Abstract
Aim The purpose of this prospective multicenter study was to test the predictive value of cortical comminution and intra-articular involvement on function and quality of life in distal radius fractures (DRFs) using the Buttazzoni's classification system.
Patients and Methods We studied 406 patients between skeletal maturity and 74 years of age with DRF. Fractures with acceptable radiographic alignment were immobilized with a cast. Fractures with nonacceptable radiographic alignment underwent closed reduction and 4 to 6 weeks cast immobilization. Radiographs were obtained after reduction and at 10 to 14 days. Redisplaced fractures were offered surgical treatment. One-year follow-up included grip strength, range of motion (ROM), quickDASH, EQ-5D (including visual analog scale [VAS] for health status), and VAS pain.
Results We found no statistically significant differences in QuickDASH, EQ-5D questionnaire, EQ-5D health status VAS, and VAS pain among the Buttazzoni classes. However, initial displacement was associated with worse quickDASH score, worse EQ-5D score, reduced grip strength, and reduced ROM. Dorsal comminution was associated with worse quickDASH score, reduced flexion, and reduced pronation–supination ability. Volar comminution predicted loss of extension, while intra-articular involvement was associated with reduced flexion–extension arc and worse EQ-5D score. There was a significant difference in ROM between noncomminuted and comminuted fracture classes.
Conclusion Initial fracture position, type of comminution, and intra-articular involvement influenced the clinical outcome in DRF.
Keywords: distal radius fracture, wrist, classification, outcome, radiology
Distal radius fracture (DRF) is the most common fracture encountered in clinical practice. 1 Numerous classification systems have been developed for evaluation of DRF. The most commonly cited are the Frykman's, AO/OTA, Melone's, Mayo's, Cooney's, and Fernandez's classifications. However, the value of these is limited since they have not showed satisfactory interobserver and intraobserver reliabilities. 2 Furthermore, the utility of these systems to predict radiographic or clinical outcome is not adequately proven. 3 4 5 These shortcomings may be one reason why optimal DRF management is still controversial. 6 New classification systems, predictive of radiological and clinical outcome, and easy to use are required to maintain a common language when defining DRF. 2
We proposed a classification system, the Buttazzoni's classification, which introduced volar comminution as a separate parameter when evaluating DRF ( Table 1 , Figs. 1 and 2 ). The interobserver reliability and intraobserver reproducibility of the Buttazzoni's classification were fair to substantial. 7 Furthermore, the Buttazzoni's classification could predict the radiographic outcome. 8 Volar comminution was highly associated with fracture instability. 8
Table 1. Fracture characteristics.
| Type | Description |
|---|---|
| B1 | Extra-articular DRF with no cortical (metaphyseal) comminution |
| B2 | Extra-articular DRF with comminution of the dorsal cortex |
| B3 | Complete intra-articular (radiocarpal joint) DRF with or without metaphyseal comminution of the dorsal cortex |
| B4 | DRF with comminution of the volar cortex regardless of other coexisting fracture properties as dorsal comminution or intra-articularity |
| B0 | DRF which cannot be classified according to the above types such as partially articular fractures, e.g., Barton's fractures, Chauffeur's fractures, or coexisting carpal fracture dislocation |
Abbreviation: DRF, distal radius fracture.
Note: The classification is hierarchical, and a fracture is always given the highest possible number from the presented fracture characteristics.
Fig. 1.
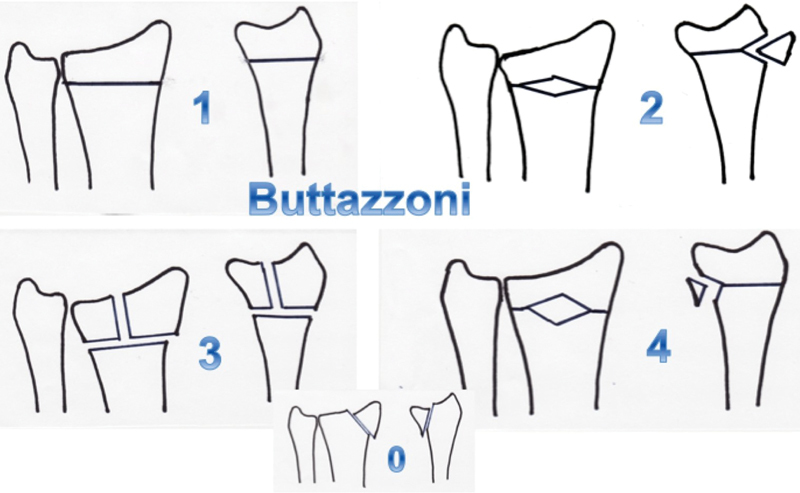
Presentation of the Buttazzoni's classification.
Fig. 2.

Example of a B4 fracture, in this case with both volar and dorsal comminution.
The aim of this study was to determine the predictive value of cortical comminution and intra-articular involvement on clinical outcome of DRF regardless of fracture class and treatment option used. Our hypothesis was that the type of comminution and intra-articular involvement would affect active range of motion (ROM), grip strength, complication rates, and self-reported function, quality of life, and pain.
Patients and Methods
Patients
The regional ethics committee approved this prospective cohort study. Between October 2009 and September 2011, all patients with DRF presenting at the emergency department of two teaching hospitals were invited to participate. A total of 417 patients with a mean age of 56 years (range: 15–74 years) were enrolled in the study after informed consent. Exclusion criteria are presented in Table 2 . We allocated the patients into two groups: age ≤ 60 and > 60 years.
Table 2. Exclusion criteria.
| Previous fracture to the same wrist Coexisting carpal fracture or SLAC wrist Rheumatoid arthritis Bilateral fractures Alcohol or drug abuse Open fracture Dementia Unfused distal radial epiphysis Neurological impairment Galeazzi's fracture |
Fracture Treatment
Anteroposterior and lateral radiographic views in neutral rotation were obtained to assess radial inclination, volar tilt, ulnar variance, and intra-articular step off. The on-call registrars, who had been trained on the classification, classified the radiographs. Dorsal or volar comminution was assessed on the lateral plain radiograph and was defined as the presence of a free-floating piece of cortex. Small fragments of 3 mm or less were not considered as comminution. All fractures were discussed at the weekday morning radiology rounds.
Fractures with volar inclination < 20 degrees, dorsal inclination < 10 degrees, radial tilt > 10 degrees, positive ulnar variance < 2 mm, and intra-articular step < 2 mm were considered to have acceptable radiographic alignment and were immobilized in a short arm cast. Fractures with nonacceptable radiographic alignment were reduced under local anesthesia using hematoma blockade or intravenous regional anesthesia and immobilized in a short arm cast. If reduction was successful, according to the same parameters as earlier, the patient was re-examined after 10 to 14 days. If the earlier parameters were still acceptable, the cast was retained for 4 to 6 weeks in total. Patients with fractures that lost acceptable radiographic alignment immediately or at follow-up at 10 to 14 days were offered further treatment with intrafocal pinning, external fixation, internal fixation, or combined method using the surgeons preferred method. No fracture was operated on if proven stable in the cast. The treatment algorithm is shown in Fig. 3 .
Fig. 3.
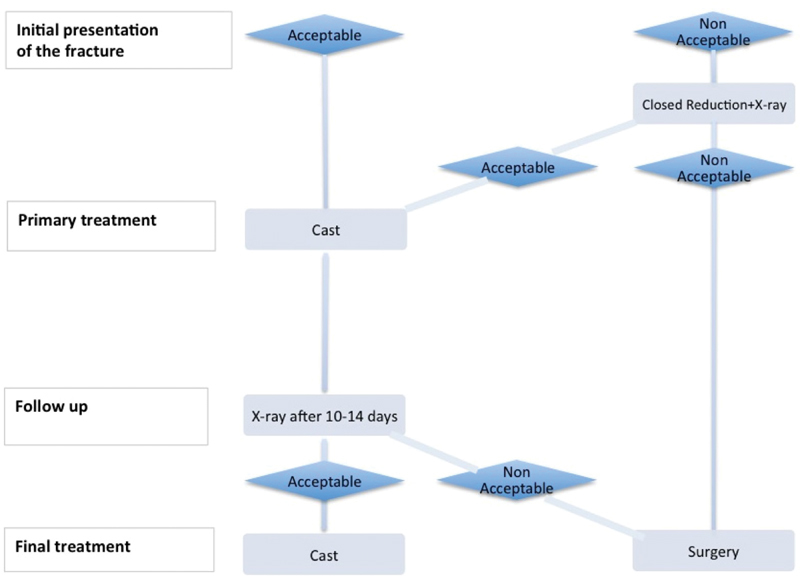
Treatment algorithm.
Outcome Measures
Clinical evaluation was made 1 year after the fracture. The QuickDASH, 9 EQ-5D 10 questionnaire, and EQ-5D health visual analog scale (VAS) 10 were used to assess functional outcome and quality of life. A research nurse blinded to fracture class registered the subjective questionnaires. An independent occupational therapist blinded to fracture class measured objective function including grip strength, active ROM, and pain VAS. The occurrence of carpal tunnel syndrome (CTS), extensor pollicis longus (EPL) rupture, and complex regional pain syndrome (CRPS) during the first year was either ruled out or confirmed according to the medical records and clinical examination. If the patient showed other signs or symptoms such as distal radioulnar joint (DRUJ) instability, paresthesia, or tenosynovitis, this was registered in free text.
Grip strength was measured using a JAMAR dynamometer set for grip size 2. Each measure was attempted three times and the mean value was used. The contralateral wrist was used as control. Grip strength was expressed as percentage of the value of the uninjured wrist.
The active ROM of the wrist and DRUJ were measured in both hands using a standard goniometer. Flexion–extension arc, pronation–supination arc, and radial–ulnar deviation arc were registered. The total ROM was calculated as the sum of these three. Loss of ROM in the fractured wrist was expressed in angular degrees compared with the uninjured wrist.
Complications were documented as existing or absent for each diagnosis during the first year.
Statistics
A power analysis was performed based on comparing quickDASH score. With a power of 0.80 and a significance level (α) of 0.05, a minimum of 32 patients was needed in each group to detect a 10-point difference (standard deviation 16) in quickDASH among the groups. We assumed that a 10-point difference in quickDASH was the smallest effect that would be clinically relevant. 11 The effect of dorsal and volar comminution, intra-articular involvement, initial position of the fracture, age, gender, and treatment on ROM and grip strength was analyzed using the t -test. The Buttazzoni fracture classes were compared for grip strength, ROM, and age distribution using the analysis of variance (ANOVA) test with Tukey's honest significant difference post hoc test. A general linear model (GLM) was created for multiple regression analysis to evaluate the effect of age, gender, fracture class, dorsal comminution, volar comminution, intraarticular involvement, and treatment on objective outcome measures. The variables were first analyzed individually using the t -test or ANOVA. Only those parameters with independent predictive significance using the t -test or ANOVA test were included in the GLM. A backward stepwise approach was used where nonsignificant variables were successively excluded from the GLM.
The QuickDASH, EQ-5D, and EQ-VAS data are ordinal. Furthermore, the data showed a skewed distribution making the nonparametric test more appropriate. The Mann–Whitney U -test was used to evaluate the effects of dorsal and volar comminution, intra-articular involvement, initial position of the fracture, age group, gender, and treatment on these outcome parameters. The effects of Buttazzoni fracture class on QuickDASH, EQ-5D, and pain VAS were analyzed using the Kruskal–Wallis's nonparametric test with post hoc test. The data were presented as median with interquartile range. Mean and confidence interval for quickDASH are included to enable comparison with previously published studies.
Fisher's exact test was used to detect differences in the presence of CTS, EPL rupture, CRPS, DRUJ instability, tenosynovitis, or paresthesia. A p -value < 0.05 was considered significant.
Results
Of the initial 417 patients, 11 had bilateral fractures. These were excluded since comparison with an uninjured hand was not possible. Of the remaining 406 patients, 72 patients were lost to follow-up. This left the cohort with 334 (82%) patients who completed the 1-year follow-up.
There were 267 women and 67 men. The mean age was 58 years for women and 51 for men. Of the 334 fractures, 231 (69%) had dorsal comminution, 42 (13%) had volar comminution, and 130 (39%) had intra-articular involvement. There were 12 B0 fractures, 64 B1 fractures, 118 B2 fractures, 98 B3 fractures, and 42 B4 fractures. Age distribution did not differ significantly between fracture classes ( p = 0.341).
Analysis of the outcome according to the fracture patterns and patient characteristics at presentation is shown in Tables 3 and 4 .
Table 3. Factors affecting different parameters of clinical outcome.
| Parameter outcome | Dorsal comminution | Intra-articular | Volar comminution | Initial displacement | Gender | Age group | Surgery |
|---|---|---|---|---|---|---|---|
| Grip strength | p = 0.053 | p = 0.080 | p = 0.549 |
p
= 0.006
( p = 0.006) |
p = 0.568 | p = 0.544 | p = 0.163 |
| Extension |
p
= 0.997
( p = 0.048) |
p
= 0.025
( p = 0.002) |
p
< 0.001
( p < 0.001) |
p
= 0.004
( p < 0.001) |
p = 0.681 | p = 0.118 |
p
= 0.112
( p < 0.001) |
| Flexion |
p
= 0.037
( p = 0.001) |
p
= 0.026
( p = 0.007) |
p = 0.863 |
p
= 0.291
( p = 0.003) |
p = 0.523 | p = 0.600 | p = 0.251 |
| Flexion–extension |
p
= 0.170
( p = 0.001) |
p
= 0.004
( p < 0.001) |
p
= 0.147
( p = 0.012) |
p
< 0.001
( p < 0.001) |
p = 0.506 | p = 0.586 |
p
= 0.720
( p = 0.002) |
| Radial–ulnar | p = 0.159 |
p
= 0.078
( p = 0.028) |
p = 0.246 |
p
= 0.343
( p = 0.034) |
p = 0.184 |
p
= 0.035
( p = 0.049) |
p
= 0.009
( p = 0.013) |
| Supination–pronation |
p
= 0.041
( p < 0.001) |
p = 0.945 | p = 0.190 |
p
= 0.021
( p < 0.001) |
p = 0.060 | p = 0.496 | p = 0.261 |
| Total ROM |
p
= 0.106
( p < 0.001) |
p
= 0.074
( p = 0.011) |
p
= 0.166
( p = 0.022) |
p
≤ 0.001
( p < 0.001) |
p = 0.019 | p = 0.225 |
p
= 0.954
( p = 0.003) |
Abbreviation: ROM, range of motion.
Note: The p -values within the parenthesis are factor with independent predictive significance using the univariate t -test or analysis of variance. The p -values in bold are significant according to the multivariate general linear model and excluded from the model. The p -values in italic are nonsignificant and not included in the model after univariate analysis. In all significant parameters, the presence of the fracture pattern was associated with a worse outcome. Regarding age group, the worse outcome was in the elderly group.
Table 4. Subjective outcome.
| Parameter outcome | Dorsal comminution | Intra-articular | Volar comminution | Initial displacement | Gender | Age group | Surgery |
|---|---|---|---|---|---|---|---|
| QuickDASH | p = 0.009 | p = 0.289 | p = 0.941 | p < 0.001 | p = 0.001 | p = 0.027 | p = 0.095 |
| EQ-5D | p = 0.184 | p = 0.037 | p = 0.978 | p = 0.007 | p = 0.306 | p = 0.769 | p = 0.669 |
Note: In all significant parameters, the presence of the fracture pattern was associated with a worse outcome. Regarding age group, the worse outcome was in the elderly group. Female had a worse outcome. The Mann–Whitney U -test was used.
Displacement at presentation was associated with worse quickDASH ( Tables 4 and 5 ) and EQ-5D ( Table 4 ). It was also associated with reduced ROM and reduced grip strength compared with fractures with acceptable position at presentation ( Table 3 ). Dorsal comminution was associated with a worse quickDASH ( Tables 4 and 5 ), reduced flexion, and reduced prosupination arc ( Table 3 ). Volar comminution at presentation was associated with reduced extension at 1 year ( Table 3 ). Intra-articular involvement resulted in a reduced flexion–extension arc ( Table 3 ) and a worse EQ-5D score ( Table 4 ). Older age group and female gender were associated with a worse outcome in quickDASH ( Table 4 ) at 1 year.
Table 5. QuickDASH median (IQRs) and mean (95% CI) according to fracture characteristics—Mann–Whitney U -test .
| Factor | Yes | No | |
|---|---|---|---|
| Initially nonacceptable radiographic alignment ( p < 0.001) |
Median (IQR) | 15 (5–32) | 9 (2–20) |
| Mean (95% CI) | 19.8 (17.2–22.3) | 12.9 (10.5–15.3) | |
| Dorsal comminution ( p = 0.009) |
Median (IQR) | 12 (5–30) | 8 (2–20) |
| Mean (95% CI) | 18.4 (16.1–20.6) | 13.5 (10.5–16.5) | |
Abbreviations: CI, confidence interval; IQR, interquartile range.
There was a significant difference between noncomminuted fracture classes (B0 and B1) and comminuted fracture classes (B2–B4) in loss of total ROM. Significant between-classes post hoc tests for each arc of motion are shown in Table 6 . The difference in ROM was manifest for fracture class ( p < 0.001) also after adjustment for operative treatment ( p = 0.418), age ( p = 0.183), and gender ( p = 0.093). There were no significant differences in grip strength among the fracture classes. We found no statistically significant differences in QuickDASH, EQ-5D questionnaire, EQ-5D health status VAS, and pain VAS scores among the Buttazzoni classes.
Table 6. Clinical outcome at 1 year.
| Uninjured wrist ROM in deg Mean (95% CI) |
Movement | Injured wrist Loss of ROM in deg Mean (95% CI) |
|||||
|---|---|---|---|---|---|---|---|
| B1 | B2 | B3 | B4 | B0 | p -Value | ||
| 137.5 (135.9–139.1) |
Extension–flexion |
6.2
B2,B3,B4
(3.4–8.9) |
13.4
B1
(11.0–15.9) |
15.9
B1
(13.2–18.6) |
17.9
B0,B1
(13.2–22.6) |
6.2
B4
(− 2.0 to 14.5) |
< 0.001 |
| 54.4 (53.0–55.8) |
Radial–ulnar | 2.6 (0.8–4.5) |
3.3 (1.9–4.6) |
5.3 (3.7–6.9) |
5.0 (2.5–7.6) |
0.4 (− 4.0 to 4.8) |
< 0.05 |
| 162.4 (161.2–163.6) |
Supination–pronation |
2.6
B2,B4
(1.0–4.1) |
9.1
B1
(6.6–11.6) |
7.3 (5.1–9.4) |
9.0
B1
(6.2–11.2) |
0.8 (− 3.0 to 4.7) |
< 0.001 |
| 354.3 (351.2–357.3) |
Total ROM |
11.4
B2,B3,B4
(6.8–16.0) |
25.8
B1
(20.7–30.9) |
28.4
B0,B1
(23.3–33.5) |
32.0
B0,B1
(24.5–39.5) |
7.5
B3,B4
(− 4.0 to 19.0) |
< 0.001 |
Abbreviations: CI, confidence interval; ROM, range of motion.
Note: Loss of ROM in the injured wrist and average ROM in the uninjured wrist are presented in degrees. Mean and 95% CIs for mean are presented using analysis of variance. Significant Tukey's honest significant difference post hoc tests are presented as B0 to B4.
Surgical technique differed among the fracture classes ( Table 7 ). No B0 and only one B1 fracture were treated surgically. Intrafocal pinning was the most commonly used surgical method in B2 fractures, while volar plating was used in most cases for B3 and B4 fractures. According to our analyses, operative or conservative treatment did not affect QuickDASH, EQ-5D, or grip strength. A difference was seen in the radial–ulnar deviation arc where operated patients had a reduced arc of motion. There were no differences in outcome in relation to choice of surgical technique.
Table 7. Choice of treatment among the fracture classes.
| Treatment | Class | Total n (%) |
||||
|---|---|---|---|---|---|---|
| B0 n (%) |
B1 n (%) |
B2 n (%) |
B3 n (%) |
B4 n (%) |
||
| Kapandji | 0 | 0 | 30 (25) | 9 (9) | 8 (19) | 47 (14) |
| Volar plate | 0 | 1 (2) | 11 (9) | 16 (16) | 16 (38) | 44 (13) |
| Dorsal plating | 0 | 0 | 1 (1) | 4 (4) | 0 | 5 (1) |
| External fixation | 0 | 0 | 5 (4) | 11 (11) | 3 (7) | 19 (6) |
| Combined method | 0 | 0 | 1 (1) | 1 (1) | 2 (5) | 4 (1) |
| Conservative cast | 12 (100) | 63 (98) | 70 (59) | 57 (58) | 13 (31) | 215 (64) |
| Total | 12 | 64 | 118 | 98 | 42 | 334 |
Regarding complications during the first year, there were no significant differences among the Buttazzoni fracture classes ( Table 8 ). Of the complications, eight of the radial neuralgias were iatrogenic, four after intrafocal pinning, one after dorsal plating, two after external fixation, and one after combined external fixation and pinning. Three cases of CRPS were postoperative, one after intrafocal pinning, one after volar plate, and one after external fixation. Malunion was registered as a complication in the two patients requiring osteotomy. Otherwise, the effect of a malunion was reflected by the clinical outcome, that is, a malunion with a good clinical outcome did not have any negative impact on the results for that type of fracture. We had no postoperative infections and no nonunions.
Table 8. Complications registered among the fracture classes during the first year after DRF.
| Complications | B0 ( n = 12) |
B1 ( n = 64) |
B2 ( n = 118) |
B3 ( n = 98) |
B4 ( n = 42) |
|---|---|---|---|---|---|
| Carpal tunnel syndrome | 4 (33%) |
12 (19%) |
24 (21%) |
11 (11%) |
9 (21%) |
| EPL rupture | 0 | 2 (3%) |
3 (3%) |
0 | 1 (2%) |
| CRPS | 0 | 0 | 3 (3%) |
4 (4%) |
1 (2%) |
| Radial nerve paresthesia | 1 (8%) |
0 | 7 (6%) |
1 (1%) |
2 (5%) |
| Ulnar nerve paresthesia | 0 | 0 | 1 (1%) |
1 (1%) |
1 (2%) |
| Cold intolerance | 0 | 0 | 1 (1%) |
2 (2%) |
1 (2%) |
| Trigger finger | 0 | 0 | 0 | 4 (4%) |
0 |
| DRUJ instability | 0 | 0 | 0 | 4 (4%) |
0 |
| Malunion with osteotomy | 0 | 0 | 1 (1%) |
1 (1%) |
0 |
| Mb de Quervain | 0 | 0 | 1 (1%) |
1 (1%) |
0 |
Abbreviations: CRPS, complex regional pain syndrome; DRF, DRF, distal radius fracture; DRUJ, distal radioulnar joint; EPL, extensor pollicis longus.
Discussion
The present study showed that the initial position of the fracture was the parameter with the highest impact on the clinical outcome. Type of comminution and intra-articular involvement also affected outcome. The Buttazzoni's classification system could predict loss of ROM between noncomminuted fracture classes and comminuted fracture classes 1 year after the injury. Functional outcomes, studied with quickDASH, EQ-5D, and pain VAS were comparable among the Buttazzoni classes.
Known factors of importance for clinical outcome after DRF are the degree of displacement at union, 12 associated ligament injuries, 13 fracture comminution, 14 age, 9 14 15 patient education level, 16 socioeconomic status, 15 and injury compensation. 16 The relationship between the degree of displacement and clinical outcome has been questioned in the elderly. 17 18 19
In this study, we evaluated the individual fracture patterns, presented at the initial presentation of the fracture, and their predictive value on clinical outcome.
Initial displacement was associated with loss of total ROM, loss of grip strength, and a worse outcome in quickDASH and EQ-5D 1 year after the fracture. Our findings are in contrast with a study by Grewal et al 16 who found no correlation between initial degree of displacement and clinical outcome when evaluated using the patient-rated wrist evaluation (PRWE) score. In their study, only education level, injury compensation, and comorbidity were associated with outcome, while no injury characteristic, including the degree of initial fracture displacement, was found to significantly influence outcome. However, their study only included extra-articular DRF.
Dorsal comminution was associated with loss of flexion and forearm rotation. Dorsal comminution was also associated with a worse outcome in quickDASH at 1 year. Our findings regarding ROM concur with the results found by Cowie et al 14 who found that dorsal comminution was associated with loss of supination. In their study, dorsal comminution also predicted loss of grip strength.
Besides causing posttraumatic arthritis, 20 21 intra-articular involvement and the degree of intra-articular displacement have been reported to affect clinical outcome. 4 5 The impact of intra-articular union without a step is uncertain. 4 20 We found that intra-articular involvement correlated to a reduced flexion–extension arc and to a worse EQ-5D outcome. Our findings are partly in agreement with those reported by Karnezis et al 5 who found that the presence of a postoperative articular step affects the range of wrist extension, and those of Gliatis et al 4 who found that union with a step in the articular surface was associated with loss of wrist mobility. However, since we have analyzed initial intra-articular involvement and not final step or gap after union, this study only evaluates the importance of presence or absence of intra-articular involvement.
Volar comminution was associated with loss of extension. Our impression is that volarly comminuted fractures often displace with axial compression or volar angulation. In fractures with volar or dorsal comminution, there may be a shift in the arc of motion in a dorsal or volar direction without affecting the total arc of motion. Cowie et al 14 also found that volar comminution was associated with reduced extension. In their study, volar comminution was also associated with loss of flexion–extension arc and poorer functional score.
The older age group had a worse quickDASH. We had no baseline prefracture data and this may have influenced the outcome. 9 Women also scored worse than men, but women were older.
The well-established classification systems of DRF have failed to predict radiographic or clinical outcome in repeated studies. 3 4 5 15 Some of them contain numerous subtypes, which give rise to confusion and unsatisfactory reliability. This has led to requests for a new classification system for DRF, predictive of outcome, and easy to use. 2 22
The Buttazzoni's classification system was introduced in 2009 as a simple, all-inclusive, and clinically relevant radiological system of DRF. It included volar cortical comminution, overlooked by previous classifications, as a separate parameter owing to its anatomical and biomechanical importance as the “calcar” of the distal radius. 23 The utility of this system by testing its interobserver reliability and intraobserver reproducibility was previously reported. 7 In a prospective multicenter clinical trial, the ability of the system to predict radiological stability was tested, and revealed that fractures with initially nonacceptable radiographic alignment and cortical comminution were highly unstable. 8
In this study, we aimed to evaluate the effect of dorsal and volar comminution, intra-articular involvement, and initial displacement on clinical outcome. We also aimed to study whether different Buttazzoni classes would show different clinical outcome measures.
The treatment algorithm used was based on previous experience by Abramo et al 9 who demonstrated good outcome in both nonoperatively and operatively managed fractures. We advocated initial nonoperative treatment for high-energy trauma if the fracture was reducible and stability was maintained with cast immobilization. Furthermore, we allocated the patients into two groups: younger than and older than 60 years of age. The reason for this division is the favorable clinical outcome in patients > 60 years reported by Young and Rayan. 17 Furthermore, Lindau et al 21 who studied the influence of age on DRF found differences in trauma mechanisms, ligament injuries, and triangular fibrocartilage complex (TFCC) injuries among the age groups. Most fractures in the young age group were the result of a severe trauma and were associated with ligament injuries in a majority of cases. In this study, we excluded patients aged > 75 years, as studies have shown that elderly patients may tolerate even severe displacement. 17 19
In this study, B0 and B1 fractures showed minimal loss of motion compared with B2 to B4 fractures. The reason for this could be more soft tissue injuries in comminuted fractures. The latter were also more likely to require surgery to maintain stability; however, after adjusting for this, the fracture type was still the crucial factor for the loss of ROM in the injured wrist. Despite of these differences, the loss of ROM was not reflected by a worse quickDASH or EQ-5D in this study population.
Karnezis and Fragkiadakis 24 found that in DRF, patients grip strength, but not wrist extension and flexion, was predictive of better self-reported outcome using the PRWE score. Wilcke et al 12 reported a similar finding regarding reduced grip strength but also that extension and ulnar deviation correlated with a poorer DASH score. Chung and Haas 25 concluded that the optimal cutoff points that distinguish satisfaction from dissatisfaction occurred when patients had recovered 65% of their grip strength and 95% of their ROM. The differences in ROM between fracture classes in this study exceeded this limit but still did not affect the subjective outcome.
We chose to use quickDASH because it is commonly used and well validated in Sweden. However, quickDASH includes the overall functional status of the upper limb as a unit and therefore may not be responsive enough to compare functional outcome of DRF patients with small differences.
EQ-5D enables different dimensions of health to be combined to form an overall single index. We hypothesized that type of DRF could affect other aspects of health than those covered by the upper limb questionnaires. Initial displacement and intra-articular involvement affected EQ-5D negatively. Other fracture patterns and Buttazzoni fracture class showed comparable results among patients. These findings concur with that of Dolan et al 26 who evaluated health-related quality of life of patients with DRF. They found that the EQ-5D loss associated with DRF is ∼2%. They concluded that EQ-5D is unlikely to be sensitive enough and less appropriate to use when planning individual treatment.
The present study has a few limitations. The obtained results can be evaluated according to the treatment algorithm used, which is commonly advocated and has shown good results for both nonoperatively and operatively treated fractures. However, fracture displacement sometimes occurs later than 2 weeks, 8 27 especially in elderly with three or more Lafontaine instability criteria. 27 Therefore, patients should probably be monitored postreduction for displacement for longer than 2 weeks. 8 27
The type of metaphyseal comminution was recorded as absent or as present. We did not register size or number of the free-floating pieces of cortex. Thus, comminution was a purely qualitative measurement. It is likely that a more extensive comminution will have a greater impact on clinical outcome.
We have not analyzed patient education level, socioeconomic status, and injury compensation. We assume however that these factors are evenly distributed among fracture types. Also, the choice of treatment and the experience level of the surgeon may have influenced functional outcome. However, only small differences among surgical techniques have been described despite numerous studies.
Most authors agree that no classification system is adequate to determine treatment and predict outcomes unless interobserver and intraobserver reliabilities is substantial. This level of agreement was only reached for two of the three observers and only in younger patients when the classification was evaluated 2009. 7 Therefore, the reliability of the classification system may be a limitation. Despite this, the classification was highly predictive of fracture instability. 8
A limitation of the classification is that involvement of the DRUJ and the TFCC is not considered. Despite numerous studies, it is still unclear to recommend for or against concurrent surgical treatment of distal radioulnar joint instability in patients with operatively treated DRF. 28 In a prospective study with a 5-year follow-up, it was found that instability of the DRUJ did not worsen the outcome using the quickDASH questionnaire. 29
At the time of initiation of the study, there were no wrist-specific questionnaires validated in the Swedish language. The PRWE score was the most responsive instrument for evaluating the outcome in patients with DRFs in a review article of 2008. 30 The two available validated versions of the Swedish PRWE were unfortunately published after the initiation of this study. 31 32 However, both these studies showed a strong correlation between the Swedish PRWE and the DASH (Spearman's rho = 0.9 and 0.86, respectively).
These limitations are counterbalanced by the strengths of the study, which is a prospective multicenter trial with an adequate sample size and well-validated objective methods and outcome scores.
Initial position of the fracture was the most important parameter in predicting clinical outcome. Type of comminution and intra-articular involvement also affected clinical outcome. The Buttazzoni's classification was predictive for ROM 1 year after DRF. Buttazzoni class did not affect self-reported clinical outcomes.
Conflict of Interest None.
Note
The authors, their immediate families, and any research foundations with which they are affiliated have not received any financial supports or other benefits from any commercial entity related to the subject of this article.
References
- 1.van Staa T P, Dennison E M, Leufkens H G, Cooper C. Epidemiology of fractures in England and Wales. Bone. 2001;29(06):517–522. doi: 10.1016/s8756-3282(01)00614-7. [DOI] [PubMed] [Google Scholar]
- 2.Küçük L, Kumbaracı M, Günay H, Karapınar L, Ozdemir O. Reliability and reproducibility of classifications for distal radius fractures. Acta Orthop Traumatol Turc. 2013;47(03):153–157. doi: 10.3944/aott.2013.3038. [DOI] [PubMed] [Google Scholar]
- 3.Flinkkilä T, Raatikainen T, Hämäläinen M. AO and Frykman's classifications of Colles' fracture. No prognostic value in 652 patients evaluated after 5 years. Acta Orthop Scand. 1998;69(01):77–81. doi: 10.3109/17453679809002362. [DOI] [PubMed] [Google Scholar]
- 4.Gliatis J D, Plessas S J, Davis T R. Outcome of distal radial fractures in young adults. J Hand Surg [Br] 2000;25(06):535–543. doi: 10.1054/jhsb.2000.0373. [DOI] [PubMed] [Google Scholar]
- 5.Karnezis I A, Panagiotopoulos E, Tyllianakis M, Megas P, Lambiris E. Correlation between radiological parameters and patient-rated wrist dysfunction following fractures of the distal radius. Injury. 2005;36(12):1435–1439. doi: 10.1016/j.injury.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 6.Koval K, Haidukewych G J, Service B, Zirgibel B J. Controversies in the management of distal radius fractures. J Am Acad Orthop Surg. 2014;22(09):566–575. doi: 10.5435/JAAOS-22-09-566. [DOI] [PubMed] [Google Scholar]
- 7.Wadsten M A, Sayed-Noor A S, Sjödén G O, Svensson O, Buttazzoni G G. The Buttazzoni classification of distal radial fractures in adults: interobserver and intraobserver reliability. Hand (NY) 2009;4(03):283–288. doi: 10.1007/s11552-009-9163-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wadsten MÅ, Sayed-Noor A S, Englund E, Buttazzoni G G, Sjödén G O. Cortical comminution in distal radial fractures can predict the radiological outcome: a cohort multicentre study. Bone Joint J. 2014;96-B(07):978–983. doi: 10.1302/0301-620X.96B7.32728. [DOI] [PubMed] [Google Scholar]
- 9.Abramo A, Kopylov P, Tagil M. Evaluation of a treatment protocol in distal radius fractures: a prospective study in 581 patients using DASH as outcome. Acta Orthop. 2008;79(03):376–385. doi: 10.1080/17453670710015283. [DOI] [PubMed] [Google Scholar]
- 10.EuroQol Group.EuroQol–a new facility for the measurement of health-related quality of life Health Policy 19901603199–208. [DOI] [PubMed] [Google Scholar]
- 11.Mintken P E, Glynn P, Cleland J A. Psychometric properties of the shortened Disabilities of the Arm, Shoulder, and Hand Questionnaire (QuickDASH) and Numeric Pain Rating Scale in patients with shoulder pain. J Shoulder Elbow Surg. 2009;18(06):920–926. doi: 10.1016/j.jse.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 12.Wilcke M K, Abbaszadegan H, Adolphson P Y. Patient-perceived outcome after displaced distal radius fractures. A comparison between radiological parameters, objective physical variables, and the DASH score. J Hand Ther. 2007;20(04):290–298. doi: 10.1197/j.jht.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Lindau T, Runnquist K, Aspenberg P. Patients with laxity of the distal radioulnar joint after distal radial fractures have impaired function, but no loss of strength. Acta Orthop Scand. 2002;73(02):151–156. doi: 10.1080/000164702753671722. [DOI] [PubMed] [Google Scholar]
- 14.Cowie J, Anakwe R, McQueen M. Factors associated with one-year outcome after distal radial fracture treatment. J Orthop Surg (Hong Kong) 2015;23(01):24–28. doi: 10.1177/230949901502300106. [DOI] [PubMed] [Google Scholar]
- 15.Chung K C, Kotsis S V, Kim H M. Predictors of functional outcomes after surgical treatment of distal radius fractures. J Hand Surg Am. 2007;32(01):76–83. doi: 10.1016/j.jhsa.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 16.Grewal R, MacDermid J C, Pope J, Chesworth B M. Baseline predictors of pain and disability one year following extra-articular distal radius fractures. Hand (NY) 2007;2(03):104–111. doi: 10.1007/s11552-007-9030-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Young B T, Rayan G M. Outcome following nonoperative treatment of displaced distal radius fractures in low-demand patients older than 60 years. J Hand Surg Am. 2000;25(01):19–28. doi: 10.1053/jhsu.2000.jhsu025a0019. [DOI] [PubMed] [Google Scholar]
- 18.Beumer A, McQueen M M. Fractures of the distal radius in low-demand elderly patients: closed reduction of no value in 53 of 60 wrists. Acta Orthop Scand. 2003;74(01):98–100. doi: 10.1080/00016470310013743. [DOI] [PubMed] [Google Scholar]
- 19.Arora R, Gabl M, Gschwentner M, Deml C, Krappinger D, Lutz M. A comparative study of clinical and radiologic outcomes of unstable Colles type distal radius fractures in patients older than 70 years: nonoperative treatment versus volar locking plating. J Orthop Trauma. 2009;23(04):237–242. doi: 10.1097/BOT.0b013e31819b24e9. [DOI] [PubMed] [Google Scholar]
- 20.Knirk J L, Jupiter J B. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68(05):647–659. [PubMed] [Google Scholar]
- 21.Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults. A descriptive arthroscopic study in 50 patients. J Hand Surg [Br] 1997;22(05):638–643. doi: 10.1016/s0266-7681(97)80364-6. [DOI] [PubMed] [Google Scholar]
- 22.Kural C, Sungur I, Kaya I, Ugras A, Ertürk A, Cetinus E.Evaluation of the reliability of classification systems used for distal radius fractures Orthopedics 20103311801. Doi: 10.3928/01477447-20100924-14 [DOI] [PubMed] [Google Scholar]
- 23.Dhillon S S, Kumar AJ S, Sadaiyyappan V, Bassi R S, Shanahan D, Deshmukh S C. Anatomical study comparing the thickness of the volar and dorsal cortex of cadaveric adult distal radii using digital photography. Arch Orthop Trauma Surg. 2007;127(10):975–977. doi: 10.1007/s00402-007-0394-8. [DOI] [PubMed] [Google Scholar]
- 24.Karnezis I A, Fragkiadakis E G. Association between objective clinical variables and patient-rated disability of the wrist. J Bone Joint Surg Br. 2002;84(07):967–970. doi: 10.1302/0301-620x.84b7.12673. [DOI] [PubMed] [Google Scholar]
- 25.Chung K C, Haas A. Relationship between patient satisfaction and objective functional outcome after surgical treatment for distal radius fractures. J Hand Ther Off J Am Soc Hand Ther. 2009;22(04):302–307. doi: 10.1016/j.jht.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dolan P, Torgerson D, Kakarlapudi T K. Health-related quality of life of Colles' fracture patients. Osteoporos Int. 1999;9(03):196–199. doi: 10.1007/s001980050136. [DOI] [PubMed] [Google Scholar]
- 27.Nesbitt K S, Failla J M, Les C. Assessment of instability factors in adult distal radius fractures. J Hand Surg Am. 2004;29(06):1128–1138. doi: 10.1016/j.jhsa.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 28.Lichtman D M, Bindra R R, Boyer M I et al. American Academy of Orthopaedic Surgeons clinical practice guideline on: the treatment of distal radius fractures. J Bone Joint Surg Am. 2011;93(08):775–778. doi: 10.2106/JBJS.938ebo. [DOI] [PubMed] [Google Scholar]
- 29.Scheer J H, Adolfsson L E. Radioulnar laxity and clinical outcome do not correlate after a distal radius fracture. J Hand Surg Eur Vol. 2011;36(06):503–508. doi: 10.1177/1753193411403690. [DOI] [PubMed] [Google Scholar]
- 30.Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop. 2008;32(01):1–6. doi: 10.1007/s00264-007-0368-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilcke M T, Abbaszadegan H, Adolphson P Y. Evaluation of a Swedish version of the patient-rated wrist evaluation outcome questionnaire: good responsiveness, validity, and reliability, in 99 patients recovering from a fracture of the distal radius. Scand J Plast Reconstr Surg Hand Surg. 2009;43(02):94–101. doi: 10.1080/02844310902734598. [DOI] [PubMed] [Google Scholar]
- 32.Mellstrand Navarro C, Ponzer S, Törnkvist H, Ahrengart L, Bergström G.Measuring outcome after wrist injury: translation and validation of the Swedish version of the patient-rated wrist evaluation (PRWE-Swe) BMC Musculoskelet Disord 201112171. Doi: 10.1186/1471-2474-12-171 [DOI] [PMC free article] [PubMed] [Google Scholar]


