Abstract
There is a paucity of data regarding testicular cancer among Saudis as well as the nonexistent of published national data. Furthermore, a substantial increase of the incidence of testicular cancer among Saudis was lately noted. The aim of the study is to determine the trends and patterns of testicular cancer among adult Saudis using national data over a period of 20 years. The national database of the Saudi Cancer Registry (SCR) on testicular cancer over the last two decades was studied including epidemiological and histological patterns. The 1004 cases of testicular cancer among adult Saudis reported by the SCR will be the subject of this study. From 1994 to 2013, 1004 cases of testicular cancer among adult Saudis were reported to the SCR, with a steadily significant increase in incidence rate reaching an annual rate of 94 cases in 2013. Age of the patients ranged 15–93 years with a mean of 34.5 years. The most affected age group was 20–34 years, where 51% of all testicular cancer accumulated. Around 85% of testicular cancer is germ cell tumors, while paratesticular and gonadal stromal tumors represent 15%. Of all testicular cancer, seminomas were seen in 40.7%, nonseminomas in 44.6%. Notably, 70.4% of the cases in the first decade were seminomas, while in the second decade 65.9% of the cases were nonseminomas. The subtypes of the nonseminomas were a mixed tumor in 51.6%, embryonal carcinoma in 19.9%, yolk sac tumor in 12.3%, germinomas in 6.7%, teratomas in 6%, and choriocarcinomas in 3.6%. Lymphomas (34.7%) and rhabdomyosarcomas (23.6%) are on the top of the paratesticular tumor group. The Surveillance Epidemiology and End Results summary stage of seminomas was localized in 61.6%, regional in 19.8%, and distant in 12.6%, while of nonseminomas was 48%, 15.5%, and 28.5%, respectively. Localized and distant status of seminomas improved over the studied period by 12% and 4% respectively, while this trend was not seen in nonseminomas. The incidence rate is on rising with doubling observed during the last decade. The most affected age group was 20–34 years. Noteworthy was the dominance of the seminomas in the first decade and of the nonseminomas in the second decade. Paratesticular tumors rate is high, third of which were lymphomas. Compared to data from Western countries, notably, there is a high rate of yolk sac tumors and germinomas and a low incidence of choriocarcinomas and embryonal carcinomas. In general, late presentation of all testicular cancer was noted, although a modest stage improvement over the studied period was observed in seminomas, not in nonseminomas.
Keywords: Adult patients, histopathology, Saudi Arabia, testicular cancer, trends
INTRODUCTION
Testicular cancer is a rare malignancy worldwide and among Saudis too. It is largely a disease of young- and middle-aged men, approximately 7% of cases occur in children. Testicular cancer accounts for around 1% of all cancer in males. Almost half of all cases of testicular cancer are in men between the ages of 20 and 34. Roughly, 98% of testicular cancer is germ cell tumors. It is one of the most curable forms of cancer, especially when diagnosed early and the 5-year survival rate is over 95%. Radical surgery is the mainstay treatment in addition to radiotherapy and or the cisplatin-based combination chemotherapy. The incidence of testicular cancer has been increasing in many countries, however, mortality rates remains low.[1,2,3] There is a paucity of data regarding testicular cancer among Saudis. The existing literature and the abstract proceedings of previous annual Saudi conferences is sparse and controversial.[4] There are no published detailed national data obtainable on testicular cancer. Furthermore, a substantial increase of the incidence of testicular cancer among Saudis was lately noted.[2] The aim of the study is to determine the trends and patterns of testicular cancer among adult Saudis using national data over a period of 20 years.
MATERIALS AND METHODS
The national database of the Saudi Cancer Registry (SCR) on testicular cancer over the last two decades was studied including epidemiological and histopathological patterns. During a period of 20 years (1994–2013), the population-based SCR accumulated 1526 cases of testicular cancer. Due to the rarity of testicular cancer, the annual cancer incidence reports of the SCR comprise only the yearly numbers of the disease. For that reason, the complete data on testicular cancer were requested. The studied raw data, uploaded kindly by the SCR-team on Excel tables, contains all required demographic, epidemiological, and histological details. 71.2% of the cases are Saudis, and 28.8% are expatriates. In addition, testicular cancer data from King Faisal Specialist Hospital (KFSH) (1975–2013) were also as a reference evaluated. The 1004 cases of testicular cancer among adult Saudis reported by the SCR will be the subject of this study.
Data analysis
The data are presented as counts, mean and percentages or annual percentage change rates. Numerical variables were summarized as the sample mean and range, and categorical variables were summarized as the number and percentage. Institutional approval for the study was obtained. There was no funding required.
RESULTS
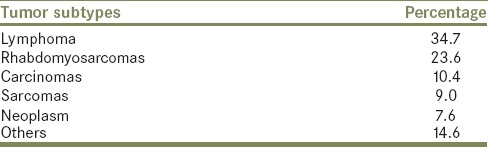
From 1994 to 2013, 1004 cases of testicular cancer among adult Saudis were reported to the SCR, with a mean incidence rate of 50 cases/year and an annual percentage change rate of 11.56%. The age-standardized rate (ASR) increased from 0.4 to 0.9/100,000 during the studied period. The incidence rate of testicular cancer was around 30.5 cases/year in the first decade (1994–2013), but a steadily significant increase in incidence rate in the second decade (2004–2013) was seen with a mean of 70 cases/year, reaching an annual rate of 94 cases in 2013 [Figure 1]. Age of the patients ranged 15–93 years with a mean of 34.5 years. The most affected age group was 20–34 years, where 51% of all testicular cancer fell in this age group [Figure 2]. Right testicles were affected in 49%, left in 41% and bilateral in 1%, while in 9% laterality was not specified. Forty-six (4.58%) of the patients had tumors in undescended testis, most of which were seminomas. Germ cell tumors are making only 85.2% of all testis tumors, while paratesticular tumors and gonadal stromal tumors represent 14.8%. Of all testicular cancer, seminomas were seen in 40.7% and nonseminomas in 44.6% [Table 1]. Notably, 70.4% of the cases in the first decade (1994–2003) were seminomas, while in the second decade (2004–2013) 65.9% of the cases were nonseminomas [Figure 3]. The subtypes of nonseminomas recorded were a mixed tumor in 51.6%, embryonal carcinoma in 19.9%, yolk sac tumor in 12.3%, germinomas in 6.7%, teratomas in 6.0%, and choriocarcinomas in 3.6% [Table 2]. The most common subtypes of paratesticular tumors were lymphomas in 34.75 and rhabdomyosarcomas in 23.6% [Table 3]. The Surveillance Epidemiology and End Results (SEER) summary stage of seminomas was localized in 61.6%, regional in 19.8%, and distant in 12.6%, while of nonseminomas was 48%, 15.5%, and 28.5%, respectively. Localized and distant status of seminomas improved over the studied period by 12% and 4% respectively, while this trend was not seen in nonseminomas.
Figure 1.
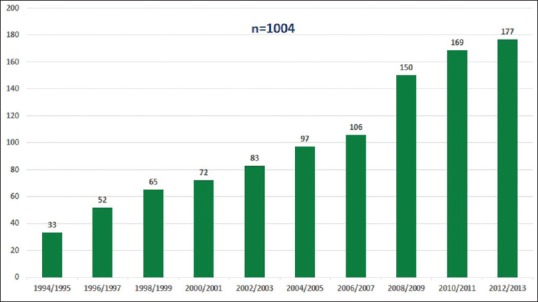
Distribution of testicular cancer in adult Saudis by year groups, Saudi Cancer Registry, 1994–2013
Figure 2.
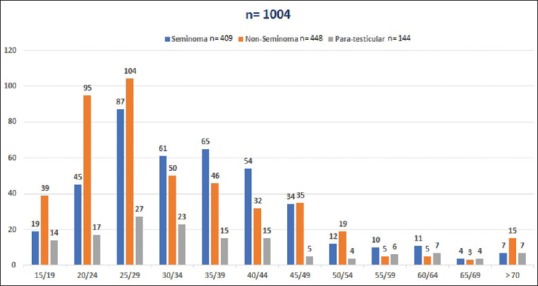
Adult testicular cancer in Saudis by age groups Saudi Cancer Registry, 1994–2013
Table 1.
Adult testicular cancer among Saudi Cancer Registry, 1994-2013 (n=1004)
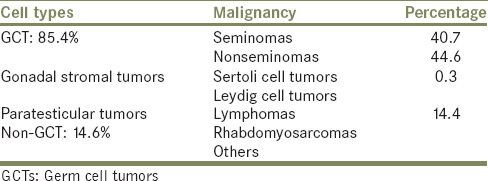
Figure 3.

Adult testicular cancer in Saudis by year groups Saudi Cancer Registry, 1994–2013
Table 2.
Malignant nonseminoma tumors in Adult Saudis: Comparative data - Saudi Cancer Registry* versus USA** (n=448)
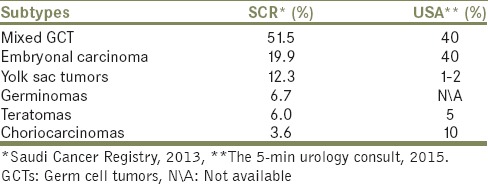
Table 3.
Malignant paratesticular tumors in adult Saudi Cancer Registry, 1994-2013 (n=144)
DISCUSSION
The incidence of testicular cancer varies based on geography, race and socioeconomic status and is on rising with substantial differences among countries.[5] This global increase appears to be more related to birth cohort effects. The incidence is highest in Europe and North America and lowest in Asia and Africa. The age-standardized incidence rate in Europe and North America is between 4 and 10/100,000, whereas in Asia and Africa is between 0.2 and 1/100,000.[5,6] The incidence among Saudis in 2013 is 1.8% of all cancer in men with an ASR of 0.9/100,000, which increased from 0.4 to 0.9/100,000 during the studied period. Due to the rarity of testicular cancer, no much attention has been given by the local urologists, contrary to other genitourinary cancer. For that reason, there is a paucity of reports concerning testicular cancer in Saudi Arabia. The existing literature and abstract proceedings of previous Saudi annual conferences are sparse and controversial. The first documented reports on testicular cancer among Saudis were published in 1986 and 1987 analyzing 62 cases of testis tumors seen between 1977 and 1983 at KFSH Riyadh, which is a main national referral cancer center receiving around 22% of all cancer cases in the country. Both articles reporting on the same patients and the investigators concluded that seminoma and nonseminoma were equal in percentage, cryptorchidism reaching up to 24% of all cases and the majority of cases were in advanced disease status at presentation.[7,8] This is confirming our current national-based study verifying seminoma in 41% and nonseminoma in 45% of the cases but cryptorchidism reaching only 4.58%. This discrepancy may be related to the patterns of referral as well as the fact that these results are noncurrent and verifying hospital-based data. An abstract delivered at the Saudi annual conference 1989 from Aramco Health Center Dhahran, East region reported 14 cases of testis cancer over a period of 8 years (1981–1988). They found seminoma in 64% and nonseminoma 36% with 2 children among the nonseminomas.[9] Another report from the same region studied 19 cases of testicular cancer over a period of 4 years (2006–2009), half of the cases were seminoma and the other half were nonseminomas, while the form of clinical presentation were reported to be scrotal mass in 58%, abdominal mass in 26% and others in 16%.[10] This reflects again the pattern of referral in the East region and the hospital-based data. Two abstracts from the West region reporting on 42 cases of testis cancer over a period of 11 years (2000–2010), where seminoma making 62% and nonseminoma 38%.[11,12] Al Zahrani et al. presented an alarming abstract in the year 2000 from KFSH examining the compliance of seven patients with testis cancer on surveillance, the investigators concluded, that none of the patients complied with their planned protocol schedule.[13] Talic et al. reported in an interesting paper on the low prevalence (0.82%) of intratubular germ cell neoplasia of the testis in Saudi patients, particularly in the high-risk group of patients with cryptorchidism.[14] Finally, El-Hsseiny studied 270 cases of testicular cancer from KFSH Riyadh (1975–1997) and found 13% of the cases having tumors in undescended testis and 85% of the tumors are seminomas.[15] This rate is much higher than our rate of 4.58% and also more than the current rate at KFSH of 9.0% (unpublished data), keeping in mind that more than 85% of testicles reaching the pathology lab were not labeled as descended or undescended (C629, ICD-0-3). The reported rate of tumors in undescended testes from the states is 5.83%.[16] The reason for this discrepancy may be related to the referral effect and the noncurrent data of El-Hsseiny study, where at that time a certain number of adolescent/adult are frequently submitted for orchidopexy, and most of these cases occurred during the first decade (1994–2003). Since then, early referral of children for orchidopexy has been improved all over the country although not reaching the optimal age on referral, as recently discussed by Neel.[17]
To the best of our knowledge, the current study is the first article reporting population-based national data on testicular cancer from Saudi Arabia. We describe the largest reported series to date of this rare tumor in Saudi Arabia and provide contemporary epidemiological and histopathological data. The current study confirms the increasing incidence of testicular cancer with doubling observed during the last decade, which is following the rising trend worldwide.[18] The increment in incidence of testicular cancer was also reported from most neighboring Gulf Cooperation Council states.[19] The most affected age group of 20–34 years is keeping well with published series globally. While testis cancer is the most common cancer in young, middle-aged men in Western countries,[20] it is the most common solid malignancy in 20–34-year-old Saudi men, as lymphoma and leukemia are prevalent, they occupy the top of the list [Table 3]. The germ cell tumors in our study are making only 85.4% of all testicular cancer compared to 98% reported in Western countries, which is mainly due to a higher rate of paratesticular tumors (14.3%).[21] Over the studied period, more nonseminomas (44.6%) than seminomas (40.7%) were observed. A more granular look at the figures of each decade alone, we observed the dominance of seminoma over the first decade (70.4%) and of the nonseminoma over the second decade (65.9%). This remarkable phenomenon which is also observed in the pediatric counterpart warrants further clarification. The most common subtype of seminomas is the classic form (94%), while the spermatocytic and anaplastic forms are present in 3% each, which is equivalent to reported series. Comparing the distribution of the subtypes of the nonseminomas with that of Western countries, we found several dissimilarities [Table 2]. A higher incidence of yolk sac tumor (9.2%) and germinomas (6.7%) was observed, and a lower rate of embryonal cell carcinoma (14.9%) and choriocarcinomas (3.6%) was noted.[22] Lymphomas (34.7%) and rhabdomyosarcomas (23.6%) are occupying the top of the paratesticular tumors list, which is much higher than published series.[23] The SEER summary stage of seminoma was localized in 61.6%, regional in 19.8% and distant in 12.6%, while of nonseminoma was 48%, 15.5%, and 28.5%, respectively. These figures are corroborating the more aggressive course of the nonseminomas compared to seminomas, which is a universal circumstance worldwide.[24] The advanced stage of the disease at presentation particularly in seminoma is confirming the delayed detection of the disease as compared to global series. Regrettably, a modest stage improvement was observed only in seminoma during the studied period, which unfortunately was not seen in nonseminoma.
The current study has some limitations. Varies important clinical features are not captured by the SCR, which limited the outcome of the study. Unfortunately, we were unable to report on the mode of patient presentation, the modality of treatment applied and updated survival and mortality data of the followed-up patients. Despite the limitations, our study has several strengths. The data delivered is the first published national figures on testicular cancer in Saudi Arabia extending over a period of two decades. The population-based data from the SCR include almost all patients diagnosed with testicular cancer nationwide. One advantage of population-based registries is that they provide the opportunity to compile a large number of cases of a given rare condition. In addition, we collected and evaluated as a reference the data on all Saudis with testis cancer accrued from 1976 to 2013 at the main referral cancer center in the country, namely the KFSH Riyadh. We anticipate that the data identified in this study will serve as a useful platform for further investigation on testicular cancer among Saudis and should urge the researcher to strive for more innovative research covering this understudied nonetheless steadily increasing urological cancer in our country. Hopefully, the newly created Saudi Cancer Center will ultimately proceed to establish, implement and supervise nationwide imperative current practice guidelines to enhance the detection, diagnosis, and treatment of all cancer and ensure the execution of these arrangements by transferring guidelines into practice such as, the national second opinion network for testicular cancer patients, which has been successfully implemented in Europe.[25,26] The Saudi pioneer work on management guidelines for testicular germ cell tumors has already been launched in 2014.[27]
CONCLUSIONS
The incidence rate is on rising with doubling observed during the last decade. The most affected age group was 20–34 years. Noteworthy was the dominance of the seminomas in the first decade and of the nonseminomas in the second decade. Paratesticular tumors rate is high, third of which were lymphomas. Compared to data from Western countries, notably, there is a high rate of yolk sac tumors and germinomas and a low incidence of choriocarcinomas and embryonal carcinomas. In general, late presentation of all testicular cancer was noted, although a modest stage improvement over the studied period was observed in seminomas, not in nonseminomas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The requested raw data of this study on testicular cancer were kindly approved and made available by the SCR office at the Council of Health Services and the Oncology Center at the KFSH Riyadh. Our acknowledgment to Miss. Lama Abomelha for the technical help by preparing the article.
REFERENCES
- 1.Shanmugalingam T, Soultati A, Chowdhury S, Rudman S, Van Hemelrijck M. Global incidence and outcome of testicular cancer. Clin Epidemiol. 2013;5:417–27. doi: 10.2147/CLEP.S34430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cancer Incidence Report Saudi Arabia 2013, June 2016, Saudi Cancer Registry, Council of Health Services, Ministry of Health, KSA. [Last accessed on 2016 Dec 06]. Available from: http://www.scr.org.sa .
- 3.Huyghe E, Matsuda T, Thonneau P. Increasing incidence of testicular cancer worldwide: A review. J Urol. 2003;170:5–11. doi: 10.1097/01.ju.0000053866.68623.da. [DOI] [PubMed] [Google Scholar]
- 4.Abomelha M, Al Zahrani H. Compiled abstracts proceeding of the 1st-23rd Saudi urological conferences (SUCs) 1983-2011, part 3: Urological cancer. Urol Ann. 2016;8(Suppl 1):S74–7. [Google Scholar]
- 5.Hanna N, Timmerman R, Foster R, Roth B, Einhom L, Nichols C. Epidemiology of testicular cancer. In: Bast RC, Gansler TS, Holland JF, editors. Holland-Frei Cancer Medicine. 6th ed. Hamilton, ON: BC Decker; 2003. [Google Scholar]
- 6.Ekbom A, Akre O. Increasing incidence of testicular cancer – Birth cohort effects. APMIS. 1998;106:225–9. doi: 10.1111/j.1699-0463.1998.tb01340.x. [DOI] [PubMed] [Google Scholar]
- 7.Bissada NK, el Senoussi M, Hanash KA, Hefty T, Morcos R. Testicular seminomas in Saudi Arabia: Clinical characteristics, prognostic indicators, and recommendations for management. J Surg Oncol. 1986;33:136–9. doi: 10.1002/jso.2930330218. [DOI] [PubMed] [Google Scholar]
- 8.el-Senoussi MA, Bissada NK, el-Akkad S, Bedikian AY, Morcos R, Bull C. Epidemiology and clinical characteristics of testicular tumors in Saudi Arabia: King Faisal Specialist Hospital and Research Centre experience. J Surg Oncol. 1987;35:39–41. doi: 10.1002/jso.2930350109. [DOI] [PubMed] [Google Scholar]
- 9.Rabadi S, Ayyat F, Milad M. Testicular cancer at Aramco Dhahran Health Center. Urol Ann. 2016;8(Suppl 1):S74. [Google Scholar]
- 10.Darwiche F, Gomha MA, Al-Mousa R, Al-Oraifi I, Jad A, Khan I, et al. Testicular tumors: King Fahad Specialist Hospital, Dammam experience. Urol Ann. 2016;8(Suppl 1):S76. [Google Scholar]
- 11.Barayan G, Farsi H, Nassir A, Salawi R, Saada H. Testicular cancer at KFSH&RC-Jeddah, Saudi Arabia: Importance of clinical features. Urol Ann. 2016;8(Suppl 1):S76. [Google Scholar]
- 12.Barayan G, Farsi H, Nassir A, Saada H, Almuhaisin T, Madani H. Testicular tumor patients at KFSH&RC-Jeddah and National Guard Hospital, Jeddah, Saudi Arabia: Disease features. Urol Ann. 2016;8(Suppl 1):S77. [Google Scholar]
- 13.Al Zahrani H, Bogmi E, Lindstedt E, Kattan S, Kardar AH, Merdad T, et al. Compliance of Saudi patients with testicular cancer on surveillance. Urol Ann. 2016;8(Suppl 1):S74. [Google Scholar]
- 14.Talic RF, Al-Rikabi AC, Al-Rayess MM. Prevalence of intratubular germ cell neoplasia of the testis. Saudi Med J. 1999;20:706–10. [PubMed] [Google Scholar]
- 15.El-Hsseiny G. Germ cell tumors in undescended testis: Prognostic factors and treatment outcome. J Egypt Natl Cancer Inst. 2001;13:209–214. [Google Scholar]
- 16.Gullett NP, Masterson TA, Johnstone PA. Germ cell tumors of undescended vs. descended testes: Population-based clinical and outcome data. J Clin Urol. 2012;5:236–40. [Google Scholar]
- 17.Neel KF. Orchidopexy for undescended testis among Saudi children: Is it conducted at the optimal age? Curr Pediatr Res. 2010;14:39–41. [Google Scholar]
- 18.Znaor A, Lortet-Tieulent J, Jemal A, Bray F. International variations and trends in testicular cancer incidence and mortality. Eur Urol. 2014;65:1095–106. doi: 10.1016/j.eururo.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 19.Cancer Incidence among Nationals of the GCC States 1998-2009, Gulf Center for Cancer Control and Prevention (GCCCP), King Faisal Specialist Hospital and Research Centre. 2013 Dec;:26–31. [Google Scholar]
- 20.Khan O, Protheroe A. Testis cancer. Postgrad Med J. 2007;83:624–32. doi: 10.1136/pgmj.2007.057992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Motzer RJ, Jonasch E, Agarwal N, Beard C, Bhayani S, Bolger GB, et al. Testicular cancer, version 2.2015. J Natl Compr Canc Netw. 2015;13:772–99. doi: 10.6004/jnccn.2015.0092. [DOI] [PubMed] [Google Scholar]
- 22.Carver BS. Testicular cancer. In: Gomella LG, editor. The -Minute Urology Consult. 3rd ed. Philadelphia: Wolters Kluwer; 2015. pp. 486–511. [Google Scholar]
- 23.Trabert B, Chen J, Devesa SS, Bray F, McGlynn KA. International patterns and trends in testicular cancer incidence, overall and by histologic subtype, 1973-2007. Andrology. 2015;3:4–12. doi: 10.1111/andr.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rosen A, Jayram G, Drazer M, Eggener SE. Global trends in testicular cancer incidence and mortality. Eur Urol. 2011;60:374–9. doi: 10.1016/j.eururo.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 25.Zengerling F, Krege S, Schrader AJ, Schrader M. National second opinion network for testicular cancer patients – Transferring guidelines into practice! Aktuelle Urol. 2014;45:454–6. doi: 10.1055/s-0034-1395624. [DOI] [PubMed] [Google Scholar]
- 26.Schrader M, Weissbach L, Hartmann M, Krege S, Albers P, Miller K, et al. Burden or relief: Do second-opinion centers influence the quality of care delivered to patients with testicular germ cell cancer? Eur Urol. 2010;57:867–72. doi: 10.1016/j.eururo.2009.10.032. [DOI] [PubMed] [Google Scholar]
- 27.Alotaibi M, Saadeddin A, Bazarbashi S, Alkhateeb S, Alghamdi A, Alghamdi K, et al. Saudi oncology society and Saudi urology association combined clinical management guidelines for testicular germ cell tumors. Urol Ann. 2016;8:141–5. doi: 10.4103/0974-7796.179240. [DOI] [PMC free article] [PubMed] [Google Scholar]


