A 45-year-old male patient presented with 2 weeks history of flu-like illness, tiredness, occipital headache, and painless progressive blurring of vision OS > OD. Past ocular and medical history were unremarkable.
Best-corrected visual acuity was 6/15 (+0.75) OD and 6/90 (+1.00) OS Color vision was 2/17 OD and 0/17 OS. Anterior segment examination was unremarkable. A relative afferent pupillary defect OS was noted. Dilated fundus examination revealed abnormal findings OU [Figure 1]. Optical coherence tomography (OCT) macula revealed abnormalities as shown in Figures 2 and 3. Systemic review by the internist was reported unremarkable.
Figure 1.
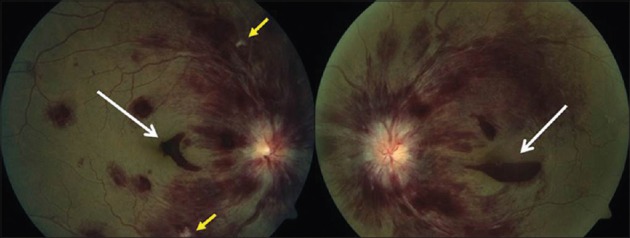
Fundus photograph of right eye and left eye
Figure 2.
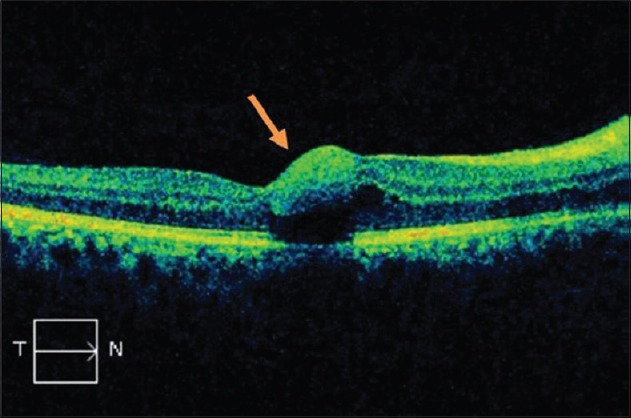
Optical coherence tomography of the right eye
Figure 3.
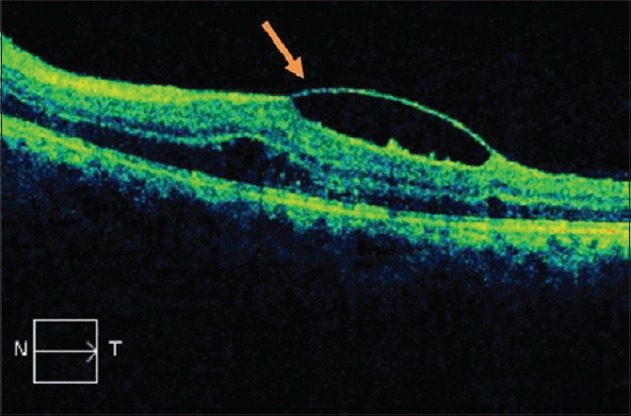
Optical coherence tomography of the left eye
Questions
Answers
-
Fundus photograph shows
- Figure 1: Bilateral disc edema with multilayered retinal hemorrhages involving all quadrants. Macula shows subhyaloid hemorrhage OS > OD (long arrows). Fundus photograph of the right eye shows cotton wool spots (small arrows)
- Figure 2: OCT macula OD shows subhyaloid hemorrhages involving the fovea (arrow)
- Figure 3: OCT macula OS shows subhyaloid hemorrhages involving the fovea (arrow).
-
Differential diagnosis
- Blood dyscrasias such as anemia, leukemia, polycythemia, platelet disorders and coagulopathies, and plasma cell dyscrasias.
- Central retinal vein occlusion
- Thrombophlebitis
- Retinal artery macroaneurysm
- Infectious optic neuropathy (Tuberculosis, Syphilis, Lyme, Toxoplasmosis, Herpes)
- Compressive optic neuropathy
- Idiopathic intracranial hypertension
- Diabetic retinopathy
- Grade IV hypertensive retinopathy
- Trauma.
-
Investigations
- Fundus fluorescein angiography
- Blood pressure measurement and basic blood workup: Complete and differential blood count, platelet count, and peripheral smear to rule out blood dyscrasias
- Blood culture and serology to rule out infectious causes
- Magnetic resonance imaging (MRI) brain and orbit to look for any space occupying lesion in the brain and optic nerve pathologies
- Lumbar puncture to look for the opening pressure and cerebrospinal fluid analysis.
Basic blood workup in this patient revealed pancytopenia with circulating blast cells on peripheral smear examination which was confirmed by bone marrow aspiration. Blood pressure monitored during patient's assessment was in the normal range. Lumbar puncture was performed which also showed circulating blasts but no organism. Blood culture grew pseudomonas. MRI brain shows left parietotemporal subcortical white matter hyperintensities with normal optic nerve enhancement.
Based on ophthalmic findings and hematological evaluation, the final diagnosis was acute myeloid leukemia (AML) with central nervous system involvement.
The ocular involvement in AML are more common in posterior segment and are related to secondary systemic changes such as anemia, thrombocytopenia, hyperviscosity, and immunosuppression. The findings include multilayered retinal hemorrhages, cotton wool spots, Roth spots, perivascular infiltrates, vitreous hemorrhage, vascular occlusions, and ischemic optic neuropathy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.


