Abstract
Iatrogenic nerve injury during fracture surgery of the upper arm is a well-known complication. Prevention of this type of injuries would be of great value. The literature describes several methods to reduce this type of injury, but no perfect solution is at hand. In this study we introduce a new radiographic evaluation of the course and variation of the radial nerve in the distal part of the humerus in relation to bony landmarks as observed on a plain (trauma) radiographs. Aim of this new approach is to reduce the chance of iatrogenic nerve injury by defining of a danger zone in the distal upper arm regarding the radial nerve and hence give an advise for future implant fabrication.
Methods and findings
Measurements were done on both arms of ten specially embalmed specimens. Arms were dissected and radiopaque wires attached to the radial nerve in the distal part of the upper arm. Digital radiographs were obtained to determine the course of the radial nerve in the distal 20 cm of the humerus in relation to bony landmarks; medial epicondyle and capitellum-trochlea projection (CCT). Analysis was done with ImageJ and Microsoft Excel software. We also compared humeral nail specifications from different companies with the course of the radial nerve to predict possible radial nerve damage.
Results
The distance from the medial epicondyle to point where the radial nerve bends from posterior to lateral was 142 mm on AP radiographs and 152 mm measured on the lateral radiographs. The average distance from the medial epicondyle to point where the radial nerve bends from lateral to anterior on AP radiographs was 66 mm. On the lateral radiographs where the nerve moves away from the anterior cortex 83 mm to the center of capitellum and trochlea (CCT). The distance from the bifurcation of the radial nerve into the posterior interosseous nerve (PIN) and superficial radial nerve was 21 mm on AP radiographs and 42 mm on the lateral radiographs (CCT).
Conclusions
The course of the radial nerve in the distal part of the upper arm has great variety. Lateral fixation is relatively safe in a zone between the center of capitellum-trochlea and 48 mm proximal to this point. The danger zone in lateral fixation is in-between 48–122 mm proximal from CCT. In anteroposterior direction; distal fixation is dangerous between 21–101 mm measured from the medial epicondyle. The more distal, the more medial the nerve courses making it more valuable to iatrogenic damage. The IMN we compared with our data all show potential risk in case of (blind) distal locking, especially from lateral to medial direction.
Introduction
Humeral shaft fractures account for 3–5% of all skeletal fractures and 20% of all humeral fractures[1]. Humeral fractures are due to a fall (87%), motor accidents (8%) or direct trauma (5%)[2]. 90% of humeral shaft fractures are treated conservatively and have good clinical outcome. Surgical intervention occurs in 10% of the fractures where surgery can either be early in open, pathological or comminuted fractures or delayed [3]. Both in conservative and surgical treatment there is a risk of soft tissue injury where neurovascular structures are especially at risk. Radial nerve palsy occurs in 11% of humeral shaft fractures due to direct trauma or temporary entrapment before fracture reposition [4, 5]. As opposed to ulnar or median nerve palsy, which are very rare as described in literature only by some case reports or cadaveric studies [6–8]. The severity of the radial nerve palsy varies from symptoms of sensory disturbance of the dorsolateral aspect of the hand to complete paralysis of the brachioradial muscle and the extensor muscles of the wrist and fingers. On average 88% of radial nerve palsies recover completely. 81% of these cases resolve spontaneously in an average period of six months. The other 19% require surgical re-intervention [8]. Ten to twenty percent of all radial nerve palsies due to humeral shaft fractures is iatrogenic and is caused by manipulation or dissection during surgical treatment [5].
The intraoperative risks of radial nerve damage depends on the surgical method. Plate osteosynthesis results in high union rates but requires extensive dissection of soft tissue with a high risk of nerve injury. Alternatively, the fracture can be stabilized by intra-medullary nailing (IMN) in which soft tissue surrounding the fracture is preserved and the chance of nerve damage is reduced. During IMN procedures the radial nerve is injured in one to six percent. The most common mechanism of injury to the radial nerve occurs during distal locking, in particular when using lateral-to-medial directed locking screws. Both plate osteosynthesis and IMN are comparable in terms of functional outcome and rates of union [9, 10].
Several anatomical studies describe the course and position of the radial nerve in relation to anatomical landmarks such as the lateral inter muscular septum, the triceps aponeurosis or bony landmarks such as the medial or lateral epicondyle. These structures serve as reliable perioperative landmarks for the course of the radial nerve [11–13]. However, no studies are known in which the position of the radial nerve was determined pre-operatively on a radiograph. In order to assess the course of the radial nerve in the distal humeral region, anatomical landmarks such as the acromion can be used. In clinical situations however, it is much more reliable to assess the position of the radial nerve by using the medial epicondyle and capitellum-trochlea line (in lateral view) as landmarks.
The aim of this study is to reduce the chance of iatrogenic injury to the radial nerve in the distal upper arm by determine the course and variation of the radial nerve. This was done in relation to anatomical bony landmarks; epicondyle and center of capitellum-trochlea, as observed on a plain (trauma) radiographs and hereby determine a ‘danger zone’ during lateral and AP fixation in which the radial nerve is at risk and hence give an advise for future implant fabrication.
Materials and methods
For this study human specimens were used. All humans whom donated their body for science used in our cadaver study had a written form of consent. Regarding the Dutch law and our institutional ethics committee, no other forms or documentation is necessary.
Twenty arms were dissected in the supine position, derived from ten Caucasian embalmed human anatomic specimens (6 female and 4 male). Mean age was 72 years (range 57–89). All specimens were embalmed at room temperature between 24 and 48 hours post-mortem. Embalming was performed according the AnubiFiX® (AnubiFiX, Rotterdam, The Netherlands) method, preserving tissue and joint flexibility thereby providing a representative anatomy and mechanics [14–16].
A direct lateral distal humerus incision was made and the triceps, brachial and brachioradial muscles were retracted. The radial nerve was identified in the distal part of the upper arm and exposed. Care was taken not to dissect the nerve and its surrounding tissue to keep normal anatomical relations of the nerve intact. A radio-opaque wire was placed directly adjacent to the radial nerve and attached with 4 metal clips (Figs 1 and 2). The bifurcation of the radial nerve in the superficial and deep branch was marked with two close adjacent clips. The fascia was then closed keeping the marked radial nerve in its anatomical position. Subcutaneous and superficial layers were closed with conventional continuous sutures. Radiographs with a calibration bar were obtained with a mobile C-arm system (BV 29, Philips, Eindhoven, The Netherlands). Lateral radiographs were directed through capitellum and trochlea (figure of 8) to obtain a true lateral image. Anteroposterior (AP) radiographs were directed perpendicular to this axis, shown in Fig 2. After scaling by using the calibration bar, measurements were performed on the standardized digital radiographs using ImageJ (version 1.38), Fig 2 [17]. Distances on AP radiographs were measured between points of interest (POI) and the line perpendicular to the humeral shaft running through the medial epicondyle and on true lateral radiographs from the center of capitellum-trochlea projection (CCT). POI are point A representing the location where the radial nerve courses from the dorsal to the lateral side of the arm. The second POI (B) locates the radial nerve bending from lateral to anterior in AP view and away from the anterior cortex in lateral view. The bifurcation of the radial nerve into the superficial and deep branch was marked as point C, Fig 2. The distance of the radial nerve to the lateral cortex on AP radiographs was measured in a 10 mm interval and the distance to the dorsal cortex on lateral radiographs is measured in a 20 mm interval.
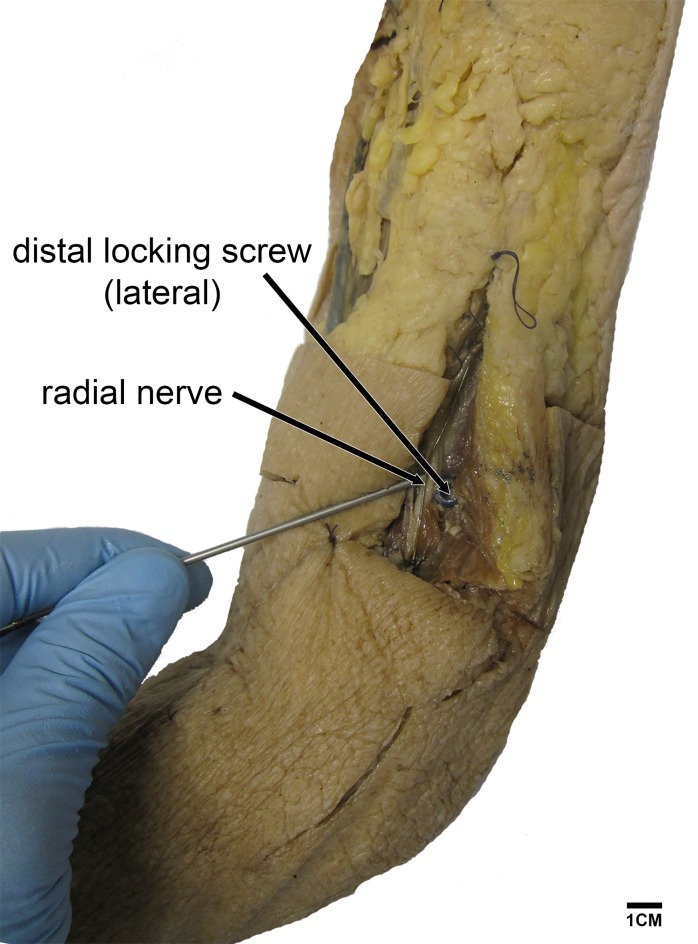
Fig 1. Left dissected humerus.
In one arm we inserted a T2 humerus nail showing potential risk of damaging the radial nerve during distal screw fixation (lateral to medial direction).
Fig 2. Radiographs (AP and lateral view) of prepared upper arm showing a marked radial nerve and method of measurements.
Points of interest A, B and C are marked.
Nail specifications from the three most commonly used intramedullary nails in the Netherlands were obtained; Synthes®, Stryker® and Smith&Nephew®. These specifications were compared to our data. A ‘danger zone’ was defined by measuring the position of the proximal ridge of the olecranon fossa in comparison to the medial epicondyle and CCT. Next, 20 mm was added to correct for the ideal position of the humerus nail (20 mm proximal to the proximal ridge of the olecranon fossa). With these data, the position of the distal locking hole(s) as it would be in an in vivo situation can be correlated to the measured location of the radial nerve in AP and lateral obtained radiographs. Data were analyzed using Microsoft Excel® version 14.7.2 (Microsoft® Excel® for Mac 2011).
Results
All measurements performed on the radiographs are presented in Table 1.
Table 1. Data overview of measurements on AP and lateral humeral radiographs with Mean, Standard Deviation and Range in cm.
| Anteriorposterior view | |||||||||
| No | Spec No | Side | Gender | Age (Y) | Position x-ray | humerus length | radial nerve curves posterior to lateral in relation to medial epicondyle | radial nerve lateral to anterior in relation to medial epicondyle | split radial nerve in profunda/superficialis in relation to medial epicondyle |
| 1 | 393 | L | M | 81 | AP | 37 | 16,23 | 6,93 | 2,14 |
| 2 | 393 | R | M | 81 | AP | 37,2 | out op pic | 10,05 | 3,76 |
| 3 | 396 | L | F | 64 | AP | 31,1 | out op pic | 4,40 | 1,86 |
| 4 | 396 | R | F | 64 | AP | 31,5 | out op pic | 5,52 | 3,39 |
| 5 | 401 | L | M | 89 | AP | 31,4 | 11,75 | 5,56 | 3,05 |
| 6 | 401 | R | M | 89 | AP | 32,4 | out op pic | 7,63 | 2,5 |
| 7 | 405 | L | F | 86 | AP | 34,5 | 16,52 | 7,39 | 1,59 |
| 8 | 405 | R | F | 86 | AP | 35,4 | 14,1 | 8,04 | 2,5 |
| 9 | 411 | L | F | 63 | AP | 34,5 | 12,36 | 6,45 | 1,33 |
| 10 | 411 | R | F | 63 | AP | 35,5 | out op pic | 7,19 | 3,34 |
| 11 | 492 | L | M | 65 | AP | 30 | 12,10 | 5,55 | 0,76 |
| 12 | 492 | R | M | 65 | AP | 30 | 12,84 | 5,51 | 2,98 |
| 13 | 522 | L | M | 64 | AP | 33 | 15,50 | 6,50 | 0,53 |
| 14 | 522 | R | M | 64 | AP | 33 | 15,96 | 6,87 | 1,29 |
| 15 | 574 | L | F | 57 | AP | 33 | 15,62 | 3,55 | -0,42 |
| 16 | 574 | R | F | 57 | AP | 33 | 12,42 | 3,74 | -0,41 |
| 17 | 582 | L | M | 85 | AP | 35 | 12,91 | 2,11 | 0,51 |
| 18 | 582 | R | M | 85 | AP | 35 | 11,90 | 2,49 | 3,48 |
| 19 | 584 | L | F | 64 | AP | 34 | 16,05 | 6,09 | 2,77 |
| 20 | 584 | R | F | 64 | AP | 34 | 16,22 | 7,56 | 4,87 |
| N | 15 | 20 | 20 | ||||||
| mean | 71,80 | 33,53 | 14,17 | 6,63 | 2,09 | ||||
| SD | 11,61 | 2,07 | 1,88 | 1,96 | 1,43 | ||||
| min | 57,00 | 30,00 | 11,75 | 2,11 | 0,42- | ||||
| max | 89,00 | 37,20 | 16,52 | 10,05 | 4,89 | ||||
| Lateral view | |||||||||
| No | Spec No | Side | Gender | Age (Y) | Position x-ray | humerus length | radial nerve curves posterior to lateral in relation to CCT | radial nerve away from anterior cortex to CCT | split radial nerve in profunda/superficialis in relation tot CCT |
| 1 | 393 | L | M | 81 | LAT | 37 | 18,16 | 7,15 | 3,93 |
| 2 | 393 | R | M | 81 | LAT | 37,2 | 19,83 | 6,17 | 5,67 |
| 3 | 396 | L | F | 64 | LAT | 31,1 | 17,04 | 4,75 | 5,41 |
| 4 | 396 | R | F | 64 | LAT | 31,5 | 14,4 | 5,07 | 3,68 |
| 5 | 401 | L | M | 89 | LAT | 31,4 | 13,56 | 11,33 | 5,76 |
| 6 | 401 | R | M | 89 | LAT | 32,4 | 12,44 | 7,30 | 4,10 |
| 7 | 405 | L | F | 86 | LAT | 34,5 | 16,75 | 7,90 | 4,46 |
| 8 | 405 | R | F | 86 | LAT | 35,4 | 14,79 | 9,66 | 5,44 |
| 9 | 411 | L | F | 63 | LAT | 34,5 | 15,10 | 6,25 | 3,49 |
| 10 | 411 | R | F | 63 | LAT | 35,5 | 16,29 | 8,07 | 6,07 |
| 11 | 492 | L | M | 65 | LAT | 30 | 12,77 | 5,89 | 0,66 |
| 12 | 492 | R | M | 65 | LAT | 30 | 11,32 | 12,17 | 3,35 |
| 13 | 522 | L | M | 64 | LAT | 33 | out op pic | 8,08 | 0,51 |
| 14 | 522 | R | M | 64 | LAT | 33 | 16,34 | 8,33 | 1,67 |
| 15 | 574 | L | F | 57 | LAT | 33 | 14,23 | 11,91 | 0,47 |
| 16 | 574 | R | F | 57 | LAT | 33 | out op pic | 6,44 | 0,98 |
| 17 | 582 | L | M | 85 | LAT | 35 | 15,96 | 10,98 | 0,41 |
| 18 | 582 | R | M | 85 | LAT | 35 | 16,93 | 10,79 | 4,11 |
| 19 | 584 | L | F | 64 | LAT | 34 | 14,11 | 9,80 | 3,13 |
| 20 | 584 | R | F | 64 | LAT | 34 | 13,11 | 7,60 | 4,00 |
| N | 18 | 20 | 20 | ||||||
| mean | 71,80 | 33,53 | 15,17 | 8,28 | 4,16 | ||||
| SD | 11,61 | 2,07 | 2,18 | 2,28 | 1,94 | ||||
| min | 57,00 | 30,00 | 11,32 | 4,75 | 0,41 | ||||
| max | 89,00 | 37,20 | 19,83 | 12,17 | 6,07 | ||||
Data is represented as mean (± SD) and range, unless otherwise stated. Average humerus length was 335 mm (SD 21; 300–372 mm) from the tip of the humerus to the medial epicondyle. No significant differences were found between humeral length and gender (Student t-test, p = 0.8). The average distance from the medial epicondyle to point where the radial nerve bends from posterior to lateral was 142 mm (SD 19; 118–165) on AP radiographs and 152 mm (SD 22; 113–198 mm) measured on the lateral radiographs to the center of capitellum and trochlea (CCT). The average distance from the medial epicondyle to point where the radial nerve bends from lateral to anterior on AP radiographs was 66 mm (SD 20; 21–101). On the lateral radiographs POI B refers to the point where the nerve moves away from the anterior cortex 83 mm (SD 23; 48–122) to the center of capitellum and trochlea (CCT). The distance from the bifurcation of the radial nerve into the posterior interosseous nerve (PIN) and superficial radial nerve was 21 mm (SD 14; -41–49) on AP radiographs and 42 mm (SD 19; 4–61) on the lateral radiographs (CCT). Fig 3 shows the average course of radial nerve in relation to both the lateral cortex (AP Fig) and the posterior cortex (lateral Fig) of the distal humerus, POI A, B and C are marked.
Fig 3. Graph representing the course of the radial nerve and the ‘danger zones’.
The red area in the AP view marks the ‘danger zone’ for AP fixation. The red area in the lateral view shows the ‘danger zone’ for lateral drilling (horizontal lines are the mean ± 2SD, red area represents range of possible radial nerve location.
The Expert nailing system (Synthes®) and TRIGEN Long Bent Humeral Nail (Smith&Nephew®) have AP distal locking holes whereas the T2-PHN (Stryker®) has both AP and lateral distal locking holes. When placed anterograde and in a correct manner, 20 mm proximal from the olecranon fossa ridge, the Expert nailing system on average locks AP between 48 and 78 mm from the medial epicondyle and locks lateral at 63 mm. TRIGEN locks AP between 44 and 54 mm. T2-PHN locks AP between at 44 mm and lateral between 52 and 62 mm. When placed retrograde and correct, Expert-nailing system locks distally AP between 34 and 68 mm and T2-PHN locks lateral between 46 and 72 mm, as is presented in Table 2. No retrograde intramedullary humerus nail by Smith&Nephew® is available. All distal locking holes were in a position in which the radial nerve is at risk when locking the nail.
Table 2. Overview of position of locking holes in long humeral intramedullary locking nails from Synthes®, Stryker® and Smith&Nephew® Distance is measured from the most distal end of the nail, to the medial epicondyle in AP direction and to the center of capitellum and trochlea in lateral view.
The range in which distal locking can be performed, measured in mm.
| Anteroposterior view | ||
| mean range | holes | |
| Synthes® anterograde | 48–78 | 3 |
| retrograde | 34–68 | 3 |
| Stryker® | 44 | 1 |
| Smith&Nephew® | 44–54 | 2 |
| Lateral view | ||
| mean range | holes | |
| Synthes® anterograde | 63 | 3 |
| Stryker® anterograde | 52–62 | 2 |
| retrograde | 46–72 | 3 |
| distance in mm | ||
Discussion
This study investigates the course of the radial nerve in relation to landmarks observed on standard radiographs. Various anatomical studies determine the course of the radial nerve in order to avoid iatrogenic injury during surgical procedures [12, 13, 18, 19]. In contrast to previous studies we used radiological guidance to determine the location of the radial nerve rather than surface anatomy [20].
We observed significant variation in the position of the radial nerve in the distal third part of the humerus. Lateral fixation or pin placement is relatively safe in a zone between the center of capitellum-trochlea (CCT) and 48 mm proximal of this point. The danger zone in lateral fixation is in-between 48 and 122 mm proximal from CCT. In anteroposterior direction; distal fixation remains dangerous between 21 and 101 mm measured from the medial epicondyle. The more distal, the more the nerve moves toward the medial side, Fig 3, making it more valuable to iatrogenic damage. Besides the radial nerve, structures such as the median nerve, brachial artery and vein are also at risk during distal locking. We therefore advocate blunt dissection to the bone and usage of a drill protector to limit the risk of iatrogenic nerve damage. Pre-operative skin marking with radiographic aid can decrease the chance of damaging the radial nerve.
Noger et al. illustrated the potential damage of the radial nerve by insertion of a distal locking nail when placing a Synthes® standard unreamed humerus nail [21]. This study further explores this potential complication by describing the average course of the radial nerve and its orientation in relation to the distal humerus and the potential risk of radial nerve damage in two more humerus nail systems. Due to natural occurring anatomical race and gender differences the course of the radial nerve can even vary more [22]. The one-third, two-thirds ratio as described by Fleming et al. was measured from the acromion to the lateral epicondyle [12]. We advocate that the sub acromial space negatively influences the measurement of the humerus as this space varies when the deltoid muscle is completely relaxed (e.g. under local or general anesthesia). Therefore no ratio comparison could be made. Small numbers of specimens and lack of in situ measurements of different intramedullary nails and their distal locking places in reference to the radial nerve location are factors that limit this study. Despite these factors, the data can very well be applied to clinical settings. The most important message is the awareness of potential radial nerve damage during surgical placement of any distal locking screw or external fixators in lateral or AP direction. We would recommend manufacturers of intramedullary implants to use this information in future implant development.
Conclusions
Based on our results we conclude that the course of the radial nerve in the distal part of the upper arm has great variety. Lateral fixation or pin placement is relatively safe in a zone between the center of capitellum-trochlea (CCT) and 48 mm proximal of this point. The danger zone in lateral fixation is in-between 48 and 122 mm proximal from CCT. In anteroposterior direction; distal fixation is dangerous between 21 and 101 mm measured from the medial epicondyle. The more distal, the more the nerve moves toward the medial side, Fig 3, making it more valuable to iatrogenic damage. The IMN we compared with our data all show potential risk in case of (blind) distal locking, especially from lateral to medial direction.
Acknowledgments
We, the authors, would like to thank all the people who donated their body for science and their relatives at our institution making it possible to perform this study. Special thanks go out for Ms. Yvonne Steinvoort (prosector) and the Erasmus Anatomy Research Project team for their time and effort during the practical sessions. Peter Frederik (PhD), Heinrich Janzing (PhD) and Tim de Jong (PhD) for their critical notes.
Compliance with ethical standards
All procedures performed in studies involving human anatomical specimen were in accordance with the ethical standards of the institutional and/or national research committee. All the human anatomical specimens used for our experiments were donated for scientific research and medical training at our faculty and were part of a national body donation program approved by Dutch law and regulations.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Schemitsch EH, Weinberg JA, McKee MD, Richards RR. The relative importance of intramedullary, intracortical, and extraosseous soft-tissue blood flow to the repair of devascularized canine tibial cortex. Ann Plast Surg. 1997;38:623–31. [DOI] [PubMed] [Google Scholar]
- 2.Kim SH, Szabo RM, Marder RA. Epidemiology of humerus fractures in the United States: nationwide emergency department sample, 2008. Arthritis Care Res (Hoboken). 2012;64:407–14. [DOI] [PubMed] [Google Scholar]
- 3.Bishop J, Ring D. Management of radial nerve palsy associated with humeral shaft fracture: a decision analysis model. J Hand Surg Am. 2009;34:991–6 e1. doi: 10.1016/j.jhsa.2008.12.029 [DOI] [PubMed] [Google Scholar]
- 4.Venouziou AI, Dailiana ZH, Varitimidis SE, Hantes ME, Gougoulias NE, Malizos KN. Radial nerve palsy associated with humeral shaft fracture. Is the energy of trauma a prognostic factor? Injury. 2011;42:1289–93. doi: 10.1016/j.injury.2011.01.020 [DOI] [PubMed] [Google Scholar]
- 5.Wang X, Zhang P, Zhou Y, Zhu C. Secondary radial nerve palsy after internal fixation of humeral shaft fractures. Eur J Orthop Surg Traumatol. 2014;24:331–3. doi: 10.1007/s00590-013-1197-y [DOI] [PubMed] [Google Scholar]
- 6.Apergis E, Aktipis D, Giota A, Kastanis G, Nteimentes G, Papanikolaou A. Median nerve palsy after humeral shaft fracture: case report. J Trauma. 1998;45:825–6. [DOI] [PubMed] [Google Scholar]
- 7.Hems TE, Mahmood F. Injuries of the terminal branches of the infraclavicular brachial plexus: patterns of injury, management and outcome. J Bone Joint Surg Br. 2012;94:799–804. doi: 10.1302/0301-620X.94B6.28286 [DOI] [PubMed] [Google Scholar]
- 8.Stahl S, Rosen N, Moscona R. Ulnar nerve palsy following fracture of the shaft of the humerus. J Orthop Trauma. 1998;12:363–4. [DOI] [PubMed] [Google Scholar]
- 9.Kurup H, Hossain M, Andrew JG. Dynamic compression plating versus locked intramedullary nailing for humeral shaft fractures in adults. Cochrane Database Syst Rev. 2011:CD005959 doi: 10.1002/14651858.CD005959.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Putti AB, Uppin RB, Putti BB. Locked intramedullary nailing versus dynamic compression plating for humeral shaft fractures. J Orthop Surg (Hong Kong). 2009;17:139–41. [DOI] [PubMed] [Google Scholar]
- 11.Arora S, Goel N, Cheema GS, Batra S, Maini L. A method to localize the radial nerve using the 'apex of triceps aponeurosis' as a landmark. Clin Orthop Relat Res. 2011;469:2638–44. doi: 10.1007/s11999-011-1791-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fleming P, Lenehan B, Sankar R, Folan-Curran J, Curtin W. One-third, two-thirds: relationship of the radial nerve to the lateral intermuscular septum in the arm. Clin Anat. 2004;17:26–9. doi: 10.1002/ca.10181 [DOI] [PubMed] [Google Scholar]
- 13.Guse TR, Ostrum RF. The surgical anatomy of the radial nerve around the humerus. Clin Orthop Relat Res. 1995:149–53. [PubMed] [Google Scholar]
- 14.Theeuwes HP MvR, Lange JF, Kleinrensink GJ. A New Model for Training on Human Specimens in Surgical-Anatomical Skills Labs. Anatomy Physiol Biochem Int J. 2017;3:5. [Google Scholar]
- 15.Klitsie PJ, Ten Brinke B, Timman R, Busschbach JJ, Theeuwes HP, Lange JF, et al. Training for endoscopic surgical procedures should be performed in the dissection room: a randomized study. Surg Endosc. 2017;31:1754–9. doi: 10.1007/s00464-016-5168-3 [DOI] [PubMed] [Google Scholar]
- 16.Slieker JC, Theeuwes HP, van Rooijen GL, Lange JF, Kleinrensink GJ. Training in laparoscopic colorectal surgery: a new educational model using specially embalmed human anatomical specimen. Surg Endosc. 2012;26:2189–94. doi: 10.1007/s00464-012-2158-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schneider CA, Rasband WS, Eliceiri KW. NIH Image to ImageJ: 25 years of image analysis. Nat Methods. 2012;9:671–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bono CM, Grossman MG, Hochwald N, Tornetta P, 3rd. Radial and axillary nerves. Anatomic considerations for humeral fixation. Clin Orthop Relat Res. 2000:259–64. [PubMed] [Google Scholar]
- 19.Chaudhry T, Noor S, Maher B, Bridger J. The surgical anatomy of the radial nerve and the triceps aponeurosis. Clin Anat. 2010;23:222–6. doi: 10.1002/ca.20903 [DOI] [PubMed] [Google Scholar]
- 20.Cox CL, Riherd D, Tubbs RS, Bradley E, Lee DH. Predicting radial nerve location using palpable landmarks. Clin Anat. 2010;23:420–6. doi: 10.1002/ca.20951 [DOI] [PubMed] [Google Scholar]
- 21.Noger M, Berli MC, Fasel JH, Hoffmeyer PJ. The risk of injury to neurovascular structures from distal locking screws of the Unreamed Humeral Nail (UHN): a cadaveric study. Injury. 2007;38:954–7. doi: 10.1016/j.injury.2007.04.014 [DOI] [PubMed] [Google Scholar]
- 22.Chou PH, Shyu JF, Ma HL, Wang ST, Chen TH. Courses of the radial nerve differ between chinese and Caucasians: clinical applications. Clin Orthop Relat Res. 2008;466:135–8. doi: 10.1007/s11999-007-0019-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.