Abstract
Forty eight of the African continent’s 54 sovereign states are located in the Sub-Saharan Africa (SSA) region, with the government of each defining and shaping its own health services and delivery systems. This paper reviews the trends and patterns of contraceptive practice in the region. Using survey data available from the Demographic and Health Surveys and Performance Monitoring and Accountability 2020, the study finds modern contraceptive practice to be on the rise overall but with much geographic variation. The contraceptive methods most frequently used are injectables and, more recently, implants. Higher levels of use are observed among unmarried sexually active than married females. Although use is rising, contraceptive discontinuation rates are also high. Recent program initiatives discussed include expanding long-acting contraceptive options, promoting and delivering contraceptive methods in the postpartum period, and relying on community health workers for contraceptive outreach and service delivery. SSA’s family planning situation remains challenged by weak health systems which must address competing priorities to manage disease prevention as well as primary health care. Increasing investments in family planning delivery in many SSA countries, however, augur for continued rapid uptake of modern contraception, possibly matching if not outpacing the record of other regions.
Background
In 1959, George Murdock, a well-known academic anthropologist, published Africa: Its Peoples and Their Culture History, offering a comprehensive ethnographic survey and an inventory of some 5,000 tribal names. Captured in the map in the appendix, Murdock grouped the 1,267 ethnic divisions into 186 cultural “provinces”. Demographer, Frank Lorimer, reviewing Murdock’s book in 1960 noted the spatial variation in ethnic clustering and their implications for population diversity and growth, constrained by such factors as water access and agricultural cultivation techniques, and facilitated by social practices such as polygyny and slavery. The visually striking coloration of the ethnographic map brings to mind lessons learned from the European fertility transition that emerged over 100 to 300 years–where rates fell more quickly along linguistic, cultural and spatial lines than along social structural ones. By implication, Africa’s ethno-geographic boundaries up to the second half of the last century would not likely have accelerated the spread of ideation around reduced fertility or the adoption of modern contraceptive methods. Rather such divergent ideas and practices, when present, likely were insulated within the many ethno-linguistic clusters and had limited transmissibility. With the added legacy of colonial languages of English, French and Portuguese, the spread and diffusion of ideas may only have been accelerated after the introduction of electronic mass media and telecommunication channels and improved road and transportation systems.
Today the peoples of the African continent are governed by 54 sovereign nations, six of which are in northern Africa and the balance in Sub-Saharan Africa (SSA). Under the African Union, established in 2002, those 54 member countries1 are further organized into five subregions—Northern, West, Middle, East, and Southern. The growing economic cooperation among African countries is enabled by sub-regional organizations for economic development, such as the Southern African Development Community (SADC), East African Community (EAC), and Economic Community of West African States (ECOWAS). Many SSA countries presently are experiencing high annual rates of economic growth. Between 2010 and 2014 growth rates have been in excess of 5% in Ethiopia (10.5%), Cote d’Ivoire (8.7%), the Democratic Republic of Congo (8.5%) and Zambia (6.7%)2, and their performance relative to those of their neighbors may motivate other SSA governments to seek to expand their trade and market opportunities to avoid being left behind. In a 2012 report of the joint meeting of African ministers of finance under the UN Economic Commission for Africa and the Africa Union, the continent is seen as a new global market and driver of consumer demand, i.e., “Africa as the Next Growth Pole”3. While a few resource-rich countries face significant fiscal deficits as a result of declining oil revenues, a recent African Economic Outlook report sees steady resilience in SSA economies and estimates growth in real GDP in 2016 for this sub-region, net of South Africa, to be 4.2% and rising to 4.5% in 2017 (African Development Bank, Organization of Economic, Cooperation and Development and UN Development Program, 2016).
The popular media has often treated Africans in the SSA region as significantly lagging behind on economic and human development indicators and continuously in need of donor aid4. There are suggestions that African consciousness of this is rising and efforts to establish self-sufficiency are growing. In 2001 at their annual meeting in Abuja, Nigeria, the African Heads of State pledged to commit 15% of their total annual government budgets to the health sector. A decade later, while just six have met this mark, annual government per capita spending on health has risen, averaging between $25–27.
From a demographic perspective, fertility rates vary considerably across Sub-Saharan Africa’s five main regions (United Nations, 2016a). Total fertility rates, which hovered at 6.5 births per woman in the early 1960s across all regions, now range from 2.38 births per woman in southern Africa, to 3.05 in northern Africa, to 4.52 in eastern Africa and to 5.2–5.3 in western and middle Africa. Demographers have identified definitive onsets but with considerable spatial and temporal variation in pace (Garenne, 2008; Johnson et al., 2011; Bongaarts and Casterline, 2012; Westoff et al., 2013; and Lesthaeghe, 2014). Johnson et al. and Westoff et al., who analyze DHS data on fertility trends, note there are at least 30-some fertility transitions underway but in various phases. Garenne (2008) observes that over a 30 to 40 year period about three-fifths of the transition from peak to replacement fertility levels have occurred in urban areas of SSA and about one fifth of this transition is being experienced in rural areas in 20 to 30 years. An UN review (NAS, 2016) notes variation in the speed of fertility declines in nine geographic clusters in SSA, with some being quite rapid. If the pace of the more rapid changes spreads to other parts of the subcontinent, SSA countries may defy the expectations of most demographers regarding the potential and realized speed of its fertility transitions. The UN anticipates the largest reductions in fertility between 2010–2015 and 2045–2050 to occur in Africa.
An important driver will be recent and significant declines in infant and child mortality. The under-five mortality rate has decreased between 2000–2005 and 2010–2015 by 20% or more in 42 out of 57 countries in all of Africa (United Nations, 2016a). The infant mortality rate in the SSA region has declined from 88 to 64 deaths per 1000 live births in this period, and is just one third its 1950–1955 estimated level of 183. Under-five mortality for the SSA region reduced from 142 deaths under age 5 per 1000 live births to 99, or a 30% reduction, in the ten-year period and is also one third of its 1950–55 rate of 307. The robust developments of the past decade are not only heralded for their reflection of improved wellbeing and longevity but also signal prospective changes in parental demand for future childbearing, particularly in the context of rising childrearing costs.
Among the main influences on fertility, marriage ages for females and levels of completed schooling, both of which have increased, are seen as responsible for some of the observed fertility declines (Garenne, 2014). The short-term effects of later marriage and higher schooling for females will appear in lower adolescent fertility rates, an age component of total fertility rates. With declining infant and child mortality, lower demand for fertility will likely lead to higher demand for contraception-assisted birth spacing. Fertility demand, though, is to be distinguished from contraceptive demand, as change in one does not automatically mean a change in the other. Casterline and El Zeini (2014) have noted the weak association between trends in unmet need and fertility in Sub-Saharan Africa. Bongaarts and Casterline (2012) have observed slow change in fertility preferences and ideal family size in the SSA region, behind the pace of those in Asia or Latin America in the 1970s. However, as will be seen subsequently, regional trends in modern contraceptive use suggest SSA’s pace of uptake, and thus contraceptive demand, has accelerated since 2005. This distinction between fertility and contraceptive demand helps explain why the measure “unmet need”, which is based on non-contracepting women not using contraception but desiring to delay or limit their births, also tends to change slowly. Also an earlier study has proposed that increases in contraceptive use were achieved by satisfying existing demand (Feyisetan and Casterline, 2000), cautioning some uncertainty over the continued pace of the SSA region’s rising trend in contraceptive use.
Family planning in Sub-Saharan Africa
Sub-Saharan African governments demonstrated little enthusiasm for international offers of population/family planning assistance in the 1980s through the 1990s (May, 2016), and Caldwell and Caldwell (2002) earlier emphasized the need to overcome strong cultural resistance to family planning. However, two developments in the health arena have spurred greater policy support for improving sexual and reproductive health (SRH), both directly and indirectly. The first was the expanding HIV epidemic in the 1990s and 2000s which forced countries with high infection rates to confront their weak health systems and inadequate per capita health spending. In so doing, these governments began to absorb significant international funding for HIV programs, as well as malaria and tuberculosis, in order to deliver specialized care and treatment. This also required policymakers and the public to recognize sexual behavior as a driver of viral transmission. By openly addressing a range of education, prevention and treatment needs for varying risk populations, health systems and providers, and tracking progress, program efforts in many SSA countries to arrest the AIDS crisis benefited other health areas, such as maternal and child health and family planning. Condoms, male circumcision, and pre-exposure prophylaxis regimens have expanded the means for disease prevention. The US government’s President’s Emergency Plan for AIDS Relief (PEPFAR) bestowed hundreds of millions of dollars in assistance that, despite the criticisms, may have strengthened health systems and service delivery. We return to this development later in the paper.
A second development was the 2006 adoption of the African Union’s Maputo Program of Action (MPoA) by 48 ministers of health. The MPoA’s goal was to ensure universal access to reproductive health by 2015, thereby aligning with one of Millennium Development Goal (MDG) 5’s targets. The MPoA framework identified six key strategies that included integration of HIV/AIDS/STI and sexual and reproductive health and rights (SRHR) services; repositioning family planning as essential to MDG achievement, addressing adolescent and youth SRH needs, addressing unsafe abortion, delivering quality and affordable services for safe motherhood, child survival, newborn and child health; and promoting African and south-south cooperation for the attainment of ICPD and MDG goals in the region. Forged through a partnership between the Africa Union and the International Planned Parenthood Federation, the MPoA was catalytic in focusing ministerial attention on the significance of SRHR needs and MDG attainment, but also appeared at a time when global health discourse and resources were disproportionately focused on mitigating the HIV epidemic, sidelining earlier priorities on reproductive health needs, in particular those of women, mothers and newborns. Although the MPoA was not the singular policy instrument to accelerate the expansion of family planning in SSA, its adoption by African heads of state in 2007 gave credence and legitimacy to the strategic objectives of repositioning contraceptive service delivery, reducing unsafe abortion and addressing the SRH needs of adolescents. Even though not accompanied by significant new funding, SRH ideation in the SSA region was accelerated. The MPoA also emerged at a politically significant time when US government conservatism was strong and had stigmatized reproductive health and family planning efforts.
Enthusiasm for family planning rose decidedly after the 2012 London Summit, co-sponsored by the Bill & Melinda Gates Foundation and the UK Government, in partnership with the United Nations Population Fund, national governments, other donors, civil society, and agencies from other sectors. The Summit issued a call for global and national commitments to enable 120 million more women and girls to use contraceptives by 20205. Some 49 governments, including 39 from African and ten others from the poorest 69 countries, have since made commitments. The Summit encouraged governmental and non-governmental organizations to expand contraceptive supply and access through improved commodity supply chains, systems and service delivery models; increased demand and support for family planning; and greater accountability through monitoring and evaluation, among other things. A biennial series of international family planning conferences, three of four having been held in the SSA region, appears to have provided added momentum for the London Summit. Yet modern contraceptive use began rising since 1995, predating the London Summit. In this context, a renewed consideration of contraceptive practices and trends is warranted.
Organization of paper
This paper begins by presenting an overview of modern contraceptive practice levels and trends in SSA and other world regions and then focuses on use in SSA countries among unmarried and married female subpopulation and by type of contraceptive method, predominantly injectables. Durations of contraceptive use and reasons for termination are examined next. With contraceptive discontinuation rates relatively high, family planning program managers have pursued several key initiatives to improve access by using community and primary care providers, expanding long-acting method options and integrating delivery during the postpartum period. After examining the SSA experience with these initiatives, we discuss the implications for future contraceptive use in Sub-Saharan Africa.
Source of data
The Demographic and Health Surveys (DHS) program offers the most extensive time series of standardized national measures of contraceptive practice, having conducted sample surveys of households and eligible women, and occasionally men, of reproductive ages since 1985. We access the data from survey reports, the online StatCompiler tool (www.statcompiler.com) and conduct primary analyis. The second source of data is from dedicated national family planning indicator surveys under the Performance Monitoring and Accountability 2020 project which began in mid-2013 (www.pma2020.org). The first four rounds of these surveys, most of which are national in scope, are conducted six months apart and are informative of recent trends in prevalence and methods used. A third data source is the United Nations world contraceptive use database (United Nations 2016b).
Findings
Trends and patterns of contraceptive use in SSA countries
With the UN contraceptive use database, we calculate regional averages of modern contraceptive prevalence rates (mCPR) among married women age 15 to 49 across four time periods: 1960–1979, 1980–1994, 1995–2004 and 2005–2015. The database compiles national survey estimates primarily for women married or in union. Countries that contribute more than one survey estimate of mCPR in a given time period are averaged and all country-specific estimates are summed and an unweighted average taken for each time period. Small differences in country composition in each region for a given time period can account for some of the observed nonlinear trend lines. For example in 2005–2015, seven countries in Oceania (e.g., Nauru, Solomon Islands, Tonga and Tuvalu) reported mCPR estimates for the first and only time, compared to others (Australia, Vanuatu, Marshall Islands) with estimates for 3 or more time points. Similarly several European countries reported mCPR estimates for the first time during 1980–1994 (e.g., Estonia, Greece, Lithuania, Slovakia, and Sweden).
Table 1 shows the Americas’ (composed of the US and Canada) mCPR average for the 2005–2015 period to be nearly 45 points higher than Africa’s (70.7% to 25.1%) and countries in Latin America/Caribbean’s averaging 58.4%, higher by 33 points. Although the Africa region has the lowest mCPR levels, the trend is upward. The slopes for the trend lines for Latin America and the Caribbean, Asia and Africa from 1980 onward are very similar, particularly from 1995–2004 to 2005–2015, as seen in Figure 1a.
Table 1.
Modern contraceptive prevalence among married women 15–49 years by world region and African sub-region and period
| World region | # of countries | # of surveys | % using modern method | Sub-Saharan African region | # of countries | # of surveys | % using modern method |
|---|---|---|---|---|---|---|---|
| Americas | 2 | 18 | 67.8 | Sub-Saharan Africa (48) | |||
| 1960–1979 | 1 | 6 | 56.7 | 1960–1979 | 6 | 6 | 7.3 |
| 1980–1994 | 2 | 4 | 68.1 | 1980–1994 | 35 | 54 | 12.0 |
| 1995–2004 | 2 | 5 | 71.5 | 1995–2004 | 45 | 85 | 17.5 |
| 2005–2015 | 1 | 3 | 70.7 | 2005–2015 | 45 | 121 | 22.9 |
| Europe | 37 | 162 | 47.6 | Northern Africa (6) | |||
| 1960–1979 | 21 | 35 | 26.5 | 1960–1979 | 2 | 2 | 16.8 |
| 1980–1994 | 22 | 35 | 56.4 | 1980–1994 | 12 | 21 | 17.1 |
| 1995–2004 | 26 | 50 | 52.2 | 1995–2004 | 17 | 36 | 20.2 |
| 2005–2015 | 23 | 42 | 53.1 | 2005–2015 | 17 | 44 | 27.1 |
| Asia | 47 | 374 | 36.6 | West Africa (16) | |||
| 1960–1979 | 21 | 54 | 20.2 | 1960–1979 | 2 | 2 | 3.1 |
| 1980–1994 | 35 | 88 | 34.1 | 1980–1994 | 15 | 22 | 4.4 |
| 1995–2004 | 46 | 116 | 39.4 | 1995–2004 | 15 | 25 | 9.9 |
| 2005–2015 | 41 | 116 | 43.8 | 2005–2015 | 16 | 51 | 14.6 |
| Latin America and Caribbean | 39 | 200 | 48.2 | Eastern Africa (18) | |||
| 1960–1979 | 18 | 31 | 30.8 | 1960–1979 | 2 | 2 | 16.8 |
| 1980–1994 | 33 | 68 | 44.7 | 1980–1994 | 12 | 21 | 17.1 |
| 1995–2004 | 27 | 49 | 54.5 | 1995–2004 | 17 | 36 | 20.2 |
| 2005–2015 | 25 | 52 | 58.3 | 2005–2015 | 17 | 44 | 27.1 |
| Oceania | 16 | 32 | 36.1 | Middle Africa (9) | |||
| 1960–1979 | 4 | 4 | 32.7 | 1960–1979 | 1 | 1 | 0.6 |
| 1980–1994 | 3 | 3 | 37.5 | 1980–1994 | 3 | 4 | 3.7 |
| 1995–2004 | 9 | 11 | 42.6 | 1995–2004 | 8 | 13 | 11.0 |
| 2005–2015 | 10 | 14 | 31.2 | 2005–2015 | 8 | 18 | 15.0 |
| All Africa | 54 | 311 | 19.7 | Southern Africa (5) | |||
| 1960–1979 | 10 | 10 | 11.1 | 1960–1979 | 1 | 1 | 3.4 |
| 1980–1994 | 40 | 69 | 14.3 | 1980–1994 | 5 | 7 | 27.7 |
| 1995–2004 | 51 | 100 | 20.1 | 1995–2004 | 5 | 11 | 41.4 |
| 2005–2015 | 51 | 132 | 25.1 | 2005–2015 | 4 | 8 | 54.3 |
Source: United Nations World Contraceptive Use 2015
Modern contraceptive prevalence averages are unweighted.
Figure 1a.
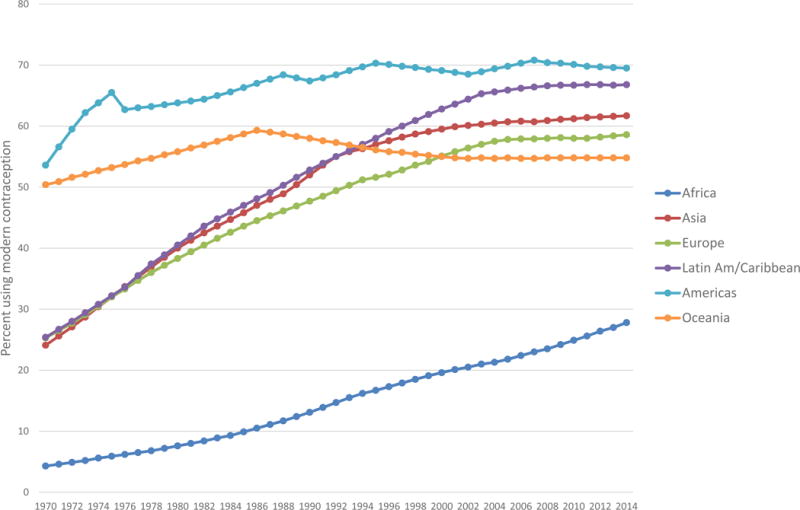
Modern Contraceptive Prevalence (%) among Married Women 15–49 Years by World Region and Year
Source: UN Model-Based Estimates 2015 for World Regions
There is internal heterogeneity in each major region in terms of sub-regional mCPRs, and Africa is no exception. Figure 1b shows the large difference in average mCPR levels in Southern Africa (based on five countries–Botswana, Lesotho, Namibia, South Africa and Swaziland). Its average mCPR for 2005–2015 is 54.3%, with the next highest of 41.5% found for six Northern African countries (Algeria, Egypt, Libya, Morocco, Sudan, and Tunisia). Both averages are substantially greater than the average of 27.2% for 18 Eastern African countries in this same period. West and Middle African countries, with 16 and 9 countries respectively, have equally low average mCPRs, around 15%, about 12% points lower than the East Africa average. Compared to average mCPRs from surveys for countries in these regions before 1980, modern contraceptive prevalence among married women has risen decidedly. The trend lines are uniformly upward with annual gains greatest in northern and Southern Africa sub-regions but steadily climbing in the other three regions.
Figure 1b.
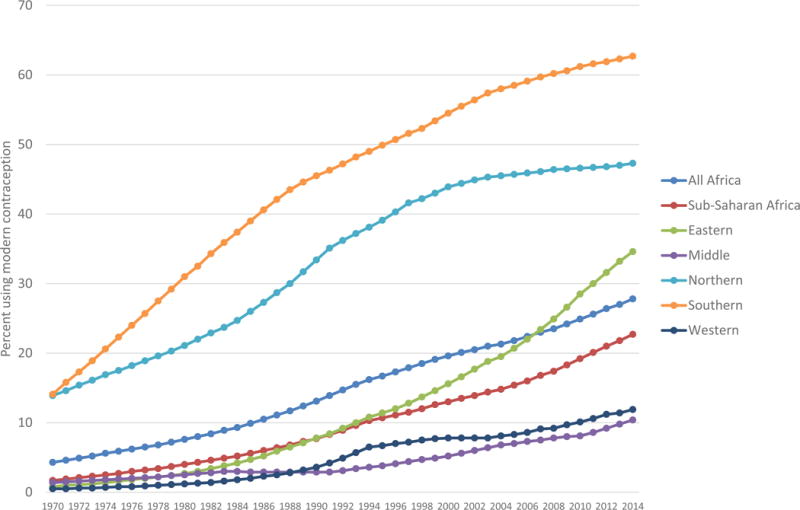
Modern Contraceptive Prevalence (%) among Married Women 15–49 Years for Africa and Its Sub-Regions by Year
Source: UN Model-Based Estimates 2015 for World Regions
We discuss next two distinctive patterns of individual contraceptive use in SSA countries, the first being higher levels of modern use by unmarried sexually active than married females and the second, the predominant use of injectables, more recently augmented by implants.
Modern contraceptive prevalence rates have been denominated traditionally against women in childbearing ages of 15 to 49 years who are currently married or in-union. Early national surveys tended to select only ever married women of reproductive age from sampled households, while reporting mCPR levels for married (and in-union) women. Recent DHS and other national surveys, particularly those conducted in Sub-Saharan Africa have included all women of reproductive age, leading researchers to recognize that contraceptive use among sexually active unmarried women age 15–49 in the SSA countries is often higher than among those currently married (Blanc et al., 2009; Prata et al., 2013). This pattern is not observed in early Latin American or Asian surveys, where unmarried females reported very little sexual activity, and thus even less contraceptive use.
Table 2 provides survey estimates for current use of modern methods among unmarried females reporting to be sexually active (SAU) and currently married (CM) females are provided for six countries with at least 5 survey rounds–Ghana (1988–2014), Mali (1987–2012), Kenya (1989–2014), Tanzania (1991–2010), Uganda (1988–2011), and Zimbabwe (1988–2011). Each has nearly a 20-year interval between the first and last survey and cover all SSA regions, except the central one.
Table 2.
Percent of females 15–49 years who are unmarried and sexually active (SAU), percent currently using a modern method among SAU, currently married (CM), and all women, % SAU and CM women using LARC: Selected Sub-Saharan African countries and DHS round
| Region/Country | Survey year | % all women who are unmarried and sexually active | % unmarried sexually active women using any method | % using modern methods
|
|||
|---|---|---|---|---|---|---|---|
| Sexually active unmarried (SAU) | Currently married (CM) | All women | Ratio SAU:CM | ||||
| West Ghana |
1988 | 5.5 | 28.3 | 6.5 | 4.2 | 3.7 | 1.55 |
| 1993 | 8.0 | 38.5 | 19.0 | 10.1 | 9.3 | 1.88 | |
| 1998 | 4.9 | 37.0 | 20.3 | 13.3 | 10.7 | 1.53 | |
| 2003 | 4.5 | 43.4 | 31.6 | 18.7 | 15.3 | 1.69 | |
| 2008 | 5.8 | 50.4 | 33.8 | 16.6 | 13.5 | 2.04 | |
| 2014 | 7.8 | 44.5 | 31.7 | 22.2 | 26.7 | 1.43 | |
| West Mali |
1987 | 0.4 | 20.2 | 8.3 | 1.3 | 1.2 | 6.38 |
| 1995 | 2.5 | 42.2 | 27.3 | 4.5 | 5.0 | 6.07 | |
| 2001 | 2.4 | 32.0 | 22.0 | 5.7 | 5.8 | 3.86 | |
| 2006 | 0.8 | 27.2 | 22.2 | 6.9 | 6.2 | 3.22 | |
| 2012 | 1.9 | 34.0 | 33.5 | 9.9 | 9.6 | 3.38 | |
| East Kenya |
1989 | 4.7 | 35.5 | 23.5 | 17.9 | 14.7 | 1.31 |
| 1993 | 6.0 | 40.0 | 30.3 | 27.3 | 20.7 | 1.11 | |
| 1998 | 5.5 | 46.5 | 36.2 | 31.5 | 23.6 | 1.15 | |
| 2003 | 3.3 | 54.4 | 44.3 | 31.5 | 22.7 | 1.41 | |
| 2008 | 3.8 | 50.3 | 45.1 | 39.4 | 28.0 | 1.14 | |
| 2014 | 1.9 | 65.4 | 60.9 | 53.2 | 39.1 | 1.14 | |
| East Tanzania |
1991 | 8.1 | 17.5 | 11.9 | 6.6 | 5.9 | 1.80 |
| 1996 | 8.3 | 26.2 | 21.4 | 13.3 | 11.7 | 1.61 | |
| 1999 | 9.1 | 33.0 | 26.1 | 16.9 | 15.6 | 1.54 | |
| 2004 | 6.3 | 40.5 | 35.7 | 20.0 | 17.6 | 1.79 | |
| 2010 | 7.3 | 50.6 | 44.7 | 27.4 | 23.6 | 1.63 | |
| 2015 | 7.0 | 54.1 | 45.8 | 32.0 | 27.1 | 1.43 | |
| East Uganda |
1988 | 6.0 | 14.7 | 7.4 | 2.5 | 2.7 | 2.96 |
| 1995 | 2.8 | 35.6 | 26.5 | 7.8 | 7.4 | 3.40 | |
| 2000 | 3.7 | 48.4 | 44.0 | 18.2 | 16.5 | 2.42 | |
| 2006 | 4.2 | 54.0 | 46.9 | 17.9 | 15.4 | 2.62 | |
| 2011 | 3.7 | 51.8 | 44.3 | 26.0 | 20.7 | 1.70 | |
| South Zimbabwe |
1988 | 6.4 | 44.0 | 40.7 | 36.1 | 27.2 | 1.13 |
| 1994 | 4.7 | 56.0 | 52.6 | 42.2 | 31.1 | 1.25 | |
| 1999 | 3.4 | 55.3 | 53.5 | 50.4 | 35.6 | 1.06 | |
| 2005 | 2.1 | 61.2 | 60.2 | 58.4 | 39.1 | 1.03 | |
| 2010 | 2.8 | 61.4 | 61.2 | 57.3 | 40.5 | 1.07 | |
Countries with 5 or more DHS rounds (1988–2013) selected
Longer acting, reversible (LARC) = implant, IUD, injectable
Source: StatCompiler, accessed on May 28, 2015; Kenya 2014 result from KDHS report
The empirical significance of including all women in the national survey samples is illustrated in Figure 2–modern contraceptive use has risen fairly steadily among SAU and CM women in these countries. In all countries, modern method use among SAU females is higher than among CM ones. In Kenya and Zimbabwe, the level of CM women’s use has paralleled that for SAU women. Use among Ghanian, Ugandan and Zimbabwean SAU females appears to be levelling off. This likely reflects the growing selection of young females remaining in school and delaying sexual activity or marriage.
Figure 2.
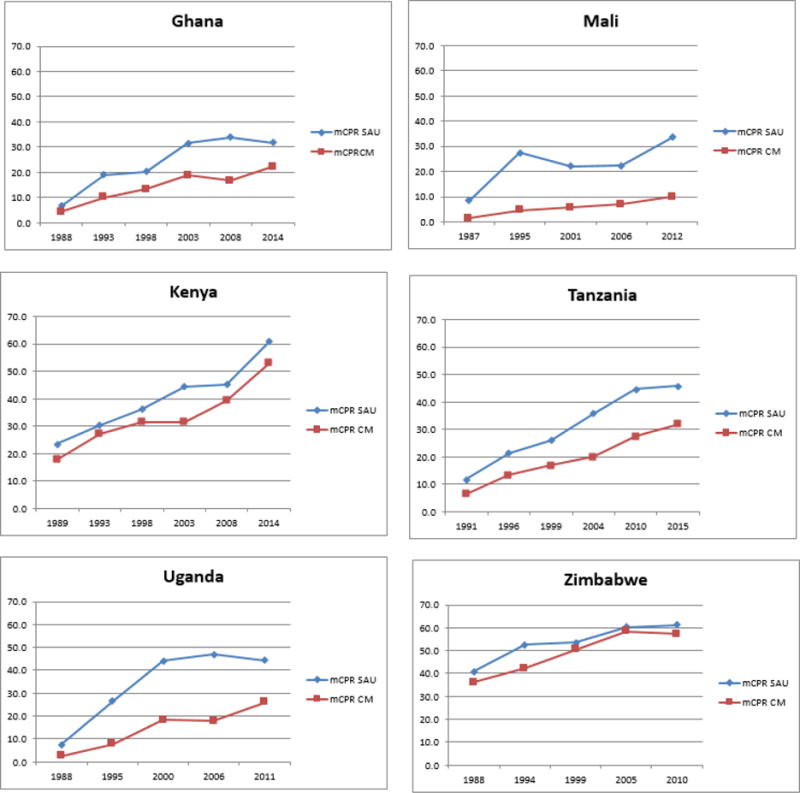
Percent of sexually active unmarried (SAU) and currently married (CM) women age 15–49 using modern contraception: Six selected countries with DHS data from 1987–2015
In a separate analysis (not shown here), the average mCPR for SAU, as compared to CM, women across 119 SSA surveys since 1985, was three times higher. In Table 2, one can see that ratio varying more widely across countries from 1.07 to 3.38 in the latest survey year and less within country. The selectivity of unmarried women self-reporting being sexually active is seen in column 2 and their intentions to avoid pregnancy with any method in column 3. The increasing convergence between use of any and use of a modern method, over time is found comparing columns 3 and 4. One interpretation of these patterns is that higher use of modern contraception by SAU than CM women signals a shift in fertility planning, from preventing unplanned pregnancies—and their social complications in the non-marital state–to having desired pregnancies within a marital context.
Table 3 draws on data from the PMA2020 surveys as well as the DHS, providing almost annual tracking of national or subnational patterns of use by main modern method for 2008–2016. PMA surveys adopt a multi-stage cluster design for sampling households and eligible women. They began in 2014 and are conducted annually although in the first two years a semi-annual cadence was followed (hence some survey years have a “B” suffix). As seen in Figure 3, mCPR levels among married women have been rising (blue line) and injectables (green line) are the predominant method. Also shown is the trend in use of long-acting permanent methods (red line), i.e., sterilization, IUDs and implants, of which the latter figure most importantly. In the PMA settings, both sterilization and IUDs are seen to be nominally used, while implants are rising. For example in Ethiopia, injectable use among currently married women rose from 20.8% in the 2011 DHS to 25.4% in the 2014 PMA and has declined slightly to 24.1% in the 2016 PMA, while implants have risen from 3.4% to 9.0% between 2011 and 2016. It also appears that implants may be addressing contraceptive demand for limiting, as opposed to spacing, methods as across these survey settings, there is little degradation in injectable use even with rising implant use. The changing composition of contraceptive methods used by married SSA women, first with injectables and then with implants, is unique in the history of international family planning, where the narrative has centered on the use of IUDs, sterilization, and pills. It should be noted, however, that both injectables and implants have not been as accessible in the regions of Asia, Latin America and the Middle East as in SSA.
Table 3.
Recent trends in modern contraceptive prevalence for selected Sub-Saharan African countries and subnational areas: DHS and PMA2020, 2008–2016
| Country/Survey round | Sterilization | Implant | IUD | Injectable | Pill | Condom | Other modern | Total |
|---|---|---|---|---|---|---|---|---|
| Burkina Faso | ||||||||
| 2010 DHS | 0.2 | 3.4 | 0.3 | 6.2 | 3.2 | 1.6 | 0.1 | 15.0 |
| 2014 PMA | 0 | 8.2 | 0.3 | 6.8 | 2.5 | 0.0 | 0.3 | 18.0 |
| 2015 PMA | 0 | 7.9 | 0.9 | 7.6 | 2.6 | 0.7 | 0.3 | 20.1 |
| 2016 PMA | 0 | 10.9 | 0.5 | 8.8 | 2.8 | 1.0 | 0.2 | 24.2 |
| DR Congo/Kinshasa | ||||||||
| 2007 DHS | 0.8 | 2.4 | 0.5 | 3.4 | 3.0 | 6.9 | 2.0 | 19.0 |
| 2013 PMA | 0.5 | 1.6 | 0.4 | 4.2 | 2.9 | 7.6 | 1.3 | 18.5 |
| 2014 PMA | 0.3 | 5.0 | 0.7 | 3.7 | 3.0 | 6.2 | 1.4 | 20.4 |
| 2015 PMA | 0.7 | 3.7 | 0.8 | 3.3 | 2.8 | 7.1 | 2.1 | 20.4 |
| 2015B PMA | 0.8 | 6.8 | 0.4 | 4.0 | 4.1 | 7.0 | 0.8 | 23.8 |
| Ethiopia | ||||||||
| 2011 DHS | 0.5 | 3.4 | 0.3 | 20.8 | 2.1 | 0.2 | 0.0 | 27.3 |
| 2014 PMA | 0.1 | 5.4 | 0.6 | 25.4 | 2.0 | 0.2 | 0.1 | 33.8 |
| 2014B PMA | 0.3 | 7.2 | 0.7 | 23.8 | 1.6 | 0.2 | 0.4 | 34.2 |
| 2015 PMA | 0.4 | 7.5 | 0.9 | 24.5 | 2.0 | 0.2 | 0.2 | 35.8 |
| 2016 PMA | 0.3 | 9.0 | 0.7 | 24.1 | 2.8 | 0.2 | 0.2 | 37.3 |
| Niger/Niamey | ||||||||
| 2012 DHS | 0.8 | 1.0 | 0.5 | 3.4 | 20.4 | 0.2 | 5.5 | 31.8 |
| 2015 PMA | 0.3 | 4.4 | 1.5 | 4.9 | 17.2 | 0.0 | 0.4 | 28.6 |
| 2016 PMA | 0.3 | 5.1 | 1.1 | 4.9 | 16.3 | 0.0 | 0.1 | 27.8 |
| Niger | ||||||||
| 2012 DHS | 0.1 | 0.3 | 0.1 | 2.1 | 5.6 | 0.0 | 3.9 | 12.2 |
| 2016 PMA | 0.2 | 1.7 | 0.4 | 5.0 | 6.8 | 0.2 | 0.1 | 14.4 |
| Nigeria/Kaduna | ||||||||
| 2013 DHS | 1.0 | 2.6 | 1.2 | 9.0 | 2.1 | 0.8 | 1.7 | 18.5 |
| 2014 PMA | 0.1 | 1.7 | 0.4 | 5.6 | 2.0 | 0.2 | 0.3 | 10.1 |
| 2015 PMA | 0.5 | 4.2 | 0.3 | 7.1 | 1.9 | 0.8 | 0.2 | 15.0 |
| 2016 PMA | 0.4 | 5.1 | 0.3 | 7.3 | 2.3 | 0.4 | 0.4 | 16.1 |
| Nigeria/Lagos | ||||||||
| 2013 DHS | 0.1 | 0.3 | 2.4 | 4.6 | 6.5 | 10.3 | 2.1 | 26.4 |
| 2014 PMA | 0.0 | 0.5 | 1.4 | 4.9 | 5.8 | 5.6 | 1.1 | 19.3 |
| 2015 PMA | 1.1 | 1.8 | 3.4 | 6.2 | 5.5 | 8.8 | 1.5 | 28.4 |
| 2016 PMA | 0.4 | 1.5 | 2.1 | 4.5 | 4.5 | 7.7 | 2.2 | 22.9 |
| Ghana | ||||||||
| 2008 DHS | 1.6 | 0.9 | 0.2 | 6.2 | 4.7 | 2.5 | 0.5 | 16.6 |
| 2013 PMA | 0.6 | 2.9 | 0.6 | 7.6 | 4.8 | 0.9 | 0.9 | 18.4 |
| 2014 PMA | 0.4 | 3.2 | 0.4 | 7.3 | 4.3 | 0.8 | 1.4 | 17.8 |
| 2014B PMA | 0.7 | 3.7 | 0.4 | 8.3 | 4.0 | 1.3 | 3.1 | 21.4 |
| 2014 DHS | 1.9 | 5.2 | 0.8 | 8.0 | 4.7 | 1.2 | 0.3 | 22.2 |
| 2015 PMA | 0.8 | 5.5 | 0.7 | 12.9 | 4.6 | 1.8 | 2.9 | 29.2 |
| Uganda | ||||||||
| 2011 DHS | 3.0 | 2.7 | 0.5 | 14.0 | 2.9 | 2.7 | 0.2 | 26.0 |
| 2014 PMA | 1.9 | 3.3 | 0.8 | 15.0 | 2.1 | 1.9 | 0.7 | 25.6 |
| 2015 PMA | 2.6 | 4.9 | 1.2 | 16.3 | 2.1 | 3.2 | 1.4 | 31.8 |
| 2015B PMA | 1.7 | 4.9 | 0.4 | 16.7 | 2.4 | 2.9 | 1.0 | 30.0 |
| 2016 PMA | 2.8 | 5.0 | 0.8 | 18.2 | 2.5 | 2.1 | 0.9 | 32.2 |
| Kenya | ||||||||
| 2008 DHS | 4.8 | 1.9 | 1.6 | 21.6 | 7.2 | 1.8 | 0.5 | 39.4 |
| 2014 PMA | 1.6 | 11.1 | 3.4 | 29.1 | 7.3 | 1.8 | 1.1 | 55.4 |
| 2014B PMA | 3.0 | 10.8 | 3.5 | 28.1 | 8.6 | 1.9 | 1.6 | 57.5 |
| 2014 DHS | 3.2 | 9.9 | 3.4 | 26.4 | 8.0 | 2.2 | 0.1 | 53.2 |
| 2015 PMA | 2.6 | 13.7 | 4.0 | 28.1 | 9.1 | 1.7 | 0.8 | 59.9 |
| 2016 PMA | 2.8 | 16.1 | 4.8 | 29.2 | 7.5 | 1.3 | 1.5 | 63.1 |
Prevalence of modern method currently used among married women 15–49 years
Figure 3.
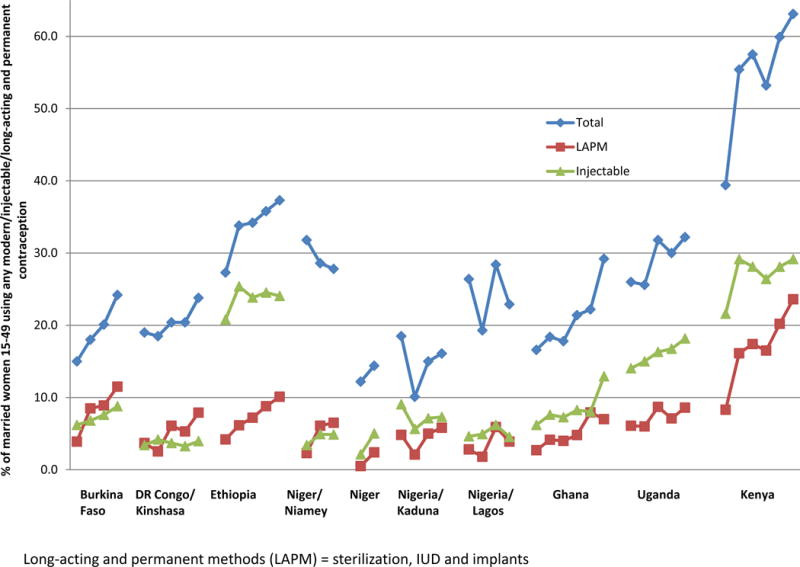
Recent trends in modern contraceptive prevalence, injectable and long-acting method use for selected Sub-Saharan African countries and subnational areas: 2008–2016 PMA2020 and DHS surveys
Long-acting and permanent methods (LAPM) = sterilization, IUD and implants
Mention should be of other geographic concentrations of specific method use. For example, there is a high prevalence of male condom use in countries in the Southern Africa region where HIV prevalence is also high. Condoms have been made available in large volume through HIV prevention programs such that more than 10% of CM women in countries such as Botswana, Namibia, Swaziland, the Congo and DR Congo, with high HIV prevalence report condom use. Not shown here, but from reviewing all 119 SSA surveys, it is apparent that neither female nor male sterilization is commonly used by CM women except in a few countries, e.g., South Africa, Malawi, and Zimbabwe. In the latter country, sterilization’s prevalence has increased significantly being the method used by more than two fifths of all CM women (41.5%). Substantial use of traditional method use, such as rhythm and withdrawal, is found among CM women in countries of the Central African region–Cameroon, Central African Republic, Congo and Democratic Republic of Congo (DRC) and Gabon–as well as in Madagascar, Ghana and Togo, where little use of modern methods exists.
There is evidence then of considerable heterogeneity in married and unmarried women’s experiences with non-artificial to permanent methods in the SSA region. In addition the spatial-temporal pace of diffusion of contraceptive innovation is on that rising and spreading.
Programmatic issues
Cross-national assessments of the strength of organized family planning effort have uniformly shown the level in SSA countries lags behind those of other developing ones (e.g., Ross and Mauldin, 1996; Ross et al., 2007; Ross and Smith 2011). The technical capacity of trained health personnel in SSA health systems has been vulnerable to better employment opportunities through immigration, creating brain drains with serious implications for health care in such countries as Ghana, Ethiopia and Malawi. The paucity of trained clinicians has left many health centers, especially those designed to deliver primary care, under-staffed. Along with limited resources for medical equipment and commodities, weak supply chain management can also create stock-outs which can in turn disrupt individual contraceptive protection. Public health facilities in many SSA countries have been unable to provide services at desired standards of quality to clients, particularly those residing in rural and economically poor areas (Bosch-Capblanch, Liaqat and Garner, 2011).
In the 1980s available contraceptive methods were primarily the pill and condom, to which was added in the mid-1990s, the hormonal injectable of depot medroxyprogesterone (Depo-Provera). The DMPA injectable has become the most popular method of contraception in SSA, representing nearly half (47%) of all modern method use (United Nations, 2016b). The US Food and Drug Administration did not approve the drug until 1992 preventing it from being supplied prior to that time through bilateral assistance channels. Additionally, the reticence of political leaders of SSA governments, particularly in the Francophone region, to openly support family planning persisted through to the mid-2000s (Shiffman and Quissell, 2012; Blanc and Tsui, 2005). As a consequence, until very recently, there was limited recognition by SSA governments of family planning as a priority investment for improving reproductive and family health.
To provide injectables to nearly half of women contracepting in SSA countries, the introduction of this method and the implant has involved considerable international assistance and support for training of providers, commodity acquisition and management of supply chains. Backed up by an expanding number of country-level social marketing programs, injectables are accessible now through private clinics and pharmacies and community-based health workers, as well as public health facilities, in many countries (Hoke et al., 2012). A new presentation of the three-month injectable in the Uniject™ system will enable access in isolated areas through community health workers. Called Sayana Press (SP), the small, lightweight injection system, which costs $1 per unit, more than a clinic injection, has been successfully tested for use by health providers in Senegal, Uganda, Burkina Faso and Niger. SP was approved in 2015 for use by self-injection in the UK and testing is underway of this modality in Senegal and Uganda. Social marketing of SP has been launched in a number of countries, e.g., Nigeria, Democratic Republic of Congo, and Burkina Faso. As more countries approve SP’s delivery by community health providers and self-injection, the method will likely scale up contraceptive access rapidly in SSA given the exceptional popularity of injectables.
In the landscape of donors contributing resources at scale to expand contraceptive access in Sub-Saharan Africa, a recent new entry is the Bill & Melinda Gates Foundation. Working with several bilateral donors, the Foundation entered into a 2013 public-private partnership with two large pharmaceutical companies, Bayer and Merck/MSD, for a volume guarantee of implant purchase. This covered both the single-rod Implanon and the two-rod Jadelle and halved the unit price to $8.50. The UN Commission on Life-Saving Commodities for Women and Children also endorsed the contraceptive implant as one of its 13 life-saving commodities. With improved affordability since 2013, the prevalence of implants has risen dramatically in a number of SSA countries as noted earlier. With a 3 to 5-year protection period, or until removal, this method will maintain contraceptive protection for the user and boost prevalence levels over time without loss to discontinuation.
Several important program delivery issues and approaches confronting family planning programs in SSA bear further discussion – high contraceptive discontinuation rates, postpartum delivery of contraception, community-based delivery of contraception, and resource competition with HIV programs. Others that are also important but not addressable in this paper include the role of the private sector, particularly social marketing, and demand generation through public messaging about family planning and contraception.
Contraceptive discontinuation
Disrupted contraceptive use, when unintended and unresolved, is problematic. In large part because the use of short-term methods has prevailed, rates of contraceptive discontinuation are high (Bradley et al., 2009; Ali and Cleland 2010). We obtained national estimates of 12-month discontinuation rates and reasons for discontinuation available through StatCompiler, as presented in Table 4. These data required that surveys included the version of the contraceptive calendar6 that captured the reason for termination at the end of each episode of use. Few SSA country surveys included this calendar version more than once, the exceptions being Kenya and Zimbabwe. As seen in Table 4, the latest estimates of first-year discontinuation rates for any method are 20% or below in Comoros and Namibia, and Zimbabwe from 1994 to 2005. However, they exceed 40% in Liberia, Mali, Senegal, Burundi, Ethiopia, and Uganda. Method failure rates range from 0.6% (Niger) to 6.3% (Uganda) in the first year and are within the expected range of contraceptive use-effectiveness under typical use conditions. Discontinuation rates to become pregnant (see Table 4) range from 2.1% (Namibia) to 18.0% (Niger) and may reflect personal efficacy in using birth control. Of concern then is stopping because of side effects or health and other reasons, these rates being as high as 16.1% in Uganda in 2011 or 15.3% in Senegal in 2010.
Table 4.
First-year contraceptive discontinuation rates due to method failure, desire for pregnancy, health reasons, or other reasons: 20 DHS countries in SSA and survey rounds
| Country | Survey | 12-month discontinuation rates
|
Total | |||
|---|---|---|---|---|---|---|
| Method failure | To become pregnant | Side effects, health reasons | All other reasons | |||
| Benin | 2011 | 3.0 | 7.8 | 6.2 | 21.6 | 38.6 |
| Burkina Faso | 2010 | 1.5 | 6.7 | 5.2 | 6.6 | 20.0 |
| Liberia | 2013 | 2.1 | 2.7 | 13.1 | 7.0 | 25.0 |
| Mali | 2012 | 4.7 | 13.7 | 10.3 | 15.6 | 44.3 |
| Niger | 2012 | 0.6 | 18.0 | 4.4 | 22.5 | 45.4 |
| Nigeria | 2013 | 3.9 | 8.6 | 2.3 | 7.5 | 22.3 |
| Senegal | 2010 | 3.5 | 7.8 | 15.3 | 22.4 | 49.1 |
| Sierra Leone | 2013 | 1.8 | 4.1 | 11.0 | 5.9 | 22.8 |
| Burundi | 2010 | 5.5 | 9.0 | 10.7 | 15.5 | 40.8 |
| Comoros | 2012 | 2.3 | 4.3 | 4.8 | 7.0 | 18.4 |
| Ethiopia | 2005 | 1.4 | 10.4 | 14.5 | 15.7 | 42.0 |
|
| ||||||
| Kenya | 1998 | 5.0 | 4.6 | 8.5 | 14.5 | 32.6 |
| 2003 | 5.5 | 5.0 | 12.8 | 14.4 | 37.6 | |
| 2014 | 3.0 | 4.7 | 10.5 | 24.1 | 30.5 | |
|
| ||||||
| Malawi | 2004 | 3.4 | 8.4 | 10.5 | 13.5 | 35.8 |
| Mozambique | 2011 | 2.3 | 11.0 | 11.7 | 20.7 | 45.7 |
| Rwanda | 2010 | 3.1 | 2.7 | 11.0 | 9.5 | 26.3 |
| Tanzania | 2004 | 3.9 | 8.4 | 11.6 | 13.9 | 37.8 |
| Uganda | 2011 | 6.3 | 7.4 | 16.1 | 13.1 | 43.0 |
| Zambia | 2013 | 3.1 | 5.6 | 7.6 | 10.5 | 26.8 |
|
| ||||||
| Zimbabwe | 1994 | 3.3 | 4.8 | 3.6 | 7.8 | 19.5 |
| 1999 | 1.8 | 3.8 | 5.1 | 9.6 | 20.2 | |
| 2005 | 2.2 | 4.4 | 3.9 | 9.7 | 20.2 | |
| 2010 | 2.4 | 5.6 | 5.9 | 10.0 | 23.9 | |
|
| ||||||
| Namibia | 2013 | 1.8 | 2.1 | 6.0 | 9.2 | 19.1 |
Among women 15–49 years who started an episode of contraceptive use within five years preceding the survey, percent of episodes discontinued within 12 months, by main reason (method failure, desire for pregnancy, health reasons, or other)
Other reasons include want more effective method, lack of access, costs too much, inconvenient to use, infrequent sex/husband away, difficult to get pregnant/menopausal, marital dissolution/separation,.
An analysis of reasons for stopping use in this period (not shown here) indicates that nearly half of use episodes (45%) end for preventable reasons. Contraceptives are being used to space births (with a weighted average 33% of episodes ending for a desired pregnancy). The prevalence of accidental pregnancies (averaging 11%) is not ideal and one fifth of episodes ended for health reasons or concerns about side effects. Strengthening contraceptive information, education and counseling services seems implicit as is providing long-acting contraception to enhance use-effectiveness.
Postpartum delivery of contraception
In an effort to meet women’s contraceptive needs early after childbearing, a number of countries are beginning to offer family planning in the immediate postpartum period, especially if the mother delivers in a health facility as opposed to at home. We carried out a survival analysis with DHS calendar data from six countries, four in SSA with 1 in Latin America (Bolivia) and 1 in Asia (Indonesia) for comparison purposes. The calendar records pregnancies, births, and contraceptive events over a five or six year period and allows for the alignment of the date of a recent birth with the month of postpartum contraceptive adoption. The cumulative proportions of recent births, where mothers adopted a modern contraceptive method up to 3, 6, 12 and 24 months after birth, are shown in Table 5 and Figure 4. The percent of births in the five to six years prior to the survey occurring in facilities ranges from 10% in Ethiopia to 68% in Zambia. In Ethiopia, Zambia and Kenya, there is an appreciably higher cumulative proportion of mothers who delivered in facilities having adopted a modern method by the third month after birth, as compared to mothers delivering at home. For example in Kenya the difference is nearly double, with 12.4% of mothers delivering at home adopting by month 3 as compared to 24.4% of mothers delivering in facilities. Figure 4 shows that adoption of a modern contraceptive method up to 24 months postpartum remains higher for mothers with facility- than home-based deliveries in all countries, exception Indonesia. Indonesia’s pattern is interesting given that home and facility-based deliveries are equally frequent and that modern contraceptive use is high at 57.9% among married women.
Table 5.
Survival Analysis of DHS Calendar Data to Estimate Postpartum Modern Contraception Adoption Rates by 3, 6, 12 and 24 months by place of delivery for 6 countries
| Country and survey year | mCPR % | Place of delivery | Births
|
PPFP cumulative adoption rate
|
||||
|---|---|---|---|---|---|---|---|---|
| Number | % facility | 3 months | 6 months | 12 months | 24 months | |||
| Ethiopia 2011 | 27.3 | Home | 10202 | 90.0 | 4.8 | 9.3 | 14 | 25.4 |
| Facility | 1129 | 10.0 | 30.2 | 43.5 | 52.3 | 61.5 | ||
| Zambia 2013–14 | 44.8 | Home | 4155 | 31.8 | 5.0 | 13.1 | 23.2 | 39 |
| Facility | 8929 | 68.2 | 12.7 | 27.4 | 42.1 | 57.9 | ||
| Burkina Faso 2010 | 15.0 | Home | 4908 | 33.4 | 0.4 | 1.7 | 3.1 | 6.4 |
| Facility | 9771 | 66.6 | 2.4 | 7.1 | 12.2 | 21.5 | ||
| Kenya 2014 | 53.2 | Home | 3797 | 38.6 | 12.4 | 22.8 | 31.3 | 41.4 |
| Facility | 6037 | 61.4 | 24.4 | 44.1 | 58.5 | 67.6 | ||
| Bolivia 2008 | 34.6 | Home | 2743 | 32.3 | 1.2 | 3.5 | 9.5 | 18.4 |
| Facility | 5761 | 67.7 | 12.9 | 21.8 | 33.8 | 45.2 | ||
| Indonesia 2012 | 57.9 | Home | 7269 | 51.6 | 43.9 | 65.3 | 71.4 | 76.4 |
| Facility | 6822 | 48.4 | 47.5 | 67.7 | 73.9 | 77.5 | ||
mCPR=Modern contraceptive prevalence among married women 15–49
Figure 4.
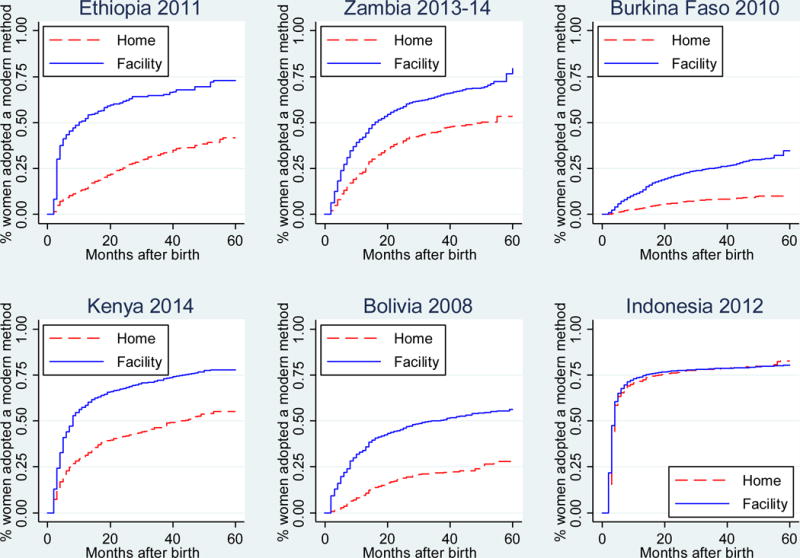
Postpartum modern contraceptive adoption: Cumulative proportions of mothers at 3, 6, 12 and 24 months by place of delivery for six countries
Source: Calculated using DHS calendar data
In terms of reducing the risk of an unplanned pregnancy shortly after birth, postpartum adoption of a modern contraceptive method that does not affect the benefits of breastfeeding is an effective option. The afforded contraceptive protection will overlap with the post-partum infecundability conferred by breastfeeding, especially when practiced exclusively for six months, and any practice of postpartum sexual abstinence. However, the safety of immediate provision of long acting reversible contraceptives, such as the IUD and implant, to postpartum mothers has been endorsed by the World Health Organization7 and the American College of Obstetricians and Gynecologists8. Furthermore, counseling of all method options and assurance of choice is also advised at all stages of pregnancy and delivery care. Cleland et al. (2015) have questioned the need for vigorous programmatic provision of postpartum contraception in some settings and where prolonged breastfeeding exists. They stress the importance of informing women and mothers of contraceptive options and enabling their choice of the timing of any adoption.
Community-based delivery of contraception information and services
Efforts to de-medicalize contraceptive delivery and move services out of clinical settings have been a part of national family planning programs globally. In the SSA region, in the mid-1980s to 1990s, household delivery of pills and condoms by local health volunteers with basic training was prominent in several countries (Zimbabwe, Kenya and Ghana, for example). This approach was enhanced with better trained (and paid) community workers, who are now able to administer contraceptive injections at the community level, if not the household. Further task-shifting emerged with the permitted insertion of contraceptive implants by community health workers. In part as a response to constrained clinical infrastructures, SSA health programs have implemented the model of community-based distribution extensively, where a wide range of short and long-term contraceptive methods being delivered by a diverse range of local trained health workers. Successful community health worker models operate in Ethiopia, Ghana, Rwanda, Malawi, and Zimbabwe and their effectiveness in providing family planning services have been systematically assessed (Scott et al., 2015).
As an indication of the effort to reach and deliver information through household visits, Figure 4 presents the proportion of non-contracepting women reporting a household visit in the past year by a health worker who discussed family planning. Across the 32 SSA countries with this information, the percent of non-users reached ranges from 2.2% in Tanzania to 23.8% in Sierra Leone, with an average of 8%. Given the relatively modest levels of contraceptive use, the percentages not using will be large and thus the effort for community outreach non-trivial. This significant effort also represents that expended above and beyond the current public and private clinical infrastructure to increase contraceptive access.
Competing health concerns: HIV/AIDS and other disease epidemics
Although the spread of the HIV epidemic was significant in several Asian countries, such as Thailand, Vietnam and Cambodia, national adult prevalence levels at their peaks, such as for Thailand at 1.8% in 2001, never reached those found in countries in southern and eastern Africa regions (e.g., South Africa, Malawi, Swaziland, Botswana, Zambia, Zimbabwe, Tanzania, Uganda and Kenya). The highest levels are estimated to be over 25% of adults in Botswana and Swaziland9. In SSA, heterosexual transmission of HIV is the main mode of transmission in affected SSA countries, whereas injecting drug use and men having sex with men have been more predominant for Asian countries. As a result, the SSA experience with controlling the HIV epidemic, aided by unprecedented levels of global attention and assistance, is unique among developing regions.
From the perspective of overlapping demographics, the African HIV crisis has had the unique impact of immediately focusing attention on populations of risk–the sexual behavior and mobility of men as sources of infection, followed by women as wives, sex workers, sexually active adolescents, couples, infants of HIV-infected mothers and orphaned and vulnerable children. The treatment model of pre-exposure prophylaxis, as a daily combination of anti-retroviral medication taken to reduce HIV acquisition by a person at substantial risk, is at its core couple-oriented. The acquisition of HIV infection at earlier ages by young females from older male partners in a number of southern and eastern African countries has furthered attention on levels of adolescent sexual activity and the pernicious effects of poverty. The AIDS epidemic in SSA has produced one distinct benefit for family planning, that of liberalizing popular discussion around sexuality, partnering and frequency and types of sexual activity.
How much the epidemic’s evolution should have influenced rates of contraceptive use, both through health service delivery and sexual risk patterns, has been debated in various quarters (e.g., Shiffman 2008; Wilcher et al., 2009). The disproportionate volume of resources allocated to HIV treatment and care, compared to contraceptive access and delivery and other primary care services, suggests distortion of health systems performance in HIV-prevalent settings and SSA overall (Grépin, 2012; Lordan et al., 2011; Biesma et al., 2009). While study findings have been mixed (e.g., Afnan-Holmes et al., 2015; Kruk et al., 2012; Mwapasa and Kadzandira, 2009), there is a growing consensus that the rising tide of HIV funding has lifted all boats. That is, the size of HIV/AIDS funding has impacted the delivery of other types of health services, such as maternal and child health, malaria and tuberculosis, but eventually in a positive direction. For example, Grépin (2013) finds child immunizations in SSA from 2003–2010 to have been compromised but prenatal blood testing to have increased. Kruk et al. (2012) finds higher maternal deliveries with increased HIV care and investments in eight African countries between 2007 and 2011. Studies of the direct impact of HIV programs on contraceptive delivery in SSA countries though are few and may reflect the latter’s exclusion or absence of integration into HIV care. There has been a shift of late toward recognizing contraceptive care’s relevance for HIV-infected women to reduce their risk of unintended pregnancies and vertical transmission of HIV to newborns (Wilcher et al., 2013; Reynolds et al., 2008).
A second area of debate relates to the potential impact of hormonal contraceptive use, including the injectable, on HIV acquisition by women and disease progression (Polis et al., 2016; Heffron et al., 2012; Polis et al., 2014; Butler et al, 2016). While the epidemiologic evidence largely remains equivocal, the concern of elevated risk has challenged the two professional communities of researchers, advocates and donors to balance access to the popular injectable against the drive to lower disease incidence. Lost at times in the epidemiologic tracking of the dual burdens of HIV infections and unintended pregnancies is the comparatively lower probability of HIV acquisition per unprotected coital act estimated by Gray et al., 2001 at 1 per 1000 (0.001)10 versus the 3–5% for pregnancy from unprotected coitus (Tietze, 1960). In the near term, there is the promise of and hopes for the dual protective benefits of multipurpose prevention technologies (MPTs) currently under development and testing. MPTs involve adding an antiretroviral agent, such as dapivarine or tenofavir, and a contraceptive compound such as levonogestrel, to intravaginal rings or other barrier devices (Fernandez-Romero et al., 2015). MPTs are likely to be popular in high HIV-prevalent countries, such as South Africa, where IUDs and female condoms are already preferred methods.
Discussion
This paper has described past and recent trends in Sub-Saharan Africa’s patterns of contraceptive practice and methods used. The sub-region has 49 of the continent’s 54 sovereign governments and is characterized by substantial socio-cultural heterogeneity. Using data from DHS and PMA2020 survey rounds in 38 of the 49 countries, we observe the highest levels of modern method use among married women to be in countries in the Southern and Eastern African regions, and contraceptive uptake to have increased more quickly in Eastern relative to Western Africa. The youth demographic will be a key component of future change in contraceptive practice for at least three reasons: 1) high proportions of those under 25 are already sexually active; 2) a higher proportion of unmarried sexually active females are using modern contraception than those who are married; and 3) youth are today better attuned to means for avoiding pregnancy timed with coitus, using methods, such as condoms and emergency contraception, or post-conception with medication abortion.
Nearly half of contraceptors in the SSA region use injectables, a method choice that is the result of a range of individual, couple, community and programmatic factors. Per the United Nations (2016b), the injectable accounts for nearly one half (47%) of overall modern method use (19.7%) in Sub-Saharan Africa. The predominance of the one method is unique compared to other developing world regions, which have relied more on a combination of sterilization, IUDs and the pill. High rates of contraceptive discontinuation of short-term methods by users in SSA countries have, however, prompted expansion of access to longer-acting methods, most recently implants. To enable better birth spacing with effective contraception and improve maternal and child health, postpartum family planning is increasingly encouraged and delivered to mothers birthing in facilities, although assuring informed options and choice is a paramount consideration. The expanded implementation of community-based models for the distribution of information and services with lower-level health workers in SSA countries is yet another important program strategy. These nonclinical distribution systems have overcome many of the geographic, psychosocial, and financial barriers in delivering injectables and implants, along with pills and condoms, to isolated rural settings in the SSA region. Programmatic efforts along these lines and accompanying rapid rises in modern contraceptive practice, coupled with strong political support at the highest government levels, in Rwanda, Ethiopia and Malawi have led to these three countries being recognized as recent family planning successes.
The regional and national diversity of Sub-Saharan Africa in terms of its government commitment to family planning and strength of health systems to provide high-quality information, counseling and services is appreciable. Countries in the eastern, western and southern parts of the continent differ internally by language, religion and ethnicity and historically have had varying degrees of sustained exposure to western ideation that can have a modernizing influence. The structural and sociocultural heterogeneity in subcontinent of 48 nations may have constrained the kind of socio-cultural diffusion of fertility regulation ideas and practices that has been observed in European countries. Colonial legacies, such as French anti-contraception laws from the last century, have reinforced pronatalist attitudes in Francophone Africa, while “liberated” thinking about female schooling may have flowed more freely in countries under British rule, such as Kenya, Ghana, or Zimbabwe.
Social structures in SSA countries are changing, and the region is rising economically. Despite the observed heterogeneity, today’s regional and sub-regional landscape shows growing evidence of the impact of the types of structural changes that customarily accompany socioeconomic development, urbanization, and normative change through mass media exposure and population movement. In particular, the establishment of linked mobile telecommunication networks throughout the region, in place of traditional trunk lines, and the rapid increase in cell and smart phone access, are accelerating the spread of information and ideas, especially among young people. This would include information on sexual and reproductive health, methods of contraception and abortion. Social change is also eroding traditional practices of postpartum abstinence, common in West Africa.
Expectations for sustained and robust economic growth are high and the projected growth in the region’s population is seen as a potential driver of global consumer demand. Foreign investment has been drawn into countries with politically stable and supportive governments, such as Kenya, Ghana, and Ethiopia. The improved infrastructure through large-scale investments by China also has expanded trade and market access with road and transportation systems and reliable access to electricity through dams and power grids. SSA countries’ considerable challenge will be the absorption of an enormously large population of youth into the labor force and into productive, paid employment without political destabilization. Prospects of a demographic dividend–the economic benefit of reducing youth dependency ratios and investing national savings in improving human capital quality and growing the economy—are extremely appealing today to African political leaders. Faced with the daunting need to create jobs for the so-called youth bulge, they have enthusiastically embraced the demographic dividend both as a development platform but also a policy option by which to legitimize increasing support for family planning. The macro-economic return on investment can be sizeable as seen in a macro-simulation for Nigeria (see Karra in this volume) but there is no guarantee the demographic dividend will be automatically realized (see Cleland and Machiyama’s review in this volume of potential obstacles).
As contraceptive practice becomes more democratized in SSA countries at the population level, with less economic inequality in availability and use, the role of international donor financing may gain importance through strategic and targeted allocations. The re-vitalization of family planning investments has benefited from advocacy efforts, such as the London Family Planning Summit to increase access to 120 million additional users by 2020 (Brown et al., 2014). Although the primary components of family planning programs may be in place in Sub-Saharan Africa, as they have been historically in other regions, a more rapid pace of growth in contraceptive practice to be observed in the next decade may make the SSA region’s experience unique.
Figure 5.
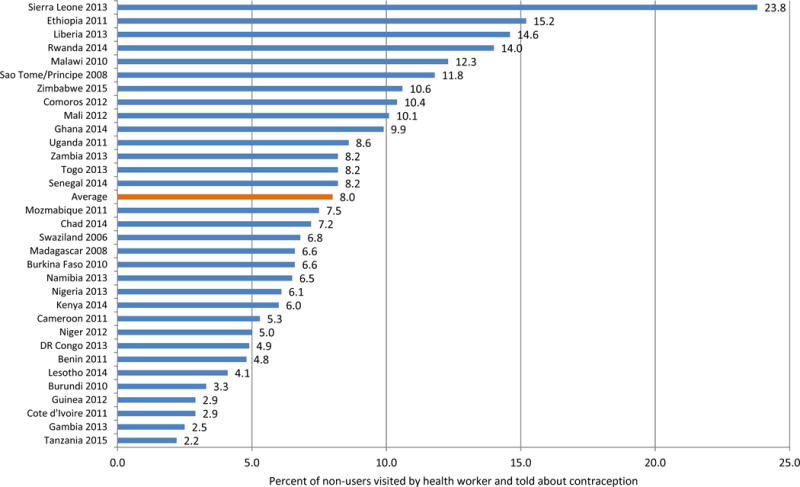
Percent of non-users of contraception visited by a health worker and told about contraception, in the 12 months before the survey: 32 Sub-Saharan African countries with DHS 2006–2015
Appendix
Figure 1.

Murdock Map of Ethnographic Regions of Africa
Source: Murdock (1959)
Footnotes
Western Sahara is a member of the African Union but its sovereignty status is contested by Morocco.
Reason for contraceptive discontinuation was often not included in the calendar in Phase VI of the DHS program.
http://www.who.int/reproductivehealth/publications/family_planning/SPR-3/en/ (Accessed January 28, 2017)
http://www.acog.org/Resources-And-Publications/Committee-Opinions/Committee-on-Obstetric-Practice/Immediate-Postpartum-Long-Acting-Reversible-Contraception (Accessed January 28, 2017)
CDC cites 8 per 10,000 exposures (0.0008) for receptive penile-vaginal intercourse; see http://www.cdc.gov/hiv/policies/law/risk.html
References
- Afnan-Holmes H, Magoma M, John T, Msemo G, et al. Tanzania’s Countdown to 2015: An analysis of two decades of progress and gaps for reproductive, maternal, newborn and child health to inform priorities for post-2015. Lancet Global Health. 2015;3(7):3396–409. doi: 10.1016/S2214-109X(15)00059-5. [DOI] [PubMed] [Google Scholar]
- African Development Bank, Organization of Economic, Cooperation and Development and UN Development Program. African Economic Outlook Report. 2016 https://www.afdb.org/en/knowledge/publications/african-economic-outlook/ Accessed January 27, 2016.
- Ali M, Cleland J. Contraceptive switching after method-related discontinuation: levels and differentials. Studies in Family Planning. 2010;41(2):129–33. doi: 10.1111/j.1728-4465.2010.00234.x. [DOI] [PubMed] [Google Scholar]
- Biesma RG, Brugha R, Harmer A, Waslh A, Spicer N, Walt G. The effects of global health initiatives on country health systems: A review of the evidence from HIV/AIDS control. Health Policy and Planning. 2009;24:239–252. doi: 10.1093/heapol/czp025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanc AK, Tsui AO. The dilemma of past success: Insiders’ views on the future of the international family planning movement. Studies in Family Planning. 2005;36(40):263–276. doi: 10.1111/j.1728-4465.2005.00069.x. [DOI] [PubMed] [Google Scholar]
- Blanc AK, Tsui AO, Croft TN, Trevitt JL. Patterns and trends in adolescents’ contraceptive use and discontinuation in developing countries and comparisons with adult women. International Family Planning Perspectives. 2009;35(20):63–71. doi: 10.1363/ipsrh.35.063.09. [DOI] [PubMed] [Google Scholar]
- Bongaarts J, Casterline J. Fertility transition: Is sub-Saharan Africa different? Population and Development Review. 2012;38(Supplement):153–168. doi: 10.1111/j.1728-4457.2013.00557.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosch-Capblanch X, Liaqat S, Garner P. Managerial supervision to improve primary health care in low- and middle-income countries. Cochrane Database Systematic Review. 2011;9:CD006413. doi: 10.1002/14651858.CD006413.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley SEK, Schwandt HM, Khan S. DHS Analytical Studies. 20. Calverton, MD: ICF Macro; 2009. Levels, trends and reasons for contraceptive discontinuation. [Google Scholar]
- Brown W, Druce N, Bunting J, Radloff S, Koroma D, Gupta S, Siems B, Kerrigan M, Kress D, Darmstadt GL. Developing the “120 by 20” goal for the Global FP2020 Initiative. Studies in Family Planning. 2014;45(1):73–84. doi: 10.1111/j.1728-4465.2014.00377.x. [DOI] [PubMed] [Google Scholar]
- Butler A, Smith JA, Polis CB, Gregson S, Stanton D, Hallett TB. Modelling the global competing risks of a potential interaction between injectable hormonal contraception and HIV risk. AIDS. 2013 Jan 2;27(1):105–113. doi: 10.1097/QAD.0b013e32835a5a52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell JC, Caldwell P. The cultural context of high fertility in sub-Saharan Africa. Population and Development Review. 13(3):409–437. [Google Scholar]
- Caldwell JC, Caldwell P. Africa: The new family planning frontier. Studies in Family Planning. 2002;33(1):76–86. doi: 10.1111/j.1728-4465.2002.00076.x. [DOI] [PubMed] [Google Scholar]
- Casterline J, El-Zeini L. Unmet need and fertility decline: A comparative perspective on prospects in Sub-Saharan Africa. Studies in Family Planning. 2014;45(2):227–245. doi: 10.1111/j.1728-4465.2014.00386.x. [DOI] [PubMed] [Google Scholar]
- Cleland J, Shah I, Benova L. A fresh look at the level of unmet need for family planning in the postpartum period, its causes and program implications. International Perspectives on Sexual and Reproductive Health. 2015;41(3):155–162. doi: 10.1363/4115515. [DOI] [PubMed] [Google Scholar]
- Fernandez-Romero J, Deal C, Herold B, Schiller J, Patton D, Zydowsky T, Romano J, Petro CD, Narasimhan M. Multipurpose prevention technologies: the future of HIV and STI protection. Cell. 2015 doi: 10.1016/j.tim.2015.02.006. Epub ahead of print: http://dx.doi.org/10.1016/j.tim.2015.02.006. [DOI] [PMC free article] [PubMed]
- Feyisetan B, Casterline J. Fertility preferences and contraceptive change in developing countries. International Family Planning Perspectives. 2000;26(30):100–109. [Google Scholar]
- Garenne MM. DHS Comparative Report No 18. Calverton, MD: Macro International Inc; Sep, 2008. Fertility changes in Sub-Saharan Africa. [Google Scholar]
- Garenne MM. DHS Analytic Studies No 42. Calverton, MD: Macro International Inc; Jan, 2014. Trends in Marriage and Contraception in Sub-Saharan Africa. [Google Scholar]
- Gray R, Wawer MJ, Brookmeyer R, Sewankambo NK, Serwadda D, Wabwire-Mangen F, Lutalo T, Li X, van Cott T, Quinn TC, Rakai Project Team Probability of HIV-1 transmission per coital act in monogamous, heterosexual HIV-1 discordant couples in Rakai, Uganda. Lanet. 2001;357(9263):1149–1153. doi: 10.1016/S0140-6736(00)04331-2. [DOI] [PubMed] [Google Scholar]
- Grépin KR. HIV donor funding has both boosted and curbed the delivery of different non-HIV health services in Sub-Saharan Africa. Health Affairs. 2012;31(7):1406–141. doi: 10.1377/hlthaff.2012.0279. [DOI] [PubMed] [Google Scholar]
- Heffron R, Donnell D, Rees H, Celum C, Mugo N, Were E, de Bruyn G, Nakku-Joloba E, Ngure K, Kiarie J, Coombs RW, Baeten JM, Partners in Prevention HSV/HIV Transmission Study Team Use of hormonal contraceptives and risk of HIV-1 transmission: a prospective cohort study. Lancet Infectious Disease. 2012;12(1):19–26. doi: 10.1016/S1473-3099(11)70247-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoke T, Brunie A, Krueger K, Driesbach C, Akol A, Rabenja NL, Olawo A, Stanback J. Community-based distribution of injectable contraceptives: Introduction strategies in four Sub-Saharan African countries. International Family Planning Perspectives. 2012;38(4):214–219. doi: 10.1363/3821412. [DOI] [PubMed] [Google Scholar]
- Johnson K, Abderrahim N, Rutstein SO. DHS Analytical Studies. 23. Calverton, MD: Macro International Inc; Sep, 2011. Changes in the direct and indirect determinants of fertility in Sub-Saharan Africa. [Google Scholar]
- Kruk ME, Jakubowski A, Rabkin M, Elul B, Friedman M, El-Sadr W. PEPFAR programs linked to more deliveries in health facilities by African women who are not infected with HIV. Health Affairs. 2012;31(7):1478–1488. doi: 10.1377/hlthaff.2012.0197. 2013. [DOI] [PubMed] [Google Scholar]
- Lesthaeghe R. Population Studies Center Research Reports. University of Michigan; Ann Arbor, Michigan: Jul, 2014. The fertility transition in Sub-Saharan Africa into the 21st century; pp. 14–823. [Google Scholar]
- Lordan G, Tang KK, Carmignani F. Has HIV/AIDS displaced other health funding priorities? Evidence from a new dataset of development aid for health. Social Science & Medicine. 2011;73:351–355. doi: 10.1016/j.socscimed.2011.05.045. [DOI] [PubMed] [Google Scholar]
- May JF. The politics of family planning policies and programs in Sub-Saharan Africa. Population and Development Review. 2016 doi: 10.1111/j.17284457.2016.00165.x. [DOI] [Google Scholar]
- Murdock G. Africa: Its Peoples and Their Culture History. New York: McGraw-Hill Book Co; 1959. [Google Scholar]
- Mwapasa V, Kadzandira J. Interactions between Global Health Initiatives and Health Systems. The Maximizing Positive Synergies Academic Consortium; Jun, 2009. Malawi: Global health initiatives and delivery of health care: the case of the Global Fund to Fight AIDS, TB and Malari. Pp. 117. [Google Scholar]
- National Academy of Sciences. The Determinants of Recent Trends in Fertility in Sub-Saharan Africa: A Workshop Summary. Washington, DC: National Academies Press; 2016. [DOI] [Google Scholar]
- Polis CB, Curtis KM, Hannaford P, Phillips SJ, Chipato T, Kiarie JN, Westreich DJ, Steyn P. An updated systematic review of epidemiological evidence on hormonal contraceptive methods and HIV acquisition in women. AIDS. 2016;30:2665–2683. doi: 10.1097/QAD.0000000000001228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polis CB, Phillips SJ, Curtis KM, Westreich DJ, Steyn PS, Raymond E, Hannaford P, Turner AN. Hormonal contraceptive methods and risk of HIV acquisition in women: A systematic review of epidemiologic evidence. Contraception. 2014;90(4):360–90. doi: 10.1016/j.contraception.2014.07.009. [DOI] [PubMed] [Google Scholar]
- Prata N, Weidert K, Sreenivas A. Meeting the need: Youth and family planning in Sub-Saharan Africa. Contraception. 2013;88(1):83–90. doi: 10.1016/j.contraception.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Reynolds H, Janowitz B, Wilcher R, et al. Contraception to prevent HIV-positive births: Current contribution and potential cost savings in PEPFAR countries. Sexually Transmitted Infections. 2008;84(Supplement 2):ii49–ii53. doi: 10.1136/sti.2008.030049. [DOI] [PubMed] [Google Scholar]
- Ross JA, Mauldin WP. Family planning programs: Efforts and results, 1972–94. Studies in Family Planning. 1996;27(3):137–147. [PubMed] [Google Scholar]
- Ross J, Smith E. Trends in national family planning programs, 1999, 2004 and 2009. International Family Planning Perspectives. 2011;37(3):125–133. doi: 10.1363/3712511. [DOI] [PubMed] [Google Scholar]
- Ross JA, Stover J, Adelaja D. Family planning programs in 2004: New assessments in a changing environment. International Family Planning Perspectives. 2007;33(1):22–30. doi: 10.1363/3302207. [DOI] [PubMed] [Google Scholar]
- Scott VK, Gottschalk LB, Wright KQ, Wright CT, Bohren MA, Schmitt ME, Ortayli N. Community health workers’ provision of family planning services in low- and middle-income countries: A systematic review of effectiveness. Studies in Family Planning. 2015;46(3):241–261. doi: 10.1111/j.1728-4465.2015.00028.x. [DOI] [PubMed] [Google Scholar]
- Shiffman J. Has donor prioritization of HIV/AIDS displaced aid for other health issues? Health Policy and Planning. 2008;23:95–100. doi: 10.1093/heapol/czm045. [DOI] [PubMed] [Google Scholar]
- Shiffman J, Quissell K. Family planning: A political issue. Lancet. 2012;380(9837):181–185. doi: 10.1016/S0140-6736(12)60782-X. [DOI] [PubMed] [Google Scholar]
- Tietze C. Probability of pregnancy resulting from a single unprotected coitus. Fertility & Sterility. 1960;11:485–488. [Google Scholar]
- United Nations. Department of Economic and Social Affairs. Population Division. 2016b World Contraceptive Use 2015 (POP/DB/CP/Rev2015) http://www.un.org/en/development/desa/population/publications/dataset/contraception/wcu2015.shtml. Accessed March 27, 2016.
- United Nations. Department of Economic and Social Affairs. Population Division. 2016a 2015 Revision of World Population Prospects. http://esa.un.org/unpd/wpp/. Accessed March 27, 2016.
- Westoff CF, Bietsch K, Koffman D, Indicators of trends in fertility in Sub-Saharan Africa . DHS Analytical Studies No 34. Calverton, MD: Macro International Inc; Aug, 2013. [Google Scholar]
- Wilcher R, Cates W, Jr, Gregson S. Family planning and HIV: Strange bedfellows no longer. AIDS. 2009;23(Suppl. 1):S1–S6. doi: 10.1097/01.aids.0000363772.45635.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcher R, Hoke T, Adamchak S, Cates W., Jr Integration of family planning into HIV services: A synthesis of recent evidence. AIDS. 2013;27(Suppl 1):S65–S75. doi: 10.1097/QAD.0000000000000051. [DOI] [PubMed] [Google Scholar]


