Abstract
Background
Early reports suggest the number of CICU patients with primary non-cardiac diagnoses is rising in the U.S., but no national data currently exist. We examined changes in primary non-cardiac diagnoses among elderly patients admitted to a cardiac intensive care unit (CICU) over the last decade.
Methods and Results
Using 2003–2013 Medicare data, we grouped elderly patients admitted to CICUs into two categories based on principal diagnosis at discharge: 1) primary non-cardiac diagnoses and 2) primary cardiac diagnoses. We examined changes in patient demographics, comorbidities, procedure use, and risk-adjusted in-hospital mortality. Among 3.4 million admissions with a CICU stay, primary non-cardiac diagnoses rose in prevalence from 38.0% to 51.7% between 2003 and 2013. The fastest rising primary non-cardiac diagnoses were infectious diseases (7.8% to 15.1%) and respiratory diseases (6.0% to 7.6%) (p < 0.001 for both), while the fastest declining primary cardiac diagnosis was coronary artery disease (32.3% to 19.0%) (p < 0.001). Simultaneously, the prevalence of both cardiovascular and non-cardiovascular comorbidities rose: heart failure (13.9% to 34.4%), pulmonary vascular disease (1.2% to 7.1%), valvular heart disease (5.0% to 9.8%) and renal failure (7.1% to 19.6%) (p < 0.001 for all). As compared with those with primary cardiac diagnoses, elderly CICU patients with primary non-cardiac diagnoses had higher rates of non-cardiac procedure use and risk-adjusted in-hospital mortality (p < 0.001 for all). Risk-adjusted in-hospital mortality declined slightly in the overall cohort from 9.3% to 8.9% (p < 0.001).
Conclusions
More than half of all elderly patients with a CICU stay across the U.S. now have primary non-cardiac diagnoses at discharge. These patients receive different types of care and have worse outcomes than patients with primary cardiac diagnoses. Our work has important implications for the development of appropriate training and staffing models for the future critical care workforce.
Cardiologists initially developed and staffed coronary care units in the 1960s to improve the rapid detection and defibrillation of life-threatening ventricular arrhythmias during acute myocardial infarction (AMI).1–4 These early units demonstrated substantial gains in survival for AMI patients, subsequently evolving into cardiac intensive care units (CICUs) that treat a wider array of acute cardiovascular diseases including cardiogenic shock, heart failure and complex arrhythmias.5, 6 More recently, a handful of reports from large academic centers have suggested that CICUs are expanding their roles even further by caring for a growing number of patients with chronic cardiovascular conditions who present with acute non-cardiac illnesses such as sepsis and renal failure.7–9 This latest trend has raised some concern among cardiologists, as caring for these groups of patients may require expertise in critical care and non-cardiac procedures that fall beyond the purview of typical general cardiology training.6, 10
In response, the American Heart Association (AHA) issued a scientific statement on the future of critical care cardiology in 2012,11 pointing to the potential need for cardiologists to expand training in managing critically-ill patients with chronic cardiovascular conditions who present with primary non-cardiac diagnoses. In 2015, the American College of Cardiology (ACC) followed this statement by publishing the Core Cardiovascular Training Statement (COCATS 4) that outlined additional requirements in non-cardiac procedures like ventilator management for trainees interested in critical care cardiology.12, 13 Despite strong interest by these professional organizations, comprehensive data on the number, types and outcomes of patients admitted to CICUs across the U.S. with primary non-cardiac diagnoses remain largely unknown outside of these few reports. This lack of data is concerning, as the composition of CICU patients and their needs may be changing over time due to an aging population14, declines in coronary artery disease15, and a shift in risk factors for cardiovascular disease.15
We examined changes in the number, types, and outcomes of hospitalized patients with CICU stays between 2003 and 2013 in the U.S. using Medicare data. We chose this cohort as it allows for a national evaluation while simultaneously focusing on elderly patients who are at the highest risk for cardiovascular and non-cardiovascular critical illness.16 We hypothesized that temporal trends in CICUs would demonstrate a rise in patients with primary non-cardiac diagnoses, non-cardiac procedure utilization and risk-adjusted in-hospital mortality. In addition, we evaluated how these trends varied across small, medium and large hospitals given the large differences in the types of critical care services and physician staffing available across such centers.
METHODS
Data Sources and Study Population
We performed a retrospective cohort study of acute-care hospitalizations with CICU stays among fee-for-service (FFS) Medicare beneficiaries aged 65 years or older using the 100% Medicare Provider Analysis and Review (MEDPAR) files from 2003 to 2013. MEDPAR data capture all billable diagnoses, procedures, demographics, and in-hospital outcomes from hospitalized patients admitted with a CICU stay. All patients with fee-for-service eligibility at the time of admission were included.
For this study, we defined hospitalization with a CICU stay using revenue center codes within the claim records. Revenue center codes are used to identify billed services from divisions or units within a hospital (e.g., radiology, emergency room, CICU, other ICUs). If charges were listed for ICU services from both the CICU and other ICUs (e.g., Medical ICU) during the same hospitalization, we classified the hospitalization as having a CICU stay when the patient spent the largest number of ICU days in a CICU. We excluded patients with hospitalizations in intermediate care units only. To avoid counting hospitalizations for patients without cardiovascular disease temporarily ‘boarding’ in the CICU, we excluded any patients who did not have a primary or secondary cardiac diagnosis at discharge (i.e., 5.1% of total patients). This approach to excluding ‘boarders’ was evaluated in a sensitivity analysis that showed consistent results (not reported but available from authors). Finally, to ensure a consistent cohort of hospitals with CICUs, we included only those 806 hospitals billing more than 20 hospitalizations with a CICU stay during every year throughout the study period (i.e., from 2003 to 2013, consecutively).
Definition of Cardiac and Non-Cardiac Diagnoses
For all patients, we included demographic data (age, sex, and race) as well as extracted information on hospital and CICU length of stay, principal and secondary International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes, procedure codes, and discharge status (alive or dead). A patient could have only one primary discharge diagnosis code but multiple secondary diagnosis codes. We used the Clinical Classification Software (CCS) developed by the Agency for Healthcare Research and Quality (AHRQ) to aggregate ICD-9-CM diagnosis codes into 281 unique diagnoses based on the multi-level CCS categories.17 Primary cardiac diseases encompassed those primary discharge diagnosis codes delineated in multi-level CCS Category 7, “Diseases of the Circulatory System,” and were consolidated into coronary artery disease, congestive heart failure, valvular disease, dysrhythmias and other circulatory diseases. Primary non-cardiac diseases included primary discharge diagnosis codes comprising other CCS Categories, including respiratory, gastrointestinal, infectious, musculoskeletal/injuries, neurologic and hematologic and oncologic disease, with infections specific to an organ system (e.g. pneumonia) grouped under the infectious category.18 Details of assignments of individual diagnoses into CCS Categories can be found in Supplementary Appendix Table A.
Case Mix and Procedures
To better characterize changes in patient case mix during the study period, we identified patients with cardiovascular and non-cardiovascular comorbidities using all primary and secondary diagnosis codes from their index hospitalization according to the method previously described by Elixhauser et al.19 We used ICD-9-CM procedure codes to identify non-cardiac procedures including invasive mechanical ventilation (96.70, 96.71, 96.72), noninvasive mechanical ventilation (93.90), central venous catheterization (38.93), blood transfusion (99.0X) and hemodialysis (39.95). For cardiac procedures, we used the following ICD-9-CM procedure codes: pulmonary artery catheterization (89.63, 89.64, 89.66, 89.67, 89.68); right heart catheterization (37.21); implantation of pulsation balloon (37.61); ventricular assist device (37.62, 37.63, 37.65, 37.66, 37.68); diagnostic cardiac catheterization (37.22, 37.23, 88.50, 88.53); percutaneous coronary intervention (PCI; 00.66, 17.55, 36.06, 36.07, 36.09, 00.4X); and coronary artery bypass surgery (CABG; 36.1X, 36.2, 36.3, 36.9).
Statistical Analysis
Baseline distributions for patient demographics (age, sex, race, comorbidities), procedure use, and outcomes are presented in 2-year intervals from 2003 to 2013 as means or percentages of total admissions for the entire patient cohort. Categorical variables are expressed as frequencies (percentages) and continuous variables as means or medians where appropriate. We calculated the percentage of total hospitalizations with a CICU stay in each disease category for each year. The denominator for these calculations was the total number of hospitalizations each year in FFS Medicare beneficiaries. The results are presented using stacked bar graphs, with the total height of each bar representing 100% of admissions. We describe changes in the rankings of primary diagnoses across years, presenting the results in Supplementary Appendix Table B and as online, interactive data visualization tools shown in Supplementary Appendix C.
Both unadjusted and risk-adjusted in-hospital mortality were reported. Risk-adjusted, in-hospital mortality rates were calculated using a logistic regression model that adjusted for age, gender, race, and total number of Elixhauser comorbidities. We also examined whether trends in primary non-cardiac diagnoses and risk-adjusted mortality varied across small (< 250 beds), medium (250–500 beds), and large (> 500 beds) hospitals during the study period after linking the Medicare data to yearly data from the American Hospital Association Annual Survey.
A p-value of less than 0.05 was used to determine statistical significance. All data management and statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC) and STATA version 14.0 (StataCorp, College Station, TX). The protocol for data analysis was formally reviewed and approved by the Institutional Review Board of the University of Michigan, Ann Arbor, MI.
RESULTS
Demographic Trends
For the study period of January 1, 2003 to December 31, 2013, a total of 3.4 million hospitalizations with a CICU stay were identified. The rate of CICU admissions per 1000 fee-for-service Medicare hospitalizations in the study cohort decreased from 93.7 in 2003 to 74.3 in 2013 (p < 0.001). Table 1 shows baseline characteristics of hospitalizations with a CICU stay between 2003 and 2013. Demographic characteristics, including sex and race, remained relatively stable over the study period. The mean age increased minimally from 77.1 to 77.6, while the proportion of patients’ aged 85 years or older grew from 17.8% to 23.6% (p < 0.001).
Table 1.
Baseline Characteristics Among Fee-For-Service Medicare Beneficiaries with a CICU Stay Between 2003 and 2013
| 2003 | 2005 | 2007 | 2009 | 2011 | 2013 | |
|---|---|---|---|---|---|---|
| Number of CICU Hospitalizations | 367587 | 354585 | 333314 | 290820 | 276155 | 237524 |
| No. of CICU per 1000 FFS Hospitalizations (%) | 93.7 | 89.2 | 88.4 | 81.2 | 80.0 | 74.3 |
| Age (mean) | 77.1 | 77.2 | 77.4 | 77.5 | 77.7 | 77.6 |
| 65–74 | 39.5 | 39.2 | 38.8 | 39.3 | 39.0 | 39.9 |
| 75–84 | 42.7 | 42.0 | 40.7 | 38.6 | 37.8 | 36.6 |
| 85–94 | 16.6 | 17.5 | 19.0 | 20.3 | 21.3 | 21.5 |
| 95+ | 1.2 | 1.3 | 1.5 | 1.7 | 1.9 | 2.1 |
| Sex | ||||||
| Male | 50.0 | 50.2 | 50.1 | 50.3 | 49.6 | 50.8 |
| Female | 50.0 | 49.8 | 49.9 | 49.7 | 50.5 | 49.2 |
| Race | ||||||
| White | 87.0 | 86.3 | 86.2 | 85.3 | 84.8 | 84.6 |
| Black | 8.3 | 8.5 | 8.8 | 9.4 | 9.7 | 9.7 |
| Other | 4.7 | 5.1 | 5.0 | 5.3 | 5.5 | 5.7 |
| Elixhauser Comorbidities | ||||||
| 0–1 | 37.2 | 32.7 | 27.1 | 22.8 | 18.8 | 18.5 |
| 2 | 29.9 | 30.0 | 29.7 | 28.9 | 26.4 | 27.0 |
| ≥3 | 32.9 | 37.4 | 43.2 | 48.3 | 54.8 | 54.6 |
| Hypertension | 54.5 | 56.2 | 54.8 | 57.5 | 60.5 | 56.8 |
| Diabetes Mellitus | 24.7 | 24.2 | 23.4 | 22.9 | 24.9 | 24.5 |
| Obesity | 3.0 | 3.3 | 3.5 | 4.4 | 4.6 | 5.2 |
| Congestive Heart Failure | 13.9 | 15.8 | 19.5 | 29.9 | 32.7 | 34.4 |
| Valvular Heart Disease | 5.0 | 5.7 | 7.7 | 10.1 | 10.2 | 9.8 |
| Pulmonary Vascular Disease | 1.2 | 1.4 | 2.4 | 5.2 | 6.3 | 7.1 |
| Peripheral Vascular Disease | 9.0 | 9.0 | 8.7 | 9.0 | 9.2 | 8.3 |
| Chronic Pulmonary Disease | 24.4 | 26.2 | 25.0 | 20.0 | 20.9 | 20.3 |
| Renal Failure | 7.1 | 10.8 | 18.3 | 16.6 | 19.8 | 19.6 |
| Malignancy | 4.2 | 4.4 | 4.9 | 5.3 | 5.7 | 5.7 |
p value < 0.001 for all comparisons. All values are reported as percentages unless otherwise noted.
Abbreviations: FFS = Fee-For-Service Medicare beneficiary
Rise in Primary Non-Cardiac and Primary Cardiac Diagnoses Over Time
Primary non-cardiac diagnoses rose from 38.0% of hospitalizations with a CICU admission in 2003 to 51.7% of hospitalizations in 2013 (p < 0.001) (Figure 1). The rise in primary non-cardiac diagnoses was not attributable to a single condition, but the largest increases resulted from primary diagnoses of infectious diseases (7.8% to 15.1%) and non-infectious respiratory diseases (6.0% to 7.6%) (p < 0.001 for both) (Figure 1). During the same interval, a corresponding decline in primary cardiac diagnoses was observed (Figure 1) largely due to a substantial decrease in primary diagnoses of coronary artery disease (CAD) from 32.3% to 19.0% (p for trend < 0.001). A more modest decrease in primary diagnoses of congestive heart failure (CHF) was noted from 9.8% to 7.5% (p for trend < 0.001). When individual discharge diagnoses were considered as opposed to grouped CCS categories, similar patterns were observed. For instance, acute myocardial infarction declined from 16.0% to 12.0% during the study period, although it remained the single most common discharge diagnosis in 2013. Sepsis increased from the eleventh most common individual discharge diagnosis in 2003 (1.9%) to the second most common discharge diagnosis in 2013 (9.2%). A complete list of the individual diagnoses categorized by the CCS and their changes over time are illustrated through online data visualization tools shown in Supplementary Appendix C.
Figure 1.
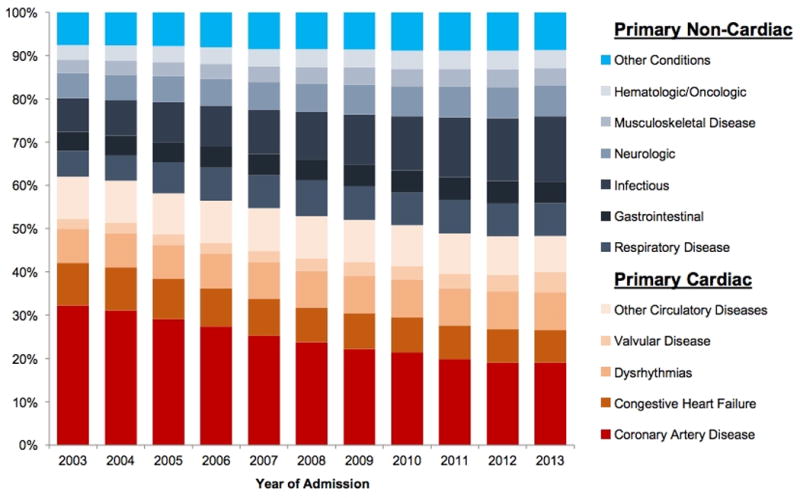
Primary Diagnosis by Disease Category Among Elderly Patients with a Cardiac Intensive Care Unit Stay Between 2003 and 2013
Changes in Comorbidities Over Time
From 2003 to 2013, the percentage of CICU patients with comorbidities increased (Table 1). The number of patients with three or more comorbidities grew from 32.9% in 2003 to 54.6% in 2013 (p < 0.001). For cardiovascular comorbidities, the number of patients with CHF increased 2.6-fold (13.9% to 34.4%), pulmonary vascular disease 5.9-fold (1.2% to 7.1%), and valvular heart disease 2.0-fold (5.0% to 9.8%) (p < 0.001 for all) (Table 1). However, the number of patients with hypertension (54.5% to 56.8%), diabetes mellitus (24.7% to 24.5%), and anemia (9.9% to 10.4%) remained relatively stable over this time period (Table 1).
Changes in Procedures and Mortality Over Time
Several changes in non-cardiac and cardiac procedures were observed during the study period from 2003 to 2013 (Table 2). For instance, mechanical (9.7% to 11.7%) and non-invasive ventilation rates (1.1% to 4.8%), central venous catheter use (7.6% to 8.8%), hemodialysis rates (3.4% to 4.8%), and transfusion use (10.2% to 14.0%) increased (p < 0.001 for all) (Table 2). With respect to cardiac procedures, pulmonary artery catheterization decreased from 1.8% to 1.1%, diagnostic cardiac catheterization declined from 25.7% to 16.5%, and PCI decreased from 12.2% to 9.1% (p < 0.001 for all) (Table 2). Similarly, CABG declined from 10.1% to 7.2% (p < 0.001). Mechanical circulatory support, in the form of intra-aortic balloon pump and ventricular assist device placement, remained stable over the study period from 1.8% to 1.9% (Table 2). The unadjusted in-hospital mortality rate decreased from 9.3% to 8.9% (p < 0.001) (Table 2).
Table 2.
Procedures and Outcomes Among Fee-For-Service Medicare Beneficiaries with a CICU Stay Between 2003 and 2013
| 2003 | 2005 | 2007 | 2009 | 2011 | 2013 | |
|---|---|---|---|---|---|---|
| General Invasive Procedures | ||||||
| Mechanical Ventilation | 9.7 | 9.9 | 9.6 | 10.6 | 11.0 | 11.7 |
| Non-Invasive Ventilation | 1.1 | 1.6 | 2.3 | 3.1 | 3.9 | 4.8 |
| Central Venous Catheterization | 7.6 | 9.1 | 10.6 | 12.5 | 10.8 | 8.8 |
| Hemodialysis | 3.4 | 3.8 | 4.1 | 4.5 | 4.7 | 4.8 |
| Transfusion | 10.2 | 11.9 | 13.6 | 14.7 | 14.8 | 14.0 |
| Cardiac Procedures | ||||||
| Pulmonary Artery Catheterization | 1.8 | 1.5 | 1.2 | 1.0 | 0.9 | 1.1 |
| Mechanical Circulatory Support | 1.8 | 2.0 | 1.8 | 1.9 | 1.8 | 1.9 |
| Diagnostic Cardiac Catheterization | 25.7 | 23.2 | 20.5 | 18.7 | 17.0 | 16.5 |
| Percutaneous Coronary Intervention | 12.2 | 12.9 | 12.0 | 10.3 | 9.6 | 9.1 |
| Coronary Artery Bypass Surgery | 10.1 | 9.2 | 8.1 | 7.9 | 6.8 | 7.2 |
| Length of Stay (days) | ||||||
| Median CICU LOS (IQR) | 3 (1–5) | 3 (2–5) | 3 (2–6) | 3 (2–6) | 3 (2–6) | 3 (2–6) |
| Median Hospital LOS (IQR) | 5 (3–9) | 5 (3–9) | 5 (3–9) | 5 (3–9) | 5 (3–9) | 5 (3–9) |
| Unadjusted In-Hospital Mortality | 9.3 | 9.0 | 8.5 | 8.7 | 8.5 | 8.9 |
p value < 0.001 for all comparisons. Mechanical Circulatory Support includes intra-aortic balloon pump placement and ventricular assist device placement.
Abbreviations: LOS = length of stay; IQR = interquartile range.
All values are reported as percentages unless otherwise noted.
Figure 2 shows risk-adjusted, in-hospital mortality rates over time in CICU patients in the overall cohort and stratified by primary non-cardiac and cardiac diagnoses. Risk-adjusted mortality declined modestly for patients admitted with primary non-cardiac diagnoses from 13.0% in 2003 to 11.2% in 2013 (p < 0.001) while risk-adjusted mortality was lower for patients admitted with primary cardiac diagnoses and remained relatively stable between 6.9% in 2003 and 6.6% in 2013. For the overall cohort, risk-adjusted mortality declined slightly from 9.3% to 8.9% (p < 0.001), similar to what was observed in the unadjusted analysis.
Figure 2.
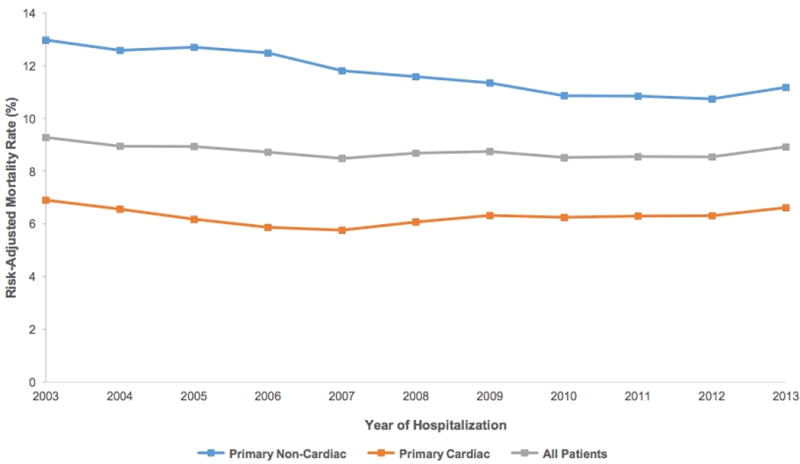
Risk-Adjusted, In-Hospital Mortality Rates Among Elderly Patients with a CICU Stay Between 2003 and 2013
Factors Associated with Primary Non-Cardiac Diagnoses and Findings Across Hospital Size
Table 3 describes differences in baseline characteristics, comorbidities, procedure use, and outcomes among patients with primary non-cardiac and cardiac diagnoses in 2012 and 2013. Patients with primary non-cardiac diagnoses were older (mean age 78 versus 77 years; p < 0.001), and were more likely to be women (52.5% versus 46.8%; p < 0.001) and black (10.7% versus 8.9%; p < 0.001) as compared with patients with primary cardiac diagnoses. Patients with primary non-cardiac diagnoses had higher rates of non-cardiac procedure utilization including mechanical (16.0% versus 6.5%; p < 0.001) and non-invasive (5.6% versus 3.3%; p < 0.001) ventilation, central venous catheterization use (13.2% versus 5.1%; p < 0.001), hemodialysis (5.9% versus 3.5%; p < 0.001) and transfusion use (18.5% versus 9.7%; p < 0.001) (Table 3). Patients with primary non-cardiac diagnoses also had higher unadjusted in-hospital mortality over the study period (10.9% versus 6.3%; p < 0.001) (Table 3). The proportion of primary non-cardiac diagnoses steadily increased at the same rate over the study period across small, medium, and large hospitals (p for interaction effect > 0.05), although primary non-cardiac diagnoses were more common at small hospitals overall (Figure 3). In particular, primary non-cardiac diagnoses increased from 44.7% to 58.1% at small hospitals, 38.2% to 51.0% at medium hospitals, and 29.9% to 45.6% at large hospitals (p < 0.001 for all) (Figure 3).
Table 3.
Characteristics, Procedures and Outcomes of Patients with Primary Cardiac and Non-Cardiac Diagnoses Admitted to the CICU in Years 2012 and 2013
| Non-Cardiac | Cardiac | |
|---|---|---|
| Number of Hospitalizations | n=260,742 | n=243,398 |
| Age (mean) | 78 | 77 |
| 65–74 | 37.3 | 41.8 |
| 75–84 | 36.8 | 36.8 |
| 85–94 | 23.5 | 19.7 |
| 95+ | 2.4 | 1.7 |
| Sex | ||
| Male | 47.5 | 53.2 |
| Female | 52.5 | 46.8 |
| Race | ||
| White | 83.3 | 85.9 |
| Black | 10.7 | 8.9 |
| Other | 6.0 | 5.1 |
| Elixhauser Comorbidities | ||
| 0–1 | 17.5 | 19.6 |
| 2 | 27.2 | 26.1 |
| ≥3 | 55.4 | 54.3 |
| Hypertension | 56.4 | 60.7 |
| Diabetes Mellitus | 22.4 | 27.0 |
| Obesity | 3.9 | 6.2 |
| Congestive Heart Failure | 30.8 | 37.2 |
| Valvular Heart Disease | 6.1 | 13.8 |
| Pulmonary Circulatory Disease | 6.0 | 7.6 |
| Peripheral Vascular Disease | 7.4 | 9.7 |
| Chronic Pulmonary Disease | 19.4 | 21.4 |
| Renal Failure | 19.2 | 20.4 |
| Malignancy | 7.6 | 3.6 |
| General Invasive Procedures | ||
| Mechanical Ventilation | 16.0 | 6.5 |
| Non-Invasive Ventilation | 5.6 | 3.3 |
| Central Venous Catheterization | 13.2 | 5.1 |
| Hemodialysis | 5.9 | 3.5 |
| Transfusion | 18.5 | 9.7 |
| Cardiac Procedures | ||
| Pulmonary Artery Catheterization | 0.3 | 1.9 |
| Mechanical Circulatory Support | 0.3 | 3.6 |
| Diagnostic Cardiac Catheterization | 3.1 | 30.9 |
| Percutaneous Coronary Intervention | 1.5 | 17.4 |
| Coronary Artery Bypass Surgery | 0.4 | 13.7 |
| Length of Stay (days) | ||
| Median CICU LOS (IQR) | 3 (2–6) | 3 (2–5) |
| Median Hospital LOS (IQR) | 6 (3–10) | 5 (2–8) |
| Unadjusted In-Hospital Mortality | 10.9 | 6.3 |
Mechanical Circulatory Support includes intra-aortic balloon pump placement and ventricular device placement.
Abbreviations: LOS = length of stay; IQR = interquartile range.
p < 0.001 for all comparisons except median CICU LOS. All values are reported as percentages unless otherwise noted
Figure 3.
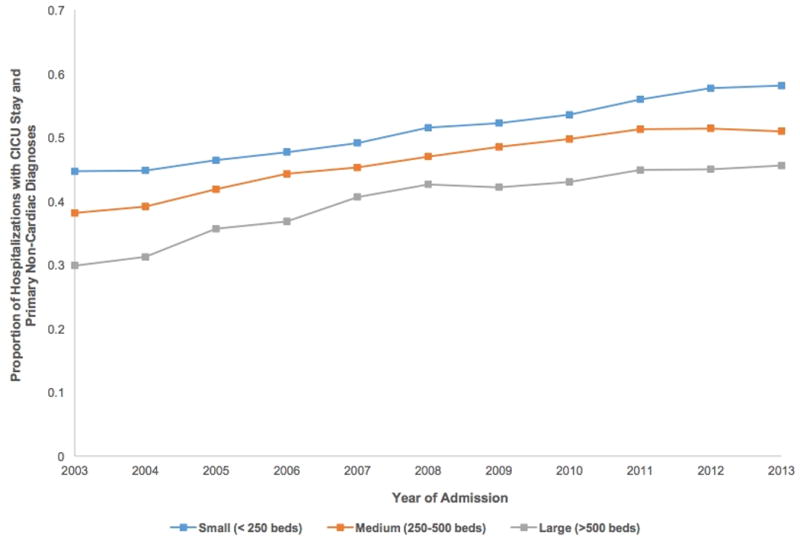
Proportion of Hospitalizations with CICU Stay Per Year and Primary Non-Cardiac Diagnoses Stratified by Hospital Size
DISCUSSION
Our study describes the changing face of critical care cardiology by examining population shifts and disease compositions over the last decade in fee-for-service Medicare hospitalizations with CICU stays in the United States. Specifically, we found that hospitalizations with a CICU stay are increasing for primary non-cardiac diagnoses while hospitalizations with a primary diagnosis of CAD have markedly declined. In addition, we found that co-morbidities—both cardiovascular and non-cardiovascular—have dramatically increased. CICU stays with primary non-cardiac diagnoses had higher rates of non-cardiac procedure use and higher risk-adjusted, in-hospital mortality. However, overall length of stay and risk-adjusted mortality did not worsen over time, and in fact, declined for the latter. These findings overall suggest the CICU may be increasingly becoming a setting where patients with cardiovascular disease are treated for a variety of acute, high-risk illnesses without compromising overall care.
We believe many factors are potentially driving the increase in patients with primary non-cardiac diagnoses receiving CICU care. Most importantly, significant improvement in the prevention and contemporary management of several acute cardiovascular diseases has occurred in recent years.20 For example, population-based rates of AMI have decreased substantially in the U.S. and the risk-adjusted mortality associated with those who suffer these events has also declined.21–23 Concurrent with the improvements in care for primary cardiac disease, the prevalence in cardiovascular comorbidities has also risen over time.18 This is due to both higher survival rates after acute events and an aging population, leading to a higher prevalence of heart failure, pulmonary vascular disease, and valvular heart disease. As these patients with chronic cardiovascular conditions are hospitalized, more of them may be brought to the CICU for any critical care needs.
A second possibility is that patients who might have been previously treated in traditional ICUs are now being managed in CICUs as hospitals attempt to maintain bed occupancy with declines in coronary artery disease. Our findings of a modest decline in the rate of hospitalizations with a CICU stay supports this possibility. Third, another reason may be that current non-cardiovascular critical care providers may feel unprepared in the management of complex cardiovascular critical illness in medical ICUs leading to a greater proportion of these patients being managed in the CICU.10 Fourth, the shift in coding toward primary non-cardiac diagnoses may reflect changes in reimbursement that encourage ‘up-coding’ or shifting of diagnoses toward higher categories of complex conditions. The fact that we found greater rates of co-morbidities despite stable-to-improving risk adjusted outcomes suggests this possibility. Unfortunately, the extent to which these phenomena are occurring is difficult to determine from the current analyses.
Regardless of the drivers of these changes, the significant evolution in the case mix of the CICU may have important ramifications for training and staffing models in cardiology, especially given the complexity of patients with primary non-cardiac diagnoses.24 Advanced, specialized training in critical care has not been specifically a part of most cardiologists’ training. A recent AHA position statement recognized this concern and suggested that the workforce around CICUs be geared toward a broader set of skills extending beyond the toolkit of general cardiologists.11 Reinforcing these concerns, in a 2012 survey of 178 medical directors of ICUs caring for cardiac patients, 81% of respondents identified an unmet need for cardiologists for intensivist training and expertise.25 Most recently, COCATS 4 added a new task force on training in critical care cardiology indicating those who wish to obtain level III or advanced training must complete a 1-year clinical fellowship in critical care medicine within the Department of Medicine in addition to the 3-year cardiovascular medicine fellowship.12, 13 Thus, given the complex patient care environment and escalating acuity of patients with primary non-cardiac diagnoses, the role of the intensivist in the CICU warrants further examination. Whether contemporary CICU providers should either co-manage with an intensivist or develop specialized expertise and in-depth knowledge to manage these heterogeneous, high-risk patients remains uncertain. Ultimately, the optimal care delivery model will have significant implications for the entire cardiac critical care team, including nurses, respiratory therapists, and pharmacists amongst others.
We also found that procedure use has significantly increased in CICUs over the past decade – a trend explained, in part, by the greater numbers of hospitalizations for primary non-cardiac diagnoses. Patients with primary non-cardiac diagnoses had higher rates of hemodialysis, transfusion use, mechanical and non-invasive ventilation, and central venous catheter use as well as higher unadjusted and risk-adjusted in-hospital mortality over the study period. Thus, CICUs have a heterogeneous patient case mix that, in many ways, mimics general medical intensive care units.6, 18 These findings are consistent with prior single center studies demonstrating shifts in demographic characteristics, discharge diagnoses, procedure use and outcomes over time in CICUs.7, 26 Our study extends these findings nationally, demonstrating these important temporal trends are not limited only to select academic medical centers. A final noteworthy observation was a steady decline in CICU hospitalizations from 2003 to 2013 from 93.7% to 74.3% (CICU per 1000 FFS hospitalizations). These findings are potentially explained by recent work demonstrating increases in billing for intermediate care among hospitalized Medicare beneficiaries between 1996 and 2010.27 Additional work is needed to identify drivers of this trend and its implications for CICUs.
Our study should be interpreted in the context of the following limitations. First, our analysis was derived from an administrative database and restricted to elderly patients hospitalized in the CICU, namely fee-for-service Medicare beneficiaries aged 65 years or older. Although national Medicare data provides a reasonable representation of CICU trends with respect to patient characteristics and diagnoses, our findings need to be confirmed in additional studies involving a broader payer mix and age distribution. Secondly, we did not specifically analyze the type of provider delivering care in the CICU (i.e., cardiologist vs. intensivist). However, this study illustrates important shifts in patterns of care in the modern CICU regardless of provider type. Understanding the types of providers involved with the care of patients with primary non-cardiac diagnoses in the CICU might help evaluate different models for care delivery.28 Third, we excluded 'boarders’ from our primary analysis to avoid counting hospitalizations for any patients who did not have a primary or secondary cardiac diagnosis at discharge. Although a sensitivity analysis was performed including these patients, our primary objective was to describe the types of patients being cared for in CICUs and not necessarily delineate the overall burden of critical care in patients with cardiovascular disease. Indeed, by describing all patients managed in CICUs (rather than cardiac patients in all ICUs), we have extended the literature on the types of patients and procedures provided in that setting and their implications for care delivery, staffing and training. Fourth, our risk-adjusted, in-hospital mortality models could not adjust for physiologic variables or severity of illness. Finally, our study relies on Medicare claims data and thus cannot specifically address the mechanisms driving the underlying shifts, such as changes in coding practices, changes in disease burden, or changes in ICU or hospitalized patients overall. Future work should probe these mechanisms and investigate the training and staffing implications of this evolving case mix in the cardiac intensive care unit.
Conclusions
We found major shifts in discharge diagnoses among fee-for-service Medicare beneficiaries hospitalized in CICUs from 2003 to 2013, with declining rates of discharges associated with primary cardiac diagnoses accompanied by a rise in patients with primary non-cardiac diagnoses and cardiovascular comorbidities. Furthermore, we found that patients with primary non-cardiac diagnoses had higher rates of procedure use and worse outcomes although their risk-adjusted in-hospital mortality is declining over time. Our work has important clinical and policy implications, including the development of appropriate training and staffing models for the future critical care workforce.
Supplementary Material
What is Known
Prior reports suggest cardiac intensive care units (CICUs) are increasingly managing complex patients with acute non-cardiac illnesses such as sepsis and renal failure but this evidence is derived from a handful of large academic centers.
No national data on the number, types and outcomes of patients admitted to CICUs across the U.S. with primary non-cardiac diagnoses currently exist.
What the Study Adds
Using national data from fee-for-service Medicare beneficiaries with CICU stays in the United States, we found declining rates of discharges associated with primary cardiac diagnoses accompanied by a concomitant rise in patients with primary non-cardiac diagnoses and secondary cardiovascular comorbidities.
Patients with primary non-cardiac diagnoses also had higher rates of procedure use and worse outcomes, but overall rates of risk-adjusted mortality declined slightly over time.
These findings have important clinical and policy implications, including the development of appropriate training and staffing models for the future critical care workforce within cardiology.
Acknowledgments
The authors wish to gratefully acknowledge the contributions of Wenying Zhang and Phyllis Wright-Slaughter with respect to data acquisition. We also appreciate the statistical support provided by Jyothi Thumma. Finally, we wish to thank Dr. Mohamad Kenaan for his critical review of the manuscript. Drs. Sinha and Sjoding had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Sinha, Sjoding, Sukul, Cooke, Nallamothu. Acquisition, analysis, or interpretation of data: Sinha, Sjoding, Sukul, Cooke, Nallamothu. Drafting of the manuscript: Sinha. Critical revision of the manuscript for important intellectual content: Sinha, Sjoding, Sukul, Prescott, Iwashyna, Gurm, Cooke, Nallamothu. Statistical analysis: Sinha, Sjoding, Sukul, Cooke, Nallamothu. Obtained funding: Iwashyna, Gurm, Cooke, Nallamothu. Study supervision: Nallamothu
Sources of Funding: Drs. Sinha and Sukul are supported by the National Institutes of Health (NIH) T32 postdoctoral research training grant (5T32HL007853). Dr. Sjoding (NHLBI T32HL0077490) and Dr. Prescott (K08 GM115859) also receive funding from the NIH. Both Dr. Iwashyna and Dr. Nallamothu are supported by a research grant from the VA Health Services Research & Development Program (IIR 13-079-2). Dr. Gurm receives research funding from Blue Cross Blue Shield of Michigan and the National Institutes of Health. Dr. Cooke is supported by AHRQ (K08 HS020672). Dr. Nallamothu is supported by a research grant from the National Heart, Lung, and Blood Institute (NHLBI, 1R01HL123980).
Footnotes
The views expressed herein are those of the authors and do not necessarily represent those of the U.S. Department of Veterans Affairs.
Disclosures: Dr. Gurm is a consultant for Osprey Medical. None of the authors have any financial disclosures or conflicts of interest directly relevant to the study to disclose.
References
- 1.Zoll PM, Linenthal AJ, Gibson W, Paul MH, Norman LR. Termination of ventricular fibrillation in man by externally applied electric countershock. N Engl J Med. 1956;254:727–732. doi: 10.1056/NEJM195604192541601. [DOI] [PubMed] [Google Scholar]
- 2.Lown B, Amarasingham R, Neuman J. New method for terminating cardiac arrhythmias. Use of synchronized capacitor discharge. JAMA. 1962;182:548–555. [PubMed] [Google Scholar]
- 3.Julian DG. Treatment of cardiac arrest in acute myocardial ischaemia and infarction. Lancet. 1961;2:840–844. doi: 10.1016/s0140-6736(61)90738-3. [DOI] [PubMed] [Google Scholar]
- 4.Killip T, 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol. 1967;20:457–464. doi: 10.1016/0002-9149(67)90023-9. [DOI] [PubMed] [Google Scholar]
- 5.Fye WB. Resuscitating a Circulation abstract to celebrate the 50th anniversary of the Coronary Care Unit concept. Circulation. 2011;124:1886–1893. doi: 10.1161/CIRCULATIONAHA.111.033597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz JN, Minder M, Olenchock B, Price S, Goldfarb M, Washam JB, Barnett CF, Newby LK, van Diepen S. The Genesis, Maturation, and Future of Critical Care Cardiology. J Am Coll Cardiol. 2016;68:67–79. doi: 10.1016/j.jacc.2016.04.036. [DOI] [PubMed] [Google Scholar]
- 7.Katz JN, Shah BR, Volz EM, Horton JR, Shaw LK, Newby LK, Granger CB, Mark DB, Califf RM, Becker RC. Evolution of the coronary care unit: clinical characteristics and temporal trends in healthcare delivery and outcomes. Crit Care Med. 2010;38:375–381. doi: 10.1097/CCM.0b013e3181cb0a63. [DOI] [PubMed] [Google Scholar]
- 8.Ratcliffe JA, Wilson E, Islam S, Platsman Z, Leou K, Williams G, Lucido D, Moustakakis E, Rachko M, Bergmann SR. Mortality in the coronary care unit. Coron Artery Dis. 2014;25:60–65. doi: 10.1097/MCA.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 9.Ensminger SA, Wright RS, Baddour LM, Afessa B. Suspected ventilator-associated pneumonia in cardiac patients admitted to the coronary care unit. Mayo Clin Proc. 2006;81:32–35. doi: 10.4065/81.1.32. [DOI] [PubMed] [Google Scholar]
- 10.Hill T, Means G, van Diepen S, Paul T, Katz JN. Cardiovascular Critical Care: A Perceived Deficiency Among U.S. Trainees. Crit Care Med. 2015;43:1853–1858. doi: 10.1097/CCM.0000000000001074. [DOI] [PubMed] [Google Scholar]
- 11.Morrow DA, Fang JC, Fintel DJ, Granger CB, Katz JN, Kushner FG, Kuvin JT, Lopez-Sendon J, McAreavey D, Nallamothu B, Page RL, 2nd, Parrillo JE, Peterson PN, Winkelman C American Heart Association Council on Cardiopulmonary CCP, Resuscitation CoCCCoCN, Council on Quality of C and Outcomes R. Evolution of critical care cardiology: transformation of the cardiovascular intensive care unit and the emerging need for new medical staffing and training models: a scientific statement from the American Heart Association. Circulation. 2012;126:1408–1428. doi: 10.1161/CIR.0b013e31826890b0. [DOI] [PubMed] [Google Scholar]
- 12.O'Gara PT, Adams JE, 3rd, Drazner MH, Indik JH, Kirtane AJ, Klarich KW, Newby LK, Scirica BM, Sundt TM., 3rd COCATS 4 Task Force 13: Training in Critical Care Cardiology. J Am Coll Cardiol. 2015;65:1877–1886. doi: 10.1016/j.jacc.2015.03.027. [DOI] [PubMed] [Google Scholar]
- 13.Sinha SS, Julien HM, Krim SR, Ijioma NN, Baron SJ, Rock AJ, Siehr SL, Cullen MW American College of Cardiology Fellow-in-Training Section Leadership C. COCATS 4: Securing the Future of Cardiovascular Medicine. J Am Coll Cardiol. 2015;65:1907–1914. doi: 10.1016/j.jacc.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 14.Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, Naghavi M, Mensah GA, Murray CJ. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333–1341. doi: 10.1056/NEJMoa1406656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Writing Group M; Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jimenez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, 3rd, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB American Heart Association Statistics C and Stroke Statistics S. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133:e38–360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 16.Krumholz HM, Nuti SV, Downing NS, Normand SL, Wang Y. Mortality, Hospitalizations, and Expenditures for the Medicare Population Aged 65 Years or Older, 1999–2013. JAMA. 2015;314:355–365. doi: 10.1001/jama.2015.8035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cowen ME, Dusseau DJ, Toth BG, Guisinger C, Zodet MW, Shyr Y. Casemix adjustment of managed care claims data using the clinical classification for health policy research method. Med Care. 1998;36:1108–1113. doi: 10.1097/00005650-199807000-00016. [DOI] [PubMed] [Google Scholar]
- 18.Sjoding MW, Prescott HC, Wunsch H, Iwashyna TJ, Cooke CR. Longitudinal Changes in ICU Admissions Among Elderly Patients in the United States. Crit Care Med. 2016;44:1353–1360. doi: 10.1097/CCM.0000000000001664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Narang A, Sinha SS, Rajagopalan B, Ijioma NN, Jayaram N, Kithcart AP, Tanguturi VK, Cullen MW. The Supply and Demand of the Cardiovascular Workforce: Striking the Right Balance. J Am Coll Cardiol. 2016;68:1680–1689. doi: 10.1016/j.jacc.2016.06.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 22.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 23.Ford ES, Ajani UA, Croft JB, Critchley JA, Labarthe DR, Kottke TE, Giles WH, Capewell S. Explaining the decrease in U.S. deaths from coronary disease, 1980–2000. N Engl J Med. 2007;356:2388–2398. doi: 10.1056/NEJMsa053935. [DOI] [PubMed] [Google Scholar]
- 24.Katz JN. Who Belongs in the Cardiac Intensive Care Unit? JAMA Cardiol. 2017;2:45–46. doi: 10.1001/jamacardio.2016.3881. [DOI] [PubMed] [Google Scholar]
- 25.O'Malley RG, Olenchock B, Bohula-May E, Barnett C, Fintel DJ, Granger CB, Katz JN, Kontos MC, Kuvin JT, Murphy SA, Parrillo JE, Morrow DA. Organization and staffing practices in US cardiac intensive care units: a survey on behalf of the American Heart Association Writing Group on the Evolution of Critical Care Cardiology. Eur Heart J Acute Cardiovasc Care. 2013;2:3–8. doi: 10.1177/2048872612472063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quinn T, Weston C, Birkhead J, Walker L, Norris R, Group MS. Redefining the coronary care unit: an observational study of patients admitted to hospital in England and Wales in 2003. QJM. 2005;98:797–802. doi: 10.1093/qjmed/hci123. [DOI] [PubMed] [Google Scholar]
- 27.Sjoding MW, Valley TS, Prescott HC, Wunsch H, Iwashyna TJ, Cooke CR. Rising Billing for Intermediate Intensive Care among Hospitalized Medicare Beneficiaries between 1996 and 2010. Am J Respir Crit Care Med. 2016;193:163–170. doi: 10.1164/rccm.201506-1252OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Morrow DA. Evidence-Based Redesign of the Cardiac Intensive Care Unit. J Am Coll Cardiol. 2016;68:2649–2651. doi: 10.1016/j.jacc.2016.10.030. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


