Abstract
Oral anticoagulation (OAC) is effective, yet reportedly underutilized for stroke prevention in atrial fibrillation (AF). Factors associated with delayed OAC after incident AF are unknown. Using a large electronic medical record, we identified incident AF diagnosed 2006–2014 using a validated algorithm. Among patients with CHADS2 score ≥1 started on OAC within 1 year, we examined baseline characteristics at AF diagnosis and their association with time to OAC using multivariable Cox proportional hazards modeling. Of 4,388 patients with incident AF and CHADS2 score ≥1 started on OAC within 1 year, the mean age was 72.6 and 41% were women. Median time to OAC was 5 days (interquartile range 1–43) and most patients received warfarin (86.3%). Among patients without prevalent stroke, 98 strokes (2.2% of the sample) occurred between AF diagnosis and OAC initiation. In multivariable analyses, several factors were associated with delayed OAC including female sex (HR 1.08, 95% CI 1.01–1.15), absence of hypertension (HR 1.15, 95% CI 1.03–1.27), previous fall (HR 1.53, 95% CI 1.08–2.17), and chronic kidney disease (HR 1.12, 95% CI 1.04–1.21). Among women, OAC prescription at 1, 3 and 6 months was 70.0%, 81.7%, and 89.5%, respectively, whereas for males OAC prescription was 73.4%, 84.0%, and 91.5%. Most patients with new AF and elevated stroke risk started on OAC receive it within 1 week, although the promptness of initiation varies. The stroke rate is substantial in the period between AF diagnosis and OAC initiation. Interventions targeting identified risk factors for delayed OAC may result in improved outcomes.
Keywords: atrial fibrillation, anticoagulation, stroke, electronic medical record
Atrial fibrillation (AF) is a prevalent arrhythmia associated with significant stroke risk.1–3 Oral anticoagulation (OAC) with either warfarin (a vitamin K antagonist) or a novel oral anticoagulant (NOAC) is effective in reducing the risk of stroke associated with AF.4 As a result, consensus guidelines recommend treatment with either warfarin or NOAC in patients with moderate to high stroke risk, a population that includes the majority of AF patients.5,6 Despite this recommendation, evidence repeatedly demonstrates that up to 50% of patients with an indication for OAC do not receive it.7,8 Although previous studies have exposed clinical factors associated with a lower incidence of OAC such as female sex and older age,8 to date studies have not focused on factors relating to a potential delay in initiation of OAC therapy after a new diagnosis of AF. Indeed, consideration of factors related to delayed OAC initiation may expose patient, provider, or other systemic characteristics that could be targeted to reduce the total time AF patients are exposed to elevated stroke risk through lack of thromboembolism prophylaxis. In this study, we leveraged a large hospital-based electronic medical record (EMR) to identify cases of incident AF. We then sought to identify clinical factors associated with delayed OAC among the AF patients at elevated stroke risk who ultimately received anticoagulation.
METHODS
The Partners HealthCare EMR utilized in this study has been described previously.9 Briefly, the Partners HealthCare EMR is a large medical record utilized by 7 Massachusetts hospitals. Using the Research Patient Database Query Tool, a large database of detailed Partners HealthCare EMR data, we applied a validated electronic AF ascertainment algorithm9 to identify unique cases of AF. Briefly, the AF algorithm utilizes diagnostic, procedure, electrocardiographic, and medication data to ascertain the presence of atrial flutter or fibrillation.
To identify potential patients with AF, we first identified all individuals with at least 1 International Statistical Classification of Diseases, 9th revision (ICD-9) code for AF at Massachusetts General Hospital between 2006–2014 (n=46,151). To ensure that we captured only new AF diagnoses, we limited the sample to patients who had an independent encounter within 3–24 months prior to AF diagnosis in which they did not meet algorithm criteria for AF. To ensure reliable follow-up during which we could ascertain the presence of OAC, we required that patients also have separate contact 3–24 months after AF diagnosis. We chose 2006 as the start date as this was the first year the American College of Cardiology/American Heart Association AF management guidelines recommended the use of the CHADS2 (Congestive heart failure, Hypertension, Age, Diabetes, and Stroke) prediction tool for stroke risk stratification in AF.10 Since we were interested in patients with new AF at elevated stroke risk with an indication for OAC, we excluded patients with a CHADS2 score of zero. We also excluded patients exposed to OAC prior to AF diagnosis as well as patients not started on OAC within 1 year of AF diagnosis given our intent to identify factors associated with de novo OAC initiation. Since we hypothesized that algorithm performance may be affected by removal of patients with previous OAC exposure, we performed manual adjudication of AF in a subset of 100 records in which algorithm PPV was found to be 97%.9 Manual adjudication of AF date in an independent subset of 100 records demonstrated median discrepancy of 0 days (interquartile range 0–18.3). In total, we included 4,388 individuals with new AF in the analysis (Figure 1).
Figure 1.
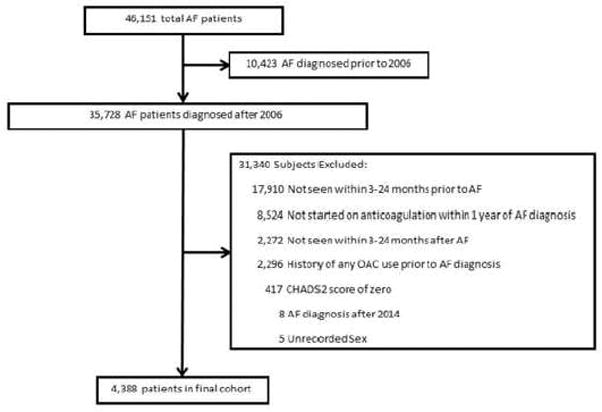
Study Design
Graphic depiction of study design. AF – atrial fibrillation, OAC – oral anticoagulant
For each patient with AF, we extracted clinical characteristics present at AF diagnosis. Demographic information including age, sex, and race were extracted directly from the EMR. Encounter-level factors including insurance provider and clinic location were obtained from billing data coded at the index AF encounter. Comorbidities prevalent at AF diagnosis were defined using the presence of at least 1 ICD-9 code for a given condition at any time prior to the index AF encounter in a manner similar to that used in previous studies.8,11 Baseline medication use was defined as the presence of a medication prescription within 30 days prior to AF diagnosis. Reversible AF was defined as the concomitant presence of AF with an ICD-9 code diagnosis corresponding to cardiac surgery or thyroid disease. To enable consideration of the total number of medications a patient is prescribed, we tabulated the number of medications prescribed to each individual within 90 days of the AF diagnosis and termed this the Medication Burden Index (MBI). For each patient, we then determined whether they were above (high MBI) or below (low MBI) the median of the MBI distribution, and utilized this binary value for subsequent analyses.
For each AF patient, we calculated time to OAC as the number of days between the date of AF diagnosis and the first appearance of OAC (warfarin or NOAC) in the medical record. To determine independent clinical factors associated with increased time to OAC following AF diagnosis, we performed multivariable Cox proportional hazards regression with time to OAC as the outcome of interest. Variables included in the multivariable models included year of AF diagnosis, age, sex, race, hypertension, heart failure, diabetes, previous stroke or transient ischemic attack (TIA), vascular disease, reversible AF, dementia, previous fall, previous bleed or thrombocytopenia, aspirin use, P2Y12 inhibitor use, dual antiplatelet therapy use (aspirin and P2Y12 inhibitor), malignancy, liver disease, pulmonary disease, rheumatic disease, weakness/paralysis, chronic kidney disease, insurance carrier, MBI, and provider specialty (medicine, non-medicine, emergency, or cardiology) at AF diagnosis. To account for the varying baseline propensity to receive OAC that may be confounded by frequent healthcare encounters, we tabulated the total number of billed encounters prior to AF diagnosis and divided the distribution into quartiles, and then stratified the Cox models by quartiles. To account for varying baseline propensity to receive OAC that may be confounded by the setting of AF diagnosis (inpatient vs. outpatient), we also stratified the Cox models by setting. In secondary analyses, we then fit multiple linear regression models with time to OAC in days as the outcome of interest (one model for inpatients and the second for outpatients) to quantify the magnitude of OAC delay associated with specific clinical factors. The same variables included in the proportional hazards models were included in the multiple linear regression models, and those used for stratification in the proportional hazards models were included as covariates in the linear models. In a separate sex-adjusted multivariable proportional hazards model, we assessed the association between CHADS2 score ≥ 2 and time to OAC.
In addition to estimating factors associated with delayed OAC within 1 year of AF diagnosis, we also constructed multivariable-adjusted cumulative incidence curves depicting estimated OAC incidence across selected strata demonstrating significant association with delay in OAC. For each adjusted cumulative incidence estimation, the mean value (for continuous variables) or the most prevalent value (for categorical variables) was modeled for each covariate.
We then estimated the incidence of ischemic stroke in the overall sample during the period in which patients were not treated with OAC by calculating the number of events prior to OAC in patients with no history of stroke at the time of AF diagnosis. We tested the association between CHADS2 score and incident stroke in sex-adjusted proportional hazards models.
We considered associations between predictor variables and time to OAC to be significant if the two-sided p-value was < 0.05. All analyses were performed using R v.3.2.2.12
RESULTS
Of 4,338 patients with incident AF included in the analysis (Figure 1), the mean age was 72.6 ± 11.5 years and 41.2% were women. AF was diagnosed in the inpatient setting in 46.4% of patients. The median CHADS2 score was 2 (interquartile range 2–3). Low molecular weight heparin (LMWH) was utilized prior to OAC in 12 (0.55%) AF outpatients. Other characteristics are listed in Table 1.
Table 1.
Study sample characteristics
| Baseline characteristic (N=4388) | Count |
|---|---|
| Woman | 1808 (41.2%) |
| Age (years)* | 72.6 ± 11.5 |
| Year of AF diagnosis† | 2011 (2008, 2013) |
| White race | 3982 (90.7%) |
| Non-private insurance | 3347 (76.3%) |
| Heart failure | 1984 (45.2%) |
| Hypertension | 3917 (89.3%) |
| Diabetes mellitus | 1439 (32.8%) |
| Previous stroke/Transient ischemic attack | 926 (21.1%) |
| Vascular disease | 3001 (68.4%) |
| CHADS2 Score | - |
| 1 | 1015 (23.1%) |
| 2 | 1349 (30.7%) |
| 3 | 1036 (23.6%) |
| 4 | 581 (13.2%) |
| 5 | 300 (6.8%) |
| 6 | 107 (2.4%) |
| Reversible AF | 397 (9.0%) |
| Dementia | 54 (1.2%) |
| Previous fall | 33 (0.75%) |
| Previous bleed or thrombocytopenia | 2392 (54.5%) |
| Aspirin use | 515 (11.7%) |
| P2Y12 inhibitor use | 84 (1.9%) |
| Dual antiplatelet use | 34 (0.77%) |
| Malignancy | 1304 (29.7%) |
| Liver disease | 608 (13.9%) |
| Pulmonary disease | 1576 (35.9%) |
| Rheumatic disease | 295 (6.7%) |
| Weakness/paralysis | 195 (4.4%) |
| Chronic Kidney Disease | 1116 (25.4%) |
| High Medication Burden Index | 2325 (53.0%) |
| Cardiology provider at AF diagnosis | 289 (6.6%) |
| Medical provider at AF diagnosis | 2529 (57.6%) |
| Emergency provider at AF diagnosis | 62 (1.4%) |
| Non-medical provider at AF diagnosis | 686 (15.6%) |
| Uncoded provider at AF diagnosis | 822 (18.7%) |
Presented as mean ± standard deviation
Presented as median (quartile 1, quartile 3)
The median time to OAC in the overall cohort was 5 days (interquartile range 1–43). During the study period from 2006 to 2014, most anticoagulated patients were treated with warfarin (86.3%). However, by 2014, 39.7% of patients were treated with a NOAC. Among patients without prevalent stroke at AF diagnosis, 272 strokes occurred during the study period and 98 strokes (2.2% of the sample) occurred prior to OAC. CHADS2 score was significantly associated with incident stroke in a sex-adjusted model (HR 1.17, 95% CI 1.03–1.33).
In multivariable analyses, factors associated with delayed OAC included female sex (HR 1.08, 95% CI 1.01–1.15), white race (HR 1.14, 95% CI 1.03–1.26), previous fall (HR 1.53, 95% CI 1.08–2.17), pulmonary disease (HR 1.09, 95% CI 1.02–1.17), malignancy (HR 1.08, 95% CI 1.01–1.16), and chronic kidney disease (HR 1.12, 95% CI 1.04–1.21). Factors associated with faster OAC included hypertension (HR 0.87, 95% CI 0.79–0.96) and reversible AF (HR 0.82, 95% CI 0.73–0.91). Associations among clinical factors and time to OAC are depicted in Figure 2. Multivariable-adjusted associations between variables and length of OAC delay determined using linear regression, stratified by AF diagnosed in the inpatient and outpatient settings, are displayed in Supplementary Tables 1 and 2, respectively.
Figure 2.
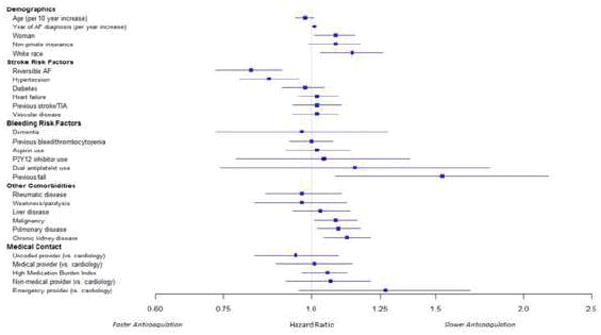
Factors associated with delay to oral anticoagulation initiation in a multivariable-adjusted model.
Forest plot depicting multivariable hazard ratios for greater delay to oral anticoagulation.
In a separate sex-adjusted model, a CHADS2 score < 2 was also associated with delayed OAC (HR 1.10, 95% CI 1.03–1.18, p < 0.01). Following multivariable modeling, we then plotted the multivariable-adjusted cumulative incidence of OAC in strata of select risk factors that were significantly associated with delayed OAC (Figure 3).
Figure 3.

Cumulative incidence of oral anticoagulation in select subgroups.
Among individuals treated with anticoagulation within 1 year of AF diagnosis, we plotted multivariable-adjusted cumulative incidence curves depicting the proportion of individuals treated with anticoagulation over time in select clinically relevant strata: a) chronic kidney disease, b) falls, c) hypertension, and d) gender. The full list of variables used in the models is displayed in Table 1.
DISCUSSION
In our sample of nearly 5,000 patients with a new diagnosis of AF and elevated stroke risk at a large academic medical center who were ultimately treated with OAC, we identified multiple clinical characteristics that were associated with a delay in initiation of OAC. Half of patients were treated with OAC within 5 days of AF diagnosis, in keeping with consensus guidelines. Importantly, women were treated with OAC following a significantly greater delay than men, despite the fact that women traditionally have a greater risk for stroke in AF.13 As expected, a variety of comorbidities were also associated with a greater delay to OAC.
Previous literature has focused on predictors of OAC in patients with AF and elevated stroke risk. In contrast, our analysis is focused on the factors related to delay in initiation of OAC among patients with AF and moderate to high stroke risk who were treated with OAC. Encouragingly, our findings demonstrate that the majority of patients with new AF receiving OAC receive it promptly and in accordance with existing guidelines.10 However, a substantial number of patients receiving OAC experience delays, with 25% of individuals not receiving OAC until after 43 days and 10% not receiving OAC until after 6–12 months following AF diagnosis. The importance of more timely initiation of OAC is underscored by our observation that 98 incident strokes occurred prior to receipt of OAC. In aggregate, our data suggest that the impact of potential interventions designed to decrease time to OAC may be maximally effective if targeted toward identified subsets at the highest risk for OAC delays.
We found female sex to be a strong predictor of increased time to OAC after AF diagnosis. The emergence of sex as an important factor in OAC use is consistent with multiple previous studies demonstrating that OAC tends to be underutilized in women with AF.8,14 Our study extends prior observations by indicating that women also are started on OAC later than their male counterparts, with 73% of men being on OAC at 1 month versus only 70% of women. Although the reason for this disparity is not entirely clear, this gender gap may be an important target for improving care quality since women with AF are at greater stroke risk compared to their male counterparts.13
A history of falls also emerged as a strong predictor of increased time to OAC and was independently associated with a 53-day mean delay in OAC initiation among AF inpatients (see Table S2). Although falls are a commonly cited reason for deferring OAC therapy in AF, the risk of intracranial bleeding associated with falls even on OAC tends to be overestimated. According to an analysis by Man-Son-Hing et al., an average elderly patient would have to fall 295 times before the benefits of OAC therapy are outweighed by the risk, although certainly risk is likely to vary on an individual basis.15 Since our analysis does not include data regarding physician or patient preference, it is possible that patients with a history of falls are more likely to decline OAC due to fear of bleeding risk despite physician recommendations. In either case, our results highlight the longstanding and well-recognized clinical dilemma encountered by providers considering the initiation of thromboembolism prophylaxis in AF patients with a history of falls. Future studies focused on improving bleeding risk stratification in patients at risk for falls may allow for more informed decision-making between providers and patients and subsequently lead to decreased OAC delays among patients for whom OAC therapy is indicated.
Medical co-morbidities are an important determinant of OAC delay. Specifically, the presence of chronic kidney disease, malignancy, and pulmonary disease were all associated with greater delay to OAC initiation. Patients with chronic kidney disease may receive OAC later due to concerns regarding bleeding. Similarly, delayed OAC in patients with malignancy may be related to uncertainty regarding the optimal anticoagulation strategy, with options also including LMWH.16 Conversely, hypertensive patients received OAC more rapidly, suggesting that providers may be aware of the increased stroke risk associated with this condition and are apt to treat such patients more promptly with OAC. Given the limited use of NOAC therapy in our AF cohort, we were unable to specifically assess whether the presence of medical co-morbidities result in similar effects on OAC therapy among patients anticoagulated with warfarin versus a NOAC.
Our study should be interpreted in the context of the study design. First, we relied on OAC prescriptions in the EMR to define the initiation of OAC therapy, limiting our ability to make conclusions regarding therapy adherence, duration, or adequacy of warfarin or NOAC dosing. Second, our study was not designed to investigate stroke outcomes. Nevertheless, previous studies have repeatedly demonstrated that stroke risk is substantial in patients with AF and that even modest periods of time without OAC can increase stroke rates.17 Third, due to limitations within the EMR data we are unable to report the frequency of bridging therapy with heparin or LMWH among AF inpatients, although its use prior to OAC among AF outpatients was <1%. Fourth, since this is a single-center retrospective study we cannot eliminate the possibility of residual confounding or limited generalizability to other settings. Fifth, we utilized the CHADS2 score rather than the newer CHA2DS2-VASc score since the majority of patients in our study were diagnosed with AF before the CHA2DS2-VASc score was incorporated into the consensus guidelines in 2014.5 Sixth, misclassification of risk factors or accumulation of additional risk factors between AF diagnosis and OAC initiation may have influenced observed rates of OAC.
In summary, among a large group of contemporary patients with newly diagnosed AF started on OAC within 1 year, the median time to OAC was < 1 week. Female sex, absence of hypertension, absence of reversible AF, previous fall, pulmonary disease, malignancy, and chronic kidney disease were all associated with delay in the initiation of OAC.
Supplementary Material
Acknowledgments
Funding Sources
Dr. Lubitz is supported by NIH grant K23HL114724 and Doris Duke Charitable Foundation Clinical Scientist Development Awards 2014105 and 2016077. This work was also supported by grants from the National Institutes of Health to Dr. Ellinor (1RO1HL092577, R01HL128914, K24HL105780). Dr. Ellinor is also supported by an Established Investigator Award from the American Heart Association (13EIA14220013) and by the Fondation Leducq (14CVD01).
Footnotes
Disclosures
Dr. Ellinor is the PI on a grant from Bayer HealthCare to the Broad Institute focused on the genetics and therapeutics of atrial fibrillation. Dr. Lubitz receives sponsored research support from Bayer HealthCare, Biotronik, and Boehringer Ingelheim, and has consulted for St. Jude Medical and Quest Diagnostics. All authors have approved the final article for publication.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Corley SD, Epstein AE, DiMarco JP, Domanski MJ, Geller N, Greene HL, Josephson RA, Kellen JC, Klein RC, Krahn AD, Mickel M, Mitchell LB, Nelson JD, Rosenberg Y, Schron E, Shemanski L, Waldo AL, Wyse DG Investigators A. Relationships between sinus rhythm, treatment, and survival in the atrial fibrillation follow-up investigation of rhythm management (AFFIRM) study. Circulation. 2004;109:1509–1513. doi: 10.1161/01.CIR.0000121736.16643.11. [DOI] [PubMed] [Google Scholar]
- 2.Stewart S, Hart CL, Hole DJ, McMurray JJV. A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Am J Med. 2002;113:359–364. doi: 10.1016/s0002-9343(02)01236-6. [DOI] [PubMed] [Google Scholar]
- 3.Wolf PA, Abbott RD, Kannel WB. Atrial-fibrillation - A major contributor to stroke in the elderly - The Framingham Study. Arch Intern Med. 1987;147:1561–1564. [PubMed] [Google Scholar]
- 4.Adam SS, McDuffie JR, Ortel TL, Williams JW. Comparative Effectiveness of Warfarin and New Oral Anticoagulants for the Management of Atrial Fibrillation and Venous Thromboembolism: A Systematic Review. Ann Intern Med. 2012;157:796–807. doi: 10.7326/0003-4819-157-10-201211200-00532. [DOI] [PubMed] [Google Scholar]
- 5.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW, Anderson JL, Halperin JL, Albert NM, Bozkurt B, Brindis RG, Creager MA, Curtis LH, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Ohman EM, Pressler SJ, Sellke FW, Shen WK. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation. J Am Coll Cardiol. 2014;64:E1–E76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 6.Olesen JB, Torp-Pedersen C, Hansen ML, Lip GYH. The value of the CHA(2)DS(2)-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS(2) score 0–1: A nationwide cohort study. Thromb Haemost. 2012;107:1172–1179. doi: 10.1160/TH12-03-0175. [DOI] [PubMed] [Google Scholar]
- 7.Waldo AL, Becker RC, Tapson VF, Colgan KJ, Comm NS. Hospitalized patients with atrial fibrillation and a high risk of stroke are not being provided with adequate anticoagulation. J Am Coll Cardiol. 2005;46:1729–1736. doi: 10.1016/j.jacc.2005.06.077. [DOI] [PubMed] [Google Scholar]
- 8.Wilke T, Groth A, Mueller S, Pfannkuche M, Verheyen F, Linder R, Maywald U, Kohlmann T, Feng YS, Breithardt G, Bauersachs R. Oral anticoagulation use by patients with atrial fibrillation in Germany Adherence to guidelines, causes of anticoagulation under-use and its clinical outcomes, based on claims-data of 183,448 patients. Thromb Haemost. 2012;107:1053–1065. doi: 10.1160/TH11-11-0768. [DOI] [PubMed] [Google Scholar]
- 9.Khurshid S, Keaney J, Ellinor PT, Lubitz SA. A Simple and Portable Algorithm for Identifying Atrial Fibrillation in the Electronic Medical Record. Am J Cardiol. 2016;117:221–225. doi: 10.1016/j.amjcard.2015.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fuster V, Ryden LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S. ACC/AHA/ESC 2006 Guidelines for the Management of Patients With Atrial Fibrillation A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation) Developed in Collaboration With the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006;114:E257–E354. doi: 10.1161/CIRCULATIONAHA.106.177292. [DOI] [PubMed] [Google Scholar]
- 11.Friberg L, Rosenqvist M, Lip GYH. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33:1500–1510. doi: 10.1093/eurheartj/ehr488. [DOI] [PubMed] [Google Scholar]
- 12.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2015. URL https://www.R-project.org/ [Google Scholar]
- 13.Lip GYH, Nieuwlaat R, Pisters R, Lane DA, Crijns H. Refining Clinical Risk Stratification for Predicting Stroke and Thromboembolism in Atrial Fibrillation Using a Novel Risk Factor-Based Approach The Euro Heart Survey on Atrial Fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 14.Hsu JC, Maddox TM, Kennedy K, Katz DF, Marzec LN, Lubitz SA, Gehi AK, Turakhia MP, Marcus GM. Aspirin Instead of Oral Anticoagulant Prescription in Atrial Fibrillation Patients at Risk for Stroke. J Am Coll Cardiol. 2016;67:2913–2923. doi: 10.1016/j.jacc.2016.03.581. [DOI] [PubMed] [Google Scholar]
- 15.Man-Son-Hing M, Nichol G, Lau A, Laupacis A. Choosing antithrombotic therapy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern Med. 1999;159:677–685. doi: 10.1001/archinte.159.7.677. [DOI] [PubMed] [Google Scholar]
- 16.Lee AYY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, Rickles FR, Julian JA, Haley S, Kovacs MJ, Gent M, Clot Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. New Engl J Med. 2003;349:146–153. doi: 10.1056/NEJMoa025313. [DOI] [PubMed] [Google Scholar]
- 17.Kaatz S, Douketis JD, Zhou H, Gage BF, White RH. Risk of stroke after surgery in patients with and without chronic atrial fibrillation. Thromb Haemost. 2010;8:884–890. doi: 10.1111/j.1538-7836.2010.03781.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


