Abstract
Background and Objectives
Fractional treatment with a dual wavelength 1,064 and 532 nm picosecond‐domain laser, delivering a 10 × 10 array of highly focused beamlets via a holographic optic, was investigated for the treatment of acne scars.
Study
Twenty‐seven of 31 subjects completed the study, 19 were treated using 1,064 nm and 8 were treated at 532 nm, all having four‐monthly treatments. Blinded evaluation of digital images by three physician evaluators comparing pre‐ and 3‐month post‐treatment images measured efficacy using a 10‐point scale. Subject self‐assessment of treatment effects were also recorded. Safety was measured by recording subject discomfort scores and adverse effects.
Results
Blinded reviewers correctly identified the baseline image in 61 of the 81 image sets (75%), and baseline acne scar scores were 1.8 ± 0.7 and 1.8 ± 0.5 for the 1,064 and 532 nm cohorts, and decreased to 1.1 ± 0.5 (P < 0.001) and 1.1 ± 0.0 (P < 0.005), respectively. Post‐treatment erythema, mild edema, and petechiae were the only side effects noted.
Conclusion
The 1,064 and 532 nm picosecond‐domain laser incorporating a 10 × 10 holographic beam‐splitting handpiece was found to be safe and effective for the treatment of facial acne scars. The treatments were well tolerated and the subjects experienced little to no downtime. Lasers Surg. Med. 49:796–802, 2017. © 2017 The Authors. Lasers in Surgery and Medicine Published by Wiley Periodicals, Inc.
Keywords: acne scars, treatment, fractionated, picosecond, laser
INTRODUCTION
Laser‐induced optical breakdown (LIOB) of tissue has been used in ophthalmology since the early 1980s, where the lack of light absorption by many structures of the eye requires optical breakdown to elicit a laser treatment effect, as opposed to thermal breakdown by selective absorption of energy by chromophores within tissue 1, 2, 3, 4. More recently, picosecond‐domain lasers have exploited LIOB in the skin for applications including skin rejuvenation and the treatment of acne scars 5, 6, 7, 8, 9. These picosecond‐domain lasers were first developed for cutaneous use to optimize removal of decorative tattoos 10, 11, 12, 13, 14. Habbema et al. describe LIOB targeting the papillary dermis with tightly focused picosecond‐domain 1,064 nm pulses 5, 6. Although these authors’ original intent was to achieve color‐insensitive hair reduction; the small, well‐confined treatment areas naturally led to applications for tissue remodeling with minimal downtime. Since the Habbema studies, new technology using a micro‐lens array with a 755 nm picosecond‐domain laser was developed to fractionate the laser beam into many focused areas of higher‐intensity laser energy allowing hand‐held, painting‐mode treatments for improving the appearance of facial acne scars and for skin rejuvenation 7, 8, 9. The lens array creates focused areas of higher‐intensity laser energy, with lower energy zones in‐between. Other lasers delivering focused beamlets of picosecond‐domain pulses were subsequently developed using different wavelengths, including both 1,064 and 532 nm neodymium: yttrium aluminum garnet (Nd:YAG) lasers incorporating a potassium titanyl phosphate (KTP) frequency‐doubling crystal, which is the type of laser used in the current study. Recent reports showed intraepithelial lesions that are consistent with those seen with the 755 nm picosecond domain laser 15, 16, 17, confirming that melanin absorption in melanosomes in the epidermis is the target for optical breakdown of tissue with 1,064 and 532 nm wavelengths as well.
Fractionated lasers have been used for improving photodamage and acne scarring, due to their ability to create microthermal treatment zones, which results in skin inflammation and subsequent remodeling 18, 19, 20, 21, 22, 23, 24, 25, 26, 27. As compared to the non‐fractionated ablative resurfacing devices that preceded them, the time to complete healing following treatment, as well as potential side effects, were generally greatly reduced when using fractionated lasers as compared to non‐fractionated lasers. Both ablative and non‐ablative lasers, mainly those targeting water absorption, have been used to induce skin remodeling in photodamaged or acne‐scarred skin 28. However, these lasers often resulted in significant hyperpigmentation when treating more darkly pigmented skin 21. In the current study, we investigate the ability of a new picosecond‐domain laser, using 532 and 1,064 nm fractionated laser energy administered with a holographic lens array, to deliver all the laser energy in highly focused beamlets arranged in a square grid. The purpose was to investigate both the safety and efficacy of this device for improving the appearance of acne scarring.
MATERIALS AND METHODS
This is a prospective study of the safety and efficacy of a new picosecond‐domain, 532 and 1,064 nm Nd:YAG laser used in combination with a fractionating holographic optic for the treatment of acne scars on the face.
Subjects
Healthy male and female subjects, 18–75 years of age, with Fitzpatrick skin types I–VI, and desiring treatment for acne scars on the face were eligible for this IRB‐approved study (Table 1). Subjects were required to have bilateral, mild to severe facial acne scars. Subjects who are pregnant or are breastfeeding, have a sensitivity to light, have an active tan, have a significant skin condition on the face, a history of squamous cell carcinoma or melanoma, a history of keloid scarring or abnormal wound healing, or who are prone to bruising, or have used isotretinoin within 12 months of the initial treatment were excluded from the study. All subjects provided written informed consent to serve as subjects in this study.
Table 1.
Age Range and Mean, as Well as Fitzpatrick Skin Types of Subjects Treated With the 1,064 nm and 532 nm Laser
| 31 subjects enrolled in study | |
| 21 subjects intent to treat at 1,064 nm | |
| 10 subjects intent to treat at 532 nm | |
| 27 subjects completed the study | |
| 19 subjects treated at 1,064 nm (3 males, 16 females) | |
| Mean age (range) | 45 (23–70) |
| Skin type II | 5 |
| III | 7 |
| IV | 5 |
| V | 2 |
| 8 subjects treated at 532 nm (1 male, 7 females) | |
| Mean age (range) | 45 (23–65) |
| Skin type II | 1 |
| III | 4 |
| IV | 3 |
Laser Treatment
A frequency‐doubled Nd:YAG picosecond‐domain laser system (PicoWay®, Syneron‐Candela Corporation, Wayland, MA), fitted with a holographic beam‐splitting optic (PicoWay Resolve®, Syneron‐Candela Corporation) was used for laser treatments. The system delivers a 10 × 10 array of 150 μm‐diameter microbeams arranged in a 6 mm × 6 mm, square treatment area (Fig. 1). The laser delivered from 1.3–2.9 mJ/microbeam at 1,064 nm with a pulse‐duration of 450 ps, and from 0.16–1.5 mJ/microbeam at 532 nm with a pulse‐duration of 375 ps. The laser repetition rate was also adjustable from 1 to 10 Hz, and treatments were administered using a repetition rate of 6 Hz.
Figure 1.
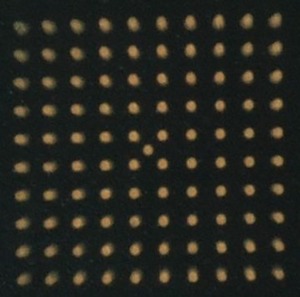
The microbeam pattern of the 1,064 nm, Nd:YAG laser with a holographic beam splitter demonstrated on flash paper showing the fine 10 × 10 pattern of 100 microbeams with no intervening reaction between spots.
No topical anesthesia was applied prior to laser treatment for any subject. Subjects received 4 monthly treatments with either the fractionated 1,064 nm or fractionated 532 nm wavelength, using a Nd:YAG picosecond‐domain laser incorporating a KTP, frequency doubling crystal fitted with novel holographic beam‐splitter optic. Subjects were treated to the entire cosmetic unit in areas of acne scarring, as evaluated by the treating physician, which ranged from the cheeks alone, to the entire face. Two laser passes were administered sequentially in rows at right angles to one another, one vertical and one horizontal, treating the affected areas by delivering pulses in a painting mode. Treatment energies were determined by the treating physician based on experience with the laser and tissue reaction, where erythema and mild petechiae were desired endpoints. Energies for the 1,064 nm wavelength were 1.3, 2.1, 2.5 ± 0.1, and 2.8 ± 0.2 (mean ± sd) for the first, second, third, and fourth treatments, respectively. For the 532 nm wavelengths, delivered energies were 1.1, 1.3, 1.5, and 1.5 for the first, second, third, and fourth treatments, respectively (Table 2). Post‐treatment care consisted of resuming normal skincare routines.
Table 2.
Average Energies Administered for Each Treatment Are Shown for Each Wavelength (1,064 and 532 nm). Where no Standard Deviation (St.Dev.), Minimum (min.) or Maximum (max.) Are Shown, Every Subject Received the Same Energy for that Treatment. Pain Scores are Also Reported as a Mean on a 0 (None) to 10 (Maximum) Point Scale
| 1,064 nm | 532 nm | |||||||
|---|---|---|---|---|---|---|---|---|
| Parameter | Txl | Tx2 | Tx3 | Tx4 | Txl | Tx2 | Tx3 | Tx4 |
| Energy (mJ/microbeam) | ||||||||
| Mean | 1.3 | 2.1 | 2.5 | 2.8 | 1.1 | 1.3 | 1.5 | 1.5 |
| St. Dev. | 0.1 | 0.2 | ||||||
| Min. | 2.9 | 2.1 | ||||||
| Max. | 2.3 | 2.9 | ||||||
| Pain score | ||||||||
| Mean | 2.1 | 3.7 | 4.2 | 5.2 | 4.7 | 4.7 | 4.4 | 4.3 |
| St. Dev. | 1.7 | 1.9 | 2.3 | 2.2 | 2.4 | 1.4 | 1.9 | 1.8 |
| Min. | 0 | 1 | 0 | 1 | 1 | 3 | 3 | 1 |
| Max. | 7 | 8 | 8 | 8 | 8 | 7 | 8 | 8 |
Post‐treatment Evaluation
Facial photography was performed just prior to treatment and 12 weeks after the fourth, and final, treatment using a commercial system (Visia CR, Canfield Scientific Inc., Fairfield, NJ). Immediate post‐treatment, cross‐polarized photographs were recorded in a representative selection of subjects to record transient post‐treatment erythema, which is highlighted upon cross‐polarization. Parallel polarized images were evaluated to determine treatment effect, at 0° (frontal view), and ±45° (left and right views), because parallel polarization highlights surface structures such as acne scars and rhytides. At the completion of the study, photographs were evaluated in pairs of pre‐ and 12‐week post‐treatment randomized as to left and right panels, by three physician reviewers blinded as to the treatment conditions. For each subject, the reviewers were first asked to identify which image was the baseline photograph and then were asked to rate the degree of improvement using a 10‐point global aesthetic improvement scale (1 = 10%, 2 = 20%, 3 = 30% improvement to 10 = 100% or total clearance). In cases where the reviewer incorrectly identifies a baseline photograph, the assessor's global evaluation would be given a negative score (i.e., a score of 3 would be recorded as a −3).
Subjects assessed their satisfaction with the treatment outcome at the 12‐week follow‐up visit using a 5‐point Likert scale (−2 = Very dissatisfied, −1 = Dissatisfied; 0 = No opinion, 1 = Satisfied, 2 = Very satisfied). Patients ranked their discomfort during treatment using a 0–10 scale (0 = no discomfort; 10 = intolerable pain).
Immediately following each treatment session, purpura, pinpoint bleeding (petechiae), erythema, edema, crusting, and blistering were evaluated by the treating physician using a 4‐point severity scale (0 = absent, 1 = mild, 2 = moderate, and 3 = severe). Hypopigmentation, hyperpigmentation, and scarring were evaluated by comparing cross‐polarized, pre‐treatment images to those taken 12 weeks following the final treatment, by the blinded physician observers. Pigmentary alterations or scarring were rated on a 4‐point scale with: 0 = none, 1 = mild, 2 = moderate, and 3 = severe hyperpigmentation, hypopigmentation, or scarring. Comparison with pre‐treatment images was done to reduce the possibility of any pigmentary alterations or scarring that were present prior to treatment being mistaken for a treatment effect. Subjects kept a diary of post‐treatment effects after the first treatment only.
RESULTS
Clinical Results
At total of 31 subjects were enrolled into the study, of which 27 completed the entire study. All had either rolling or boxcar type acne scars. Nineteen of 21 subjects that were treated with the 1,064 nm wavelength completed the study and consisted of 3 males and 16 females with a mean age of 45 ± 14 years (mean ± sd) and an age range of 23–70 years. Their Fitzpatrick skin types ranged from type II to type V (five had skin type II, seven had type III, five had type IV, and two had type V). Eight of 10 subjects completed treatments and follow‐up visits with the 532 nm wavelength and consisted of one male and seven females with a mean age of 45 ± 18 years with a range of 23–65 years of age. Fitzpatrick Skin Types in this group ranged from skin type II to skin type IV (one subject had type II, four type III, and three had skin type IV).
Blinded reviewers correctly identified the baseline image in 61 of the 81 (75%) image sets (27 subjects × three reviewers). Of the 27 subjects, baseline images of 16 subjects were correctly identified by all three reviewers, while all three reviewers incorrectly identified the baseline image in four subjects, and the remaining seven subjects were mixed among the reviewers (χ2 = 57.2, two‐tail P‐value < 0.0001). Blinded reviewers revealed on a 10‐point scale a mean improvement score of 1.4 (range −4 to 6, 95%CI 0.85–1.9) for all subjects (Fig. 2). No difference was noted in the mean improvement when comparing subjects treated with 1,064 nm to subjects treated with 532 nm (P = ns, 2 tailed unpaired Student's t‐test). After averaging scores from the three blinded reviewers, 22 of 27 (81%) subjects showed some level of improvement, 13 of the 27 (48%) subjects had a mean improvement score of at least 2 (>20%), and 7 of 27 (26%) had a mean improvement score of 3 or better (>30%). The mean improvement score for the 16 subjects whose baseline image was correctly identified by all three blinded reviewers was 2.8, corresponding to a 28% improvement on average in the appearance of acne scars, with the scores ranging from 1 to 6 or 10–60% improvement.
Figure 2.

Parallel‐polarized, digital images taken before (a,c) laser treatment and 3 months following the fourth and final treatment (b,d). The subject pictured in a,b was treated with the 532 nm laser, while the subject shown in c,d was treated with the 1,064 nm wavelength. Parallel‐polarized photography enhances visibility of surface texture over conventional lighting or non‐polarized flash photography.
Subjects reported high satisfaction rates with the treatment results. For subjects treated with the 1,064 nm laser, 15 of 19 subjects were satisfied or very satisfied (nine very satisfied, six satisfied, two no opinion, two dissatisfied) with their treatment results. Of the eight subjects treated with the 532 nm, all were satisfied or very satisfied (four very satisfied, four satisfied).
Side Effects
Discomfort scores ranged from none to mild with a mean discomfort score of 3.8 ± 2.3 for the 1,064 nm laser, and 4.3 ± 1.8 for 532 nm laser (Table 2). Immediate post‐treatment responses were limited to mild‐to‐moderate erythema (100% for 1,064 nm, 100% for 532 nm), mild to moderate edema (95% for 1,064 nm, 97% for 532 nm), mild to moderate petechiae (50% for 1,064 nm, 38% for 532 nm), mild purpura (17% for 1,064 nm, 0% for 532 nm), and mild pruritus (3% for 1,064 nm, 0% for 532 nm). All post‐treatment responses resolved on their own with erythema and edema clearing a few hours after treatment, and petechiae typically clearing a few days following treatment by subject report. No severe or unexpected adverse events were noted during the study.
According to subjects’ diaries, 17 of 19 subjects treated with 1,064 nm reported that their erythema resolved 1 day after treatment while three of eight subjects treated with 532 nm reported resolution of erythema 1 day after treatment, with erythema persisting for 2 days in one, 3 days in five, and up to 4 days in one. All 19 subjects treated with the 1,064 nm laser reported that their edema resolved on the day of treatment; while three of eight subjects treated with the 532 nm laser reported resolution of edema 1 day after treatment. In the remaining five subjects, edema resolved by day 4. All 19 subjects treated with 1,064 nm reported no or mild discomfort only on the day of treatment; while six of eight subjects treated with 532 nm reported no or mild discomfort only on the day of treatment, with one subject reporting mild discomfort persisting 1 day after treatment and another for 2 days after treatment.
Blinded evaluation of photographs, comparing pre‐treatment images to the 12‐week post‐treatment follow‐up images revealed no pigmentary alterations such as post‐treatment hypopigmentation or hyperpigmentation.
DISCUSSION
This study demonstrates that this picosecond‐domain, 1,064 and 532 nm, Nd:YAG laser, when used with a holographic beam‐splitter, is safe and effective for the treatment of facial acne scars. As evaluated by blinded observers rating parallel‐polarized pre‐ and post‐treatment photographs, improvement was noted in 81% of subjects, with improvement ranging up to 60%. Subject satisfaction was very high with 23 of 27 subjects reporting they were satisfied or very satisfied with the treatments. The study was open to all Fitzpatrick skin types, with enrolled subjects having skin types ranging from II–V. In the current study, 10 of the 27, or 37%, of the subjects had skin types IV–V. No pigmentary alterations were noted in the current study, however there were no subjects in this study with skin type VI and only two with skin type V treated with the 1,064 nm wavelength; thus, no conclusions regarding treatment of skin types V–VI can be drawn from this current study. However, further clinical experience with this laser and studies with other picosecond‐domain lasers and nanosecond‐domain fractionated devices used at 1,064 nm suggest that fractionated picosecond‐domain devices may represent a potential benefit over earlier ablative and non‐ablative fractionated lasers for treating acne scarring in darker skin types 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 29, 30, 31. The first non‐fractionated carbon dioxide (CO2) lasers proved highly efficacious for improving rhytides and acne scarring; however, the side‐effect profiles were much higher with non‐fractionated CO2 lasers 29, 30, 31 than with fractionated CO2 lasers 18, 32, 33, or the even safer non‐ablative fractionated lasers 20, 21, 22, 24, 25. Non‐fractionated CO2 lasers produced outstanding results for improving rhytides, and quite good results for improving acne scarring, and now are the gold‐standard to which every subsequent laser used for these indications is compared 29, 30, 31. But the side effects from these lasers, many of which, such as significant hyperpigmentation, and delayed permanent hypopigmentation, were identified, often months following treatment 30. Fractionated CO2 lasers delivered slightly less efficacy when treating photodamage, but with the benefit of greatly reduced long‐ and short‐term side effects 29, 30.
Because the biology and physiology of acne scarring is dramatically different than that of wrinkles and photodamage, one would expect that these conditions would respond quite differently to laser treatment. Many clinicians prefer non‐alative fractional lasers delivered with a series of treatments for the treatment of acne scarring, over a single fractionated CO2 laser treatment, due to greater efficacy of the former when treating acne scarring, as opposed to photodamage. Non‐ablative 1,550, 1,440, and 1,320 nm fractionated lasers were among the first non‐ablative devices used for treating photodamage and acne scarring 20, 21, 22, 24, 25. Experienced clinicians use the 1,550 nm fractionated laser to treat patients with skin types I–V without causing any post‐treatment hyperpigmentation 24, 25, although only 7 of the 53 subjects in one large study had skin type IV or V 25. Less experienced physicians, or those operating in warm, sunny climates treating patients with Fitzpatrick skin types IV–VI, or lighter skin types who have a tan, will likely observe a great incidence of post‐treatment hyperpigmentation when using these devices. Consensus guidelines for treatment with the erbium‐doped yttrium aluminum garnet (Er:YAG) 1,550 nm fiber laser suggested that only the most experienced laser surgeons should treat skin type VI patients with these lasers due to the high risk of hyperpigmentation 22. Others reported a significant incidence of hyperpigmentation when treating skin types IV–VI with the 1,550 nm, Er:YAG fiber laser 21. In the current study, 11 of 27 subjects completing the study, or 41%, had Fitzpatrick skin type IV or V, and no subject experienced hyperpigmentation. Current results and ongoing clinical experience from others in the field suggest that the risk of post‐treatment hyperpigmentation is quite low with fractionated, picosecond‐domain lasers. Future peer‐reviewed studies including those with skin type VI are necessary to further clarify the safety of these devices when treating skin of color.
In our current study, no significant difference was observed when comparing mean improvement scores between subjects treated with the 1,064 and 532 nm fractionated lasers. One reason for the lack of any difference in treatment effect may be the fact that the treatment parameters for each wavelength were optimized to give the same clinical endpoint of mild‐to‐moderate post‐treatment erythema and/or petechiae. The maximum energies delivered were 2.9 and 1.5 mJ/microbeam for 1,064 and 532 nm, respectively; while the mean energies delivered over all treatments were 2.2 ± 0.6 and 1.4 ± 0.2 mJ/microbeam, respectively. This suggests that lower energies are needed at 532 nm as compared to 1,064 nm to reach the same clinical endpoints, most likely due to the higher absorption by melanin at 532 nm versus 1,064 nm. The extremely high peak powers and small 150 μm‐diameter microbeams confine the laser energy to small areas and superficial depths within the epidermis and superficial dermis, so dramatic differences in the depth of penetration that might normally occur when treating with larger beam diameters using these two different wavelengths are not noted with these picosecond‐domain fractionated lasers. Since both devices are quite similar, further work to tease out potential advantages, disadvantages, and synergies will add to our ability to better utilize this versatile device.
A 755‐nm picosecond‐domain laser with a fractionating micro‐lens array was used previously for the treatment of facial acne scars 7. This device focuses much of the energy to small treatment zones, but also delivers background energy to the entire treatment field. The treatment energy for that study was fixed at 0.71 mJ/microbeam, with 17 subjects receiving six treatments spaced 4–8 weeks apart. Improvement was evaluated 3 months after six treatments, with an improvement score of 1.4 using a 4‐point improvement scale (0 = 0–25%, 1 = 26–50%, 2 = 51–75%, and 3 = 76–100%) 7. This roughly equates to a 35% mean improvement in the appearance of acne scars at 3 months following six treatments and delivering an average of 3,000 pulses per treatment. In the current study, we report a 14% mean improvement at 3 months after four treatments and an average of 1,000 pulses per treatment. In the current study blinded investigators first identified the baseline image, and then graded the percent improvement. If the wrong baseline image was selected, then the improvement score was penalized by setting to its negative value, in effect lowering the mean improvement. It is unclear if the above study used this methodology of choosing the baseline image, and subtracting for a negative result. In addition, a 4‐point scale makes the minimum increment of improvement 25–50%, with the first choice indicating anywhere from no improvement all the way to 25% improvement, and thus not distinguishing between no change at all and a 25% improvement. Thus, an image getting a score of 0 could have had no change or even a 25% change, making this scale too coarse to tease incremental improvements less than 25%. The weighted average of all 0 scores would be a 12.5% improvement, and this is true even if all the images being evaluated in a study were the exact same image. Thus, direct comparisons between such a 4‐point scale and the 11‐point scale used in the current study are not possible. The disadvantages of such a rough scale would be overestimating minimal or even no change, while the disadvantages of a more granular scale used in the current study would be going beyond the resolution capabilities of the reviewers.
A 755 nm picosecond‐domain laser with a fractionating micro‐lens array was also used previously for the treatment of facial wrinkles 9. Once again, the treatment energy was fixed at 0.71 mJ/microbeam. For this study, 17 subjects received four treatments spaced 3 weeks apart. Improvement was assessed by reporting that baseline photos were correctly identified in 69% of subjects 3‐month following treatment, which, despite evaluating a completely different condition 9, is similar to the 75% correctly identified in this current study of acne scar treatment.
Potential limitations of this current study include a single 3‐month follow‐up evaluation and the use of parallel polarized photography as the study endpoint. The longevity of improvement cannot be assessed from the short 3‐month follow‐up period. It also possible because tissue remodeling occurs over many months that further improvement could occur over a longer follow‐up period. The use of parallel polarized photography was chosen as it better accentuates skin surface structures enabling better contrast for the blinded reviewers when grading the photographs, however, non‐polarized flash photography could have been used. In reality, one looks at a subject in three dimensions with binocular vision and natural lighting, so any photograpy of the subject is an alteration of real‐life viewing.
The results of this study and a previous one by Brauer et al. 7 offer strong evidence that treatment with an array of highly focused picosecond‐domain laser beams, with intensities sufficient to cause LIOB in tissue, improves acne scaring. The use of picosecond‐domain pulses delivers clinical benefits at lower fluences and energies than would be required at longer pulse‐durations, and may offer qualitatively different tissue effects than earlier‐generation lasers. Future studies investigating combinations of the 1,064 and 532 nm picosecond‐domain fractionated wavelengths, as well as larger trials with skin types V and VI should increase the ways the device is used, and the conditions it is used to treat.
ACKNOWLEDGMENTS
Dr. Bernstein is a consultant for Syneron/Candela. Drs. Bhawalkar and Schomacker were employees of Syneron/Candela at the time this work was done. Research funding for this project and equipment loan were provided by Syneron/Candela.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1. Aron‐Rosa D, Aron JJ, Griesemmann J, Thyzel R. Use of the neodymium YAG laser to open the posterior capsule after lens implant surgery: A preliminary report. J Am Intraocul Implant Soc 1980; 6:352–354. [DOI] [PubMed] [Google Scholar]
- 2. Aron‐Rosa D. Use of a pulsed neodymium‐YAG laser for anterior capsulotomy before extracapsular extraction. J Am Intraocul Implant Soc 1980; 7:332–333. [DOI] [PubMed] [Google Scholar]
- 3. Steinert RF, Puliafito CA. The Nd:YAG Laser in Ophthalmology: Principles and Clinical Applications of Photodisruption. Philadelphia: W.B. Saunders; 1985. [Google Scholar]
- 4. Loertscher H. Laser‐induced breakdown for ophthalmic applications In: Trokel S, editor. YAG Laser Ophthalmic Microsurgery. Norwalk, CT: Appleton‐Century‐Crofts; 1983. pp 39–66. [Google Scholar]
- 5. Habbema L, Verhagen R, Van Hal R, Liu Y, Varghese B. Minimally invasive non‐thermal laser technology using laser‐induced optical breakdown for skin rejuvenation. J Biophotonics 2012; 5(2):194–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Habbema L, Verhagen R, Van Hal R, Liu Y, Varghese B. Efficacy of minimally invasive nonthermal laser‐induced optical breakdown technology for skin rejuvenation. Lasers Med Sci 2013; 28:935–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brauer JA, Kazlouskaya V, Alabdulrazzaq H, et al. Use of a picosecond pulse duration laser with specialized optic for the treatment of facial acne scarring. JAMA Dermatol 2015; 151:278–284. [DOI] [PubMed] [Google Scholar]
- 8. Weiss RA, McDaniel DH, Weiss MA, Mahoney AM, Beasley KL, Halvorson CR. Safety and efficacy of a novel diffractive lens array using a picosecond 755nm alexandrite laser for treatment of wrinkles. Lasers Surg Med 2017; 49:40–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Khetarpal S, Desai S, Kruter L, et al. Picosecond laser with specialized optic for facial rejuvenation using a compressed treatment interval. Lasers Surg Med 2016; 48:723–726. [DOI] [PubMed] [Google Scholar]
- 10. Ross V, Naseef G, Lin G, et al. Comparison of responses of tattoos to picosecond and nanosecond Q‐switched neodymium: YAG lasers. Arch Dermatol 1998; 134:167–171. [DOI] [PubMed] [Google Scholar]
- 11. Herd RM, Alora MB, Smoller B, Arndt KA, Dover JS. A clinical and histologic prospective controlled comparative study of the picosecond titanium:sapphire (795nm) laser versus the Q‐switched alexandrite (752nm) laser for removing tattoo pigment. J Am Acad Dermatol 1999; 40:603–606. [DOI] [PubMed] [Google Scholar]
- 12. Izikson L, Farinelli W, Sakamoto F, Tannous Z, Anderson RR. Safety and effectiveness of black tattoo clearance in a pig model after a single treatment with a novel 758nm 500 picosecond laser: A pilot study. Lasers Surg Med 2010; 42:640–646. [DOI] [PubMed] [Google Scholar]
- 13. Brauer JA, Reddy KK, Anolik R, et al. Successful and rapid treatment of blue and green tattoo pigment with a novel picosecond laser. Arch Dermatol 2012; 148:820–823. [DOI] [PubMed] [Google Scholar]
- 14. Bernstein EF, Schomacker KT, Basilavecchio LD, Plugis JM, Bhawalkar JD. A novel dual‐wavelength, Nd:YAG, picosecond‐domain laser safely and effectively removes multicolor tattoos. Lasers Surg Med 2015; 47:542–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Balu M, Lentsch G, Korta DZ, et al. In vivo multiphoton‐microscopy of picosecond‐laser induced optical breakdown in human skin. Laser Surg Med 2017; 49(6):555–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tanghetti EA, Tartar DM. Comparison of the cutaneous thermal signatures over twenty‐four hours with a picosecond alexandrite laser using a flat or fractional optic. J Drugs Dermatol 2016; 15:1347–1352. [PubMed] [Google Scholar]
- 17. Tanghetti EA. The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med 2016; 48:646–652. [DOI] [PubMed] [Google Scholar]
- 18. Hunzeker CM, Weiss ET, Geronemus RG. Fractionated CO2 laser resurfacing: our experience with more than 2000 treatments. Aesthetic Surg J 2009; 29:317–322. [DOI] [PubMed] [Google Scholar]
- 19. Tierney EP, Hanke CW, Petersen J, Bartley T, Eckert JR, McCutchen C. Clinical and echographic analysis of ablative fractionated carbon dioxide laser in the treatment of photodamaged facial skin. Dermatol Surg 2010; 36:2009–2211. [DOI] [PubMed] [Google Scholar]
- 20. Bernstein EF. A multiplexed 1,440 and 1,320 nm laser for treatment of chronic photodamage. J Drugs Dermatol 2011; 10:1266–1270. [PubMed] [Google Scholar]
- 21. Mahmoud BH, Srivastava D, Janiga JJ, Yang JJ, Lim HW, Ozog DM. Safety and efficacy of erbium‐doped yttrium aluminum garnet fractionated laser for treatment of acne scars in type IV to VI skin. Dermatol Surg 2010; 36:602–609. [DOI] [PubMed] [Google Scholar]
- 22. Sherling M, Friedman PM, Adrian R, et al. Consensus recommendations on the use of an erbium‐doped 1,550‐nm fractionated laser and its applications in dermatologic laser surgery. Dermatol Surg 2010; 36:461–469. [DOI] [PubMed] [Google Scholar]
- 23. Manstein D, Herron GS, Sink RK, Tanner H, Anderson RR. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med 2004; 34:426–438. [DOI] [PubMed] [Google Scholar]
- 24. Chrastil B, Glaich AS, Goldberg LH, Friedman PM. Second‐generation 1,550‐nm fractional photothermolysis for the treatment of acne scars. Dermatol Surg 2008; 34:1327–1332. [DOI] [PubMed] [Google Scholar]
- 25. Alster TS, Tanzi EL, Lazarus M. The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg 2007; 33:295–299. [DOI] [PubMed] [Google Scholar]
- 26. Cohen BE, Brauer JA, Geronemus RG. Acne scarring: A review of available therapeutic lasers. Lasers Surg Med 2016; 48:95–115. [DOI] [PubMed] [Google Scholar]
- 27. Wat H, Wu DC, Chan HH. Fractional resurfacing in the Asian patient: Current state of the art. Lasers Surg Med 2017; 49:45–59. [DOI] [PubMed] [Google Scholar]
- 28. Min S, Park SY, Moon J, Kwon HH, Yoon JY, Suh DH. Comparison between Er;YAG laser and bipolar radiofrequency combined with infrared diode laser for the treatment of acne scars: Differential expression of fibrogenetic biomolecules may be associated with differences between ablative and non‐ablative laser treatment. Lasers Surg Med 2017; 49:341–347. [DOI] [PubMed] [Google Scholar]
- 29. Alster TS, Tanzi EL. Resurfacing of atrophic facial acne scars with a high‐energy, pulsed carbon dioxide laser. Dermatol Surg 1996; 22:151–154. [DOI] [PubMed] [Google Scholar]
- 30. Bernstein LJ, Kauvar AN, Grossman MC, Geronemus RG. The short‐ and long‐term side effects of carbon dioxide laser resurfacing. Dermatol Surg 1997; 23:519–525. [DOI] [PubMed] [Google Scholar]
- 31. Chan NP, Ho SG, Yeung CK, Chan HH. Fractional ablative carbon dioxide laser resurfacing and acne scars in Asians. Lasers Surg Med 2010; 42:615–634. [DOI] [PubMed] [Google Scholar]
- 32. Chapas AM, Brightman L, Sukai S, et al. Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med 2008; 40:381–386. [DOI] [PubMed] [Google Scholar]
- 33. Fitzpatrick RE, Goldman MP, Satur NM, Tope WD. Pulsed carbon dioxide laser resurfacing of photo‐aged facial skin. Arch Dermatol 1996; 132:395–402. [PubMed] [Google Scholar]


