Abstract
INTRODUCTION:
Venous thromboembolism (VTE) during hospitalization is a serious and potentially fatal condition. Despite its effectiveness, evidence-based thromboprophylaxis is still underutilized in many countries including Saudi Arabia.
OBJECTIVE OF THE STUDY:
Our objectives were to determine how often hospital-acquired VTE patients received appropriate thromboprophylaxis, VTE-associated mortality, and the percentage of patients given anticoagulant therapy and adherence to it after discharged.
METHODS:
This study was conducted in seven major hospitals in Saudi Arabia. From July 1, 2009, till June 30, 2010, all recorded deep vein thrombosis (DVT) and pulmonary embolism (PE) cases were noted. Only patients with confirmed VTE diagnosis were included in the analysis.
RESULTS:
A total of 1241 confirmed VTE cases occurred during the 12-month period. Most (58.3%) of them were DVT only, 21.7% were PE, and 20% were both DVT and PE. 21.4% and 78.6% of confirmed VTE occurred in surgical and medical patients, respectively. Only 40.9% of VTE cases received appropriate prophylaxis (63.2% for surgical patients and 34.8% for medical patients; P < 0.001). The mortality rate was 14.3% which represented 1.6% of total hospital deaths. Mortality was 13.5% for surgical patients and 14.5% for medical patients (P > 0.05). Appropriate thromboprophylaxis was associated with 4.11% absolute risk reduction in mortality (95% confidence interval: 0.24%–7.97%). Most (89.4%) of the survived patients received anticoagulation therapy at discharge and 71.7% of them were adherent to it on follow-up.
CONCLUSION:
Thromboprophylaxis was underutilized in major Saudi hospitals denoting a gap between guideline and practice. This gap was more marked in medical than surgical patients. Hospital-acquired VTE was associated with significant mortality. Efforts to improve thromboprophylaxis utilization are warranted.
Keywords: Deep vein thrombosis, diagnosis, pulmonary embolism, Saudi Arabia, thromboprophylaxis, venous thromboembolism
Venous thromboembolism (VTE), whether deep vein thrombosis (DVT) or pulmonary embolism (PE), may complicate acute illnesses requiring hospitalization. It can lead to significant morbidity[1,2] and mortality[3,4] and has a high economic burden.[5] Thromboprophylaxis is effective in preventing VTE[6,7] and is recommended for at-risk hospitalized patients.[8,9,10] Nevertheless, multiple studies have demonstrated that VTE prophylaxis is underutilized. The Epidemiologic International Day for the Evaluation of Patients at Risk for Venous Thromboembolism in the Acute Hospital Care Setting (ENDORSE) study was a cross-sectional survey across 32 countries and showed a low rate of appropriate thromboprophylaxis.[11] The rate varied between 0.2% and 92% (mean 59%) for surgical patients and 3%–70% (mean 40%) for medical patients.[11] According to the ENDORSE study, the mean national rate of thromboprophylaxis in medical and surgical patients (n = 467) in the Saudi Arabia was about 50% as 66% of medical patients and 32% of surgical patients received the American College of Chest Physicians (ACCP)-recommended thromboprophylaxis.[11] The AVAIL ME study, which was conducted in the Middle East, included 2266 patients (200 patients from a hospital in Saudi Arabia), showed that compliance with guideline-based thromboprophylaxis was as low as 40.1% in medical patients and 36.4% in surgical patients.[12] Similar data were obtained by a retrospective single center study conducted at King Fahd General Hospital in Jeddah, Saudi Arabia, which showed that thromboprophylaxis was administered in 44.1% of surgical patients and 22% of medical patients who were at VTE risk.[13] In addition, a significant variability in the implementation of thromboprophylaxis guidelines has been reported among hospitals in the same country.[11]
The elaboration of national policies for the implementation of the guidelines for VTE prophylaxis is a major step for the improvement of quality of care in hospitalized patients. To this aim, regular audits offer crucial information of the status of VTE prophylaxis and can allow targeted interventions to ameliorate the actual practices. The primary objectives of this study were to estimate how often hospital-acquired VTE patients received appropriate thromboprophylaxis according to the 2008 ACCP guidelines[14] and to assess the mortality rate in VTE patients.
Methods
Patients and setting
This study is a retrospective cohort study that was conducted at seven major hospitals representing different health sectors in Saudi Arabia. These hospitals were (1) King Fahd General Hospital, Jeddah, (2) King Abdulaziz Medical City National Guard, Jeddah, (3) King Abdulaziz University Hospital, Jeddah, (4) King Saud University Hospital, Riyadh, (5) King Saud Medical City, Riyadh, (6) King Abdulaziz Medical City National Guard Hospital, Riyadh, and (7) Prince Sultan Military Hospital, Riyadh. The Institutional Review Board of each of these hospitals approved the study.
We first identified the patients who were admitted to the seven hospitals between July 1, 2009, and June 30, 2010, and had ICD-9 codes related to VTE (DVT and PE). Their medical records were reviewed afterward and only the confirmed cases of VTE that developed during hospitalization were included in this study. DVT was diagnosed by Doppler ultrasound of the extremities and PE by helical chest computed tomography (CT) or ventilation-perfusion (V/Q) scan. However, the final diagnosis of PE/DVT was based on the conclusion of the radiological findings of the studied imaging (CT chest, V/Q scan, and Doppler studies) and the acceptance of the diagnosis by the primary physician rather than the details of each modality.
Data collection
The following data were noted for each VTE-confirmed patient: age, sex, admission category (medical vs. surgical), VTE risk factors, VTE risk according to the Caprini Risk Assessment Model,[15] thromboprophylaxis method, survival status, anticoagulation treatment administered, and adherence to anticoagulation treatment after discharge. In addition, we obtained statistics on all deaths that occurred in the hospital during the study period and on in-hospital deaths due to circulatory and respiratory collapse, which could be caused by PE as per the written cause of death (nonautopsy report).
Outcomes
The primary outcomes of this study were (1) the rate of hospital-acquired VTE patients received appropriate thromboprophylaxis utilization according to 2008 ACCP guidelines[14] and (2) the hospital mortality rate in VTE patients. The secondary outcomes were to determine percentage of VTE mortality among all-cause hospital mortality, to assess the percentage of VTE confirmed patients in each ward type (surgical and medical), and to estimate the rate of adherence to anticoagulation therapy for patients who survived their issuing VTE episode after discharge.
Statistical analysis
Descriptive statistics were stated as mean with standard deviation for continuous variables and frequency with percentage for categorical variables. Inferential statistics were performed to test differences between groups using the Chi-square test for categorical variables. Whenever any of the expected values was <5, Fisher's exact test was used instead. The Student's t-test was used to assess the differences between continuous variables. All statistical tests used were two-tailed at 5% level of significance. All statistical analyses were performed using Statistical Package for Social Sciences (SPSS Statistics for Windows, version 17, released 2008, SPSS Inc., Chicago, IL, USA).
Results
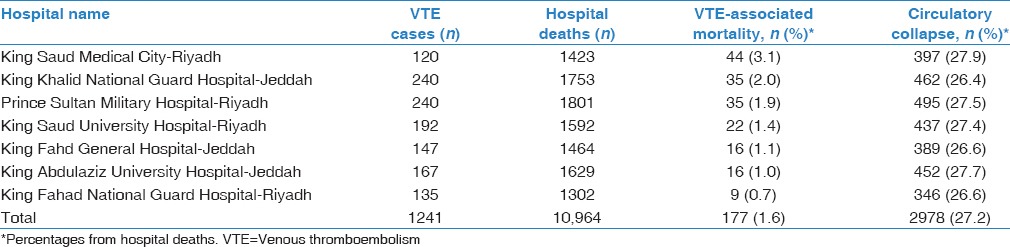
Seven Saudi major hospitals participated in the study and reported that 1241 patients developed VTE during hospitalization between July 1, 2009, and June 30, 2010. Out of the 1241 VTE patients, King Fahd General Hospital-Jeddah included 147 patients (11.8%), King Khalid National Guard Hospital-Jeddah included 240 patients (19.3%), King Abdulaziz University Hospital-Jeddah included 167 patients (13.5%), King Saud University Hospital-Riyadh included 192 patients (15.5%), King Saud Medical City-Riyadh included 120 patients (9.7%), King Fahad National Guard Hospital-Riyadh included 135 patients (10.9%), and Prince Sultan Military Hospital-Riyadh included 240 patients (19.3%).
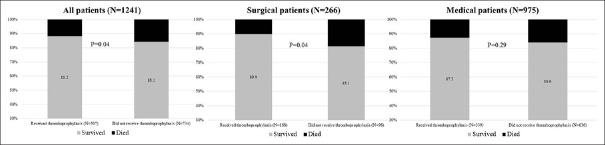
Table 1 shows the baseline characteristics of all included patients. The majority of patients were >40 years old and 52% were males. Two hundred and sixty-six (21.4%) patients had undergone surgery, while 975 (78.6%) were hospitalized for acute medical illnesses. The surgeries in decreasing order of frequency were abdominal (n = 113), orthopedic (n = 52), urology (n = 22), vascular (n = 16), thoracic (n = 15), obstetrics/gynecology (n = 13), and neurosurgery (n = 12). Eighty-five patients had surgery for cancer. General anesthesia was used in 213 patients. Eight patients were on erythropoietin analogs, 23 on estrogen-containing medications, 3 on hormone replacement therapy, and 7 on chemotherapy.
Table 1.
Baseline characteristics of patients with confirmed diagnosis of venous thromboembolism
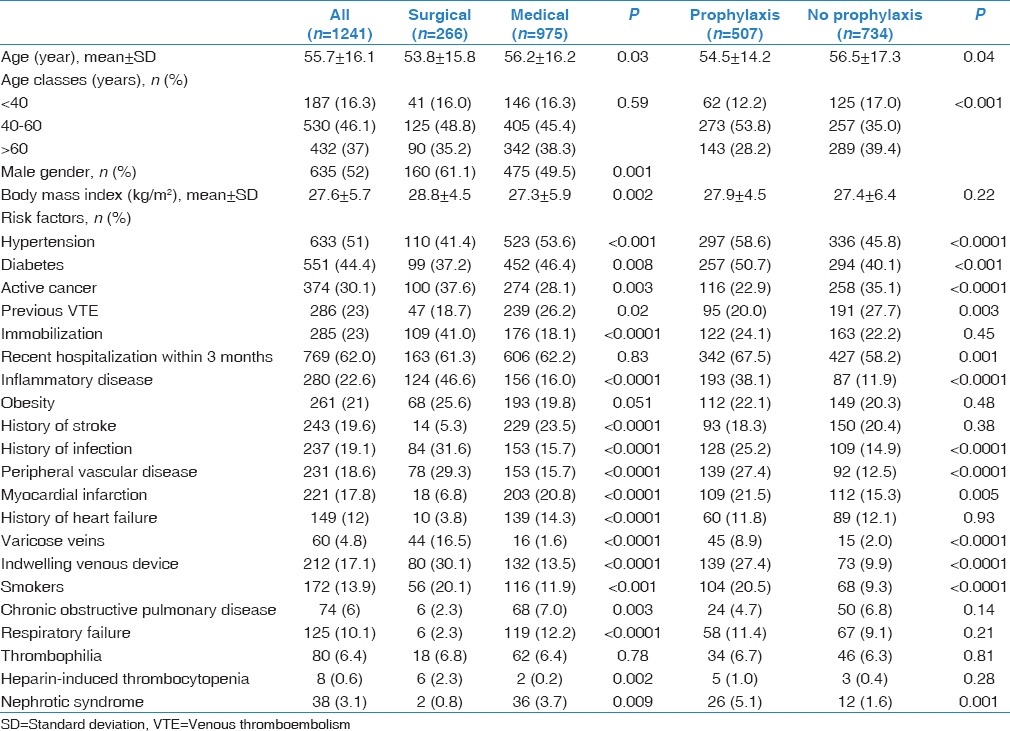
Table 2 describes the VTE risk assessment of the study patients and the percentage of patients who received the appropriate thromboprophylaxis of each group. Among all the surgical patients (266 patients), 168 patients (63.2%) received the appropriate thromboprophylaxis; 134/189 (70.9%) were at very high risk, 16/44 (36.4%) were at high risk, and 18/33 (54.5%) were at moderate risk. Among all the medical patients (975 patients), only 339 patients (34.7%) received the appropriate thromboprophylaxis; 204/621 (32.9%) were at high risk and 135/354 (38.1%) patients were at moderate risk.
Table 2.
The relationship between venous thromboembolism prophylaxis and the mortality of patients who developed venous thromboembolism during hospital stay
Type and symptoms associated with venous thromboembolism
In this cohort, 724 (58.3%) patients suffered from DVT, 248 (20%) had DVT and PE, and 269 (21.7%) were diagnosed with PE alone.
The symptoms associated with DVT included leg pain 73.2% (81.1% surgical and 71.1% medical; 82.4% on prophylaxis and 66.8% on no prophylaxis), leg swelling 62.9% (74.4% surgical and 59.9% medical; 79.7% on prophylaxis and 51.2% on no prophylaxis), leg redness 54.0% (69.9% surgical and 43.0% medical; 69.9% on prophylaxis and 43.0% on no prophylaxis), and warmth 55.6% (55.2% surgical and 55.6% medical; 68.9% on prophylaxis and 46.2% on no prophylaxis).
The symptoms associated with PE included dyspnea 360/481, 74.8% (89.8% surgical and 71.0% medical; 84.5% of those on prophylaxis and 70.0% in patients on no prophylaxis), tachypnea 69.6% (84.2% surgical and 66.0% medical; 79.9% on prophylaxis and 64.5% on no prophylaxis), chest pain 50.3% (61.5% surgical and 47.5% medical; 51.3% on prophylaxis and 49.8% on no prophylaxis), and hemoptysis 7.7% (9.7% surgical and 7.3% medical; 7.8% on prophylaxis and 7.7% on no prophylaxis). Circulatory instability was present in 21.0% (20.0% surgical and 21.2% medical; 23.3% on prophylaxis and 19.8% on no prophylaxis).
Venous thromboembolism prophylaxis practices
Based on the 8th ACCP guidelines for VTE prophylaxis, all the 1241 patients in the cohort were eligible to receive VTE prophylaxis. The analysis of the medical records showed that 40.9% (507) patients received prophylaxis and 59.1% (734) patients did not receive it. Surgical patients received VTE prophylaxis more frequently than medical patients (63.2% vs. 34.8%, respectively, P < 0.001). Among patients who received prophylaxis, enoxaparin was the most commonly used agent (n = 422, 83.2%) followed by unfractionated heparin (n = 60, 11.8%) and fondaparinux (n = 15, 3.0%). Graduated compression stocking was used in 125 patients and intermittent pneumatic compression devices in 24 patients. However, the history of use of mechanical devices was not known in most patients of this cohort.
Considering the different VTE-risk groups, pharmacological prophylaxis with low molecular weight heparin (LMWH) was administered to 134 (70.9%) very high-risk, 16 (36.4%) high-risk, and 18 (54.5%) moderate-risk surgical patients. Among medical patients who developed VTE, pharmacological prophylaxis with LMWH was administered to 204 (34.8) high-risk and 135 (38.1%) moderate-risk medical patients [Table 2].
We also found that more patients with DVT alone than PE alone received VTE prophylaxis as compared to those patients who had DVT progressing to PE (46.7% and 41.6% vs. 23%, respectively, P < 0.001) [Figure 1].
Figure 1.
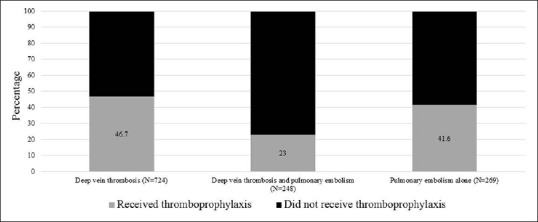
Thromboprophylaxis according to venous thromboembolism diagnosis
Mortality
In the current study, 177 (14.3%) patients who developed VTE during hospitalization died. The mortality rate in medical patients was not significantly different compared with that of surgical patients (14.5% vs. 13.5%, respectively, P > 0.05). In the medical patients, deaths occurred in high-risk patients (19.2%) and moderate-risk patients (6.2%); the difference is statistically significant (P < 0.001) [Table 2].
In surgical patients, deaths occurred in 13.8% of the very high-risk group, 15.9% of the high-risk group, and 9.1% of the moderate-risk group, with no statistical difference (P > 0.05) [Table 2].
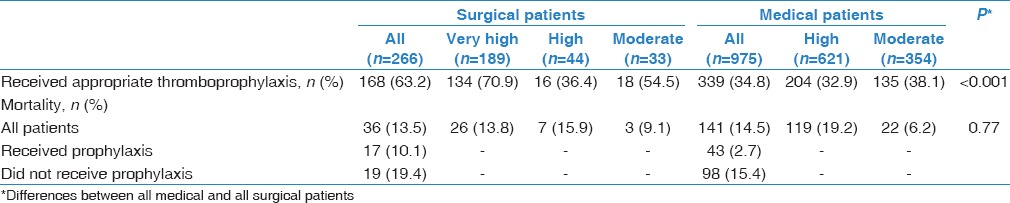
The mortality rate in the VTE patients who received thromboprophylaxis was significantly lower than the mortality of those who did not receive it (11.8% vs. 15.9%, respectively; P = 0.04) as shown in Figure 2. The absolute risk reduction was 4.11% (95% confidence interval [CI]: 0.24%–7.97%). The difference in mortality was significantly different in surgical (10.1% vs. 19.4%, respectively; P < 0.05) but not in medical patients (12.7% vs. 15.4%, respectively; P > 0.05). The absolute risk reduction in surgical patients was 9.27% (95% CI: 0.21–18.33%). The absolute risk reduction in medical patients was 2.72% (95% CI: −1.79%–7.24%).
Figure 2.
Mortality according to receiving prophylaxis in all surgical and medical patients
From the diagnosis perspective, 79 patients (31.9%) of DVT patients progressing to PE died, and 54 patients (20.1%) of PE and 44 patients (6.1%) of DVT died due to VTE, with statistically significant (P < 0.001).
During the current study period, 10,964 patients died in the seven hospitals. Hence, the VTE-associated hospital mortality (n = 177) accounted for 1.6% of the total hospital mortality. We also found that 2978 patients had hospital deaths labeled to be due to “circulatory and respiratory collapse.” Table 3 describes VTE case in relationship to hospital deaths.
Table 3.
Mortality due to venous thromboembolism in relation to hospital deaths
Adherence to anticoagulation treatment after discharge
Out of the 1064 VTE patients who survived to hospital discharge, 951 (76.6%) were prescribed anticoagulation therapy after discharge. On follow-up, 682 of them were adherent to it. There were no differences in the adherence to anticoagulation therapy between surgical and medical patients (70.1% and 72.2%, respectively, P > 0.05). Out of our surprise, patients who developed DVT alone were significantly more adherent to anticoagulation therapy treatment after discharge as compared to patients who developed DVT that was progressed to PE and PE alone (78.5%, 60.4%, and 58.1%, P < 0.001).
Discussion
In this study, we found that thromboprophylaxis was underutilized in this seven major hospitals in Saudi Arabia; the compliance with guideline-based thromboprophylaxis was less common in medical patients than in surgical patients; VTE-associated mortality rate was lower in patients who received thromboprophylaxis compared with those who did not. Moreover, lack of adherence to anticoagulation treatment after discharge was observed.
According to the ACCP guidelines, all of the included 1241 patients should have had received pharmacological thromboprophylaxis. Despite their eligibility, we found that only 40.9% of them received it denoting underutilization of VTE thromboprophylaxis. A plethora of studies highlighted the same observation. In the ENDORSE study, while 50% of hospitalized patients should have received VTE prophylaxis, only half of them received it actually.[11] In a study that was conducted in 10 nonacademic Polish hospitals, 2673 patients were enrolled, of which 1111 were judged to be eligible for VTE prophylaxis. However, only 51.8% received ACCP-recommended prophylaxis.[16] In a retrospective cross-sectional study in India, 2058 patients from 10 hospitals were evaluated (between August 2006 and January 2007) as per the 2004 ACCP evidence-based consensus guidelines,[17] 1104 (53.6%) patients were found to be eligible for VTE prophylaxis, and only 17.4% received ACCP-recommended thromboprophylaxis.[17] In the DVT-free prospective registry, 5451 patients with ultrasound-confirmed DVT from 183 United States centers were enrolled.[18] Out of the 2726 patients who had their DVT diagnosed while in the hospital, only 1147 (42%) were found to receive prophylaxis.[18] In the CURVE study, a multicenter Canadian survey study, about 4124 medical admissions from 20 teaching and 8 community hospitals were screened to assess the adherence to the 6th ACCP consensus guidelines for VTE prophylaxis.[19] Of the screened admissions, 1894 patients (46%) were eligible for study inclusion.[19] Forty-one percent of patients were bedridden for more than 24 h and 31% had one or more identified risk factors for VTE.[19] Appropriate prophylaxis was found to be administered to only 16% of patients.[19] The IMPROVE study reported that appropriate VTE prophylaxis was administered in less than 60% of 15,156 high-risk medically ill patients enrolled at 52 hospitals.[20] In Lebanon, a study was conducted at the American University of Beirut Medical Center (AUBMC) to evaluate VTE prophylaxis under the care of the Department of Internal Medicine at AUBMC during 2005. Two hundred and fifty patients staying >2 days were randomly selected, and their medical records were reviewed. About 139 patients were found to have two or more risk factors, with no absolute contraindications. Out of them, only 37 patients (26.6%) received VTE prophylaxis. Out of 144 patients with two or more risk factors, with no contraindications, only 40 patients (27.8%) received VTE prophylaxis.[21] In the AVAIL ME study, only 37% of eligible patient received VTE prophylaxis.[12] A similar finding was reported in King Fahd General Hospital-Jeddah, during the period from July 1, 2008, till June 30, 2009, as only 36.5% of patients received prophylaxis.[13]
Complying with thromboprophylaxis guidelines appears to be a worldwide problem despite proven efficacy. Our study adds more evidence to this problem. Many strategies to close the gap between underutilization and complying with guidelines have been suggested such as periodic educational session,[22,23] electronic alerts,[24] and order sets.[25] However, the efficacy of some methods is questionable.[26] Multifaceted strategies have been suggested to be more effective than single strategy.[27,28,29,30] Whatever the strategies adopted, there is a need to enforce it by either the administrative medical staff in each hospital or better by regulatory medical authorities in each country to guarantee durability, compliance, and hence efficacy. Recently, the Saudi Ministry of Health has endorsed national clinical practice guidelines on thromboprophylaxis.[31] Healthcare administrative authorities should assess the effectiveness of selected strategies as modifications may be needed depending on results. We found that surgical patients received thromboprophylaxis significantly more often than medical patients. Many studies reported similar finding.[11,13,16] In the ENDORSE study, medical patients receiving thromboprophylaxis ranged between 3% and 70%.[11] This suggests that more efforts on improving thromboprophylaxis practices should be directed toward patients in medical wards.
The mortality of patients with confirmed VTE in the seven hospitals was 14.3% with no significant difference between surgical and medical patients. However, it was significantly higher in patients who did not receive thromboprophylaxis compared with patients who received it. VTE was found to account for 1.6% of total hospitals mortalities. This is similar to the previous retrospective study that was conducted in King Fahd General Hospital in Saudi Arabia where the mortality was 20.8% of confirmed VTE patients and VTE accounts for 1.4% of total hospital mortality.[13] Our study adds more evidence to the importance of thromboprophylaxis in lowering VTE-related mortality.
As a form of nonadherence to ACCP guidelines, only 76.6% were prescribed anticoagulation treatment upon discharge and 71.7% of them were adherent to it upon follow-up. Such lack of guideline compliance was also reported before where 97.2% prescribed anticoagulation therapy and 83.7% of them were adherents upon follow-up.[13] Adherence to guidelines should not be limited to prophylactic measures as it should extend to adherence to anticoagulation therapy after VTE and the strategy to be implemented should consider the whole picture of the VTE, starting from prophylaxis through treatment and follow-up.
The study was limited by being retrospective and by depending on patients' records and databases for data collection. However, we do not believe that these factors affected the results. We reported VTE-associated mortality. However, the study did not assess the exact causes of death, which could have been conditions other than VTE. We expect that a proportion of hospital deaths, including those who followed circulatory or respiratory arrest, were due to VTE. The study was also limited by the absence of autopsy data as autopsy was seldom practiced in Saudi Arabia. Autopsy studies would have increased the numbers of VTE cases. This should add more enthusiasm to enforce applying the guidelines.
Conclusion
Thromboprophylaxis therapy is underutilized denoting a gap between guideline and practice for patients at-risk of developing VTE. This gap is markedly more in medical patients compared to surgical patients. Efforts must be directed to improve prophylaxis utilization. VTE-associated mortality was lower in surgical patients who received thromboprophylaxis, which further emphasizes the importance of thromboprophylaxis in this vulnerable group of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We would like to acknowledge Dr. Wael El-Mursy, Dr. Jalal Rifai, and Mrs. Ohoud Al-Orabi, Department of Intensive Care, King Abdulaziz Medical City, NGHA, Jeddah, Saudi Arabia. We would also like to acknowledge Dr. Saleh AlGhamdi, Dr. Mohammed Alansari, Dr. Ameen Jaddoh, Dr. Ahmed Alsheheri, and Dr. Ryan Abduljawad, Internal Medicine Department, King Saud Medical City, Riyadh, Saudi Arabia. We are also thankful to Dr. Ahmed Omar, Sanofi, Jeddah, Saudi Arabia.
References
- 1.Mohr DN, Silverstein MD, Heit JA, Petterson TM, O'Fallon WM, Melton LJ. The venous stasis syndrome after deep venous thrombosis or pulmonary embolism: A population-based study. Mayo Clin Proc. 2000;75:1249–56. doi: 10.4065/75.12.1249. [DOI] [PubMed] [Google Scholar]
- 2.Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004;350:2257–64. doi: 10.1056/NEJMoa032274. [DOI] [PubMed] [Google Scholar]
- 3.Alikhan R, Peters F, Wilmott R, Cohen AT. Fatal pulmonary embolism in hospitalised patients: A necropsy review. J Clin Pathol. 2004;57:1254–7. doi: 10.1136/jcp.2003.013581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sandler DA, Martin JF. Autopsy proven pulmonary embolism in hospital patients: Are we detecting enough deep vein thrombosis? J R Soc Med. 1989;82:203–5. doi: 10.1177/014107688908200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caprini JA, Botteman MF, Stephens JM, Nadipelli V, Ewing MM, Brandt S, et al. Economic burden of long-term complications of deep vein thrombosis after total hip replacement surgery in the United States. Value Health. 2003;6:59–74. doi: 10.1046/j.1524-4733.2003.00204.x. [DOI] [PubMed] [Google Scholar]
- 6.Kanaan AO, Silva MA, Donovan JL, Roy T, Al-Homsi AS. Meta-analysis of venous thromboembolism prophylaxis in medically Ill patients. Clin Ther. 2007;29:2395–405. doi: 10.1016/j.clinthera.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 7.Mismetti P, Laporte S, Darmon JY, Buchmüller A, Decousus H. Meta-analysis of low molecular weight heparin in the prevention of venous thromboembolism in general surgery. Br J Surg. 2001;88:913–30. doi: 10.1046/j.0007-1323.2001.01800.x. [DOI] [PubMed] [Google Scholar]
- 8.Wickham N, Gallus AS, Walters BN, Wilson A NHMRC VTE Prevention Guideline Adaptation Committee. Prevention of venous thromboembolism in patients admitted to Australian hospitals: Summary of National Health and Medical Research Council clinical practice guideline. Intern Med J. 2012;42:698–708. doi: 10.1111/j.1445-5994.2012.02808.x. [DOI] [PubMed] [Google Scholar]
- 9.Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, et al. Prevention of VTE in nonsurgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed.: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e195S–226S. doi: 10.1378/chest.11-2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qaseem A, Chou R, Humphrey LL, Starkey M, Shekelle P Clinical Guidelines Committee of the American College of Physicians. Venous thromboembolism prophylaxis in hospitalized patients: A clinical practice guideline from the American College of Physicians. Ann Intern Med. 2011;155:625–32. doi: 10.7326/0003-4819-155-9-201111010-00011. [DOI] [PubMed] [Google Scholar]
- 11.Cohen AT, Tapson VF, Bergmann JF, Goldhaber SZ, Kakkar AK, Deslandes B, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): A multinational cross-sectional study. Lancet. 2008;371:387–94. doi: 10.1016/S0140-6736(08)60202-0. [DOI] [PubMed] [Google Scholar]
- 12.Taher AT, Aoun J, Salameh P. The AVAIL ME study: A multinational survey of VTE risk and prophylaxis. J Thromb Thrombolysis. 2011;31:47–56. doi: 10.1007/s11239-010-0492-2. [DOI] [PubMed] [Google Scholar]
- 13.Essam AE, Sharif G, Al-Hameed F. Venous thromboembolism-related mortality and morbidity in King Fahd General Hospital, Jeddah, Kingdom of Saudi Arabia. Ann Thorac Med. 2011;6:193–8. doi: 10.4103/1817-1737.84772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition) Chest. 2008;133(6 Suppl):381S–453S. doi: 10.1378/chest.08-0656. [DOI] [PubMed] [Google Scholar]
- 15.Caprini JA. Thrombosis risk assessment as a guide to quality patient care. Dis Mon. 2005;51:70–8. doi: 10.1016/j.disamonth.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Musial J, Sydor WJ ENDORSE Investigators-Poland. Venous thromboembolism risk and prophylaxis in the acute hospital care setting – Results of the ENDORSE study in Poland. Pol Arch Med Wewn. 2008;118:555–61. [PubMed] [Google Scholar]
- 17.Pinjala R ENDORSE-India investigators. Venous thromboembolism risk & prophylaxis in the acute hospital care setting (ENDORSE), a multinational cross-sectional study: Results from the Indian subset data. Indian J Med Res. 2012;136:60–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Goldhaber SZ, Tapson VF DVT FREE Steering Committee. A prospective registry of 5,451 patients with ultrasound-confirmed deep vein thrombosis. Am J Cardiol. 2004;93:259–62. doi: 10.1016/j.amjcard.2003.09.057. [DOI] [PubMed] [Google Scholar]
- 19.Kahn SR, Panju A, Geerts W, Pineo GF, Desjardins L, Turpie AG, et al. Multicenter evaluation of the use of venous thromboembolism prophylaxis in acutely ill medical patients in Canada. Thromb Res. 2007;119:145–55. doi: 10.1016/j.thromres.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Tapson VF, Decousus H, Pini M, Chong BH, Froehlich JB, Monreal M, et al. Venous thromboembolism prophylaxis in acutely ill hospitalized medical patients: Findings from the International Medical Prevention Registry on Venous Thromboembolism. Chest. 2007;132:936–45. doi: 10.1378/chest.06-2993. [DOI] [PubMed] [Google Scholar]
- 21.Masroujeh R, Shamseddeen W, Isma'eel H, Otrock ZK, Khalil IM, Taher A. Underutilization of venous thromboemoblism prophylaxis in medical patients in a tertiary care center. J Thromb Thrombolysis. 2008;26:138–41. doi: 10.1007/s11239-007-0084-y. [DOI] [PubMed] [Google Scholar]
- 22.Cohn SL, Adekile A, Mahabir V. Improved use of thromboprophylaxis for deep vein thrombosis following an educational intervention. J Hosp Med. 2006;1:331–8. doi: 10.1002/jhm.137. [DOI] [PubMed] [Google Scholar]
- 23.Al-Hameed F, Al-Dorzi HM, Aboelnazer E. The effect of a continuing medical education program on Venous thromboembolism prophylaxis utilization and mortality in a tertiary-care hospital. Thromb J. 2014;12:9. doi: 10.1186/1477-9560-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kucher N, Koo S, Quiroz R, Cooper JM, Paterno MD, Soukonnikov B, et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352:969–77. doi: 10.1056/NEJMoa041533. [DOI] [PubMed] [Google Scholar]
- 25.O'Connor C, Adhikari NK, DeCaire K, Friedrich JO. Medical admission order sets to improve deep vein thrombosis prophylaxis rates and other outcomes. J Hosp Med. 2009;4:81–9. doi: 10.1002/jhm.399. [DOI] [PubMed] [Google Scholar]
- 26.Al-Dorzi HM, Cherfan A, Al-Harbi S, Al-Askar A, Al-Azzam S, Hroub A, et al. Knowledge of thromboprophylaxis guidelines pre- and post-didactic lectures during a venous thromboembolism awareness day at a tertiary-care hospital. Ann Thorac Med. 2013;8:165–9. doi: 10.4103/1817-1737.114298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gallagher M, Oliver K, Hurwitz M. Improving the use of venous thromboembolism prophylaxis in an Australian teaching hospital. Qual Saf Health Care. 2009;18:408–12. doi: 10.1136/qshc.2007.024778. [DOI] [PubMed] [Google Scholar]
- 28.Al-Tawfiq JA, Saadeh BM. Improving adherence to venous thromoembolism prophylaxis using multiple interventions. Ann Thorac Med. 2011;6:82–4. doi: 10.4103/1817-1737.78425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tooher R, Middleton P, Pham C, Fitridge R, Rowe S, Babidge W, et al. A systematic review of strategies to improve prophylaxis for venous thromboembolism in hospitals. Ann Surg. 2005;241:397–415. doi: 10.1097/01.sla.0000154120.96169.99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scaglione L, Piobbici M, Pagano E, Ballini L, Tamponi G, Ciccone G. Implementing guidelines for venous thromboembolism prophylaxis in a large Italian teaching hospital: Lights and shadows. Haematologica. 2005;90:678–84. [PubMed] [Google Scholar]
- 31.Al-Hameed FM, Al-Dorzi HM, Abdelaal MA, Alaklabi A, Bakhsh E, Alomi YA, et al. The Saudi clinical practice guideline for the prophylaxis of venous thromboembolism in medical and critically ill patients. Saudi Med J. 2016;37:1279–93. doi: 10.15537/smj.2016.11.15268. [DOI] [PMC free article] [PubMed] [Google Scholar]