taioli E. Racial/ ethnic differences in the prevalence of snoring and sleep disordered breathing in young children. J Clin Sleep Med. 2011;7(2):163–171. [PMC free article] [PubMed] [Google Scholar]
- 18.Spilsbury JC, Storfer-Isser A, Kirchner HL, et al. Neighborhood disadvantage as a risk factor for pediatric obstructive sleep apnea. J Pediatr. 2006;149(3):342–347. doi: 10.1016/j.jpeds.2006.04.061. [DOI] [PubMed] [Google Scholar]
- 19.Rosen CL, Larkin EK, Kirchner HL, et al. Prevalence and risk factors for sleep-disordered breathing in 8-to 11-year-old children: association with race and prematurity. J Pediatr. 2003;142(4):383–389. doi: 10.1067/mpd.2003.28. [DOI] [PubMed] [Google Scholar]
- 20.Montgomery-Downs HE, Jones VF, Molfese VJ, Gozal D. Snoring in preschoolers: associations with sleepiness, ethnicity, and learning. Clin Pediatr. 2003;42(8):719–726. doi: 10.1177/000992280304200808. [DOI] [PubMed] [Google Scholar]
- 21.Rubens SL, Patrick KE, Williamson AA, Moore M, Mindell JA. Individual and socio-demographic factors related to presenting problem and diagnostic impressions at a pediatric sleep clinic. Sleep Med. 2016;25:67–72. doi: 10.1016/j.sleep.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 22.Black MM, Walker SP, Fernald LC, et al. Early childhood development coming of age: science through the life course. Lancet. 2017;389(10064):77–90. doi: 10.1016/S0140-6736(16)31389-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guerra NG, Williamson AA, Lucas-Molina B. Normal development: Infancy, childhood and adolescence. In: Rey JM, editor. IACAPAP Textbook of Child and Adolescent Mental Health. Geneva: International Association for Child and Adolescent Psychiatry and Allied Professions; 2012. [Google Scholar]
- 24.Bonuck KA, Chervin RD, Cole TJ, et al. Prevalence and persistence of sleep disordered breathing symptoms in young children: a 6-year population-based cohort study. Sleep. 2011;34(7):875–884. doi: 10.5665/SLEEP.1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kataria S, Swanson MS, Trevathan G. Persistence of sleep disturbances in preschool children. J Pediatr. 1987;110(4):642–646. doi: 10.1016/s0022-3476(87)80571-1. [DOI] [PubMed] [Google Scholar]
- 26.Bourke R, Anderson V, Yang JS, et al. Cognitive and academic functions are impaired in children with all severities of sleep-disordered breathing. Sleep Med. 2011;12(5):489–496. doi: 10.1016/j.sleep.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 27.Jackman AR, Biggs SN, Walter LM, et al. Sleep-disordered breathing in preschool children is associated with behavioral, but not cognitive, impairments. Sleep Med. 2012;13(6):621–631. doi: 10.1016/j.sleep.2012.01.013. [DOI] [PubMed] [Google Scholar]
- 28.Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen L, Ystrom E, Hysing M. Later emotional and behavioral problems associated with sleep problems in toddlers: a longitudinal study. JAMA Pediatr. 2015;169(6):575–582. doi: 10.1001/jamapediatrics.2015.0187. [DOI] [PubMed] [Google Scholar]
- 29.Williams KE, Berthelsen D, Walker S, Nicholson JM. A developmental cascade model of behavioral sleep problems and emotional and attentional self-regulation across early childhood. Behav Sleep Med. 2017;15(1):1–21. doi: 10.1080/15402002.2015.1065410. [DOI] [PubMed] [Google Scholar]
- 30.Quach J, Hiscock H, Ukoumunne OC, Wake M. A brief sleep intervention improves outcomes in the school entry year: a randomized controlled trial. Pediatrics. 2011;128(4):692–701. doi: 10.1542/peds.2011-0409. [DOI] [PubMed] [Google Scholar]
- 31.Ravid S, Afek I, Suraiya S, Shahar E, Pillar G. Kindergarten children's failure to qualify for first grade could result from sleep disturbances. J Child Neurol. 2009;24(7):816–822. doi: 10.1177/0883073808330766. [DOI] [PubMed] [Google Scholar]
- 32.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(2):e286–e298. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- 33.Larson K, Cull WL, Racine AD, Olson LM. Trends in access to health care services for US children: 2000-2014. Pediatrics. 2016;138(6):e20162176. doi: 10.1542/peds.2016-2176. [DOI] [PubMed] [Google Scholar]
- 34.Marcus C, Brooks LJ, Draper KA, et al. Clinical practice guideline: Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130:576–584. doi: 10.1542/peds.2012-1671. [DOI] [PubMed] [Google Scholar]
- 35.American community survey. 2005-2009 5-year estimates. United States Census Bureau American Fact Finder website. [Accessed September 14, 2017]. http://factfinder.census.gov.
- 36.American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 37.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.CHOP Care Network Information for grants 2017. Pediatric Research Consortium website. [Accessed September 14, 2017]. http://perc.research.chop.edu. Published 2017.
- 39.Salm Ward TC, Doering JJ. Application of a socio-ecological model to mother- infant bed-sharing. Health Educ Behav. 2014;41(6):577–589. doi: 10.1177/1090198114543010. [DOI] [PubMed] [Google Scholar]
- 40.Boergers J, Koinis-Mitchell D. Sleep and culture in children with medical conditions. J Pediatr Psychol. 2010;35(9):915–926. doi: 10.1093/jpepsy/jsq016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Larson AM, Ryther RC, Jennesson M, et al. Impact of pediatric epilepsy on sleep patterns and behaviors in children and parents. Epilepsia. 2012;53(7):1162–1169. doi: 10.1111/j.1528-1167.2012.03515.x. [DOI] [PubMed] [Google Scholar]
- 42.Owens JA, Mindell J, Baylor A. Effect of energy drink and caffeinated beverage consumption on sleep, mood, and performance in children and adolescents. Nutr Rev. 2014;72(Suppl 1):65–71. doi: 10.1111/nure.12150. [DOI] [PubMed] [Google Scholar]
- 43.Warzak WJ, Evans S, Floress MT, Gross AC, Stoolman S. Caffeine consumption in young children. J Pediatr. 2011;158(3):508–509. doi: 10.1016/j.jpeds.2010.11.022. [DOI] [PubMed] [Google Scholar]
- 44.Schneider MB, Benjamin HJ. Sports drinks and energy drinks for children and adolescents: are they appropriate? Pediatrics. 2011;127(6):1182–1189. doi: 10.1542/peds.2011-0965. [DOI] [PubMed] [Google Scholar]
- 45.Zhou ES, Owens J. Behavioral treatments for pediatric insomnia. Curr Sleep Med Rep. 2016;2(3):127–135. [Google Scholar]
- 46.Sadeh A, Tikotzky L, Scher A. Parenting and infant sleep. Sleep Med Rev. 2010;14(2):89–96. doi: 10.1016/j.smrv.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 47.Tikotzky L, Shaashua L. Infant sleep and early parental sleep-related cognitions predict sleep in pre-school children. Sleep Med. 2012;13(2):185–192. doi: 10.1016/j.sleep.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 48.Sadeh A, Mindell J, Rivera L. “My child has a sleep problem”: a cross-cultural comparison of parental definitions. Sleep Med. 2011;12(5):478–482. doi: 10.1016/j.sleep.2010.10.008. [DOI] [PubMed] [Google Scholar]


