Abstract
Objective:
To demonstrate a benefit in diminished adverse events such as hypotension and hematuria with gradual drainage of the bladder when compared to rapid decompression in patients with acute urinary retention (AUR) due to benign prostatic hyperplasia in a case–control study.
Methods:
Sixty-two patients matched our selection criteria presenting with AUR. They were divided into two groups – the first was managed by rapid drainage of the bladder, the second was managed by gradual drainage through a urethral catheter (The first 100 mL immediately evacuated, then the rest evacuated gradually over 2 h).
Results:
The mean age was 64.4 and 63.2 years in the first and second group, respectively. Diagnosed cause was benign hyperplasia of the prostate. Hematuria occurred in two patients in the first group and none in the second group. The two cases of hematuria were mild and treated conservatively. After the relief of the obstruction, the mean blood pressure was noticed to decrease by 15 mmHg and 10 mmHg in the first and second group, respectively, however, no one developed significant hypotension. Pain relief was achieved after complete drainage in the first group and after the evacuation of 100 mL in the second group.
Conclusions:
We conclude that there is no significant difference between rapid and gradual decompression of the bladder in patients with AUR. Hematuria and hypotension may occur after rapid decompression of the obstructed urinary bladder, but these complications are rarely clinically significant.
Keywords: Benign prostatic hyperplasia, prostate, retention
INTRODUCTION
Acute urinary retention (AUR) is a common urological emergency in men and is defined as a sudden and painful inability to pass urine voluntarily. It represents a significant worldwide health issue. The annual incidence of primary AUR varies from 2.2 to 6.8/1000 men, according to the series by Jacobsen et al. 1997,[1] Meigs et al. 1999,[2] Verhamme et al. 2005,[3] and Cathcart et al. 2006.[4]
The immediate management of AUR involves bladder decompression by catheterization. The catheter (urethral or suprapubic) may be inserted at a general practice or hospital, with follow-up treatment varying according to local policy.[5]
Hematuria, hypotension, and postobstructive diuresis can occur after bladder drainage by catheter, and the risk of these complications has been thought to be increased when the bladder is rapidly decompressed; however, there are reports supporting gradual bladder decompression to avoid hematuria, hypotension, and postobstructive diuresis, the evidence is overall weak.[6,7,8] Therefore, rapid and complete emptying of the bladder is generally recommended and practiced widely.
The standard treatment of AUR at our hospital is gradual decompression. As it is also a training hospital, there have been instances of inadvertent rapid drainage of the bladder due to accidental late clamping of the urethral catheter. No adverse events were seen in these instances, which led to considering this trial at our institution.
Our goal was to compare rapid versus gradual decompression of the bladder in patients with AUR. A comparison was made regarding effectiveness treatment and adverse events. The effectiveness of treatment was evaluated by pain relief and resolution of the urine retention. The adverse events evaluated were hematuria and hypotension.
METHODS
Sixty-two patients matched our selection criteria presenting with AUR.
Our selection criteria for AUR were:
Presentation of painful urinary retention with bladder distension
Presumptive diagnosis of benign prostatic hyperplasia from history at admission
This was confirmed after admission
Exclusion of other causes of urinary retention such as infections, trauma, or surgery
Exclusion of other life-endangering condition on admission such as cardiac patients.
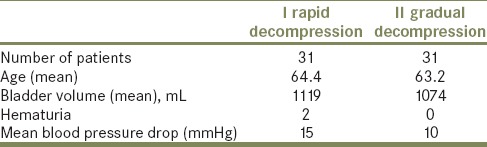
These 62 patients were randomized into two groups of 31 as shown in Table 1:
Table 1.
Study groups
The first group (rapid decompression) was managed by rapid drainage of the bladder
The second group (gradual decompression) was managed by gradual drainage using an IV giving set as suggested by Perry et al.[9] An intravenous line is connected between the urethral catheter and the drainage bag. The required slow bladder decompression is ensured by the roller of the giving set, which can also be used to control the rate of drainage[9] (The first 100 mL were immediately evacuated, then the rest was evacuated gradually in 2 h).
A Foley was used for urethral catheterization. The bladder is catheterized in the normal way under aseptic conditions using a two-way Foley catheter.
Patients were evaluated for pain (treatment success), hematuria, and hypotension. Pain was assessed as present or absent. The assessment was done using pain analog score.
Blood pressure was obtained using a standard blood pressure cuff with the patient in a dorsal decubital position.
Results were analyzed using Chi-square analysis, Fisher's exact test, and Student's t-test.
RESULTS
The mean age was 64.4 and 63.2 years in the first and second group, respectively. The final diagnosis was benign hyperplasia of the prostate. The mean bladder volumes before decompression were in the range of 1119 ± 233 mL and 1074 ± 214 mL in the first and second groups, respectively. The difference was not significant between the two groups.(P = 0.97)
The results are summarized in Table 1. Hematuria occurred in two patients in the first group and none in the second group. The two cases of hematuria were mild and treated conservatively. The difference was not statistically significant.
After the relief of the obstruction, the mean blood pressure was noticed to decrease by 15 mmHg and 10 mmHg in the first and second group, respectively, however, no one developed hypotension. The difference in blood pressure drop observed in the two groups was also not statistically significant.
Pain relief was achieved after complete drainage in the first group and initially after evacuation of 100 mL in the second group.
DISCUSSION
Initial management of urinary tract obstruction, specifically the rate of release of the retained urine, has been debated for decades. The two primary methods to empty the obstructed bladder are rapid, complete emptying or gradual, slow emptying.
Gradual release of the obstructed bladder continues to be recommended as the method of choice based on a theory that slow decompression of the intrabladder pressure will reduce the rate of complications, specifically hematuria and hypotension.[6,7,10] Although there is no evidence to support its recommendation.
Although there is no significant complications were reported with either method. Results of fractionated release were similar to those of quick release - an initial, sudden decrease in intravesical pressure followed by minimal further reduction in pressures. Therefore, to effect gradual reductions in intrabladder pressures, <50 mL of urine should be released from the bladder.
The two most concerning complications of relief of AUR are hematuria and hypotension.
Hematuria as a complication of the release of urinary tract obstruction has been a concern for many years. Quick, complete emptying of the bladder has been thought to be a predisposing factor for hematuria.
Various mechanisms have been suggested to explain the onset of hematuria after quick, complete emptying of the bladder, all based on sudden decompression causing injury to the urinary tract and resulting in hemorrhage.
This theory, however, ignores the possibility of other etiologic factors contributing to the occurrence of hematuria, such as infection and iatrogenic trauma. Alternatively, animal studies suggest that hematuria develops as a result of bladder wall damage that occurs before catheterization. Therefore, the rate of release is unrelated to the onset of hematuria. In addition, some investigators believe that gradual decompression blunts the vesicovascular reflex and avoids subsequent hypotension.
In studies of quick, complete emptying, hematuria occurred in 2% to 16% of patients. None of these studies, however, reported any episodes of severe hematuria, In addition, none of the studies found an association between the evacuated initial bladder volume and the risk of hematuria.[5,11,12,13,14,15,16]
Hypotension and circulatory collapse after emptying of the obstructed bladder have been reported.[17]
The systemic blood pressure is increased by the urinary vesicovascular reflex in response to acute urinary distention and pain.[12,13] Taylor,[12] in studies of bladder emptying in animals and humans, showed that a sudden reduction in bladder wall tension reflexly produced vasodilatation with a concomitant decrease in blood pressure. Taylor concluded that a reduction in blood pressure occurs with no serious clinical consequences when a patient has healthy cardiovascular and nervous systems. These studies demonstrate a decrease in systemic blood pressure with quick, complete emptying; however, the actual change in blood pressure within normal blood pressure range.
We gradually evacuated the bladder by 100 mL initially; this was supported by two studies which have quantified the decrease in intrabladder pressure as a function of released volume.[14,18] These investigations have shown a decrease in intravesical pressure of approximately 50% with removal of the first 100 mL of urine. After this initial substantial decrease in pressure, the intravesical pressure declines only slightly.
CONCLUSIONS
We conclude that there is no significant difference between rapid and gradual decompression of the bladder in patients with AUR. Hematuria and hypotension may occur after rapid decompression of the obstructed urinary bladder, but these complications are rarely clinically significant.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jacobsen SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, Guess HA, et al. Natural history of prostatism: Risk factors for acute urinary retention. J Urol. 1997;158:481–7. doi: 10.1016/s0022-5347(01)64508-7. [DOI] [PubMed] [Google Scholar]
- 2.Meigs JB, Barry MJ, Giovannucci E, Rimm EB, Stampfer MJ, Kawachi I. Incidence rates and risk factors for acute urinary retention: The health professionals followup study. J Urol. 1999;162:376–82. [PubMed] [Google Scholar]
- 3.Verhamme KM, Dieleman JP, van Wijk MA, Bosch JL, Stricker BH, Sturkenboom MC. Low incidence of acute urinary retention in the general male population: The triumph project. Eur Urol. 2005;47:494–8. doi: 10.1016/j.eururo.2004.11.011. [DOI] [PubMed] [Google Scholar]
- 4.Cathcart P, van der Meulen J, Armitage J, and Emberton M. Incidence of primary and recurrent acute urinary retention between 1998 and 2003 in England. J Urol. 2006;176:200–4. doi: 10.1016/S0022-5347(06)00509-X. [DOI] [PubMed] [Google Scholar]
- 5.Emberton M, Fitzpatrick JM. The Reten-World survey of the management of acute urinary retention: Preliminary results. BJU Int. 2008;101(Suppl 3):27–32. doi: 10.1111/j.1464-410X.2008.07491.x. [DOI] [PubMed] [Google Scholar]
- 6.Fontanarosa PB, Roush WR. Acute urinary retention. Emerg Med Clin North Am. 1988;6:419–37. [PubMed] [Google Scholar]
- 7.Martinez-Maldonado M, Kumjian DA. Acute renal failure due to urinary tract obstruction. Med Clin North Am. 1990;74:919–32. doi: 10.1016/s0025-7125(16)30526-0. [DOI] [PubMed] [Google Scholar]
- 8.Stine R, Chudnofsky CA. Practical Approach to Emergency Medicine. 2nd ed. Boston: Little, Brown; 1994. [Google Scholar]
- 9.Perry A, Maharaj D, Ramdass MJ, Naraynsingh V. Slow decompression of the bladder using an intravenous giving set. Int J Clin Pract. 2002;56:619. [PubMed] [Google Scholar]
- 10.Blandy J. Emergency situations: Acute retention of urine. Br J Hosp Med. 1978;19:109–11. [PubMed] [Google Scholar]
- 11.Nyman MA, Schwenk NM, Silverstein MD. Management of urinary retention: Rapid versus gradual decompression and risk of complications. Mayo Clin Proc. 1997;72:951–6. doi: 10.1016/S0025-6196(11)63368-5. [DOI] [PubMed] [Google Scholar]
- 12.Taylor DE. Viscero-vascular reflexes and the surgical patient. J R Coll Surg Edinb. 1966;12:61–7. [PubMed] [Google Scholar]
- 13.Lapides J, Lovegrove RH. Urinary vesicovascular reflex. J Urol. 1965;94:397–401. doi: 10.1016/S0022-5347(17)63638-3. [DOI] [PubMed] [Google Scholar]
- 14.Osius T, Hinman F., Jr Dynamics of acute urinary retention: A manometric, radiographic and clinical study. J Urol. 1963;90:702–12. [Google Scholar]
- 15.Glahn BE, Plucnar BJ. Quick complete emptying of the bladder in 300 cases of urinary retention. The occurrence of haematuria. Dan Med Bull. 1984;31:68–70. [PubMed] [Google Scholar]
- 16.Paquin JM, Perreault JP, Faucher R, Mauffette F, Berlinguet JC. Treatment of the acute phase of urinary retention (author's transl) J Urol (Paris) 1981;87:37–8. [PubMed] [Google Scholar]
- 17.O’Conor V. Observations on the blood pressure in cases of prostatic obstruction. Archives of Surgery. 1920;1:2:359–67. [Google Scholar]
- 18.Christensen J, Ostri P, Frimodt-Møller C, Juul C. Intravesical pressure changes during bladder drainage in patients with acute urinary retention. Urol Int. 1987;42:181–4. doi: 10.1159/000281891. [DOI] [PubMed] [Google Scholar]


