Abstract
Objective
The current analysis examines whether opioid use is associated with insomnia in a community sample, as the consequences of the growing epidemic of prescription opioid use continue to cause public health concern.
Study Design
A cross-sectional study including 8,433 members in a community outreach program, HealthStreet, in Northeast Florida.
Methods
Community Health Workers (CHWs) assessed health information, including use of opioids (i.e., Vicodin®, Oxycodone, Codeine, Demerol®, Morphine, Percocet®, Darvon®, Hydrocodone) from community members during field outreach. Insomnia was determined based on self-report: "Have you ever been told you had, or have you ever had a problem with insomnia?" Summary descriptive statistics were calculated and logistic regression modelling was used to calculate adjusted odds ratios (ORs) with 95% confidence intervals for insomnia, by opioid use status, after adjustment for demographics and other covariates.
Results
Among 8,433 community members recruited (41% male; 61% black), 2,115 (25%) reported insomnia, and 4,200 (50.3%) reported use of opioids. After adjusting for covariates, opioid users were significantly more likely to report insomnia than non-users (adjusted OR, 1.42; 95% CI, 1.25 –1.61).
Conclusion
Insomnia was 42% more likely among those who reported using prescription opioids compared to those who did not. With one half of the sample reporting prescription opioid use, and a fourth reporting insomnia it is important to further investigate the relationship between the two. Findings provide useful preliminary information from which to conduct further analyses.
Keywords: prescription opioids, insomnia, community, opioid use
1. Introduction
Insomnia is one of the most common sleep disorders with approximately 30% of the general population reporting brief symptoms of insomnia and 10% reporting chronic insomnia.1, 2 The International Classification of Sleep Disorders, 3rd edition (ICSD-3) defines insomnia as “a repeated difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, and results in some form of daytime impairment."3 Insomnia usually occurs independently or in combination with psychiatric and medical disorders, such as depression4, anxiety5, pain6, and sleep-disordered breathing (SDB). Half of all individuals suffering from SDB (50%) also report insomnia.7 In addition to difficulty initiating or maintaining sleep, the diagnostic criteria for primary insomnia from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) also includes that the difficulty causes distress or impairment in social, occupational, or other areas of functioning that does not occur exclusively during another sleep disorder, and that it is not due directly to physiological effects of a substance or medical condition.8 Insomnia can cause psychological9, occupational10,11, and economical12 consequences. For example, the National Transportation Safety Board (NTSB) has estimated that 57% of crashes leading to truck driver fatality were caused by fatigue,13 which may have been precipitated by inability to sleep due to insomnia or work requirements, and workers who report insomnia are much more likely to report injuries or industrial accidents than workers who report sleeping well.14
Prescription opioid use has increased dramatically in the United States in the last 25 years.16, 15 The number of opioid prescriptions almost tripled from 76 million to 207 million between 1991 and 2013, with the United States being one of the largest consumers globally.15 The increase in opioid prescriptions is problematic because of the associated consequences related to prescription opioid misuse and related to an increase in associated health problems. According to the Centers for Disease Control and Prevention (CDC), nearly 91 Americans die daily due to overdose of prescription opioids.16 This epidemic does not just have a direct effect on those who use opioids, but its consequences have far reaching effects on both families and whole communities all over the nation.
Previous studies have investigated the relationship between some substances and disrupted sleep, including the association between sleep and cigarette smoking17, antihypertensive drugs18, alcohol19, benzodiazepines20, hypnotics and anxiolytics.21 Common side effects from prescription opioid use are sleep disturbances such as SDB22 and reduction in sleep efficiency.23 Specifically, a clear relationship between SDB and opioid use has been established24 with studies reporting prevalence of SDB ranging from 42% to 85% among individuals taking chronic opioids.25 Insomnia has been found to be common among individuals with opioid use disorder who are going through withdrawal.8 Recently, Dolsen and Harvey reported that insomnia was related to heroin use among individuals seeking substance use treatment.26 Additionally, another study by Tran et al., found opioid use to be associated with five times the odds of developing or at risk of developing a sleep disorder.27 Insomnia may be an unintended pharmacological effect (side effect) of opioids. While such a relationship is likely, there is limited, but suggestive, information on the association between prescription opioid use and insomnia. This paper presents an analysis of prescription opioid use and insomnia, which was conducted among a large sample of community members in Northeast Florida. We hypothesize that insomnia will be more prevalent among individuals who report using prescription opioids in their lifetime compared to those who do not report prescription opioid use.
2. Methods
2.1 Setting and subjects
Participants were part of a community outreach program, HealthStreet, based in Gainesville, Florida. Through HealthStreet, Community Health Workers (CHWs) directly engage community members to reduce health disparities in health research participation.28 CHWs are trained and certified to make connections with people where they live and work to assess their health conditions and concerns with a University of Florida Institutional Review Board (IRB) approved Health Intake. Upon obtaining signed informed consent, the CHWs assess health information such as demographics and social determinants of health, research perceptions, medical conditions, and drug use. These data are then used to link people to social and medical services and opportunities to participate in health research. We were interested in examining the history of insomnia and prescription opioid use. These are the focus of these analyses among 8,433 community members who were interviewed between November 2011 and January 2017.
2.2 Measures
As part of an ongoing study this secondary data analysis used sociodemographic variables including age, gender, race (Black/African-American, White, or Other), ethnicity (Hispanic or Latino), marital status (never married; currently married; or separated, divorced, or widowed), and employment (yes or no). Additional self-reported variables were history of depression, history of anxiety, history of pain (back pain, headaches, or arthritis), and history of cancer elicited as: “Have you ever been told you had, or have you ever had a problem with [medical condition]?” Self-reported insomnia was also assessed by asking: “Have you ever been told you had, or have you ever had a problem with insomnia?”
Additional self-report measures for substance use included cigarette use, at risk alcohol use, and prescription opioid use. Cigarette use was assessed for lifetime use: “Have you ever smoked cigarettes? “At risk alcohol use was assessed for past 30 day use: “Within the last 30 days, have you had more than (4 for men, 3 for women) drinks like beer, wine, liquor in a single day?” We do not know if members only drank this quantity of alcohol once in the past 30 days or multiple times; however, we have used this question as a proxy for at risk drinking. Past 30 day and lifetime use of opioids was assessed: “Have you ever used prescription pain medication like Vicodin®, Oxycodone, codeine, Demerol®, morphine, Percocet®, Darvon® ? If yes, have you used prescription pain medications in the last 30 days?” Responses for the insomnia, opioid use, depression, anxiety, and alcohol use variables were coded as yes/no. Persons were coded as a never user, a lifetime but not past 30 day user or a past 30 day user. We used the term prescription opioids to distinguish between these and illicit opioids e.g., heroin; however, it should be noted that we cannot confirm if members had legitimate prescriptions for these opioids. Community members could have been using these opioids medically or non-medically.
2.3 Data Analysis
Data analysis was conducted using SAS, version 9.4.29 Demographic data were summarized using descriptive statistics. A chi-square test of independence was performed to compare whether there was a significant association between all variables and insomnia. An independent t-test was conducted to compare mean age in individuals who reported insomnia and those who did not. Multivariate logistic regression was used to calculate adjusted odds ratios (ORs) and 95% confidence intervals for insomnia. The covariates of age, gender, ethnicity, race, marital status, employment, history of depression, history of anxiety, history of cancer, cigarette use, alcohol use, and history of pain along with prescription opioid use were included in the model. The Hosmer-Lemeshow test was used to confirm adequate model fit.
3. Results
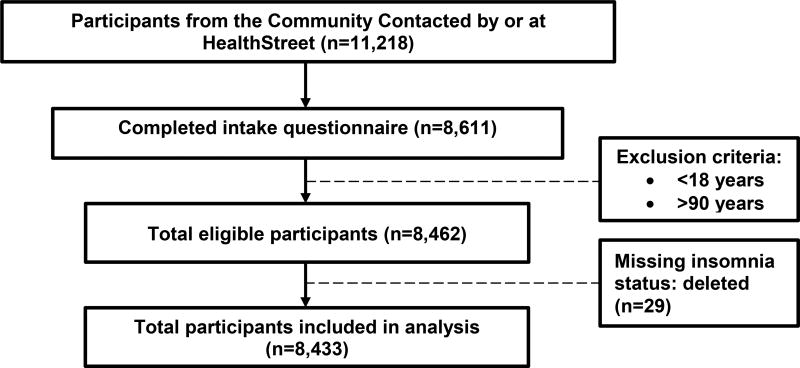
As shown in Figure 1, 11,218 community members received a 3 minute contact with a CHW and 8,611 stopped to talk and were assessed with the Health Intake questionnaire. After exclusion of persons under 18 and over 90, the sample size was reduced to 8,462 then further reduced to 8,433 to account for 29 people who did not provide information on insomnia. The sample was 58.8% female, 60.8% black, 21.1% are married, 35.1% employed, 27.9% with depression, 23.0% with anxiety, 51.9% used cigarettes in their lifetime, 23.9% alcohol users in the past 30 days, and 65.7% with pain. In addition, 3,475 (41.3%) reported neither insomnia nor prescription opioid use, 707 (8.4%) reported insomnia without any prescription opioid use, 2,831 (33.6%) reported prescription opioid use without insomnia, and 1,405 (16.7%) reported both insomnia and prescription opioid use.
Figure 1.
Participant flow of HealthStreet members 11/2011 through 1/2017
Table 1 displays the demographic characteristics of participants, stratified by reported insomnia, and results of the crude tests of association. Overall, the mean age of participants was 44.2 years and those who reported insomnia were significantly older than those who did not (47.1 years vs 43.3 years). Those who reported insomnia compared to those who did not were significantly more likely to be female, Caucasian, not employed, report depression, anxiety, pain, cancer, cigarette use, and lifetime and past 30 day only opioid use (p <.0001).
Table 1.
Characteristics of HealthStreet members who have and who have not reported insomnia (N=8,433)
| Characteristics | Overall (n=8,433) n (%) |
No Insomnia (n=6,318) n (%) |
Insomnia (n=2,115) n (%) |
p value | |
|---|---|---|---|---|---|
| Mean age (±SD) *: | 44.2 (15.8) | 43.3 (16.1) | 47.1 (14.3) | <.0001 | |
|
| |||||
| Gender (n=8,423)*: | |||||
| Male | 3473 (41.2) | 2729 (43.2) | 744 (35.2) | <.0001 | |
| Female | 4950 (58.8) | 3582 (56.7) | 1368 (64.8) | ||
|
| |||||
| Ethnicity (n=8,318): | |||||
| Hispanic/Latino | 495 (5.9) | 353 (5.6) | 142 (6.8) | .0577 | |
|
| |||||
| Race (n=8,421)*: | |||||
| Black | 5117 (60.8) | 4089 (64.8) | 1028 (48.6) | ||
| Caucasian | 2740 (32.5) | 1827 (30.0) | 913 (43.2) | <.0001 | |
| Other | 564 (6.7) | 390 (6.2) | 174 (8.2) | ||
|
| |||||
| Marital status (n=8,413)*: | |||||
| Never married | 3998 (47.5) | 3165 (50.2) | 833 (39.4) | ||
| Currently married | 1771 (21.1) | 1361 (216) | 410 (19.4) | <.0001 | |
| Separated, divorced, or widowed | 2644 (31.4) | 1775 (28.2) | 869 (41.2) | ||
|
| |||||
| Employed (n=8,382)*: | 2941 (35.1) | 2383 (40.0) | 558 (26.6) | <.0001 | |
|
| |||||
| Depression (n=8,344)*: | 2342 (27.9) | 1175 (18.7) | 1167 (55.4) | <.0001 | |
|
| |||||
| Anxiety (n=8,412)*: | 1993 (23.0) | 932 (14.8) | 1001 (47.5) | <.0001 | |
|
| |||||
| Pain (n=8,395)*: | 5513 (65.7) | 3745 (59.6) | 1768 (83.8) | <.0001 | |
|
| |||||
| Cancer (n=8,390)* | 677 (8.1) | 418 (6.7) | 259 (12.3) | <.0001 | |
|
| |||||
| Cigarette use (n=8,431)*: | 4378 (51.9) | 3051 (48.3) | 1327 (62.7) | <.0001 | |
|
| |||||
| At risk alcohol use (3/4 drinks in past 30 days; n=8,416) | 2007 (23.9) | 1465 (23.2) | 542 (25.7) | .0237 | |
|
| |||||
| Opioid use (n=8,418)*: | |||||
| Never | 4182 (49.7) | 3475 (55.1) | 701 (33.5) | ||
| Lifetime (not past 30 days) | 3074 (36.5) | 2100 (33.3) | 974 (46.1) | <.0001 | |
| Past 30 day only | 1162 (13.8) | 731 (11.6) | 431 (20.4) | ||
Note: P value= P value of chi-square or t-test
p-value and t-test significant (<.0001)
After adjustment for age, gender, ethnicity, race, marital status, employment, history of depression, history of anxiety, history of pain, lifetime use of cigarettes and at risk alcohol use in the past 30 days, opioid users were significantly more likely to report insomnia than non-users. There was no evidence of effect modification after stratification by sex (data not shown). Table 2 provides results of the adjusted multivariate logistic regression model predicting self-reported insomnia. Depression was the strongest risk factor for insomnia, with those reporting a history of depression 2.74 times more likely to report insomnia than those without a history of depression (adjusted OR: 2.74; 95% CI, 2.40–3.12). Lifetime opioid users were as likely to report insomnia (adjusted OR: 1.42; 95% CI, 1.25 –1.61) as current users (adjusted OR: 1.44; 95% CI, 1.22 – 1.70), compared to never users.
Table 2.
Adjusted odds ratios for the association between self-reported insomnia and risk factors among HealthStreet members (n=2,095)
| Characteristic | Adjusted odds ratio for self-reported insomnia | ||
|---|---|---|---|
|
| |||
| Odds Ratio | 95% Confidence Interval | Beta coefficient | |
| Age : | 1.01 | 1.00* | 0.0081 |
|
| |||
| Gender: | |||
| Male | Ref | Ref | |
| Female | 1.11 | 0.98, 1.25 | 0.0994 |
|
| |||
| Ethnicity: | |||
| Non-Hispanic/Latino | Ref | Ref | |
| Hispanic/Latino | 1.14 | 0.89, 1.47 | 0.1340 |
|
| |||
| Race: | |||
| Black | Ref | Ref | |
| White | 1.19 | 1.05, 1.35* | 0.1709 |
| Other | 1.51 | 1.89, 1.93* | 0.4136 |
|
| |||
| Marital status: | |||
| Never married | Ref | Ref | |
| Currently married | 0.92 | 0.78, 1.03 | −0.0826 |
| Separate, divorced, or widowed | 1.11 | 0.96, 1.29 | 0.1071 |
|
| |||
| Employed: | |||
| Not employed | Ref | Ref | |
| Employed | 0.91 | 0.80, 1.03 | −0.0982 |
|
| |||
| Depression: | |||
| No depression | Ref | Ref | |
| Depression | 2.74 | 2.40, 3.12** | 1.0067 |
|
| |||
| Anxiety: | |||
| No anxiety | Ref | Ref | |
| Anxiety | 2.26 | 1.97, 2.60** | 0.8167 |
|
| |||
| Pain: | |||
| No pain | Ref | Ref | |
| Pain | 2.01 | 1.75, 2.32** | 0.6994 |
|
| |||
| Cancer: | |||
| No cancer | Ref | Ref | |
| Cancer | 1.28 | 1.06, 1.55* | 0.2458 |
|
| |||
| Cigarette use: | |||
| No cigarette use | Ref | Ref | |
| Cigarette use | 1.27 | 1.13, 1.43** | 0.2415 |
|
| |||
| Alcohol use: | |||
| No alcohol use | Ref | Ref | |
| Alcohol use | 1.17 | 1.02, 1.33* | 0.1558 |
|
| |||
| Prescription opioid use: | |||
| Never | Ref | Ref | |
| Lifetime | 1.42 | 1.25, 1.61** | 0.3480 |
| Past 30 days | 1.44 | 1.22, 1.70** | 0.3620 |
p<.0001,
p<0.05, Insomnia reported as yes or no; event= yes
4. Discussion
In this sample of 8,433 community members we assessed the association between insomnia and prescription opioid use. One-fourth of our sample reported insomnia (25.0%), similar to the rate of insomnia symptoms among the general population (30%).30 Additional data from the CDC show that 35% of Americans report insufficient sleep (fewer than 7 hours).31 This high rate of insufficient sleep may contribute to the rate of self-reported insomnia in this sample.
Florida has had one of the highest rates in the nation for prescribing opioids, resulting in an increase in adverse health outcomes associated with prescription opioid use which has prompted the launch of the state’s Prescription Drug Monitoring Program.32 Data from the National Health and Nutrition Examination Survey (NHANES) estimates that 6.9% of Americans have used a prescription opioid in the past 30 days.33 The results from this community sample yielded a much higher rate than NHANES, with 13.8% reporting past 30 day use, suggesting that this may be a geographic area where targeted interventions to reduce opioid use may be required; however, it is also possible that over-reporting may have occurred in the sample or that this sample represents a group that is using at a higher rate than the general population for other uncaptured reasons.
Risk factors for insomnia are in line with previous studies. Alcohol19,34, cigarette smoking17, depression4, anxiety5, older age35, and pain6 have all been previously associated with insomnia. Specifically, multiple studies have linked pain to sleep disturbance and there is evidence of temporal precedence of sleep disturbances over pain.36,37 Prior literature has also shown that gender is a risk factor for insomnia, with females more likely to report insomnia than males38,39; however after adjustment for confounders in our analysis we did not find a higher rate of insomnia among women. As expected from previous studies4,40,41, depression was the greatest risk factor for insomnia in our study. Interestingly, after controlling for these established risk factors, including depression, those who reported any opioid use were still more likely to report insomnia than those who never used opioids.
Overall, self- reported insomnia was significantly associated with prescription opioid use and this association remained significant after controlling for demographic and health factors. With opioid use continuing to escalate in the US, and insomnia reaching epidemic proportions42, it is important to further investigate the possible relationship between insomnia and prescription opioids. The increase in prescription opioid use in the past decade43 has had many other health implications aside from insomnia such as dependence44 and overdose.45 As such, it is important to address both the issue of high levels of opioid use and to further investigate the relationship between prescription opioids and insomnia.
This study had a few limitations. First, the data collected relating to prescription opioid use and insomnia are self-reported; however, the study did not attempt to ask participants to quantify amount of opioid use and so the potential for misclassification of the exposure was limited. We also do not have information on individual dose, frequency and duration of opioid use. Insomnia may be over-reported by participants and so the outcome in this study may not necessarily meet the diagnoses of insomnia according to DSM-5 criteria. Some individuals who reported insomnia may have self-diagnosed rather than visiting a physician. However, results from a sleep study by Lauderdale et al., show that participants self-report of the amount of sleep they attain is moderately correlated with actual sleep time;46 self-reported data relating to insomnia may also be reported with minimal measurement error. However, we recognize that people may over or under report their sleep problems. In addition to the potential error introduced through self-report, we also used a proxy measure for at risk drinking which may not reflect a pattern of at risk drinking. Secondly, our findings are based on cross sectional data and reflect an association between insomnia and prescription opioid use and not causality. Additionally, we cannot discern whether prescription opioid use occurred at the same time as the sleep impairment. However, the strengths of this study are that this is among the first analyses to assess insomnia and opioid use in a community sample, which has a large sample size and was conducted in a diverse population.
4.1 Conclusions
Overall, these results show a high prevalence of insomnia among community members in Northeast Florida. An association between prescription opioids and insomnia was found even after adjustment for known risk factors. These results provide useful preliminary information and future studies should further investigate the temporal relationship between insomnia and prescription opioid use.
Acknowledgments
This work was supported by the National Institutes of Health and National Clinical and Translational Science Award UF grant [UL1, TR000064]; and the National Institute on Drug Abuse of the National Institutes of Health at the UF Substance Abuse Training Center, University of Florida, FL [T32DA035167 Cottler, PI].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interests:
None to declare.
Ethical approval:
This study was approved by the University of Florida Institutional Review Board and informed consent was obtained for each participant.
References
- 1.Benca RM. Diagnosis and treatment of chronic insomnia: a review. Psychiatr Serv Wash DC. 2005;56(3):332–343. doi: 10.1176/appi.ps.56.3.332. [DOI] [PubMed] [Google Scholar]
- 2.Roth T. Insomnia: Definition, Prevalence, Etiology, and Consequences. J Clin Sleep Med JCSM Off Publ Am Acad Sleep Med. 2007;3(5 Suppl):S7–S10. [PMC free article] [PubMed] [Google Scholar]
- 3.Darien IL, editor. American Academy of Sleep Medicine. International Classification of Sleep Disorders. 3. American Academy of Sleep Medicine; 2014. [Google Scholar]
- 4.Benca RM, Peterson MJ. Insomnia and depression. Sleep Med. 2008;9(Supplement 1):S3–S9. doi: 10.1016/S1389-9457(08)70010-8. [DOI] [PubMed] [Google Scholar]
- 5.Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: Exploration of the direction of risk. J Psychiatr Res. 2006;40(8):700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Tang NKY, Wright KJ, Salkovskis PM. Prevalence and correlates of clinical insomnia co-occurring with chronic back pain. J Sleep Res. 2007;16(1):85–95. doi: 10.1111/j.1365-2869.2007.00571.x. [DOI] [PubMed] [Google Scholar]
- 7.Lavie P. Insomnia and sleep-disordered breathing. Sleep Med. 2007;8(Supplement 4):S21–S25. doi: 10.1016/S1389-9457(08)70005-4. [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM 5. (5) 2013 [Google Scholar]
- 9.Karaz SS. Insomnia in Psychiatric Disorders. In: Attarian HP, Schuman C, editors. Clinical Handbook of Insomnia. Current Clinical Neurology. Humana Press; 2010. pp. 229–241. [DOI] [Google Scholar]
- 10.Sivertsen B, Overland S, Neckelmann D, et al. The Long-term Effect of Insomnia on Work Disability The HUNT-2 Historical Cohort Study. Am J Epidemiol. 2006;163(11):1018–1024. doi: 10.1093/aje/kwj145. [DOI] [PubMed] [Google Scholar]
- 11.Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J, Baillargeon L. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10(4):427–438. doi: 10.1016/j.sleep.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 12.Daley M, Morin CM, LeBlanc M, Grégoire J-P, Savard J. The Economic Burden of Insomnia: Direct and Indirect Costs for Individuals with Insomnia Syndrome, Insomnia Symptoms, and Good Sleepers. Sleep. 2009;32(1):55–64. [PMC free article] [PubMed] [Google Scholar]
- 13.Safety Study: Fatigue, Alcohol, Other Drugs, and Medical Factors in Fatal-to-the-Driver Heavy Truck Crashes. 1990;1 [Google Scholar]
- 14.Léger D, Guilleminault C, Bader G, Lévy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep. 2002;25(6):625–629. [PubMed] [Google Scholar]
- 15.Abuse NI on D. America’s Addiction to Opioids: Heroin and Prescription Drug Abuse. [Accessed July 18, 2016]; https://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2016/americas-addiction-to-opioids-heroin-prescription-drug-abuse. Published May 14, 2014.
- 16.Understanding the Epidemic [Internet] Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. 2016 [cited 2017Jan28]. Available from: https://www.cdc.gov/drugoverdose/epidemic/.
- 17.Fucito LM, Redeker NS, Ball SA, Toll BA, Ikomi JT, Carroll KM. Integrating a Behavioural Sleep Intervention into Smoking Cessation Treatment for Smokers with Insomnia: A Randomised Pilot Study. J Smok Cessat. 2014;9(01):31–38. doi: 10.1017/jsc.2013.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruno RM, Palagini L, Mancuso V, et al. Abstract 438: Association between Insomnia and Use of BP-lowering Drugs in hypertensive Patients: a Cross-sectional Cohort Study. Hypertension. 2014;64(Suppl 1):A438–A438. [Google Scholar]
- 19.Thakkar MM, Sharma R, Sahota P. Alcohol disrupts sleep homeostasis. Alcohol. 2015;49(4):299–310. doi: 10.1016/j.alcohol.2014.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lu X-M, Zhu J-P, Zhou X-M. The effect of benzodiazepines on insomnia in patients with chronic obstructive pulmonary disease: a meta-analysis of treatment efficacy and safety. Int J Chron Obstruct Pulmon Dis. 2016;11:675–685. doi: 10.2147/COPD.S98082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stewart R, Besset A, Bebbington P, et al. Insomnia comorbidity and impact and hypnotic use by age group in a national survey population aged 16 to 74 years. Sleep. 2006;29(11):1391–1397. doi: 10.1093/sleep/29.11.1391. [DOI] [PubMed] [Google Scholar]
- 22.Opioid Therapy and Sleep Disorders: Risks and Mitigation Strategies - Cheatle - 2015 - Pain Medicine - Wiley Online Library. [Accessed July 18, 2016]; doi: 10.1111/pme.12910. http://onlinelibrary.wiley.com/doi/10.1111/pme.12910/full. [DOI] [PMC free article] [PubMed]
- 23.Moore P, Dimsdale JE. Opioids, sleep, and cancer-related fatigue. Med Hypotheses. 2002;58(1):77–82. doi: 10.1054/mehy.2001.1461. [DOI] [PubMed] [Google Scholar]
- 24.Jungquist CR, Flannery M, Perlis ML, Grace JT. Relationship of Chronic Pain and Opioid Use with Respiratory Disturbance during Sleep. Pain Manag Nurs. 2012;13(2):70–79. doi: 10.1016/j.pmn.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 25.Correa D, Farney RJ, Chung F, Prasad A, Lam D, Wong J. Chronic Opioid Use and Central Sleep Apnea: A Review of the Prevalence, Mechanisms, and Perioperative Considerations. Anesth Analg. 2015;120(6):1273–1285. doi: 10.1213/ANE.0000000000000672. [DOI] [PubMed] [Google Scholar]
- 26.Dolsen MR, Harvey AG. Lifetime history of insomnia and hypersomnia symptoms as correlates of alcohol, cocaine, and heroin use and relapse among adults seeking substance use treatment in the United States from 1991 to 1994. Addiction. 2017 Jan; doi: 10.1111/add.13772. n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tran A, Fuller JM, Wong KK, Krass I, Grunstein R, Saini B. The development of a sleep disorder screening program in Australian community pharmacies. Pharm World Sci. 2009;31(4):473–480. doi: 10.1007/s11096-009-9301-4. [DOI] [PubMed] [Google Scholar]
- 28.Meeting APA, Cottler LB. Mental Health in Public Health: The Next 100 Years. Oxford University Press; 2011. [Google Scholar]
- 29.SAS Institute Inc., 9.4. Cary, NC: SAS Institute Inc.; 2011. [Google Scholar]
- 30.CDC - Sleep Home Page - Sleep and Sleep Disorders. [Accessed July 18, 2016]; http://www.cdc.gov/sleep/index.html.
- 31.Liu Y. Prevalence of Healthy Sleep Duration among Adults — United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65 doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- 32.Surratt HL, O’Grady C, Kurtz SP, et al. Reductions in prescription opioid diversion following recent legislative interventions in Florida. Pharmacoepidemiol Drug Saf. 2014;23(3):314–320. doi: 10.1002/pds.3553. [DOI] [PubMed] [Google Scholar]
- 33.Products - Data Briefs - Number 189 - February 2015. [Accessed July 18, 2016]; http://www.cdc.gov/nchs/data/databriefs/db189.htm.
- 34.Brower KJ, Perron BE. Sleep disturbance as a universal risk factor for relapse in addictions to psychoactive substances. Med Hypotheses. 2010;74(5):928–933. doi: 10.1016/j.mehy.2009.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Newman AB, Enright PL, Manolio TA, Haponik EF, Wahl PW On behalf of the Cardiovascular Health Study Research Group. Sleep Disturbance, Psychosocial Correlates, and Cardiovascular Disease in 5201 Older Adults: The Cardiovascular Health Study. J Am Geriatr Soc. 1997;45(1):1–7. doi: 10.1111/j.1532-5415.1997.tb00970.x. [DOI] [PubMed] [Google Scholar]
- 36.Bigatti SM, Hernandez AM, Cronan TA, Rand KL. Sleep disturbances in fibromyalgia syndrome: Relationship to pain and depression. Arthritis Care Res. 2008;59(7):961–967. doi: 10.1002/art.23828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bromberg MH, Gil KM, Schanberg LE. Daily sleep quality and mood as predictors of pain in children with juvenile polyarticular arthritis. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2012;31(2):202–209. doi: 10.1037/a0025075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ohayon MM, Roth T. What are the contributing factors for insomnia in the general population? J Psychosom Res. 2001;51(6):745–755. doi: 10.1016/S0022-3999(01)00285-9. [DOI] [PubMed] [Google Scholar]
- 39.Krystal AD. Insomnia in women. Clin Cornerstone. 2003;5(3):41–50. doi: 10.1016/S1098-3597(03)90034-2. [DOI] [PubMed] [Google Scholar]
- 40.Riemann D, Voderholzer U. Primary insomnia: a risk factor to develop depression? J Affect Disord. 2003;76(1–3):255–259. doi: 10.1016/S0165-0327(02)00072-1. [DOI] [PubMed] [Google Scholar]
- 41.Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rössler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473–480. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Research C on SM and, Policy B on HS, Medicine I of. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. National Academies Press; 2006. [PubMed] [Google Scholar]
- 43.Vital Signs: Overdoses of Prescription Opioid Pain Relievers --- United States, 1999–2008. [Accessed July 18, 2016]; http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6043a4.htm?s_cid=mm6043a4_w#fig2. [PubMed]
- 44.Katz C, El-Gabalawy R, Keyes KM, Martins SS, Sareen J. Risk factors for incident nonmedical prescription opioid use and abuse and dependence: Results from a longitudinal nationally representative sample. Drug Alcohol Depend. 2013;132(1–2):107–113. doi: 10.1016/j.drugalcdep.2013.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jones CM, Mack KA, Paulozzi LJ. PHarmaceutical overdose deaths, united states, 2010. JAMA. 2013;309(7):657–659. doi: 10.1001/jama.2013.272. [DOI] [PubMed] [Google Scholar]
- 46.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-Reported and Measured Sleep Duration: How Similar Are They? Epidemiology. 2008;19(6):838–845. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]