Introduction
Hip and knee osteoarthritis (OA) are considered the most common joint disorders, affecting at least 250 million individuals worldwide, who experience pain, reduced physical function, and lower‐leg disability 1, 2. OA is an extreme burden on society, through the costs related to disease treatment and productivity loss 1. Furthermore, this burden will increase during the next decades because of the aging population and obesity epidemic 1.
Due to their walking disability, individuals with OA are more prone to mortality, for instance from cardiovascular diseases 3. This disability is reflected in their sedentary and inactive lifestyle, as only a part of this population meets current guidelines for physical activity in daily life 3, 4. Sedentary behavior impairs a person's health by contributing to the onset and progression of chronic diseases (e.g., OA and cardiovascular diseases) 4, 5, 6, 7. Since reducing sedentary behavior and increasing physical activity are known to prevent further functional loss and reduce mortality and pain in individuals with hip and knee OA 3, 4, 8, 9, current treatment interventions incorporate lifestyle modifications, thereby improving physical activity and well‐being 10. Consequently, a reliable assessment of physical activity behavior is necessary to accurately evaluate treatment efficacy 11.
According to the World Health Organization, physical function can be subdivided into capacity, i.e., the capability to perform a specific task within a controlled environment, and performance, which is defined as “activities performed by an individual on a day‐to‐day basis in the context of their own life” 12. Activity monitoring, which focuses on a person's performance in daily life, can be accomplished with a multitude of methods, each with its own advantages and disadvantages 13. Subjective methods, e.g., questionnaires, are cheap and easily applicable in large cohorts but lack objectivity and are prone to bias and inconsistencies 14, 15. The gold standard methods, i.e., doubly labeled water and indirect calorimetry, are not always applicable, as they are laboratory‐based, expensive, and not able to distinguish various postures or types of physical activity 13, 15, 16. Especially in patients with knee‐ and hip‐related impairments, alterations in activities involving the lower legs (e.g., sit‐to‐stand transfers, walking, and cycling) could provide useful insights of treatment efficacy. Activity monitors are feasible for objectively assessing physical activity in daily life 15. Furthermore, they have the potential to measure the 4 dimensions of physical activity: frequency (how many single events per time period), intensity (energy expenditure of a single event), time (duration of a single event), and type (of activity) 5, 15. Examining all dimensions of physical activity rather than only a single component could be worthwhile, since the different components are related to varying diseases or disease sites 11, 17.
Existing body‐mounted activity monitors use parameters such as heart rate or body motion to assess physical activity and/or energy expenditure 5. Furthermore, multiple sensor systems are available, employing several sensors simultaneously or combining technologies 9, 18. Pedometers are fairly simple and low‐cost devices that detect the steps taken during daily life (which are considered to be the main contribution to lower‐leg activities) but are unable to register other types of activities (e.g., cycling) or distinguish different postures 9, 11, 13.
Accelerometers are relatively unobtrusive devices that are able to detect the magnitude and frequency of acceleration in 1 or multiple planes. Acceleration counts can be used to determine energy expenditure and categorize activities into different levels 9, 11. Novel devices measuring the gravitational field can be used to distinguish body postures and to accurately distinguish sedentary behavior 19. Such information is of high relevance within hip and knee OA research due to the patients' susceptibility to reduced activity levels and a more sedentary lifestyle caused by pain and depression symptoms 4. Furthermore, acceleration signals can be used for activity classification, thus improving the information on activity behavior during daily life 19. A current limitation of accelerometers is their inability to measure all activities with equal accuracy 14, 20.
Nevertheless, these activity assessment tools seem to offer the best balance between feasibility and utility for clinical monitoring of free‐living behavior in patients. A wide range of monitors is currently available, and selecting a device for scientific applications often depends on numerous factors, such as the study objective and the monitor's applicability and reliability 11, 14, 16. Reviews have been written on various topics related to physical activity monitors (e.g., types, advantages, and best practices) 9, 11, 14, 16, but little attention has been given to the variety of devices available.
Therefore, this review aims to provide an up‐to‐date overview of physical activity monitors and their specifications, used within hip and knee OA research. By using the information provided in this review, informed decisions regarding the most appropriate activity monitor for specific research goals can be made.
Materials and methods
A review was conducted to identify activity monitors used in hip and knee OA research. Studies were included when 1) the participants were diagnosed with hip or knee OA, either clinically (e.g., American College of Rheumatology guidelines 21, 22), radiographically (e.g., Kellgren/Lawrence grade ≥2), by a physician or when patients had received surgery (i.e., osteotomy, arthroscopy, or partial or total joint arthroplasty) due to OA, 2) activity monitors assessed habitual physical activity during daily life for at least 3 days (the minimal requirement for gathering physical activity data) 12, and 3) texts were available in English, Spanish, German, or Dutch. Articles were excluded if the device was used only to determine parameters of gait (e.g., step length, gait symmetry, or peak tibial acceleration), the device was used as an assistive device during surgery, the article described study protocols or abstracts of studies that were already included in this review, the article described animal studies, or the employed activity monitor was not specified.
The following databases were searched from January 2000 until January 2016: Medline via PubMed, Embase via OVID and Scopus. Due to recent technologic advances, we considered it unnecessary to include older articles. Included reviews and reference lists were screened for further devices and references. The search strategy comprised medical subject headings (i.e., MeSH) terms and text words related to “knee osteoarthritis,” “hip osteoarthritis,” “activity monitor,” “heart rate monitor,” “pedometer,” and “accelerometer” (see Supplementary Appendix A, available on the Arthritis Care & Research web site at http://onlinelibrary.wiley.com/doi/10.1002/acr.23170/abstract, for the complete Medline search strategy). When necessary, the Medline strategy was adjusted to apply it to other databases.
The device's name and manufacturer were obtained for each reference. Relevant specifications were identified for each device by extracting information from the manufacturers' websites, device manuals, and literature. In general, these specifications regarded the monitor's hardware (e.g., incorporated technology, battery, and storage capacity), the financial burden (expenses for a sensor and software), and the measurement abilities (e.g., energy expenditure, step detection, and posture allocation).
If the monitor that was originally extracted from the literature search was no longer commercially available or a successive device had been developed in the meantime, the company's next generation device was included. If no direct successive device was available, the manufacturer's current, most advanced research‐grade monitor was included in this review (decisions were reached after discussion between MS, MB, and DR). To ensure accuracy of the device's specifications, every manufacturer was requested to reconfirm the correctness of the provided specifications.
Results
The initial search resulted in 369 articles, of which 181 duplicates were removed. An additional 70 articles were omitted for further analysis due to the inclusion and exclusion criteria. Finally, the search resulted in 118 eligible articles, in which activity monitors were used to determine physical activity during daily life in knee and/or hip OA patients (Figure 1).
Figure 1.
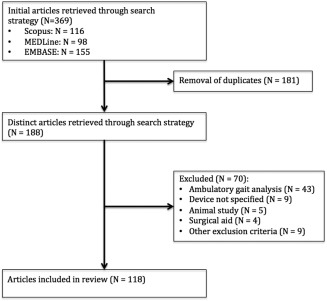
Flowchart describing identified and included articles.
There were 15 different devices identified from the articles, with the majority (n = 10) containing accelerometers. The remaining monitors were defined as pedometers (n = 5). However, only 14 devices are presented in this article, since the Vitaport Activity Monitor is not commercially available anymore. The technical specifications and analytical parameters of the remaining 14 devices are summarized and compared in Tables 1 and 2.
Table 1.
Overview of hardware specifications per activity monitora
| Model (manufacturer) | Technology | Sampling rate, Hz | Weight, grams | Dimensions, mm | Battery capacity | Storage capacity | Water resistant | Data transfer | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Length | Height | Width | Days | MB | |||||||
| Actical (Koninklijke Philips) | 3D accelerometer | 32 | 22 | 29 | 37 | 11 | 12 days | NS | 32 | ✓ | Docking station |
| ActivPal3 (PAL Technologies) | 3D accelerometer | 20 | 15 | 35 | 53 | 7 | 10 days | NS | 16 | Docking station | |
| AX3 (Axivity) | 3D accelerometer, temperature sensor, light sensor | 13–3,200 | 11 | 23 | 33 | 8 | 14 days | NS | 512 | ✓ | USB |
| Dynaport MoveMonitor (McRoberts) | 3D accelerometer, 3D magnetometer, temperature sensor, barometer | 50–200 | 55 | 107 | 58 | 12 | 14 days | NS | 1,000 | NS | USB |
| FitBit Zip (Fitbit) | 3D accelerometer | Prop. | 8 | 28 | 36 | 10 | 4–6 months | 7 | NS | Bluetooth | |
| IDEEA 3 (Minisun) | 3D accelerometer | 64 | Sensors: 2 Rec.: 59 |
18 70 |
15 54 |
3 17 |
3 days | 7 | 2,000 | NS | USB |
| Lifecorder EX (Suzuken) | accelerometer | NS | 60 | 73 | 42 | 28 | 5 months | 200 | NS | USB | |
| Polar Loop 2 (Polar Electro) | 3D accelerometer | NS | 38 | 11 | – | 20 | 8 days | 12 | 4 | ✓ | USB, Bluetooth |
| RT6 (Stayhealthy) | 3D accelerometer, 3D gyroscope | 5–20 | 51 | 51 | 51 | 13 | 2–14 days | NS | 32 | USB | |
| SenseWear Mini (Bodymedia) | 3D accelerometer, heat flux, skin temperature, galvanic skin response | 32 | 45 | 55 | 62 | 13 | 5–7 days | 28 | NS | USB | |
| Stepwatch Activity Monitor (Modus Health) | 2D accelerometer | 128 | 38 | 75 | 50 | 20 | 7 years | 50 | 0.032 | Docking station | |
| SW200 Digiwalker (YAMAX Health & Sports) | Pedometer | NA | 21 | 50 | 38 | 14 | 3 years | NS | NS | NA | |
| Walking Style Pro 2.0 (Omron Healthcare Europe) | 3D accelerometer | NS | 27 | 78 | 34 | 12 | 6 months | 21 | NS | USB | |
| wGT3X‐BT (Actigraph) | 3D accelerometer, ambient light sensor | 30–100 | 19 | 46 | 33 | 15 | 25 days | 120 | 2,000 | ✓ | USB, Bluetooth |
Hz = herz; MB = megabytes; NS = not specified; ✓ = yes; Prop. = proprietary; Rec. = recorder; NA = not applicable.
Table 2.
Overview of measurement abilities, wear position, feedback, and price per activity monitora
| Model | Step detection | EE | PA intensity | Postures and movements | Sleep | Wear position | Feedback | Raw data | Price, €b | Refs. | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lie down | Sit | Stand | Walk | Cycle | Run | Climb stairs | AM | Starter package | |||||||||
| Actical | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | – | Wrist, ankle, hip | – | ✓ | NS | NS | 5,12,18,20 |
| ActivPal3 | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | – | – | – | – | Thigh (anterior) | – | ✓ | 426 | 1,059 | 3,5,18 |
| AX3 | – | ✓ | ✓ | – | – | – | – | – | – | – | – | Wrist | – | ✓ | 128 | NA | 23 |
| Dynaport MoveMonitor | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | ✓ | Middle lower‐back | – | ✓ | 695 | 1,095 | 18 |
| FitBit Zip | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | – | Hip, pocket, bra | ✓ | – | 60 | NA | – |
| IDEEA 3 | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | Sensors: sternum 1, thigh 2, ankle 2, foot sole 2 Recorder: hip | – | ✓ | 4,045 | 6,296 | 5,9,18,20 |
| Lifecorder EX | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | – | Hip | ✓ | – | 266 | 536 | 3,5,18 |
| Polar Loop 2 | ✓ | ✓ | ✓ | – | – | – | – | – | – | – | ✓ | Wrist | ✓ | – | 120 | NA | 18 |
| RT6 | – | ✓ | ✓ | – | – | – | – | – | – | – | – | Hip | ✓ | ✓ | 248 | NA | 3,5,12,18,20 |
| SenseWear Mini | ✓ | ✓ | ✓ | ✓ | – | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | Upper arm (posterior) | – | ✓ | NS | NS | 5,12,18 |
| Stepwatch Activity Monitor | ✓ | – | ✓ | – | – | – | – | – | – | – | – | Ankle | – | – | 473 | 1,323 | 3,5,12 |
| SW200 Digiwalker | ✓ | – | – | – | – | – | – | – | – | – | – | Hip | ✓ | – | 25 | NA | 3 |
| Walking Style Pro 2.0 | ✓ | ✓ | – | – | – | – | – | – | – | – | – | Hip, pocket, bag | ✓ | – | 50 | NA | 5 |
| wGT3X‐BT | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | – | – | – | – | ✓ | Wrist, hip, ankle, thigh | – | ✓ | 203 | 1,728 | 3,5,12,18,20 |
Starter package includes monitor, software, and docking station (if applicable). EE = energy expenditure; PA = physical activity; AM = activity monitor; Refs. = references; ✓ = yes; NS = not specified; NA = not applicable.
Price was determined and converted with current exchange rate in May, 2016.
Overall, the hardware features of the devices vary considerably in weight (mean 33 grams, range 8–61 grams) and dimensions (mean 29 cm3, range 1–83 cm3). With regard to battery life, the majority (n = 11) can assess physical activity for 1 week or more. The battery can be recharged in 8 devices, whereas for the remainder the batteries need to be replaced once depleted (all by the consumer, except for the Stepwatch Activity Monitor). Furthermore, most of the monitors connect to a computer over USB connections (n = 11), either through a docking station or through a direct connection. Only a few (n = 3) can also transfer data via Bluetooth. In general, the monitors are not waterproof (Table 1).
The financial burden varies widely between the devices, ranging from €25 to €700 (mean €599), excluding the most expensive device (Intelligent Device for Energy Expenditure and Activity 3 [IDEEA 3] at €4,500). Also, the need for and cost of required software varies greatly between the devices. Nine of the monitors have 1 distinct, recommended wear position, usually at the hip, thigh, ankle, or wrist. Every manufacturer provides a user data interface, with the most common measurement outcomes being energy expenditure and step detection (n = 11). Many of the manufacturers provide summarized data output on at least a daily basis (n = 8). Additionally, 8 monitors offer the option of extracting raw data (Table 2). Every sensor is compatible with the Windows operating system, whereas only 4 are compatible with an OS X operating system. Only the IDEEA 3 has previously been validated in OA patients. The vast majority of the activity monitors have been validated solely in healthy populations, without walking impairments potentially affecting gait characteristics (data not shown). Finally, references describing additional features of the monitor are shown in Table 2.
Discussion
This review provides an extensive overview consisting of 14 currently available monitors, along with their hardware specifications and measuring capabilities. The information on the devices should enable the scientific community to compare the available options and decide which device would be most appropriate for their specific research goal, ultimately improving the assessment of physical activity.
When choosing an activity monitor, several considerations should be taken into account. Some devices are allegedly able to measure various activities, whereas others can only measure a single category, yet this difference does not necessarily imply the superiority of 1 device over the others. Devices are generally validated with highly heterogeneous protocols, in different populations, and against varying criteria methods 18. The validation of devices solely in healthy participants could lead to an erroneous reflection of the device's true validity for lower‐leg OA patients, as knee and hip OA lead to abnormalities in gait dynamics and increased energy expenditure during gait compared to healthy individuals 23, 24.
Furthermore, validation studies are often conducted in a laboratory setting, which represents a showcase situation deviating from free‐living conditions, thereby confounding gait parameters compared to habitual gait performance 25. Therefore, activity monitors measuring a single category but validated in OA patients could be a superior option to a device able to measure various activities, validated only in healthy young participants.
Accurate detection of human motion is dependent on various factors, among them the sampling rate. To capture the full range of human movement, the sampling frequency should be twice as high as the highest movement frequency performed, which in healthy individuals varies from 8 Hz (lower body) up to 25 Hz in upper body activities 26. A lower frequency rate might be sufficient for measurements with OA patients, due to their functional impairment and slower movements 23, 24, 27. A higher sampling rate, however, more quickly depletes storage capacity and battery life, increasing the demand on a sensor's hardware 28. While some studies suggest assessing physical activity behavior for 3 days, others recommend a minimum of 7 days, providing additional insight into differences between weekdays and weekends 12, 14. This information could describe a patient's behavioral pattern in more detail, as differences occur between weekdays and weekends 29. However, most devices included here allow for 7 or more measurement days with at least 25 Hz.
Accurately measuring sedentary behavior is of critical importance, as such behavior is shown to detrimentally affect health 5, 6. However, particular devices rely on surrogate measures to detect sedentary behavior, (e.g., threshold of activity counts). Such measures may incorporate light‐intensity activities (e.g., standing) as sedentary, ultimately leading to erroneous measurements 30. Furthermore, due to distinct monitoring protocols and data reduction strategies, sedentary behavior measured with differing monitors should be compared carefully 6. Since hip and knee OA commonly result in reduced sleep duration and quality, being able to measure these parameters objectively could be a significant addition to the measurement protocol 31.
Monitors are often worn at different locations, and the wear position is assumed to be trivial at a group level 11. Participants could be less compliant to wear a monitor due to aesthetic motives, even though commercially available wrist‐worn activity monitors, such as the Fitbit and JawboneUP, have become increasingly popular 20, 32. This elevated acceptance towards popular, commercially available activity monitors obviously depends on the weight, dimensions, and appearance of a monitor. With regard to measurement options, one should recognize the effect of the wear position on a device's measuring abilities (e.g., the Actigraph wGT3X‐BT can only distinguish standing from sitting if it is worn on the hip).
Especially in accelerometers, an important feature might be the possibility to extract raw data that can be analyzed independent of the manufacturers' algorithms, if these are specified insufficiently for specific needs and study aims. Moreover, raw data can be re‐analyzed retrospectively if new algorithms are developed.
The sensor's prices are presented to provide an estimate, but might vary slightly due to country‐specific taxes, order size, or conversion rates. The sensors' prices vary from less than €50 for relatively simple pedometers, to €6,300 for a portable gait‐analysis system. A pedometer might be sufficient to get an overall idea of physical activity in a specific population, especially since walking is considered the main contributor to lower‐leg activities, but devices with further analytical options might be worth the higher costs 33.
To summarize, a large variety of specifications and features should be considered, ultimately leading to a well‐informed choice of the most appropriate monitor. Themes such as whether a monitor has been sufficiently validated in the target population (as activity assessment can be hampered by certain patient characteristics [27]), whether a device should be able to measure for at least 7 days (as differences in activity behavior have been shown in knee OA patients between weekdays and weekends [29]), how much a device can maximally cost, and what size and weight are acceptable with regard to compliance (as compliance with a monitoring protocol often remains challenging [20]), should be taken into consideration.
The description of every single activity monitor currently available on the market is a difficult task due to the rapid progression of technical developments within this field. Therefore, the monitors mentioned in this review will not encompass the full scale of available devices, both research‐grade and consumer available devices. This review consequently focused only on devices used within knee and hip OA research, as these diseases affect at least 250 million people worldwide 2.
Second, this review has not addressed the validity of the described activity monitors. Clearly, a device's validity should be thoroughly examined beforehand. Using a valid and reliable monitor improves study results, and therefore, one should assess whether and how a device has been validated.
Finally, we were unable to retrieve all specifications and/or related references for each device due to various reasons (Tables 1 and 2). Probably, some of the specifications were proprietary and therefore unavailable to the public, whereas other features were simply not applicable or specified by the manufacturer. We were able, however, to retrieve most specifications, in part by contacting the manufacturers.
The choice for the most appropriate monitor requires weighing specific features and limitations of every device, since the assessment of all domains of physical activity with 1 single device is arguably impossible. A well‐defined study objective as well as issues such as the measurement duration and financial costs should be taken into consideration prior to the device selection, as such a procedure will optimize the choice for an activity monitor. This review has provided a detailed list of currently available devices with a broad spectrum of features, enabling the scientific community to select the most appropriate activity monitor, thereby hopefully improving the assessment of physical activity in hip and knee OA research.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Mr. Sliepen had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Sliepen, Rosenbaum.
Acquisition of data
Sliepen, Brandes.
Analysis and interpretation of data
Sliepen, Brandes.
Supporting information
Supplementary Appendix A
ACKNOWLEDGMENTS
The authors thank Gregory Welk, PhD, for his valuable feedback on the review, and Elsa Mauricio Reus and Rosie Richards for their assistance on the data collection.
Supported by the European Union Seventh Framework Programme (FP7/2007‐2013, grant 607510).
REFERENCES
- 1. Woolf AD, Erwin J, March L. The need to address the burden of musculoskeletal conditions. Best Pract Res Clin Rheumatol 2012;26:183–224. [DOI] [PubMed] [Google Scholar]
- 2. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2163–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wallis JA, Webster KE, Levinger P, Taylor NF. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta‐analysis. Osteoarthritis Cartilage 2013;21:1648–59. [DOI] [PubMed] [Google Scholar]
- 4. Herbolsheimer F, Schaap LA, Edwards MH, Maggi S, Otero A, Timmermans EJ, et al. Physical activity patterns among older adults with and without knee osteoarthritis in six European countries. Arthritis Care Res (Hoboken) 2016;68:228–36. [DOI] [PubMed] [Google Scholar]
- 5. Strath SJ, Kaminsky LA, Ainsworth BE, Ekelund U, Freedson PS, Gary RA, et al. Guide to the assessment of physical activity: clinical and research applications. A scientific statement from the American Heart Association. Circulation 2013;128:2259–79. [DOI] [PubMed] [Google Scholar]
- 6. Hardy LL, Hills AP, Timperio A, Cliff D, Lubans D, Morgan PJ, et al. A hitchhiker's guide to assessing sedentary behaviour among young people: deciding what method to use. J Sci Med Sport 2013;16:28–35. [DOI] [PubMed] [Google Scholar]
- 7. Semanik PA, Lee J, Song J, Chang RW, Sohn MW, Ehrlich‐Jones LS, et al. Accelerometer‐monitored sedentary behavior and observed physical function loss. Am J Public Health 2015;105:560–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee J, Chang RW, Ehrlich‐Jones L, Kwoh CK, Nevitt M, Semanik PA, et al. Sedentary behavior and physical function: objective evidence from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 2015;67:366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Butte NF, Ekelund U, Westerterp KR. Assessing physical activity using wearable monitors: measures of physical activity. Med Sci Sports Exerc 2012;44 Suppl 1:S5–12. [DOI] [PubMed] [Google Scholar]
- 10. Focht BC, Garver MJ, Devor ST, Dials J, Rose M, Lucas AR, et al. Improving maintenance of physical activity in older, knee osteoarthritis patients trial‐pilot (IMPACT‐P): design and methods. Contemp Clin Trials 2012;33:976–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Warren JM, Ekelund U, Besson H, Mezzani A, Geladas N, Vanhees L, et al. Assessment of physical activity: a review of methodologies with reference to epidemiological research. A report of the exercise physiology section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil 2010;17:127–39. [DOI] [PubMed] [Google Scholar]
- 12. Tomkins‐Lane CC, Haig AJ. A review of activity monitors as a new technology for objectifying function in lumbar spinal stenosis. J Back Musculoskelet Rehabil 2012;25:177–85. [DOI] [PubMed] [Google Scholar]
- 13. Vanhees L, Lefevre J, Philippaerts R, Martens M, Huygens W, Troosters T, et al. How to assess physical activity? How to assess physical fitness? Eur J Cardiovasc Prev Rehabil 2005;12:102–14. [DOI] [PubMed] [Google Scholar]
- 14. Matthews CE, Hagstromer M, Pober DM, Bowles HR. Best practices for using physical activity monitors in population‐based research. Med Sci Sports Exerc 2012;44 Suppl 1:S68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Verlaan L, Bolink SA, Van Laarhoven SN, Lipperts M, Heyligers IC, Grimm B, et al. Accelerometer‐based physical activity monitoring in patients with knee osteoarthritis: objective and ambulatory assessment of actual physical activity during daily life circumstances. Open Biomed Eng J 2015;9:157–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sylvia LG, Bernstein EE, Hubbard JL, Keating L, Anderson EJ. Practical guide to measuring physical activity. J Acad Nutr Diet 2014;114:199–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Barisic A, Leatherdale ST, Kreiger N. Importance of frequency, intensity, time and type (FITT) in physical activity assessment for epidemiological research. Can J Public Health 2011;102:174–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Van Remoortel H, Giavedoni S, Raste Y, Burtin C, Louvaris Z, Gimeno‐Santos E, et al. Validity of activity monitors in health and chronic disease: a systematic review. Int J Behav Nutr Phys Act 2012;9:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Troiano RP, McClain JJ, Brychta RJ, Chen KY. Evolution of accelerometer methods for physical activity research. Br J Sports Med 2014;48:1019–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Trost SG, McIver KL, Pate RR. Conducting accelerometer‐based activity assessments in field‐based research. Med Sci Sports Exerc 2005;37 Suppl:S531–43. [DOI] [PubMed] [Google Scholar]
- 21. Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum 1991;34:505–14. [DOI] [PubMed] [Google Scholar]
- 22. Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum 1986;29:1039–49. [DOI] [PubMed] [Google Scholar]
- 23. Jones A, Silva PG, Silva AC, Colucci M, Tuffanin A, Jardim JR, et al. Impact of cane use on pain, function, general health and energy expenditure during gait in patients with knee osteoarthritis: a randomised controlled trial. Ann Rheum Dis 2012;71:172–9. [DOI] [PubMed] [Google Scholar]
- 24. Reininga IH, Stevens M, Wagenmakers R, Bulstra SK, Groothoff JW, Zijlstra W. Subjects with hip osteoarthritis show distinctive patterns of trunk movements during gait: a body‐fixed‐sensor based analysis. J Neuroeng Rehabil 2012;9:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Del Din S, Godfrey A, Galna B, Lord S, Rochester L. Free‐living gait characteristics in ageing and Parkinson's disease: impact of environment and ambulatory bout length. J Neuroeng Rehabil 2016;13:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chen KY, Bassett DR Jr. The technology of accelerometry‐based activity monitors: current and future. Med Sci Sports Exerc 2005;37 Suppl:S490–500. [DOI] [PubMed] [Google Scholar]
- 27. Hermann A, Ried‐Larsen M, Jensen AK, Holst R, Andersen LB, Overgaard S, et al. Low validity of the Sensewear Pro3 activity monitor compared to indirect calorimetry during simulated free living in patients with osteoarthritis of the hip. BMC Musculoskelet Disord 2014;15:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Zhang S, Murray P, Zillmer R, Eston RG, Catt M, Rowlands AV. Activity classification using the GENEA: optimum sampling frequency and number of axes. Med Sci Sports Exerc 2012;44:2228–34. [DOI] [PubMed] [Google Scholar]
- 29. Farr JN, Going SB, Lohman TG, Rankin L, Kasle S, Cornett M, et al. Physical activity levels in patients with early knee osteoarthritis measured by accelerometry. Arthritis Rheum 2008;59:1229–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Judice PB, Santos DA, Hamilton MT, Sardinha LB, Silva AM. Validity of GT3X and Actiheart to estimate sedentary time and breaks using ActivPAL as the reference in free‐living conditions. Gait Posture 2015;41:917–22. [DOI] [PubMed] [Google Scholar]
- 31. Hawker GA, Stewart L, French MR, Cibere J, Jordan JM, March L, et al. Understanding the pain experience in hip and knee osteoarthritis: an OARSI/OMERACT initiative. Osteoarthritis Cartilage 2008;16:415–22. [DOI] [PubMed] [Google Scholar]
- 32. Chiauzzi E, Rodarte C, DasMahapatra P. Patient‐centered activity monitoring in the self‐management of chronic health conditions. BMC Med 2015;13:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. White DK, Tudor‐Locke C, Felson DT, Gross KD, Niu J, Nevitt M, et al. Walking to meet physical activity guidelines in knee osteoarthritis: is 10,000 steps enough? Arch Phys Med Rehabil 2013;94:711–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Appendix A


