Abstract
Background
Empathy is an essential aspect of clinical care, associated with improved patient satisfaction, increased adherence to treatment, and fewer malpractice complaints. Previous studies suggest that empathy declines during medical training. However, this past research relied on a single narrowly operationalized self-report measure of empathy. As empathy is a complex socio-emotional construct, it is critical to assess changes across its distinct components using multiple measures, to better understand how medical training influences empathy.
Methods
In a longitudinal design, medical students completed a series of self-report and behavioral measures twice a year during the first three years of their study (2012 – 2015). These included the previously used Jefferson Scale of Physician Empathy (JSE), designed to assess empathy in the clinical context, the Questionnaire of Cognitive and Affective Empathy (QCAE), designed to assess overall empathy and its main components, and behavioral measures of sensitivity to others’ pain and understanding of other’s emotions, both important aspects of empathy. Employing multiple measures allowed for a more complete assessment of medical students’ empathy and related processes.
Results
Replicating previous work, students’ empathy assessed by the JSE decreased over training. However, on the QCAE, aspects of students empathy, specifically overall cognitive empathy and it’s subcomponent perspective-taking and the emotion contagion subcomponent of affective empathy improved while the remaining subcomponents stayed stable. Students also exhibited comparable growth in their understanding of others’ emotions and increased sensitivity for others’ pain during medical school.
Conclusions
Changes in empathy during medical school cannot be simply characterized as an overall decline. Indeed, aspects of empathy thought to be valuable in positive patient physician interactions improve during training. Overall, this study points to the importance of assessing the distinct components of empathy using multiple forms of measurement in order to better understand the mechanisms involved in empathy changes in medical practice.
Introduction
It is generally acknowledged that empathy is beneficial, and that it should be the basis of attitudes towards patient care, or should at least play an important role in the doctor-patient relationship alongside deductive logic, physical examinations, and treatment(1). Physician empathy is associated with multiple beneficial outcomes for both the patient and physician, including increased patient adherence to treatment, fewer malpractice complaints, and increased physician health, well-being, and professional satisfaction(2) along with decreased burnout, personal distress, depression, and anxiety(3–5). Additionally, patients’ perceptions of their physicians’ empathy are positively associated with more favorable health outcomes(6,7).
This relationship between empathy and improved physician and patient outcomes has led to the argument that empathy is critical in physician patient interactions(1,8,9). Despite this, research suggests that empathy declines over the course of medical school, with medical students exhibiting decreases in self-reported empathy during their studies(10). Worryingly, it is thought the steepest decreases occur between medical students’ second and third year as they begin their clinical training(10), a time when empathic communication is critical. However, it is not clear how reliable this decline is(11). Recent work failed to find changes in empathy during medical school(12), or found only declines in some aspects of empathy and none in others(13). There is some evidence for increases in behavioral aspects of empathy(14). This suggests that empathy changes during medical training may be more complex than an overall decline.
Empathy reflects an innate ability to perceive and be sensitive to the emotional states of others coupled with a motivation to care for their wellbeing. This construct encompasses both cognitive and affective components which are intertwined and not completely separable from one another(15–18), making it important to assess them in concert as each contributes to various aspects of the experience of empathy and its outcomes such as caring.
In medicine, cognitive empathy is generally considered as the ability to recognize and understand another’s experience, to communicate and confirm that understanding with the other person, and to take effective action to then act appropriately in a helpful manner(19); affective empathy, is viewed as a form of emotional resonance or attunement with the patient(17). The medical literature on empathy emphasizes cognitive empathy as most important to the clinical interaction given it enables physicians’ understanding of how their patients feel without sharing those emotions. Affective empathy, being attuned to the patients emotions, is thought to impede the physician’s ability to effectively diagnose and treat the patient(20). However, this conceptualization is both simplistic and misleading. There is convincing empirical evidence from developmental science, social neuroscience, and clinical neuroscience that the cognitive and affective facets of empathy interact in the experience of empathy(15,21–25), and contribute in facilitating the physician patient interaction(26). It is important for physicians to both accurately recognize their patients’ emotions and react accordingly(27), making it critical to examine the multiple processes and components involved in changes in empathy during medical school with the goal of better understanding how empathy evolves over the course of this training and what factors contribute to that change.
Most of the research reporting negative changes in empathy during medical school has primarily relied on one self-report measure, the Jefferson Scale of Physician Empathy (JSE) designed to assess cognitive empathy specifically within the patient-physician interaction(10,28). However, relying on this sole measure as a primary form of assessment is potentially misleading given it focuses on one component of empathy, neglecting the complex integration across empathic components and processes, making it difficult to understand the mechanisms underlying observed changes. Indeed, some work indicates that changes in components of empathy measured behaviorally demonstrates different patterns across medical training than self-report measures(14). Additionally, there is evidence that self-reported empathy as measured by the JSE does not correlate with observer reported empathy(29), which is the most pertinent to the physician-patient relationship, as the patient’s perception of the physician’s empathy is going to shape how they respond to the physician. This, along with the lack of consensus on how reliable those changes are across medical training(12,13), makes it critical to further our understanding of what contributes to those alterations by assessing both cognitive and affective facets of empathy alongside the behavioral expressions of those components.
Within the broader literature on empathy, this construct is typically measured using a combination of self-report and behavioral measures to understand the underlying neurological and physiological mechanisms promoting empathy and caring (15,27,30,31). The Questionnaire of Cognitive and Affective Empathy (QCAE) (32–35) was developed to address inconsistencies in current measurement tools such as the Interpersonal Reactivity Index (IRI). It reliably assesses the different components of empathy (cognitive and affective and their respective subcomponents) based on the social cognitive neuroscience literature on empathy and it’s underlying neural processes. This measure captures the multidimensional nature of empathy as a complex socioemotional construct(32), and allows for a more complete assessment of empathy as a construct. Utilizing these measures in combination with behavioral manifestations of empathy provides a comprehensive framework to identify the mechanisms underlying and contributing to individuals’ empathetic capacity. These behavioral measures include cognitive tasks that assess individuals’ sensitivity to suffering of others, via rating videos depicting individuals’ expressing pain (36), and those assessing individuals’ understanding of others’ thoughts and emotions, such as the Reading the Mind in the Eyes Test (RMET) (37). Incorporating this variety of measurement when assessing empathy in medical students and physicians can help provide a more complete understanding of how empathy changes over the course of medical school and what processes underlie those observed changes. It also has the potential to provide insight into the current observed discrepancies within the medical empathy literature, which is likely in part due to differing forms of assessment.
The current study aims to examine multiple facets of empathy through four primary questions: 1) How does cognitive empathy specific to the patient-physician relationship, as assessed in much of the previous work (using the JSE), change over the course of medical school; 2) How does empathy and it’s subcomponents assessed more broadly change (using the QCAE) over the course of medical training and do these changes differ from those observed with the JSE; 3) How do behavioral manifestations of empathy (individuals’ sensitivity to pain and understanding of others thoughts and emotions) change over the course of medical training; and 4) Are these changes related, and how can these relationships inform our understanding of the mechanisms underlying empathy changes during medical school? To do this, we collected self-report measures (i.e JSE and QCAE), and behavioral measures (ratings of videos of individuals expressing pain and the RMET) to assess medical students’ sensitivity to pain in others, and their understanding of others’ thoughts and emotions.
Methods
Participants
All first year students at three Chicago medical schools (Loyola, Northwestern, University of Chicago) were emailed by their respective Dean and asked if they were interested in participating in the study. To reduce any potential bias due to students thinking participation may affect their academic career, this letter stressed the voluntary nature of the study, unrelated to their own academic studies, and informed students that all the data would be kept confidential by the research team. Of 406 eligible students, 129 (62 male) medical students, aged 21 – 33, volunteered to participate in the study (80 (62%) Caucasian, 18 (14%) Asian/Asian American, 8 (6.2%) African American, 6 (4.7%) Hispanic/Latino, 16 (12.4%) multi-racial, and the remainder identifying as other. (For demographic information separated by school, see Table 1). This sample is similar to those observed in previous studies(10,14) as well as overall class compositions at the respective medical schools. Participants gave written informed consent and were provided with $60 compensation at each study appointment. This study was approved by the University of Chicago’s Institutional Review Board and conducted in accordance with the Declaration of Helsinki.
Table 1.
Demographic information by school (three prestigious schools in the Chicago area) for 129 medical students at the beginning of medical school (2012)
| School | Number of Students | Age (years) | Race | Gender | |
|---|---|---|---|---|---|
| 1 | 34 | 23.44 (2.32) |
Asian/Asian American | 4 (11.8%) | M – 13 (38.2%) F – 21 (61.7%) |
| African American | 4 (11.8%) | ||||
| Hispanic/Latino | 0 (0%) | ||||
| Caucasian | 22 (64.7%) | ||||
| Multi | 4 (11.8%) | ||||
| Other | 0 (0%) | ||||
|
| |||||
| 2 | 43 | 23.12 (1.90) |
Asian/Asian American | 10 (23.3%) | M – 20 (46.5%) F – 23 (53.5%) |
| African American | 2 (4.7%) | ||||
| Hispanic/Latino | 5 (11.6%) | ||||
| Caucasian | 21 (48.8%) | ||||
| Multi | 5 (11.6%) | ||||
| Other | 0 (0%) | ||||
|
| |||||
| 3 | 52 | 23.58 (1.50) |
Asian/Asian American | 4 (7.7%) | M – 29 (55.8%) F – 23 (44.2%) |
| African American | 2 (3.8%) | ||||
| Hispanic/Latino | 1 (1.9%) | ||||
| Caucasian | 37 (71.2%) | ||||
| Multi | 1 (1.9%) | ||||
| Other | 7 (13.5%) | ||||
Procedure
Students attended appointments at the beginning and end of each academic year for their first three years of medical school (2012 – 2015). At each appointment, students completed a set of online surveys and computerized tasks, assessing different components of empathy. The number of students no longer in the study by the last data collection time point was low: n = 15 (11.6%) (for table of dropout rates by school see Appendix S1; available online), and 108 of the 129 subjects (83.7%) had complete data for all time points (for sample characteristics of students who dropped out see Appendix S1). For analyses, we included participants with full survey data for at least 3 of the 6 time-points, n = 122 (58 male).
Survey Measures
Students’ completed two questionnaires assessing changes in empathy over the course of their medical training. First was the Jefferson Scale of Physician Empathy – Student Version (JSE), developed to measure physician and medical student empathy specific to patient interactions (for validity and reliability see(38)). As the JSE is thought to assesses primarily cognitive aspects of clinical empathy(38), students also completed the Questionnaire of Cognitive and Affective Empathy (QCAE), which assesses overall cognitive and affective empathy in concert (for validity and reliability see(32)). The QCAE comprises two main scales, cognitive and affective empathy, as well as five subscales (see Appendix S1 for scale information and scoring). The QCAE was chosen to assess empathy because of its clear distinction between the two main components of empathy and their underlying processes compared to other common measures such as the Interpersonal Reactivity Index(32).
Behavioral Measures
At each appointment, students completed a set of computerized behavioral tasks assessing processes important to empathy. First, students’ sensitivity to pain was measured by having participants view ten videos of different individuals expressing pain, and rating the amount of pain being experienced using a visual analogue scale from “no pain” to “intense pain”(36). Participants’ ability to infer other’s mental states was assessed using a modified version of the Reading the Eyes in the Mind Task (RMET)(37). During the RMET, participants saw 24 black and white images of eyes expressing different mental states with a forced choice between four different mental states for each. Participants’ performance was coded by how accurate they were at identifying the correct mental state and their log transformed reaction time to respond for trials in which they correctly identified the mental state. For both tasks, there were two sets of stimuli, randomized and counterbalanced across students and appointments, so students never saw the same set of images at two appointments in a row.
Statistical Analyses
To assess changes in empathy and its related processes over the course of the first three years of medical school, we utilized hierarchical linear modeling (HLM) techniques, a complex form of ordinary least square (OLS) regression fits a linear function to the observed data while accounting for variation across individuals to estimate the population level rate of change based on the observed data set.(39,40). Given longitudinal data are inherently nested with time grouped within subject (each individual has a series of outcomes for each time point), and HLM accounts for potential variation in observed outcomes across individuals, HLM was deemed the more appropriate method of analysis (as compared to repeated measure ANOVA) (39). Additionally, HLM can handle missing values without imputation (i.e. replacing missing values with substituted values based on distribution of data set) which is well suited for the current data set where we did not have complete data for each subject at every time point (39). All models were run using the nlme package for R, developed for building hierarchical linear models, with full maximum likelihood estimation (method of computing estimates of population parameters that jointly maximize the likelihood of observing a particular sample of data; for more explanation see 25) in R v3.2.3.
Inspection of individual subject level trajectories indicated that a linear growth model was most appropriate for the data set and there was no indication that growth patterns differed across the summer versus academic months. For each outcome measure we assessed two models, the first including only time as a predictor. As gender (32) and age (41) have previously been associated with empathy, the second model incorporated these variables to control for any effects. Since the RMET and pain sensitivity tasks included two stimulus set versions, an additional model, including order, age, and gender, was created accounting for any potential effects of order of presentation of the sets (for model equations as well as a discussion of missing data, see Appendix S1). All control covariates were mean centered. Model fit was assessed using chi-square tests comparing log likelihood values.
Results
Changes in Empathy
Students exhibited a significant decline over time in JSE scores (β = −0.030, SE = 0.900, p < 0.01; Figure 1). This effect remained significant after controlling for gender and age (β = −0.092, SE = 0.030, p < 0.01), and there were significant effects of gender (β = 5.21, SE = 1.72, p < 0.01) and age (β = 1.36, SE = 1.36, p < 0.01) on initial status but not rate of change, with women exhibiting higher initial scores compared to men and initial scores being higher for older students. In contrast, students exhibited increases in QCAE total scores over time (β = 0.053, SE = 0.477, p < 0.05). This effect remained significant after controlling for gender and age (β = 0.024, SE = 0.024, p < 0.05). Gender had a significant effect on initial scores (β = 8.13, SE = 1.56, p < 0.001), but not rate of change, with women exhibiting higher scores compared to men. This pattern was the same for all of the subscales examined except for the cognitive scale online simulation which had no significant effects of predictors. Age did not have a significant effect on initial scores, but did have a significant effect on rate of change, with older students demonstrating a less steep slope of change (β = −0.033, SE = 0.013, p < 0.0). Examining the subscales revealed that there were significant increases in overall cognitive empathy (β = 0.042, SE = 0.018, p < 0.05), specifically the ability to take the perspective of others (β = 0.036, SE = 0.011, p < 0.01; Figure 1). After incorporating gender and age, the effect of time on overall cognitive empathy (β = 0.043, SE = 0.018, p < 0.05) and perspective taking (β = 0.034, SE = 0.011, p < 0.01) remained significant. Age had a significant effect on initial score for overall cognitive empathy (β = 0.65, SE = 0.327, p < 0.05) but not rate of change, with older students having higher initial cognitive empathy scores than younger students, and no significant effects on either initial scores or rate of change for perspective taking. There were no significant effects of time on overall affective empathy or any of the affective subscales, except for emotion contagion, which demonstrated a significant effect with score increasing over time (β = 0.012, SE = 0.006, p < 0.05), and this remained unchanged after incorporating gender and age. For both overall affective empathy and emotion contagion there were significant effects of age on rate of change (β = −0.022, SE = 0.006, p < 0.001; β = −0.009, SE = 0.003, p < 0.01 respectively), with older students demonstrating a less steep slope of change. Overall, these results suggest that students’ affective empathy primarily remained stable over the course of training while cognitive empathy increased (for full model results see Table 2). For all models except for online stimulation, the model including age, gender, and time demonstrated the best fit, indicating that these factors, even if not significant predictors, are important to explaining medical students empathy levels and changes over the course of medical school and should be taken into account when trying to understand the mechanisms underlying these changes.
Figure 1.
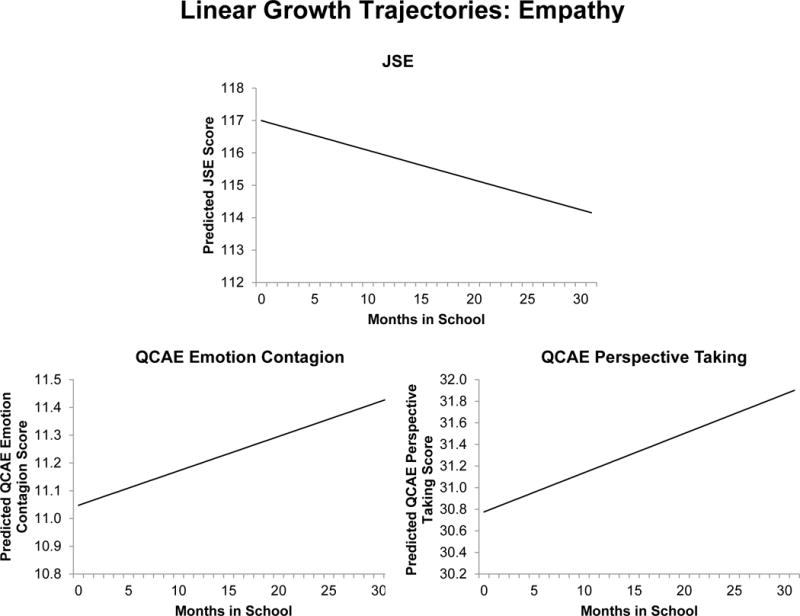
Linear growth trajectories for the JSE and QCAE Perspective Taking Scale based on linear models for 122 medical students followed over their first three years of school (2012 – 2015).
Table 2.
Linear growth model results for questionnaire measures for 122 medical students followed over their first three years of study (2012 – 2015). Model A: includes only time as a predictor. Model B: Includes time, gender, and age as predictors. Degrees of freedom correspond to the classical decomposition of degrees of freedom in balanced, multilevel ANOVA designs.
| Questionnaire | Effect | Model A | Model B | ||||
|---|---|---|---|---|---|---|---|
| β (SE) |
df | β (SE) |
df | ||||
| JSPE | Initial Status | Intercept | 117.09*** (0.900) |
582 | 117.09*** (0.851) |
580 | |
| Gender | – | – | 5.22 ** (1.722) |
119 | |||
| Age | – | – | 1.36** (0.481) |
119 | |||
| Rate of Change | Time | −0.092** (0.030) |
582 | −0.092* (0.030) |
580 | ||
| Gender | – | – | 0.011 (0.061) |
580 | |||
| Age | – | – | −0.001 (0.017) |
580 | |||
| QCAE | Total | Initial Status | Intercept | 93.16*** (0.855) |
592 | 93.15*** (0.772) |
590 |
| Gender | – | – | 8.14 *** (1.56) |
119 | |||
| Age | – | – | 0.837† (0.436) |
119 | |||
| Rate of Change | Time | 0.053* (0.024) |
592 | 0.053* (0.024) |
590 | ||
| Gender | – | – | −0.003 (0.048) |
590 | |||
| Age | – | – | −0.033* (0.013) |
590 | |||
| Affective | Initial Status | Intercept | 34.24 *** (0.474) |
592 | 34.24*** (0.406) |
590 | |
| Gender | – | – | 5.46*** (0.821) |
119 | |||
| Age | – | – | 0.187 (0.230) |
119 | |||
| Rate of Change | Time | 0.011 (0.012) |
592 | 0.011 (0.012) |
590 | ||
| Gender | – | – | −0.002 (0.023) |
590 | |||
| Age | – | – | −0.022** (0.006) |
590 | |||
| Affective: Emotion Contagion | Initial Status | Intercept | 11.04*** (0.194) |
592 | 11.03*** (0.188) |
590 | |
| Gender | – | – | 0.990* (0.381) |
119 | |||
| Age | – | – | −0.121 (0.106) |
119 | |||
| Rate of Change | Time | 0.012† (0.006) |
592 | 0.012* (0.006) |
590 | ||
| Gender | – | – | 0.014 (0.012) |
590 | |||
| Age | – | – | −0.009** (0.003) |
590 | |||
| Affective: Proximal Responsivity | Initial Status | Intercept | 11.97*** (0.184) |
592 | 11.97*** (0.167) |
590 | |
| Gender | – | – | 1.76*** (0.38) |
119 | |||
| Age | – | – | 0.103 (0.094) |
119 | |||
| Rate of Change | Time | −0.005 (0.005) |
592 | −0.004 (0.005) |
590 | ||
| Gender | – | – | 0.002 (0.011) |
590 | |||
| Age | – | – | −0.005† (0.003) |
590 | |||
| Affective: Peripheral Responsivity | Initial Status | Intercept | 11.24*** (0.228) |
592 | 11.24*** (0.194) |
590 | |
| Gender | – | – | 2.71*** (0.392) |
119 | |||
| Age | – | – | 0.204† (0.109) |
119 | |||
| Rate of Change | Time | 0.003 (0.005) |
592 | 0.003 (0.005) |
590 | ||
| Gender | – | – | −0.019† (0.011) |
590 | |||
| Age | – | – | −0.007* (0.003) |
590 | |||
| Cognitive | Initial Status | Intercept | 58.91*** (0.597) |
592 | 58.91*** (0.579) |
590 | |
| Gender | – | – | 2.70* (1.17) |
119 | |||
| Age | – | – | 0.654* (0.327) |
119 | |||
| Rate of Change | Time | 0.042* (0.018) |
592 | 0.043* (0.018) |
590 | ||
| Gender | – | – | 0.004 (0.036) |
590 | |||
| Age | – | – | −0.012 (0.010) |
590 | |||
| Cognitive: Perspective Taking | Initial Status | Intercept | 30.74*** (0.415) |
592 | 30.74*** (0.406) |
590 | |
| Gender | – | – | 1.90* (0.821) |
119 | |||
| Age | – | – | 0.302 (0.229) |
119 | |||
| Rate of Change | Time | 0.036** (0.011) |
592 | 0.036** (0.011) |
590 | ||
| Gender | – | – | −0.015 (0.022) |
590 | |||
| Age | – | – | −0.008 (0.006) |
590 | |||
| Cognitive: Online Simulation | Initial Status | Intercept | 28.18*** (0.335) |
592 | 28.17*** (0.330) |
590 | |
| Gender | – | – | 0.798 (0.668) |
119 | |||
| Age | – | – | 0.349† (0.186) |
119 | |||
| Rate of Change | Time | 0.0.006 (0.0.010) |
592 | 0.006 (0.010) |
590 | ||
| Gender | – | – | 0.019 (0.021) |
590 | |||
| Age | – | – | −0.002 (0.006) |
590 | |||
Significance levels:
p<0.10,
p<0.05,
p<0.01,
p<0.001
Changes in Behavioral Measures
Students improved at accurately recognizing other’s emotional states, exhibiting significant increases in accuracy (β = 0.001, SE = 0.0003, p < 0.01) and significant decreases in reaction times on the RMET over time (β = −0.013, SE = 0.001, p < 0.001; Figure 2). These effects remained significant after controlling for gender, age, and order (Accuracy: β = 0.001, SE = 0.001, p < 0.05; Reaction time: β = −0.016, p < 0.001). Gender, order, and age had no significant effects on rate of change of performance. However, gender had a significant effect on initial scores for reaction time (β = −0.161, p < 0.01), suggesting women exhibited faster reaction times for accurate judgments than men. Students also demonstrated a trend towards increased ratings of other’s pain over time (β = 0.073, SE = 0.039, p = 0.064; Figure 2). However, this effect became significant after controlling for gender, order, and age (β = 0.324, SE = 0.087, p < 0.01). Gender and age had no significant effects on pain ratings, but order significantly affected change over time (β = 0.254, SE = 0.078, p < 0.01) (for more explanation of order effects see Appendix S1). Overall, over the course of medical training, students appear to become more sensitive to others’ feelings and mental states. (For full model results for behavioral outcomes see Table 3.) For RMET accuracy, the best fit model was the model including only time indicating that including order, gender, and age does not account for significantly more variability in the data beyond that accounted for by time. This suggests that these factors are not significant contributors to variability in individuals’ accuracy on the RMET. In contrast, for RMET reaction times the best fit model included gender, age, order, and time suggesting these additional factors (even if not significant predictors) along with time are important to explaining the observed data and should be taken into account. This was also the case for pain sensitivity, indicating that order, gender, and age are also important explanatory variables in students’ sensitivity to pain in others for this stimulus set.
Figure 2.
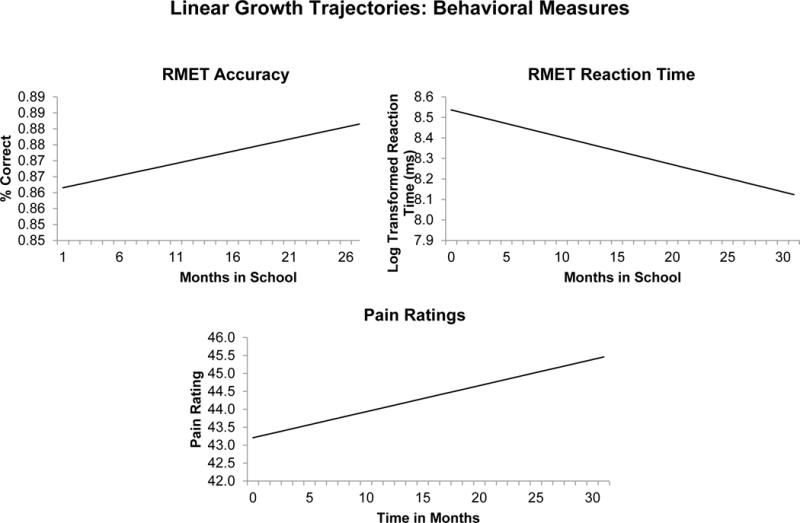
Linear growth trajectories for the RMET, a performance-based measure involving mental state attribution and complex facial emotion recognition, and sensitivity to others’ pain based on linear models for 122 medical students followed over their first three years of school (2012 – 2015).
Table 3.
Linear growth model results for behavioral measures for 122 medical students followed over their first three years of study (2012 – 2015). Model A: includes only time as a predictor. Model B: Includes time, gender, age, and order as predictors. Degrees of freedom correspond to the classical decomposition of degrees of freedom in balanced, multilevel ANOVA designs.
| Task | Effect | Model A | Model B | ||||
|---|---|---|---|---|---|---|---|
| β (SE) |
df | β (SE) |
df | ||||
| RMET | Accuracy | Initial Status | Intercept | 0.861*** (0.005) |
571 | 0.859*** (0.011) |
568 |
| Gender | – | – | −0.003 (0.010) |
118 | |||
| Age | – | – | −0.005† (0.003) |
118 | |||
| Order | – | – | −0.002 (0.010) |
118 | |||
| Rate of Change | Time | 0.001** (0.0002) |
571 | 0.001* (0.001) |
568 | ||
| Gender | – | – | 0.001 (0.001) |
568 | |||
| Age | – | – | 0.0001 (0.0001) |
568 | |||
| Order | – | – | 0.0004 (0.001) |
568 | |||
| Reaction Time | Initial Status | Intercept | 8.55*** (0.028) |
571 | 8.52*** (0.061) |
568 | |
| Gender | – | – | −0.161** (0.055) |
118 | |||
| Age | – | – | 0.020 (0.015) |
118 | |||
| Order | – | – | −0.033 (0.055) |
118 | |||
| Rate of Change | Time | 0.013*** (0.001) |
571 | −0.016*** (0.002) |
568 | ||
| Gender | – | – | 0.003† (0.002) |
568 | |||
| Age | – | – | −0.0004 (0.0004) |
568 | |||
| Order | – | – | −0.002 (0002) |
568 | |||
| Pain | Initial Status | Intercept | 43.13*** (0.975) |
570 | 39.49*** (2.18) |
567 | |
| Gender | – | – | −0.164 (1.97) |
118 | |||
| Age | – | – | −1.06† (0.550) |
118 | |||
| Order | – | – | −3.66 (1.96) |
118 | |||
| Rate of Change | Time | 0.073† (0.039) |
570 | 0.324*** (0.087) |
567 | ||
| Gender | – | – | 0.045 (0.079) |
567 | |||
| Age | – | – | 0.039† (0.021) |
567 | |||
| Order | – | – | 0.253** (0.078) |
567 | |||
Significance levels:
p<0.10,
p<0.05,
p<0.01,
p<0.001
Relationships among different outcome variables
To examine any relationships in change across the different outcome measures, we calculated difference scores (last collection point – first collection point) for each outcome measure and looked at correlations between them. Interestingly, the JSE difference score was significantly correlated with all of the total QCAE score (r = 0.43, p < 0.001) and all of the cognitive empathy subscales (Cognitive: r = 0.48, p < 0.001; Perspective Taking: r = 0.33, p < 0.01; Online Simulation: r = 0.49, p < 0.001). All p values were adjusted for multiple comparisons. This suggests that while on aggregate, JSE decreases and QCAE increases, at the subject level there may be consistency in individual trajectories. Additionally, while performance on the pain and RMET were not significantly correlated with each other, both behavioral measures were correlated with JSE scores.
Discussion
Characterizing changes in student empathy throughout medical school is an important endeavor given the importance of this capacity in clinical practice. While medical schools are increasingly selecting doctors who they feel are effective and empathetic communicators with patients and other hospital staff, some studies indicate an erosion of the capacity. Our study only partly replicates these previous findings—specifically, JSE scores decreased over the course of training. However, empathy levels, measured with the QCAE, exhibited a strikingly different pattern, with cognitive and affective empathy improving, specifically perspective taking and emotion contagion, along with the overall cognitive scale, over the course of training. These findings highlight the importance of assessing both cognitive and affective aspects of empathy when examining the effects of medical training on students’ empathetic processes. Furthermore, it suggests that empathy changes in medical school may not be as straight forward as an overall decline. Indeed, while it may decrease in the context of the patient interaction, as assessed by the JSE, the consistent stable or improvement in empathy components on the QCAE indicates that the capacity for these processes is still strong and even improving during medical school.
Importantly, behavioral assessments of empathic processes also demonstrated an improvement over the course of medical training. Students exhibited progress in their ability to recognize other’s emotional states, in line with previous work(14), and greater sensitivity to facial expressions of pain. As cognitive empathy involves understanding and developing a working model of others emotional states(27), the ability to recognize subtle expressions of emotions is critical to developing this understanding. In the context of medicine, it is important that doctors are able to identify their patients’ emotional expressions, especially in regards to suffering, in order to understand and effectively respond to their needs and concerns.
Additionally, we found that overall female students exhibited higher levels of self-reported empathy. This is unsurprising and consistent with findings across studies of both medical students and general population(20,32). Interestingly, these differences appear to be stable over time, with gender having few significant effects on rate of change over time. Importantly, for most models, including the effects of gender and age (even if not significant) as predictors accounted for a significant amount of variability in the data above and beyond that accounted for by time suggesting these are important contributors to medical students’ empathy levels and should be considered when exploring patterns of change in empathy during medical school.
Altogether, our study demonstrates that medical school does not lead to an overall decline in students’ broad capacity for empathy, assessed with the QCAE and objective behavioral tasks, but instead indicates a more complex, and less dire, pattern, with some aspects of empathy actually strengthening over the course of training. Indeed, the only measure that demonstrated a decline (the JSE) relies on self-report limited to a one facet and context, cognitive empathy within the physician-patient relationship. These discrepant findings are in line with one study demonstrating small, albeit significant, correlations between JSE scores and more general measures of empathy (the IRI) (42). It is possible, that within the specific context of the physician-patient relationship, cognitive empathy does decline. However, the current work suggests the observed declines are not a loss of overall empathic capacity, which is more reliably assessed with the QCAE, but rather a lack of use within the patient physician interaction. Additionally, to our knowledge, neither the JSE nor QCAE have been assessed alongside doctors’ and students’ behavior within the physician patient interaction. Thus it is still unclear how the observed changes would translate into that interaction. Given the JSE has been previously demonstrated to have poor correlations with observed empathetic behavior (29), and the behavioral components of empathy measure in the context of this study significantly improve over the course of training, there is a need for further exploration into how observed changes in self-report measures directly relate to physician’s behavior when interacting with patients.
Notably, the facets of empathy for which we do observe improvement, especially perspective taking and understanding others’ emotions, are those argued to be most important to physician empathy(10), and most susceptible to change through teaching(43). Future interventions could focus on supporting and maintaining these skills, specifically in the context of patient-physician interaction. It is possible that the observed changes are a result of specific curriculum focuses on understanding the patient’s perspective and conveying that understanding to the patient. Indeed, many medical schools, including those studied in this work, have explicit empathy curriculums aimed at developing these skills. However, it is also possible that the nature of medical training facilitates improvement in these skills without explicit practice. More work needs to be done to illuminate the interrelationships among the complex socio-emotional components of empathy, and how they then, as stated previously, relate to practitioners’ actual behaviors within the physician-patient relationship, to determine what aspects might be most susceptible to intervention, and even if intervention is necessary.
While this study is unique in that it provides an in-depth, longitudinal assessment of several component processes of empathy, self-reported and behavioral, across a large number of students and multiple time points, it has some limitations. First, the sample size is small compared to recent work looking at changes over time in empathy during medical as assessed by the JSE as well as it’s factor validity(13)However, this sample size is comparable to much of the other longitudinal research on changes in empathy over the course of medical school(10,14), and is the first study, to the authors’ knowledge, to assess and compare empathy changes in medical students as assessed by the JSE, or empathy in context of the patient interaction, and a more general measure of students’ capacity for empathy, the QCAE, along with measures designed to assess the behavioral manifestation of this capacity. Additionally, there may be potential bias due to self-selection of participants, in that patterns of change might be different in students who did not volunteer for the study. However, this is a limitation inherent to all research done with human subjects, as it is unethical to compel an individuals’ participation. The study is also somewhat limited by the lack of behavioral measures of empathy within the physician patient interaction, which makes it difficult to assess how self-reported changes in empathy translate into the clinical interaction. Additionally, our study did not look at individual differences in respect to empathy changes. While the primary goal was to examine how different aspects of empathy change over medical school, there is a wealth of literature suggesting that individual differences in factors such as burnout(5), mental health(44), and lack of social support(3) may influence students’ susceptibility to empathy changes over the course of medical training. It could also be that the changes being observed are just a result of natural changes over the course of life. However, while some work, suggests life-course changes in empathy, the evidence is mixed(45,46). Additionally, many of these life-course studies use a measure of empathy neglecting its different subcomponents, and where significant changes are found, they are often declines. Lastly, while the QCAE has been used and demonstrated reliability across a variety of population, including those with comparable backgrounds to first year medical students (i.e. university undergraduate and graduate students) (32–35), it is possible the scales structure may differ in the medical student population and should be explored further in future research.
Overall, our study provides the first integration of multiple self-reports and objective measures of medical students’ empathic capacity, based on more resent theoretical and empirical research from behavioral neuroscience. The findings demonstrate that changes in empathy during medical training are not necessarily negative. It appears to be much more complex than initially thought, and shows how problematic it is to rely on a single subjective measure to assess a complex psychological construct. Empathy is not one single psychological process, but an integration of different facets. Importantly, clinical empathy, to be effective for both the patient and his/her doctor, should not be reduced to its cognitive facet (perspective-taking), but needs to encompass emotional engagement and attunement(26). All facets of empathy (affective, cognitive, and motivational) are important and have to be adaptively engaged to positively influence patients’ health(1).
There is a need for more research examining the different subcomponents of this complex socio-emotional process and their behavioral manifestations, followed by an examination of what factors may influence individual differences in these changes. Future work should focus on outlining the nature of these changes, how they translate into a clinical interview setting, which individuals are most susceptible to these changes, and the neurobehavioral mechanisms that contribute to that susceptibility. Ultimately, this new empirically-based knowledge will be used to inform potential interventions aimed educating medical students to engage in clinical empathy by enhancing both the effectiveness of their care for patients and their own career fulfillment (26).
Supplementary Material
Acknowledgments
None
Financial Support: This work was supported by a grant from the John Templeton Foundation (The Science of Philanthropy Initiative and Wisdom Research at the University of Chicago) and from National Institutes of Health (R01MH087525; R01MH084934) to J. Decety.
Footnotes
Other disclosures: No competing interests to disclose
Ethical approval: This study was approved by the University of Chicago’s Institutional Review Board (Ref. # IRB12-1561, Most Recent Continuing Review Approval Date: 3/19/2015) and conducted in accordance with the Declaration of Helsinki.
Contributor Information
Ms. Karen E. Smith, Department of Psychology, Integrative Neuroscience Area, University of Chicago, 5848 S University Ave, Chicago, IL, 60637.
Dr. Greg J. Norman, Department of Psychology, University of Chicago, 5848 S University Ave, Chicago, IL, 60637 and Grossman Institute for Neuroscience, University of Chicago, 5812 S Ellis Ave, Chicago, IL, 60637.
Dr. Jean Decety, Department of Psychology, University of Chicago, 5848 S University Ave, Chicago, IL, 60637, Grossman Institute for Neuroscience, University of Chicago, 5812 S Ellis Ave, Chicago, IL, 60637, and Department of Psychiatry and Behavioral Neuroscience, University of Chicago, 5848 S University Ave, Chicago, IL, 60637.
References
- 1.Decety J, Fotopoulou A. Why empathy has a beneficial impact on others in medicine: unifying theories. Front Behav Neurosci. 2015;8(January):457. doi: 10.3389/fnbeh.2014.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halpern J. What is clinical empathy? J Gen Intern Med. 2003 Aug;18(8):670–4. doi: 10.1046/j.1525-1497.2003.21017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009. doi: 10.1097/ACM.0b013e318221e615. [DOI] [PubMed] [Google Scholar]
- 4.Dyrbye LN, Power DV, Massie FS, Eacker A, Harper W, Thomas MR, et al. Factors associated with resilience to and recovery from burnout: A prospective, multi-institutional study of US medical students. Med Educ. 2010 Oct;44(10):1016–26. doi: 10.1111/j.1365-2923.2010.03754.x. [DOI] [PubMed] [Google Scholar]
- 5.Brazeau CMLR, Schroeder R, Rovi S, Boyd L. Relationships Between Medical Student Burnout, Empathy, and Professionalism Climate. Acad Med. 2010;85(10):S33–6. doi: 10.1097/ACM.0b013e3181ed4c47. [DOI] [PubMed] [Google Scholar]
- 6.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011 Mar;86(3):359–64. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 7.Rakel DP, Hoeft TJ, Barrett BP, Chewning BA, Craig BM, Niu M. Practitioner empathy and the duration of the common cold. Fam Med. 2009;41(7):494–501. [PMC free article] [PubMed] [Google Scholar]
- 8.Haque OS, Waytz A. Dehumanization in medicine: Causes, solutions, and functions. Perspect Psychol Sci. 2012 Mar 9;7(2):176–86. doi: 10.1177/1745691611429706. [DOI] [PubMed] [Google Scholar]
- 9.Riess H. Empathy in medicine — A neurobiological perspective. JAMA. 2010;304(14):1604–5. doi: 10.1001/jama.2010.1455. [DOI] [PubMed] [Google Scholar]
- 10.Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–91. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. Clarifying changes in student empathy throughout medical school: a scoping review. Adv Heal Sci Educ. 2016:1–21. doi: 10.1007/s10459-016-9704-7. [DOI] [PubMed] [Google Scholar]
- 12.Costa P, Magalhães E, Costa MJ. A latent growth model suggests that empathy of medical students does not decline over time. Adv Heal Sci Educ. 2013;18(3):509–22. doi: 10.1007/s10459-012-9390-z. [DOI] [PubMed] [Google Scholar]
- 13.Stansfield RB, Schwartz A, O’Brien CL, Dekhtyar M, Dunham L, Quirk M. Adv Heal Sci Educ. Springer; Netherlands: 2015. Development of a metacognitive effort construct of empathy during clinical training: a longitudinal study of the factor structure of the Jefferson Scale of Empathy; pp. 5–17. [DOI] [PubMed] [Google Scholar]
- 14.Handford C, Lemon J, Grimm MC, Vollmer-conna U. Empathy as a Function of Clinical Exposure - Reading Emotion in the Eyes. PLoS One. 2013;8(6):1–7. doi: 10.1371/journal.pone.0065159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Decety J. Curr Opin Behav Sci. Vol. 3. Elsevier Ltd; 2015. The neural pathways, development and functions of empathy; pp. 1–6. [Google Scholar]
- 16.Singer T, Lamm C. The Social Neuroscience of Empathy. Ann NY Acad Sci. 2009;1156:81–96. doi: 10.1111/j.1749-6632.2009.04418.x. [DOI] [PubMed] [Google Scholar]
- 17.Shamay-Tsoory S. Empathic processing: Its cognitive and affective dimensions and neuroanatomical basis. In: Decety J, Ickes W, editors. The Social Neuroscience of Empathy. Cambridge: MIT Press; 2009. pp. 215–32. [Google Scholar]
- 18.Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev. 2004 Jun;3(2):71–100. doi: 10.1177/1534582304267187. [DOI] [PubMed] [Google Scholar]
- 19.Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002 Oct;52(Suppl):S9–12. [PMC free article] [PubMed] [Google Scholar]
- 20.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: Definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159(9):1563–9. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 21.Cheng Y, Lin C-P, Liu H-L, Hsu Y-Y, Lim K-E, Hung D, et al. Expertise modulates the perception of pain in others. Curr Biol. 2007 Oct 9;17(19):1708–13. doi: 10.1016/j.cub.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 22.Decety J, Yang C-Y, Cheng Y. Neuroimage [Internet] 4. Vol. 50. Elsevier Inc; 2010. May 1, Physicians down-regulate their pain empathy response: an event-related brain potential study; pp. 1676–82. [cited 2013 Mar 1]; Available from: http://www.ncbi.nlm.nih.gov/pubmed/20080194. [DOI] [PubMed] [Google Scholar]
- 23.Decety J, Ben-Ami Bartal I, Uzefovsky F, Knafo-Noam A. Empathy as a driver of prosocial behaviour: Highly conserved neurobehavioural mechanisms across species. Philos Trans R Soc B Biol Sci. 2016;371(1686):20150077. doi: 10.1098/rstb.2015.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Decety J, Meidenbauer KL, Cowell JM. The development of cognitive empathy and concern in preschool children: A behavioral neuroscience investigation. Dev Sci. 2017 Mar;:1–12. doi: 10.1111/desc.12570. [DOI] [PubMed] [Google Scholar]
- 25.Shdo SM, Ranasinghe KG, Gola KA, Mielke CJ, Sukhanov PV, Miller BL, et al. Deconstructing empathy: Neuroanatomical dissociations between affect sharing and prosocial motivation using a patient lesion model. Neuropsychologia. 2016 Sep;:1–10. doi: 10.1016/j.neuropsychologia.2017.02.010. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Halpern J. Clinical empathy in medical care. In: Decety J, editor. Empathy: From bench to bedside. Cambridge, MA: MIT Press; 2012. pp. 229–44. [Google Scholar]
- 27.Decety J, Smith KE, Norman GJ, Halpern J. A social neuroscience perspective on clinical empathy. World Psychiatry. 2014;13(3):233–7. doi: 10.1002/wps.20146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hojat M, LaNoue M. Exploration and confirmation of the latent variable structure of the Jefferson scale of empathy. Int J Med Educ. 2014;5:73–81. doi: 10.5116/ijme.533f.0c41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen DCR, Pahilan ME, Orlander JD. Comparing a self-administered measure of empathy with observed behavior among medical students. J Gen Intern Med. 2010;25(3):200–2. doi: 10.1007/s11606-009-1193-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Decety J, Norman GJ, Berntson GG, Cacioppo JT. Prog Neurobiol. 1. Vol. 98. Elsevier Ltd; 2012. Jul, A neurobehavioral evolutionary perspective on the mechanisms underlying empathy; pp. 38–48. [DOI] [PubMed] [Google Scholar]
- 31.Eres R, Decety J, Louis WR, Molenberghs P. Individual differences in local gray matter density are associated with differences in affective and cognitive empathy. Neuroimage. 2015;117:305–10. doi: 10.1016/j.neuroimage.2015.05.038. [DOI] [PubMed] [Google Scholar]
- 32.Reniers RL, Corcoran R, Drake R, Shryane NM, Völlm Ba. The QCAE: a Questionnaire of Cognitive and Affective Empathy. J Pers Assess. 2011;93(1):84–95. doi: 10.1080/00223891.2010.528484. [DOI] [PubMed] [Google Scholar]
- 33.Yoder KJ, Decety J. The Good, the Bad, and the Just: Justice Sensitivity Predicts Neural Response during Moral Evaluation of Actions Performed by Others. J Neurosci. 2014;34(12):4161–6. doi: 10.1523/JNEUROSCI.4648-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lockwood PL, Seara-Cardoso A, Viding E. Emotion regulation moderates the association between empathy and prosocial behavior. PLoS One. 2014;9(5) doi: 10.1371/journal.pone.0096555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Michaels TM, Horan WP, Ginger EJ, Martinovich Z, Pinkham AE, Smith MJ. Psychiatry Res. 3. Vol. 220. Elsevier; 2014. Cognitive empathy contributes to poor social functioning in schizophrenia: Evidence from a new self-report measure of cognitive and affective empathy; pp. 803–10. [PubMed] [Google Scholar]
- 36.Decety J, Echols S, Correll J. The blame game: the effect of responsibility and social stigma on empathy for pain. J Cogn Neurosci. 2009;22(5):985–97. doi: 10.1162/jocn.2009.21266. [DOI] [PubMed] [Google Scholar]
- 37.Baron-Cohen S, Wheelwright S, Hill J, Raste Y, Plumb I. The “Reading the Mind in the Eyes” Test revised version: a study with normal adults, and adults with Asperger syndrome or high-functioning autism. J Child Psychol Psychiatry. 2001;42(2):241–51. [PubMed] [Google Scholar]
- 38.Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, et al. The Jefferson Scale of Physician Empathy: Development and Preliminary Psychometric Data. Educ Psychol Meas. 2001;61(2):349–65. [Google Scholar]
- 39.Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press; 2003. [Google Scholar]
- 40.Raudenbush SW, Bryk AS. Volume. Sage Publications; 2002. Hierarchical linear models: Applications and data analysis methods; p. 1. [Google Scholar]
- 41.Schieman S, Van Gundy K. The personal and social links between age and self-reported empathy. Soc Psychol Q. 2000;63(2):152–74. [Google Scholar]
- 42.Costa P, de Carvalho-Filho MA, Schweller M, Thiemann P, Salgueira A, Benson J, et al. Measuring medical students’ empathy skills: Exploring the underlying constructs of and associations between two widely used self-report instruments in five countries. Acad Med. 2017 doi: 10.1097/ACM.0000000000001449. [DOI] [PubMed] [Google Scholar]
- 43.Batt-Rawden Sa, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013 Aug;88(8):1171–7. doi: 10.1097/ACM.0b013e318299f3e3. [DOI] [PubMed] [Google Scholar]
- 44.Dunn LB, Iglewicz A, Moutier C. A conceptual model of medical student well-being: Promoting resilience and preventing burnout. Acad Psychiatry. 2008;32:44–53. doi: 10.1176/appi.ap.32.1.44. [DOI] [PubMed] [Google Scholar]
- 45.Helson R, Kwan VSY, John OP, Jones C. The growing evidence for personality change in adulthood: Findings from research with personality inventories. J Res Pers. 2002;36(4):287–306. [Google Scholar]
- 46.O’Brien E, Konrath SH, Grühn D, Hagen AL. Empathic concern and perspective taking: Linear and quadratic effects of age across the adult life span. Journals Gerontol - Ser B Psychol Sci Soc Sci. 2013;68(2):168–75. doi: 10.1093/geronb/gbs055. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


