The US healthcare system is in a period of unprecedented change. The threats posed by increasing healthcare costs and the growing consensus that much of current spending is wasted[1] have stimulated a broad array of public and private initiatives aimed at improving care and lowering costs: new technologies, increased investments in patient centered outcomes research (PCOR); public reporting on the quality and cost of care; pay for performance initiatives; and continued efforts to adopt value-based payment models. The health system has responded. For example, the number of Accountable Care Organizations (ACOs) has increased from a handful in 2009 to 775 at the present time.[2]
However, not every change is an improvement. Understanding which of the multitude of technological, policy and organizational changes underway are most effective at improving care will be critical if the nation is to achieve the goals of better, less expensive care and greater population health. In this Viewpoint, we describe three ideas that could be helpful: application of a well-grounded conceptual framework; distinguishing three distinct types of innovations that health systems are using to improve care; and a focus on building the information systems needed to accelerate timely learning.
A FRAMEWORK DRAWN FROM IMPLEMENTATION SCIENCE
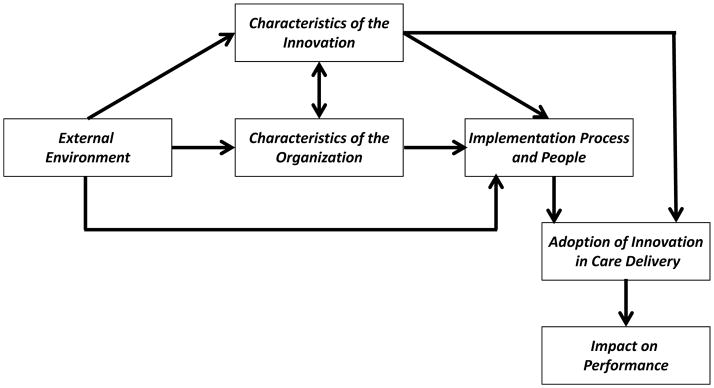
The emerging field of implementation science focuses on understanding how change takes place. Damschroder and others [3] identified four main groups of variables that interact to influence the adoption of innovations (see Figure): the external environment (e.g. new payment models); the structure of the organization (e.g. integrated delivery system); the characteristics of the innovation (e.g. the strength of the evidence supporting it); and the processes used (e.g. bottom up versus top down decision-making).
Figure. Framework for Analyzing the Adoption of Innovations.
Examples of attributes that influence the adoption of innovations
Environment: policies, market structure, incentives, network structure
Organization: structure, resources, capabilities, professional network structure
Implementation: incentives, management processes, use of peer norms
Innovation: quality of evidence, financial attributes, modes of delivery
While most attention is focused on how to more quickly adopt and spread innovations that will benefit patients, the framework can also be used to help understand how organizations eliminate treatments, practices, and policies that do not benefit patients, referred to as “exnovation”. Organizations that can do this better than others need to be identified and how they successfully accomplished ‘exnovation’ described.
WHAT KIND OF INNOVATION IS BEING IMPLEMENTED?
Different decision-makers and stakeholders are likely to be involved in three different types of innovations: biomedical innovations; changes in care delivery; and new ways of engaging patients in their own care.
Biomedical innovations are targeted at specific biologic or pathophysiologic abnormalities or problems. Examples include new medications, new technologies (such as implantable cardioverter-defibrillators), and new surgical treatments (new surgical approaches to joint replacement). Applications of these innovations are the traditional focus of clinical comparative effectiveness research and “evidence-based” practice. Physicians are the primary decision-makers about whether and to whom these interventions should be offered, whether at the point of care or in the administrative offices of payers faced with a coverage decision. Adoption and implementation decisions are highly influenced by the magnitude of benefit and the quality of the evidence
Care delivery innovations focus on groups of patients defined not by their pathophysiology but by factors such as the site of care (primary care practice) or the complexity of their clinica7l situation ( complex chronic illness). Examples include adoption and spread of team based primary care, case management for complex patients, and quality improvement initiatives. Although front-line physicians and the patients for whom they provide care are affected by these innovations, decision-making about their use is the primary responsibility of practice managers (whether clinicians or administrators) and organizational leaders. Implementation of care delivery innovations is often complex because they engage diverse individuals from different organizational levels and sometimes beyond. Existing evidence suggests that such innovations have substantial potential to improve care and reduce costs[4] and, therefore, the implementation science framework can be used to identify the barriers to their successful implementation and strategies for overcoming them.
The growing interest in patient engagement innovations rests largely on two observations: recognition that the increasing burden of chronic illness in the U.S. population cannot be addressed without engaging patients and their caregivers in effective self-care, behavior change and chronic disease management; and the need to better align treatment choices with patients’ well-informed preferences and values through shared decision-making. These changes in practice involve a fundamental change in the historical framework of the physician as expert and the patient as passive recipient relationship. As such, a comprehensive framework such as that offered by implementation science is needed to identify the ways in which such patient engagement strategies can be adopted and spread throughout the healthcare system. For example, at Intermountain Healthcare the framework is being used to implement patient reported measures ( PRMs) to support collaborative treatment planning with patients.
DATA – AND DATA LINKAGE TO ACCELERATE LEARNING
The effective application of this framework will require much better and more timely information on each of the domains in the figure, including whether innovations are actually being used (and by whom) and the influence of the innovations on the quality, outcomes and costs of care. One approach is to draw on national data sets, such as Medicare and private payer claims data, complemented by existing or new surveys of healthcare organizations. Such national data can provide important insights, but are likely to lack key information, including details about exactly how innovations were implemented, especially at the level of individual clinical practices within organizations and, importantly, detailed clinical information such as lab results, biometrics or patient reported outcomes.[5]
A complementary approach is to build on the more detailed data being assembled and used by health care organizations participating in emerging learning networks, such as the HMO research network, or the High Value Healthcare Collaborative. In the latter, system leaders are working to accelerate learning relevant to their strategic priorities to improve care and lower costs, providing an incentive for accurate data collection and a commitment to more robust quality and outcome measures. These efforts, however, involve several data challenges,[6] including insufficient data standards, lack of interoperability across EHR systems and the varying and inconsistent approaches to capturing patient and care-related data.
Strategies for overcoming some of these challenges have been devised[7] including standardized approaches to handling missing data, text-based vs. coded data entries, and out-of-range entries. Implementing such approaches is critical because the application of the implementation science framework depends upon the effective quilting together of data elements from multiple sources—i.e., linking claims with EHR and survey data—over time and across vendor and homegrown systems. In addition, expanded data collection of patient reported measures, which is essential to understanding whether care is improving on dimensions important to consumers, presents unique challenges in harmonizing measures and understanding the effects of varying approaches to data collection and recording. Insights from successful data development and linkage initiatives can provide guidance on how best to accelerate the development of information systems capable of capturing the information highlighted in the framework to support rapid-cycle learning and improvement. For example, pooling multicenter data provides sufficient power to rapidly establish evidence-based appropriateness criteria to support targeted shared decision-making for patients being considered for total knee arthroplasty.
CONCLUSION
Since innovations that work in one context will not necessarily work in another, stakeholders need granular information about what works, for whom, and in what contexts. Implementation science offers a helpful framework for accelerating the learning necessary to drive improvement.
Acknowledgments
The authors acknowledge others who contributed to our thinking as co-investigators in the AHRQ Center of Excellence award upon which this viewpoint is based including: Julie Bynum, Carrie Colla, Taressa Fraze, Valerie Lewis, Ellen Meara, James O’Malley, Meredith Rosenthal, Anna Tosteson, Hector Rodriguez and Nilay Shah.
This work was supported in part by a grant from the Agency for Health Care Research and Quality #1U19HS024075. The opinions are those of the authors.
Contributor Information
Elliott S. Fisher, Director, The Dartmouth Institute for Health Policy & Clinical Practice, John E. Wennberg Distinguished Professor, Geisel School of Medicine at Dartmouth, Phone: 603-653-0802, WTRB, Level 5, 1 Medical Center Drive, Lebanon, NH 03756.
Stephen M. Shortell, Blue Cross of California Distinguished Professor of Health Policy and Management, Director, Center for Healthcare Organizational and Innovation Research (CHOIR), Dean Emeritus, School of Public Health, Professor of Organization Behavior, Haas School of Business, University of California, Berkeley, Phone: 510-643-5346, 140 Warren Hall, Rm 19, Berkley, CA 94720.
Lucy A. Savitz, Director, Center for Health Research, Vice President, Health Research, Kaiser Permanente, Phone: 503-335-2400, 38000 N. Interstate Avenue, Portland, OR 97227-1098.
References
- 1.Berwick DM, Hackbarth AD. Eliminating waste in US health care. Jama. 2012;307(14):1513–6. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- 2.Petersen M, et al. Growth and dispersion of accountable care organizations: June 2014 update. 2014. [Google Scholar]
- 3.Damschroder LJ, et al. Fostering Implementation of Health Services Research Findings Into Practice: A Consolidated Framework for Advancing Implementation Science. Implementation Science. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milstein A, Shortell S. Innovations in care delivery to slow growth of US health spending. JAMA. 2012;308(14):1439–1440. doi: 10.1001/jama.2012.12659. [DOI] [PubMed] [Google Scholar]
- 5.Cassel CK, Kronick R. Learning From the Past to Measure the Future. JAMA. 2015;314(9):875–6. doi: 10.1001/jama.2015.9186. [DOI] [PubMed] [Google Scholar]
- 6.Hubbard T, et al. An Evolving Landscape: Comparative Effectiveness Research, Outcomes Research and Care Innovation. 2014. NEHI Issue Brief. [Google Scholar]
- 7.Bayley KB, et al. Challenges in using electronic health record data for CER: experience of 4 learning organizations and solutions applied. Medical care. 2013;51:S80–S86. doi: 10.1097/MLR.0b013e31829b1d48. [DOI] [PubMed] [Google Scholar]