Abstract
The paper examines the contribution of weight status to Black-White differences in mortality at ages 40–79 using data from the National Health and Nutrition Examination Survey. We measure body mass index (BMI) based on the highest BMI attained and contrast the contribution of BMI to that of smoking and educational attainment. We estimate both additive and multiplicative models. In addition to estimating regression coefficients we ask what would happen to B-W differences in mortality if blacks had the BMI distribution of whites, the smoking prevalence of whites, or the educational distribution of whites. B-W differences in BMI account for close 30 percent of the B-W difference in female mortality but only about 1 percent of the B-W difference in male mortality at ages 40–79. In contrast, smoking makes a much larger contribution to the B-W difference in male (17 percent) than female (6 percent) mortality. Differences in educational attainment in turn explain 19 to 25 percent of the B-W mortality difference among men and women, respectively. Our results underscore the importance of two key risk factors as well as educational attainment in generating B-W differences in mortality.
Introduction
Black-white (B-W) mortality differences in the United States are sizable and persistent, posing a significant, longstanding public health concern. The B-W gap in life expectancy at birth has fluctuated over time, and despite its recent narrowing, the gap remains large (Harper et al. 2014). In 2010, the non-Hispanic black male life expectancy at birth (71.4 years) was 5.0 years lower than that of non-Hispanic white males (76.4 years). The respective gap for women was 3.4 years (77.7 [blacks] and 81.1 years [whites]). At age 50, to which 89–93% of non-Hispanic black and white men and 93–96% of non-Hispanic black and white women survive, the gap remained sizable at 3.4 years for men and 2.2 years for women (Arias 2014).
In 2008, mortality from cardiovascular diseases and diabetes together accounted for 38% of the B-W life expectancy gap at birth among men and 54% among women (Harper et al. 2012). Two well-known behavioral risk factors, smoking and obesity, are significant risk factors for mortality from these causes. Ho and Elo (2013) investigated the contribution of smoking to B-W differences in mortality above age 50 and found that smoking accounted for 20% to 48% of the difference between 1980 and 2005 among men, but smoking did not explain B-W difference in mortality among women. Several studies have examined the contribution of obesity to mortality among whites and blacks in the United States (Abell et al 2008; Cohen et al. 2012), but these studies have not explicitly measured the contribution of obesity to B-W differences in mortality.
Black Americans have a higher prevalence of obesity than white Americans. Using measured heights and weights in the 2013–2014 National Health and Nutrition Examination Survey (NHANES), Flegal et al. (2016: Table 2) estimated the prevalence of age-standardized obesity (BMI ≥ 30) above age 20 to be 57.2% (95%CI:52.9–61.3) among non-Hispanic black women compared to 38.2% (95%CI:31.3–38.1) among non-Hispanic white women. Comparable male figures are 38.0% (95%CI: 32.7–43.5) and 34.7% (95%CI: 31.3–38.1).
Obesity is a major risk factor for diabetes and cardiovascular disease (Abdullah et al. 2011, 2014; Tarleton et al. 2014). The higher prevalence of obesity among blacks may explain why blacks at ages 20 and above are more than twice as likely to have diagnosed or undiagnosed diabetes and are more likely to be hospitalized for diabetes-related diseases compared to whites (Centers for Disease Control 2014; Chow et al. 2012; Selvin et al. 2014). Blacks also have a higher prevalence of cardiovascular disease than whites, especially among women. In 1999–2006, the B-W age-adjusted prevalence ratio of self-reported cardiovascular disease (heart failure, stroke and myocardial infarction) at ages 35 and above was 1.6 for women and 1.2 for men. The ratios were larger at younger than at older ages (Jolly et al. 2010: Table 3).
In this paper, we examine the contribution of weight status to B-W differences in mortality at ages 40–79 and extend prior research in several ways. First, instead of measuring body mass index (BMI) at the start of the mortality follow-up (“baseline” BMI), we use the highest BMI attained, “maximum BMI,” that has proven to be a better predictor of excess risk of death than baseline BMI in prior studies (Mehta et al. 2014; Stokes and Preston 2016a, 2016b). Second, we use both additive and multiplicative models to investigate the contribution of obesity to B-W difference in mortality. Third, we estimate what fraction of the excess mortality among blacks can be explained by the B-W difference in the maximum BMI distribution by gender. Fourth, we compare the contribution of weight status to that of smoking in the B-W difference in mortality at ages 40–79. Fifth, we compare the contributions of obesity and smoking to the B-W difference in mortality with that of educational attainment.
B-W Differences in the Risk of Death Associated with Obesity
While ample evidence indicates that obesity increases the risk of death, there is conflicting evidence about whether this risk is equally damaging for blacks and whites. Several studies have concluded that the risk of death associated with overweight or obesity is more pronounced for Whites than Blacks, especially among women (e.g., Adams et al. 2006; Calle et al. 1999; Cohen et al. 2012; Jackson et al. 2014; Xiao et al. 2014; Zheng and Yang 2012). Other studies show risks from obesity among black women that are similar to those observed for white women (Boggs et al. 2011; Patel et al. 2014; Park et al. 2012). In a very large sample, Patel et al. (2014) formally investigate interactions between race and BMI in predicting mortality and find them to be insignificant. Furthermore, a recent pooled analysis of seven prospective cohort studies of the association between BMI and mortality among African Americans concluded: “Obesity was associated with a higher risk of mortality [relative to normal weight] in African Americans, similar to that observed in pooled analyses of whites and East Asians” (Cohen et al. 2014: Abstract).
Possible reasons for the inconsistent findings include differences in the length of follow-up, samples analyzed (e.g., national vs. regional samples), adjustment for diseases that may be in the causal pathway between obesity and mortality, and treatment of smoking (Ibid; Boggs et al 2011; Cohen et al. 2012; Zeng and Yang 2012).
Whether the association between obesity and mortality is the same for Blacks and Whites may also depend on the type of statistical model used. Nearly all studies examining the association between weight status and mortality have used a Cox-proportional hazards model or logistic regression. Such models assume that race and BMI are multiplicative in their relation to mortality. However, a recent paper by Mehta and Preston (2016) using NHANES data concludes that race and BMI are additive rather than multiplicative in their effects on mortality. When these associations are additive, the relative risks and hazard ratios for obesity estimated from Cox proportional hazard models or discrete time logistic models will be lower for blacks, the group with higher overall mortality; the same absolute increase in mortality represents a smaller proportionate increase for Blacks than for Whites. Thus a finding that Blacks have lower hazard ratios associated with obesity than Whites may simply reflect the fact that the hazards are additive rather than multiplicative. In this paper, we use both additive and multiplicative models to investigate the contribution of obesity to B-W difference in mortality.
The Measurement of Weight Status
In the studies that have examined whether the risk of death associated with overweight and obesity is similar for Blacks and Whites, BMI is measured at the start of the mortality follow-up. Because illness is often associated with loss of weight, the presence of sick individuals in the lower weight categories can lead to underestimates of the risk of death associated with overweight and obesity (Stokes and Preston 2016a, 2016b). This source of bias, termed “reverse causation”, is likely to vary by race given that black Americans experience a higher burden of chronic disease at an earlier age than white Americans (Hayward et al. 2000; Jolly et al. 2010). Prior studies have addressed the issue by excluding the first few years of follow-up, limiting the analysis to individuals free of disease at baseline, controlling for health status and/or pre-existing chronic conditions at baseline, controlling for smoking status or limiting the analysis to never smokers (Adams et al. 2006; Boggs et al. 2011; Cohen et al. 2014; Park et al. 2012; Patel 2014). These strategies often eliminate large fractions of the population and call into question the external validity of results.
An alternative means of addressing reverse causation is to measure BMI at an earlier point in the life cycle. Using both baseline and retrospective information on height and weight collected in NHANES, Preston et al. (2013) found that BMI at age 25 and BMI at age 40 (or 10 years prior to the survey) were statistically significant predictors of mortality at ages 50 and above even in the presence of controls for BMI at the start of the mortality follow-up. Similarly, Park et al. (2012) concluded that overweight in young adulthood conferred excess risk of mortality in later life, and that this association appeared to be stronger than the association between BMI measured at an older age in a multiethnic cohort of individuals living in California and Hawaii.
Other recent research finds that the highest BMI ever attained, “maximum BMI,” regardless of the age at which it occurs, is a robust predictor of mortality. For example, Mehta et al. (2014), using data from Finland, found that the excess risk of death associated with obesity measured by maximum BMI was double the risk of obesity measured at the start of the mortality follow-up. Similarly, using NHANES data, Stokes (2014) found that among non-smokers aged 50–84 the number of deaths attributable to BMI ≥ 25.0 was 33% when it was calculated based on maximum BMI compared to only 5% when calculated based on BMI measured at the time of the survey. Stokes and Preston (2016a) use model-selection criteria AIC and BIC and show that models using maximum BMI decisively outperform those using weight measured at the time of the survey. Consistent with this finding, Framingham life cycle data show that models using duration of obesity outperform models based on baseline obesity in predicting the onset of diabetes (Abdullah et al. 2011) and cardiovascular disease (Abdullah et al. 2014). Maximum BMI has not been previously used to examine the contribution of obesity to B-W differences in mortality.
Data and Methods
We use data from the National Health and Nutrition Examination Survey (NHANES) III (1988–1994) and 1999–2010 NHANES. NHANES are a series of cross-sectional health surveys of the non-institutionalized U.S. population conducted by the National Center for Health Statistics (NCHS). The NCHS has linked each survey to the National Death Index (NDI) through December 31, 2011. Our analyses are restricted to native-born, non-Hispanic whites (whites hereafter) and native-born, non-Hispanic blacks (blacks hereafter) aged 40–69 at the time of survey (Dupre et al. 2012). Mortality is modeled up to age 80; individuals are censored when they reach age 80. We exclude individuals whose BMI was missing (N=60), below 18.5 (N=20) and 50 or above (N=166). We also exclude respondents who had missing information on educational attainment (N=18) and/or smoking (N=5). Our sample size, which combines respondents from each wave, consists of 12,291 individuals, 123,733 person-years of follow-up, and 1,749 deaths. All analyses incorporate sampling weights.
Body Mass Index (BMI) and Other Explanatory Variables
Our measure of “maximum BMI” is based on the highest weight the respondent reported ever having attained and height measured at the time of the survey (Mehta et al. 2014, Stokes 2014). In preliminary analysis, we also calculated BMI based on measured weight and height at the time of the survey and compared the results of our multivariate models using maximum BMI and baseline BMI. Similar to previous findings, we found maximum BMI to be associated with a higher relative risk of death than baseline BMI (Mehta et al., 2014; Stokes 2014; Stokes and Preston 2016a, 2016b). We report results for maximum BMI only.
We model the association between maximum BMI and mortality using BMI as a continuous variable above BMI = 25.0, the level of BMI in the beginning of the overweight range. Although the coding of BMI as a categorical variable has been the most common method of estimating the mortality risk associated with BMI, a continuous form of BMI has been shown to provide results that are much less sensitive to error in reporting weight (Preston et al. 2015). Two major pooled analyses also use a continuous linear BMI term to estimate the effect on mortality of increments in BMI above 25 (Berrington de Gonzalez et al. 2010, Whitlock et al. 2009). To capture potential non-linearity in the association between BMI and mortality, we model BMI with a second-degree polynomial. Kivimäki et al. (2008) experimented with six functional forms to represent the relation between mortality and BMI. Using the likelihood ratio statistic, they conclude that a second-degree polynomial provided the best fit.
Our measure of maximum BMI uses self-reported maximum weight. Self-reported weight is subject to random error and to downward bias (Gorber et al. 2007). However, the consequences of misreporting of weight for estimates of the association between BMI and mortality are much smaller when a continuous version of BMI is used, as in this paper, rather than a categorical variable (Preston et al. 2015).
Our other explanatory variables include age as a time-varying covariate, race (white, black), educational attainment (less than high school, high school graduate, some college, 4+ years of college), and smoking status (current, former and never smoker).
Statistical Approach
We show sample characteristics separately for white and black men and women. Our outcome variable is the probability of dying from all causes combined. As noted above, Mehta and Preston (2016) have shown that race and BMI are additive rather than multiplicative in their associations with mortality, whereas nearly all prior studies have assessed these associations between obesity, race, and mortality using Cox proportional hazard or logistic regression models. In this paper, we will estimate multivariate discrete time linear probability models in which the effects of race and BMI are additive rather than multiplicative. We repeat the analyses using multivariate discrete time logistic models that allow us to compare our results with previous studies.
In each case, we estimate three models. Model 1 contains variables representing age, race, gender, and a gender*race interaction. Model 1 establishes the excess risk of death for black men and women when only age is controlled (in 5-year intervals). In Model 2 we add educational attainment and smoking behavior to Model 1. Model 3 adds maximum BMI and maximum BMI squared to Model 2. Comparison of Models 1, 2 and 3 shows to what extent the excess risk of death associated with race is reduced when we control for maximum BMI. We also tested interactions between race and maximum BMI. These interactions were not statistically significant nor did they improve the fit of the models.
We employ two different strategies to investigate the impact of increments in BMI above 25.0 on mortality. In both strategies, our BMI variable is expressed as [Excess BMI = actual BMI minus 25.0]. In one case, we employ all individuals with a BMI of 18.5–50.0 and assign those with a BMI below 25.0 the value of zero, reflecting the fact that they are not above the “normal” BMI range. In the other case, we limit analysis to those with BMI above 25.0, which requires no assumption about the risk associated with BMI for the population below 25.0. Since we are aiming at making inferences about the entire population, we emphasize the former set of results and use the latter set as a confirmatory check.
In addition to estimating the effect of BMI on regression coefficients that indicate the excess mortality of black men and women, we use a counterfactual approach. We ask what would happen to B-W differences in mortality if the maximum BMI distribution of whites were substituted for the black maximum BMI distribution. The resulting change in the mortality difference provides a second estimate of the effect of BMI on B-W differences in mortality. We use Model 3 that includes all explanatory variables and the linear probability model in these calculations. When using the linear probability model, the regression plane passes through the mean of all variables, including the dependent variable, the probability of dying. So answering the basic question simply requires substituting the white mean of maximum BMI for the black mean. The answer is identical but of opposite sign to that which we would obtain if we substituted the black mean maximum BMI for the white mean in the equation predicting white mortality. Similar substitutions for smoking and educational attainment provide equivalent information about their importance in explaining B-W differences in mortality. The means of the variables used in these analyses are those based on person-years of follow-up. As in the analysis of black regression coefficients, we wish to use the counterfactuals to examine B-W mortality differences net of differences in B-W age distributions. Accordingly, the B-W difference that we seek to explain compares the black death rate to an age-standardized white death rate that assumes that whites had the same age distribution as blacks.
Results
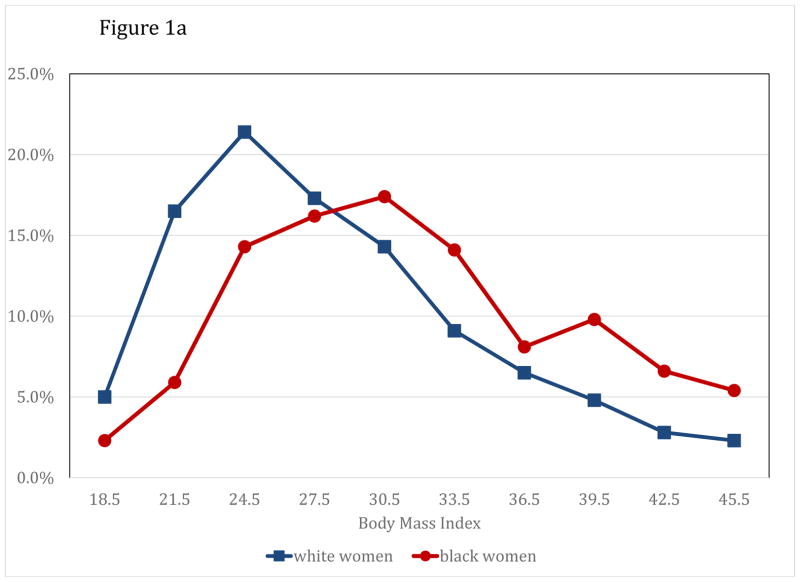
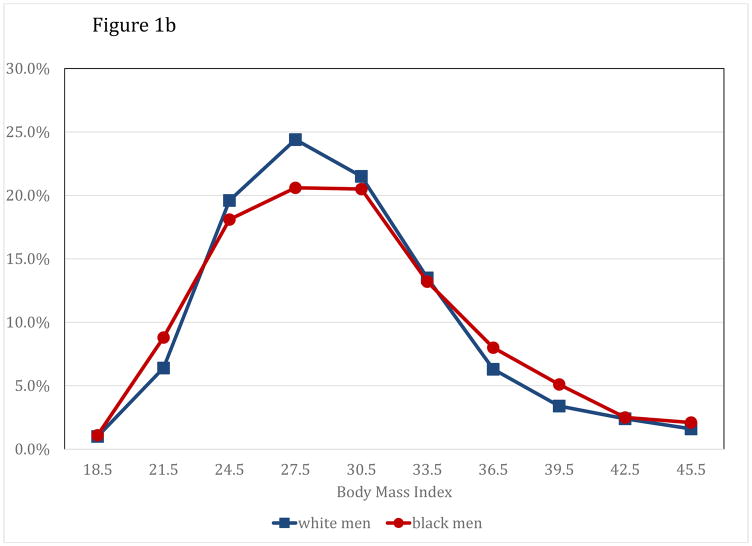
Table 1 provides sample characteristics and Figure 1 plots the distribution of maximum BMI by race and gender. Black women have a significantly higher mean maximum BMI (33.3) than white women (29.9). Figure 1a, which plots the age-standardized percentage distribution of maximum BMI in 3-unit increments for women, shows that a much larger percentage of black women than white women (64% vs. 43%) have maximum BMI in the obese range above 30.0. In contrast, the mean maximum BMI of black (31.3) and white (31.0) men is nearly identical. This similarity is also evident in Figure 1b, which shows the age-standardized percentage distribution of maximum BMI for men. These comparisons suggest that B-W differences in the distribution of maximum BMI are likely to contribute more to B-W difference in mortality among women than among men.
Table 1.
Sample characteristics by race and gender, ages 40–69 at baseline, National Health and Nutrition Examination Survey,a Mean (standard deviation in parentheses) or percent
| Variable | Men | Women | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Black | White | p-value | Black | White | p-value | |
|
|
||||||
| Mean BMI | 31.3 (5.6) | 31.0 (5.2) | 0.090 | 33.3 (6.6) | 29.9 (6.4) | 0.000 |
| Mean BMI above 25b | 32.4 (5.1) | 31.9 (4.8) | 0.042 | 34.4 (6.0) | 32.3 (5.6) | 0.000 |
| Mean age (baseline) | 51.8 (9.0) | 52.6 (8.7) | 0.001 | 51.9 (8.9) | 52.9 (8.7) | 0.000 |
| Mean age (exposure) | 55.6 (9.5) | 57.0 (9.4) | 0.000 | 56.2 (9.5) | 57.4 (9.4) | 0.000 |
| Smoking behavior | ||||||
| Current smoker | 40.6 | 23.6 | 0.000 | 26.4 | 20.8 | 0.000 |
| Former smoker | 23.6 | 36.8 | 20.5 | 27.8 | ||
| Never smoker | 35.9 | 39.6 | 53.1 | 51.4 | ||
| Education | ||||||
| <12 years | 30.5 | 12.4 | 0.000 | 27.0 | 11.6 | 0.000 |
| High school graduate | 27.8 | 27.2 | 26.0 | 29.1 | ||
| < 4 years college | 28.4 | 28.2 | 31.1 | 30.1 | ||
| 4+ years college | 13.4 | 32.2 | 15.9 | 29.3 | ||
| N | 1,965 | 4,200 | 2,075 | 4,051 | ||
| Person-Years | 19,251 | 41,039 | 22,701 | 40,742 | ||
| Deaths | 432 | 593 | 320 | 404 | ||
National Health and Nutrition Examination Survey (NHANES) III (1988–1994) and 1999–2010 NHANES continuous. Persons with BMI values between 18.5 and 50.0.
Calculated only among those whose maximum BMI is between 25.0 and 50.0.
Figure 1.
Figure 1a: Percent Distribution of Maximum BMI by Race, Females NHANES III 1988–1994 and NHANES 1999–2010. Figure 1b: Percent Distribution of Maximuma BMI by Race, Males NHANES III 1988–1994 and NHANES 1999–2010
Both smoking behavior and educational attainment differ significantly between Blacks and Whites. (Table 1). Black men are significantly more likely to be current smokers than white men (40.6 versus 23.6 percent), whereas white men are significantly more likely to be former smokers than black men (36.8 versus 23.6 percent). A somewhat higher percentage of white (39.6 percent) than black (35.9 percent) men are never smokers. The differences in smoking behavior among women less pronounced. For example, 26.4 percent of black women are current smokers compared to 20.8 percent of white women. Thus, we can expect that B-W differences in smoking will explain a larger share of the B-W difference in mortality among men than among women. Finally, white men and women are more highly educated on average than black men and women, with the differences being somewhat greater for men than women (Table 1).
Tables 2 and 3 present results from the discrete time linear probability model (Table 2) and from the discrete time logistic model (Table 3). These models are estimated on the sample that includes all individuals whose maximum BMI was between 18.5 and 50. As seen in Model 1, Table 2, the one-year probability of dying is significantly higher among black women than white women, by 4.38 per 1000 person years. Similarly, black men’s probability of dying is higher than that of white men (4.38 + 2.61 = 6.99 per 1,000). The estimated coefficients for educational attainment and smoking are in line with expectations (Model 2). The results are consistent with prior studies documenting a significant inverse educational gradient in mortality (Elo 2009). Relative to never smokers, current and former smokers have significantly higher mortality with current smokers having the highest mortality.
Table 2.
Estimated coefficients from discrete time linear probability model, NHANES III (1988–1994), NHANES 1999–2010, ages 40–69 at baseline (Coefficients expressed as incremental annual probability of dying per 1,000)
| Characteristica | Model 1c | Model 2c | Model 3c |
|---|---|---|---|
| Black (white)b | 4.38 (2.62–6.13) | 3.01 (1.23–4.78) | 1.73 (−0.10–3.55) |
| Male (female) | 2.99 (1.73–4.25) | 2.39 (1.10–3.68) | 2.33 (1.01–3.66) |
| Male*black | 2.61 (−0.21–5.42) | 1.35 (−1.48–4.18) | 2.56 (−0.28–5.41) |
| Education (4+ yrs. college) | |||
| <12 years | 8.16 (6.05–10.28) | 7.29 (5.16–9.42) | |
| High school graduate | 3.31 (1.91–4.70) | 2.65 (1.25–4.04) | |
| < 4 years college | 2.62 (1.25–4.00) | 1.99 (0.63–3.35) | |
| Smoking (Never smoker) | |||
| Current smoker | 9.70 (8.04–11.36) | 10.17 (8.50–11.84) | |
| Former smoker | 3.48 (2.19–4.77) | 3.52 (2.23–4.81) | |
| Maximum BMId | 0.05 (−0.27–0.38) | ||
| Maximum BMI squaredd | 0.02 (0.00–0.04) | ||
| Constant | −2.88 (−1.58–1.00) | −5.64 (−7.16–−4.12) | −7.09 (−8.72–−5.45) |
|
| |||
| N | 12,291 | ||
| Person-Years | 123,733 | ||
| Deaths | 1,749 | ||
All models also control for age as a time-varying covariate.
Omitted categories are given in parentheses.
Confidence intervals are in parentheses.
Additional precision for estimates of: BMI = 0.0548 [−0.2683–0.3779]; BMI squared = 0.0247 [0.000465–0.0448] expressed per 1,000.
Table 3.
Estimated odds ratios from discrete time logistic model, NHANES III (1988–1994), NHANES 1999–2010, ages 40–69 at baseline
| Characteristica | Model 1c | Model 2c | Model 3c |
|---|---|---|---|
| Black (white)b | 1.67 (1.38–2.03) | 1.48 (1.21–1.79) | 1.26 (1.04–1.54) |
| Male (female) | 1.44 (1.23–1.68) | 1.33 (1.13–1.56) | 1.32 (1.12–1.56) |
| Male*black | 1.11 (0.86–1.43) | 0.97 (0.75–1.25) | 1.12 (0.87–1.46) |
| Education (4+ yrs. college) | |||
| <12 years | 2.59 (2.04–3.30) | 2.32 (1.82–2.96) | |
| High school graduate | 2.01 (1.59–2.56) | 1.85 (1.46–2.36) | |
| < 4 years college | 1.77 (1.37–2.29) | 1.63 (1.26–2.10) | |
| Smoking (Never smoker) | |||
| Current smoker | 3.23 (2.70–3.86) | 3.51 (2.93–4.20) | |
| Former smoker | 1.79 (1.48–2.17) | 1.80 (1.49–2.18) | |
| Maximum BMId | 1.03 (1.00–1.07) | ||
| Maximum BMI squaredd | 1.00 (1.00–1.00) | ||
| Constant | 0.00 (0.00–0.00) | 0.00 (0.00–0.00) | 0.00 (0.00–0.00) |
|
| |||
| N | 12,291 | ||
| Person-Years | 123,733 | ||
| Deaths | 1,749 | ||
All models also control for age as a time-varying covariate.
Omitted categories are given in parentheses.
Confidence intervals are in parentheses.
Additional precision for estimated of: BMI = 1.03298 [0.99854–1.06860]; BMI squared = 1.00117 [0.99952–1.00282]
The inclusion of maximum BMI and BMI squared in Model 3 (Table 2) significantly improves the model fit (Prob F(2;123,731) = 0.000) even though both coefficients are not statistically significant (they are individually significant at p > 0.000 if added one at a time). When we introduce controls for maximum BMI and maximum BMI squared in Model 3, the coefficient for black females drops by 1.28 compared to Model 2. This drop represents 29.2 percent of the original age adjusted difference of 4.38 in Model 1. Thus, using this metric, about 29 percent of the difference in the age-adjusted mortality between black and white women is accounted for by the difference in their BMI distributions. In contrast, controls for maximum BMI do little to account for the excess mortality of black men. Black males have excess mortality relative to white males of 6.99 (4.38 + 2.61) in Model 1, 4.36 in Model 2, and 4.29 in Model 3, Thus, the difference in the black male coefficient between Models 2 and 3 is only 0.07 per 1,000, representing only 1.0 percent of the initial B-W difference of 6.99 for males in Model 1. These results reflect the much greater racial disparity in BMI distributions for women than for men, as shown in Figures 1a and 1b. Note that introducing BMI nearly doubles the coefficient of the term representing the interaction of black and male from Model 2 (1.35) to Model 3 (2.56). The similarity of black and white BMI distributions for males mutes the racial difference in total risks when it is not separately identified.
Table 3 presents odds ratios for Models 1, 2 and 3 from the logistic model. The conclusions based on these results are similar to those using the linear probability model. High BMI, smoking, and low educational attainment remain associated with higher mortality. The change in excess mortality for black women between Models 2 and 3 is 0.22 (0.48–0.26) per 1,000, representing the absolute reduction in the odds ratio when account is taken of BMI differences between black and white women. This change represents 32.8 percent of the 0.67 excess risk of black women in Model 1. This reduction is very similar to the reduction in mortality identified using the linear probability model. For men, the odds ratio for black men relative to white men changes from 1.854 (=1.67 × 1.11) in Model 1 to 1.436 in Model 2 and 1.411 in Model 3. So introducing BMI in Model 3 reduces the B-W odds ratio by about 2.9 percent of the total excess risk between Models 1 and 3 (0.025/0.854).
Table 4 presents results of the counterfactual analysis using the regression parameters estimated by the linear probability model. Setting all variables for black women at their mean value, the predicted mortality for black women is 9.45 per 1,000 based on Model 3, Table 2. If white women had all the white characteristics but the age distribution of black women, their probability of dying would be 5.35 per 1,000. The difference between the two values, 4.10 per 1,000, is what we attempt to account for. Substituting the white maximum BMI distribution for the black distribution produces a reduction of 1.13 per 1,000 in predicted black women’s mortality (9.45–8.32). This change represents 27.6 percent of the age-adjusted B-W difference (4.10) in mortality. This figure is very close to that obtained from the analysis of changes in regression coefficients in the linear model (29.2 percent). If black women had the educational distribution of white women, the B-W gap would be reduced by 1.01 per 1,000, or by 24.6 percent. If they had the smoking characteristics of white women, the gap would be reduced by 0.24 per 1,000, or by 5.9 percent. Among these three variables, B-W differences in obesity are the most important in accounting for the B-W difference in women’s mortality.
Table 4.
Predicted change in the probability of death (per 1,000) associated with substituting the distribution of white characteristics for those of blacks based on coefficients shown in Table 2, Model 3
| Characteristic | Predicted death per 1,000 | Difference relative to all black |
|---|---|---|
| WOMEN | ||
|
|
||
| All Black | 9.45 | |
| White, Black age distribution | 5.35 | 4.10 |
| Black, White BMI | 8.32 | 1.13 |
| Black, White smoking | 9.21 | 0.24 |
| Black, White education | 8.44 | 1.01 |
| MEN | ||
|
|
||
| All Black | 14.97 | |
| White, Black age distribution | 8.12 | 6.85 |
| Black, White BMI | 14.88 | 0.09 |
| Black, White smoking | 13.79 | 1.18 |
| Black, White education | 13.64 | 1.33 |
Results are different for black men. Their mortality is higher than the predicted mortality for white men with the black male age distribution by 6.85 per 1,000 [14.97–8.12] (Table 4). The substitution of the white male BMI distribution for the black male distribution produces a predicted reduction in black male mortality of 0.09, or 1.3 percent. Substitution of the white male smoking distribution for that of black males produces a reduction of 1.18 per 1,000, or 17.2 percent, while differences in educational distributions account for 1.33 per 1,000, or 19.4 percent of the difference.
Relative to whites, black women and men suffer nearly the same penalty from the combined effects of smoking and excess weight. The sum of the estimated impacts of the two risks in Table 4 is 1.37 per 1, 000 for women and 1.27 for men. However, this level is achieved through very different routes, with smoking the dominant influence among men and obesity among women. This result mirrors the inverse association between smoking and obesity in the United States. We speculate that the relatively small difference in BMI distributions between black and white men reflects the very high intensity of smoking among black men. Differences in educational distributions contribute relatively similar values for men (1.33), representing 19 percent of the B-W difference in mortality, and for women (1.01), representing 25 percent of the B-W difference in mortality.
Summary and Discussion
During recent decades, obesity has emerged as a leading risk factor for morbidity and mortality in the United States. It has been estimated that in 2006 obesity reduced U.S. life expectancy at age 50 by 1.54 years for women and 1.85 years for men (Preston and Stokes 2011). In this paper, we examine the contribution of obesity to B-W differences in US mortality. We use one’s maximum body mass index as our indicator of obesity. Altogether, 64% of black women are currently obese or have been obese during their lifetime, compared to 43% of white women. Combined with the estimated mortality risk from obesity, this difference in prevalence explains close to 30 percent of B-W difference in mortality at ages 40–79 among women, but plays a very small role in the B-W difference among men. We found no evidence that the excess risk of death associated with obesity varies between Blacks and Whites when BMI is based on maximum weight attained.
We contrast the contribution of obesity to that of smoking, another well-known behavioral risk factor for mortality. In contrast to obesity, smoking explains about 17 percent of the B-W difference in mortality among men but only about 6 percent among women. That smoking plays a more important role in B-W mortality differences among men than women is consistent with prior studies (Ho and Elo 2013). In addition, we showed that B-W differences in educational attainment, a widely-used indicator of socioeconomic status, account for 19 percent and 25 percent of the B-W mortality difference among men and women, respectively.
Blacks possess a riskier behavioral profile than Whites. It has also been hypothesized that Blacks may be more likely to engage in risky behaviors than Whites as a coping mechanism against exposure to unusually stressful life conditions (e.g., extreme socioeconomic deprivation, racial discrimination, exposure to crime and inferior neighborhood environments) (Jackson 2002; Jackson et al. 2010; Winkleby and Cubbin 2004). Our findings elucidate the distinct behavioral pathways through which B-W mortality differences evolve for men and women. Among women, obesity is the dominant pathway, whereas among men smoking dominates. Targeted public health efforts toward these risk factors could yield sizeable reductions in B-W mortality differences.
Our results also underscore the important role of poorer educational attainment among black men and women in producing B-W mortality disparities. Low educational attainment is associated not only with more adverse health behaviors but also with lifelong material deprivation, inferior access to healthcare, and a range of other factors pertinent to health. Educational attainment may also be linked to cognitive factors that influence starting and stopping risky behaviors and the ability to obtain and effectively use health-related information more generally (Elo 2009; Margolis 2013; Mehta, House and Elliott 2015).
Limitations
We have modeled the risk of weight status based on maximum BMI, which does not distinguish between muscle mass and body fat. Heymsfield et al. (2015) in a review of BMI-adiposity relationship based on NHANES find that at a given BMI, non-Hispanic blacks have a lower percentage body fat than non-Hispanic whites when BMI is measured at baseline. Further analysis of the role of other measures of body composition may shed additional light on the role of weight status in generating B-W differences in mortality.
Second, as noted previously, our measure of peak BMI is self-reported, and it may overestimate the contribution of BMI to B-W disparities in mortality, especially among women. Self-reporting biases have been shown to result in underreporting of BMI among whites, especially among women (Wen and Kowaleski-Jones 2013).
Our models were estimated on a sample that included all individuals with BMI between 18.5 and 50. We made the assumption that zero risk was associated with having a BMI between 18.5 and 25.0, i.e., being in the “Normal” BMI range. To investigate how sensitive our results are to this assumption, we re-estimated models using only a sample of individuals whose BMI values were above 25.0. Results presented demonstrate that our estimates of the contribution of excess BMI to B-W mortality differences are not sensitive to this assumption (results available from the authors).
Conclusion
Table 4 shows that black-white differences in obesity and smoking together account for a sizable fraction of B-W differences mortality at ages 40–79 among both men (18.5 percent) and women (33.4 percent). Obesity is the key risk factor among women and smoking among men. In addition, B-W differences in educational attainment, which is associated not only with behavioral risk factors but also contributes to B-W differences in income and wealth, account for an additional 19.4 percent and 24.6 percent of the B-W mortality difference among men and women, respectively.
Acknowledgments
This research was supported by Network on Life Course Health Dynamics and Disparities in 21st Century America - NIA R24AG045061; Population Aging Research Center, University of Pennsylvania – NIA P30 AG012836; and NIA R01 AG040212, The Contribution of Obesity to International Differences in Longevity.
Footnotes
An earlier version of this paper was presented at the annual meeting of the Population Association of America, March 31, 2016.
Contributor Information
Irma T. Elo, Population Studies Center, University of Pennsylvania
Samuel Preston, Population Studies Center, University of Pennsylvania.
Neil Mehta, Rollins School of Public Health, Emory University.
References
- Abell JE, Egan BM, Wilson PWF, Lipsitz S, Woolson RF, Lackland DT. Differences in cardiovascular disease mortality associated with body mass between black and white persons. American Journal of Public Health. 2008;98(1):63–66. doi: 10.2105/AJPH.2006.093781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdullah A, Stoelwinder J, Shortreed S, Wolfe R, Stevenson C, Walls H, et al. The duration of obesity and the risk of type 2 diabetes. Public Health Nutrition. 2011;14(01):119–126. doi: 10.1017/S1368980010001813. [DOI] [PubMed] [Google Scholar]
- Abdullah A, Amin FA, Stoelwinder J, Tanamas SK, Wolfe R, Barendregt J, Peeters A. Estimating the risk of cardiovascular disease using an obese-years metric. BMJ open. 2014;4(9):e005629. doi: 10.1136/bmjopen-2014-005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Hollenbeck A, Leitzmann MF. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. New England Journal of Medicine. 2006;355(8):763–78. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- Arias E. National vital statistics reports. 7. Vol. 63. Hyattsville, MD: National Center for Health Statistics; 2014. United States life tables, 2010. 2014. [PubMed] [Google Scholar]
- Berrington de Gonzalez A, et al. Body-mass index and mortality among 1.46 million white adults. New England Journal of Medicine. 2010;363(23):2211–2219. doi: 10.1056/NEJMoa1000367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boggs, Rosenberg DAL, Cozier YC. General and abdominal obesity and risk of death among black women. New England Journal of Medicine. 2011;365:901–908. doi: 10.1056/NEJMoa1104119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW. Body-mass index and mortality in a prospective cohort of U.S. adults. New England Journal of Medicine. 1999;341(15):1095–105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services; 2014. [Google Scholar]
- Chow EA, Foster H, Gonzalez V, McIver L. The disparate impact of diabetes on racial/ethnic minority populations. Clinical Diabetes. 2012;30:130–133. [Google Scholar]
- Cohen SS, Park Y, Signorello LB, et al. A pooled analysis of body mass index and mortality among African Americans. PLOS ONE. 2014;9(11):e111980. doi: 10.1371/journal.pone.0111980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen SS, Signorello LB, Cope EL, et al. Obesity and all-cause mortality among black adults and white adults. American Journal of Epidemiology. 2012;176:431–442. doi: 10.1093/aje/kws032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins E, Faul J, Kim JK, Guyer H, et al. Documentation of Biomarkers in the 2006 and 2008 Health and Retirement Study. Survey Research Center, University of Michigan; Ann Arbor, MI: 2013. DR-12. http://hrsonline.isr.umich.edu/sitedocs/userg/Biomarker2006and2008.pdf. [Google Scholar]
- Dupre ME, Gu D, Vaupel JW, JW Survival differences among native-born and foreign-born older adults in the United States. PLOS ONE. 2012;7(5):e37177. doi: 10.1371/journal.pone.0037177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo IT. Social class differentials in health and mortality: Patterns and explanations in comparative perspective. Annual Review of Sociology. 2009;35:553–572. [Google Scholar]
- Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005–2014. JAMA. 2016;315:2284–2291. doi: 10.1001/jama.2016.6458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obesity Reviews. 2007;8(4):307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- Heymsfield SB, Peterson CM, Thomas DM, Heo M, Schuna JM., Jr Why are there race/ethnic differences in adult body mass index-adiposity relationships? A quantitative critical review. Obesity Reviews. 2016;17:262–275. doi: 10.1111/obr.12358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S, Rushani D, Kaufman JS. Trends in the black-white life expectancy gap, 2003–2008. JAMA. 2012;307:2257–2259. doi: 10.1001/jama.2012.5059. [DOI] [PubMed] [Google Scholar]
- Harper S, MacLehose RF, Kaufman JS. Trends in the black-white life expectancy gap among US states, 1990–2009. Health Affairs. 2014;8:1375–1382. doi: 10.1377/hlthaff.2013.1273. [DOI] [PubMed] [Google Scholar]
- Hayward Mark D, Crimmins Eileen M, Miles Toni P, Yang Yu. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. American Sociological Review. 2000;65(6):910–930. [Google Scholar]
- Ho JY, Elo IT. The contribution of smoking to black-white differences in U.S. mortality. Demography. 2013;50:545–568. doi: 10.1007/s13524-012-0159-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. Race and Unhealthy Behaviors: Chronic Stress, the HPA Axis, and Physical and Mental Health Disparities Over the Life Course. Am J Public Health. 2010;100:933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS. Health and mental health disparities among Black Americans. In: Hager M, editor. Modern Psychiatry: Challenges in Educating Health Professionals to Meet New Needs. New York, NY: Josiah Macy Jr. Foundation; 2002. pp. 246–254. [Google Scholar]
- Jackson N-CL, Wang Y, Yeh H-C, et al. Body-mass index and mortality risk in US blacks compared to whites. Obesity. 2014;22:842–851. doi: 10.1002/oby.20471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jolly Stacey, Vittinghoff E, Chattopadhyay A, Bibbins-Domingo K. Higher cardiovascular disease prevalence and mortality among younger blacks compared to whites. American Journal of Medicine. 2010 doi: 10.1016/j.amjmed.2010.04.020. [DOI] [PubMed] [Google Scholar]
- Kivimäki Mika, et al. Optimal form of operationalizing BMI in relation to all-cause and cause-specific mortality: The original Whitehall Study. Obesity. 2008;16:1926–32. doi: 10.1038/oby.2008.322. http://www.nature.com/doifinder/10.1038/oby.2008.322. [DOI] [PubMed] [Google Scholar]
- Margolis R. Educational Differences in Healthy Behavior Changes and Adherence Among Middle-aged Americans. Journal of Health and Social Behavior. 2013;54:353–368. doi: 10.1177/0022146513489312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta NK, House JS, Elliott MR. Dynamics of health behaviours and socioeconomic differences in mortality in the USA. J Epidemiol Community Health. 2015;69:416–422. doi: 10.1136/jech-2014-204248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta NK, Stenholm S, Elo IT, Aromaa A, Heliövaara M, Koskinen S. Weight histories and mortality among Finnish adults: The role of duration and peak body mass index. Epidemiology. 2014;25(5):707–710. doi: 10.1097/EDE.0000000000000147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta NK, Preston SH. Are major behavioral and sociodemographic risk factors for mortality additive or multiplcative in their effects? Social Science and Medicine. 2016;154:93–99. doi: 10.1016/j.socscimed.2016.02.009. http://dx.doi.org/10.1016/j.socscimed.2016.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orpana HM, Berthelot JM, Kaplan MS, Feeny DH, McFarland B, Ross NA. BMI and mortality: results from a national longitudinal study of Canadian adults. Obesity (Silver Spring, Md) 2010;18(1):214–218. doi: 10.1038/oby.2009.191. [DOI] [PubMed] [Google Scholar]
- Park Y, Hartge P, Moore SC, et al. Body mass index and mortality in non-Hispanic black adults in the NIH-AARP diet and health study. PLOS ONE. 2012;7:e50091. doi: 10.1371/journal.pone.0050091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel AV, Hildebrand JS, Gapstur SM. Body mass index and all-cause mortality in a large prospective cohort of white and black U.S. adults. PLOS ONE. 2014;9:e109153. doi: 10.1371/journal.pone.0109153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston SH, Stokes A. Contribution of obesity to international differences in life expectancy. American Journal of Public Health. 2011;101:2137–2143. doi: 10.2105/AJPH.2011.300219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston SH, Mehta NK, Stokes A. Modeling obesity histories in cohort analyses of health and mortality. Epidemiology. 2013;24(1):158–166. doi: 10.1097/EDE.0b013e3182770217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preston SH, Fishman E, Stokes A. Effects of categorization and self-report bias on estimates of the association between obesity and mortality. Annals of Epidemiology. 2015 doi: 10.1016/j.annepidem.2015.07.012. http://dx.doi.org/10.1016/j.annepidem.2015.07.012. [DOI] [PMC free article] [PubMed]
- Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. American Journal of Public Health. 1998;88:15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selvin E, Parrinello CM, Sacks DB, Coresh J. Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann Intern Med. 2014;160:517–525. doi: 10.7326/M13-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes A. Using maximum weight to redefine body mass index categories in studies of the mortality risks of obesity. Population Health Metrics. 2014;12(1):6. doi: 10.1186/1478-7954-12-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes A, Preston SH. Revealing the burden of obesity using weight histories. Proceedings of the National Academy of Sciences. 2016a;113:575–577. doi: 10.1073/pnas1515472113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes A, Preston SH. How dangerous is obesity? Issues in measurement and interpretation. Population and Development Review. 2016b;42:595–614. doi: 10.1111/padr.12015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarleton HP, Smith LV, Zhang Z-F, Kuo T. Utility of anthropometric measures on a multiethnic population: Their association with prevalent diabetes, hypertension and other chronic disease comorbidities. Journal of Community Health. 2014;39:471–4. doi: 10.1007/s10900-013-9780-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M, Kowaleski-Jones L. Sex and ethnic differences in validity of self-reported adult height, weight and body mass index. Ethnicity & Disease. 2012;22(1):72–78. [PMC free article] [PubMed] [Google Scholar]
- Whitlock G, et al. Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkleby MA, Cubbin C. Racial/ethnic disparities in health behaviors: a challenge to current assumptions. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Disparities in Health in Later Life. Washington, DC: National Research Council; 2004. pp. 171–226. [Google Scholar]
- Xiao Q, Hsing AW, Park Y, et al. Body mass index and mortality among blacks and white adults in the prostrate, lung, colorectal, and ovarian (PLOC) cancer screening trial. Obesity. 2014;22:260–268. doi: 10.1002/oby.20412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, Yang Y. Population heterogeneity in the impact of body weight on mortality. Social Science and Medicine. 2012;75:990–996. doi: 10.1016/j.socscimed.2012.05.013. [DOI] [PubMed] [Google Scholar]