Abstract
Purpose To determine the reliability of wrist range of motion (WROM) measurements based on digital photographs taken by patients at home compared with traditional measurements done in the office with a goniometer.
Methods Sixty-nine postoperative patients were enrolled in this study at least 3 months postoperatively. Active and passive wrist flexion/extension and radial/ulnar deviation were recorded by one of the two attending surgeons with a 1-degree resolution goniometer at the last postoperative office visit. Patients were provided an illustrated instruction sheet detailing how to take digital photographic images at home in six wrist positions (active and passive flexion/extension, and radial/ulnar deviation). Wrist position was measured from digital images by both the attending surgeons in a randomized, blinded fashion on two separate occasions greater than 2 weeks apart using the same goniometer. Reliability analysis was performed using the intraclass correlation coefficient to assess agreement between clinical and photography-based goniometry, as well as intra- and interobserver agreement.
Results Out of 69 enrolled patients, 30 (43%) patients sent digital images. Of the 180 digital photographs, only 9 (5%) were missing or deemed inadequate for WROM measurements. Agreement between clinical and photography-based measurements was “almost perfect” for passive wrist flexion/extension and “substantial” for active wrist flexion/extension and radial/ulnar deviation. Inter- and intraobserver agreement for the attending surgeons was “almost perfect” for all measurements.
Discussion This study validates a photography-based goniometry protocol allowing accurate and reliable WROM measurements without direct physician contact. Passive WROM was more accurately measured from photographs than active WROM. This study builds on previous photography-based goniometry literature by validating a protocol in which patients or their families take and submit their own photographs.
Clinical Relevance Patient-performed photography-based goniometry represents an alternative to traditional clinical goniometry that could enable longer-term follow-up, overcome travel-related impediments to office visits, improve convenience, and reduce costs for patients.
Keywords: wrist goniometry, wrist range of motion, digital images, distance learning, remote access
Clinical goniometric measurement of wrist range of motion (WROM) is an important tool for hand surgeons and occupational therapists in the assessment of patients with hand and wrist conditions. Normative standards for WROM as well as range of motion (ROM) requirements for performance of activities of daily living have been described previously. 1 WROM has traditionally been measured with a manual goniometer; however, limitations in this technique have been reported. 2 3 Sources of error for measurements made by clinical goniometry include incorrect goniometer placement, incorrect anatomic landmark identification, and variable force applied for passive ROM measurements. 4 5 Alternative goniometry techniques have been studied to achieve improved accuracy, precision, and/or convenience, including radiograph-based measurements, visual estimation, three-dimensional (3D) motion analysis, smartphone-assisted measurements, and photography-based measurements. 4 6 7 8 9 Additionally, traditional assessment of WROM necessitates an office visit; long-term interval visits after the acute postoperative period may be difficult or impossible secondary to insurance issues, travel distances, patient relocation, inconvenience, and cost.
Blonna et al validated a photography-based goniometry method for measuring elbow ROM. 10 In this study of elbow contracture patients, clinical goniometry measurements were compared with measurements taken from pictures of the patients in full elbow extension and flexion. The authors concluded that photography-based goniometry was accurate and reliable for measuring elbow ROM. Another study concluded that photography-based goniometry for measuring knee ROM has excellent intra- and interobserver reliability and potentially offers a superior method of measurement over traditional goniometry. 11 Both these studies examined the use of photography-based goniometry in joints with a simple arc of motion in one plane (i.e., the knee and elbow). The wrist, however, is a multiaxial joint with multiple complex planes of motion: flexion/extension, radial/ulnar deviation, coupled motion, and circumduction. 12 Crasto et al recently reported that photography-based goniometry of the wrist is accurate and has improved inter-rater reliability compared with clinical goniometry. 13 Taken together, photography-based goniometry has been validated in the knee, elbow, and wrist, and represents a promising alternative to traditional clinical goniometry.
It is important to note that in each of the previously cited studies on photography-based goniometry, photographs were taken by member(s) of the research team. Validating a protocol in which patients take their own photographs at home would greatly increase the potential value and applicability of photography-based goniometry, particularly in regards to remote data acquisition and distance medical care. The purpose of this study was to test the reliability of WROM measurements based on digital photographs taken by patients at home. We hypothesized that photography-based WROM measurements would be as reliable as traditional clinical goniometry.
Materials and Methods
This study was approved by the Hospital for Special Surgery Institutional Review Board (#2013–129). Study participants were consented and enrolled from March 2014 to September 2015 according to the institution's IRB-approved protocol. Sixty-nine postoperative patients, whose WROM would be measured routinely in the office following their wrist surgery, were enrolled at least 3 months postoperatively by one of the two attending surgeons (S.K.L. and S.W.W.). Surgical treatments included a broad range of repair or reconstruction for common wrist injuries, arthritis, and tendinopathy. Patients with painful WROM (visual analog scale [VAS] > 4), patients younger than 18, patients who had not yet reached a stable postoperative plateau, and/or patients who did not have a family member or friend available at home to assist with photography were excluded.
The following demographic data were collected from patients during the enrollment and consent process: age, sex, handedness, height, weight, diagnosis, surgical date, and type of surgery. Active and passive wrist flexion/extension and radial/ulnar deviation were recorded by the attending surgeon at the preceding postoperative office visit with a 1-degree resolution goniometer using methodology previously described. 14 Patients were provided an illustrated instruction sheet detailing how to take digital photographs in the six positions required for WROM measurements (i.e., active and passive flexion/extension and radial/ulnar deviation) ( Fig. 1 ). The illustrated instruction sheet was developed and optimized in a pilot study (abstract presented at the American Association for Hand Surgery 2015 Annual Meeting) 15 ( Supplementary Material , available in the online version). Patients e-mailed de-identified digital photographs to an HIPAA-compliant hospital research server. If an e-mail was not received within 2 weeks of the office visit, two phone calls were made to remind the patient by a research assistant, which resulted in either a phone conversation or voicemail message. The mean response time was 4 weeks (ranging from 1 day to 16 weeks).
Fig. 1.
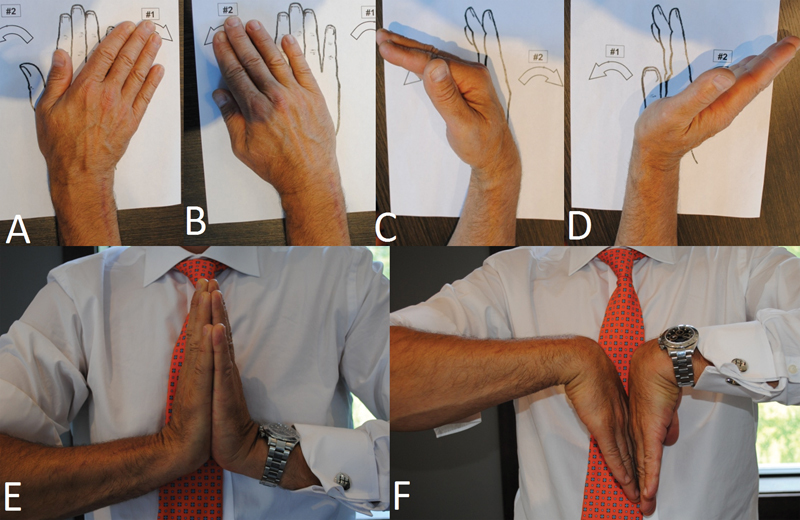
Digital photographs demonstrating this 51-year-old man's range of motion 20 months status post-distal radius osteotomy for malunion and 8 months status post-right ulnar shortening osteotomy. ( A ) Ulnar deviation, ( B ) radial deviation, ( C ) active flexion, ( D ) active extension, ( E ) passive extension, and ( F ) passive flexion.
De-identified photographs were reviewed by both the attending surgeons in a randomized, blinded fashion on two separate occasions greater than 2 weeks apart using the same goniometer. Both the attending surgeons reviewed all patient photographs (i.e., not just those from patients he measured in his office) to determine interobserver reliability of photography-based goniometry.
Reliability analysis was performed using the intraclass correlation coefficient (ICC) to assess agreement between clinical and photography-based WROM goniometry, as well as intra- and interobserver agreement for photography-based measurements. ICC agreement was classified according to previously published criteria: “almost perfect” (0.81–1), “substantial” (0.61–0.80), “moderate” (0.41–0.60), “fair” (0.21–0.40), “slight,” or “poor” (0–0.20). 16 An a priori power analysis was performed to determine the size of the study population.
Results
Out of 69 enrolled patients, 30 patients sent digital images (43% response rate). Surgical indications for the enrolled patients included distal radius fracture (19), scaphoid fracture (10), scapholunate interosseous ligament tear (9), four corner fusion (7), scaphoid nonunion (5), ulnar shortening osteotomy (4), basal joint arthroplasty (4), triangular fibrocartilage complex tear (2), distal ulna fracture (1), distal radius osteotomy (1), radial shortening osteotomy (1), hook of hamate fracture (1), partial wrist fusion (1), proximal row carpectomy (1), extensor carpi ulnaris injury/triangular fibrocartilage complex tear (1), distal radius fracture/scaphoid fracture (1), and distal radius fracture/distal ulna fracture (1).
Of the 180 digital photographs, only 9 (5%) were missing or deemed inadequate due to inappropriate vantage point and/or lack of minimum anatomic landmarks required for WROM measurements ( Fig. 2 ). Agreement between clinical and photography-based measurements was “almost perfect” for passive wrist flexion/extension ( p < 0. 01) and “substantial” for active wrist flexion/extension and radial/ulnar deviation ( p < 0.01) ( Table 1 ). Interobserver agreement between the two attending surgeons for all six photography-based measurements was “almost perfect” ( p < 0.01) ( Table 2 ). Intraobserver agreement for both the attending surgeons for all six photography-based measurements was “almost perfect” ( p < 0.01) ( Table 3 ).
Fig. 2.
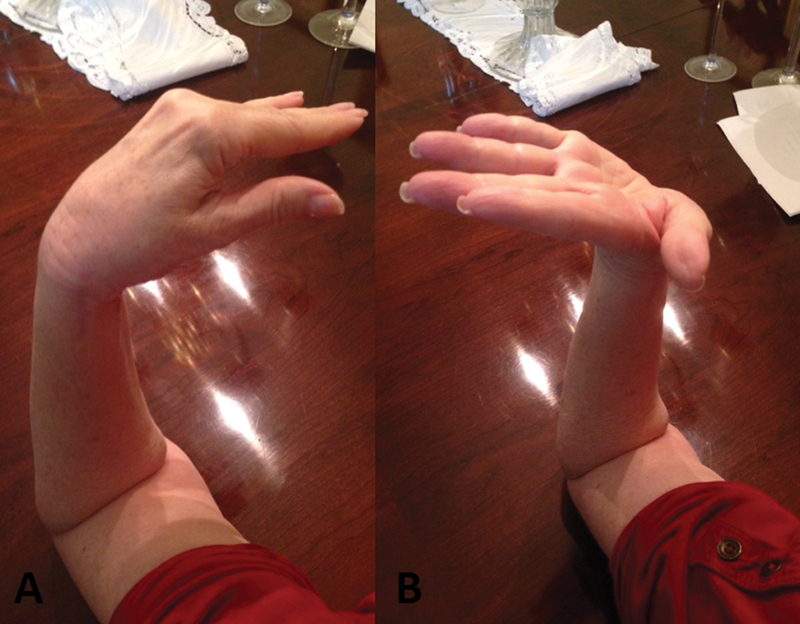
Digital photographs that were deemed inadequate for measurement of ( A ) active flexion and ( B ) active extension.
Table 1. Reliability analysis using ICC between clinical and photography-based wrist range of motion measurements.
| Measurement | ICC | p Value |
|---|---|---|
| Wrist flexion (active) | 0.72 | < 0.01 |
| Wrist extension (active) | 0.74 | < 0.01 |
| Wrist flexion (passive) | 0.91 | < 0.01 |
| Wrist extension (passive) | 0.85 | < 0.01 |
| Ulnar deviation | 0.63 | < 0.01 |
| Radial deviation | 0.75 | < 0.01 |
Abbreviation: ICC, intraclass correlation coefficient.
Table 2. Interobserver reliability analysis using ICC between two attending surgeons' photography-based wrist range of motion measurements.
| Measurement | ICC | p Value |
|---|---|---|
| Wrist flexion (active) | 0.98 | < 0.01 |
| Wrist extension (active) | 0.91 | < 0.01 |
| Wrist flexion (passive) | 0.97 | < 0.01 |
| Wrist extension (passive) | 0.91 | < 0.01 |
| Ulnar deviation | 0.92 | < 0.01 |
| Radial deviation | 0.86 | < 0.01 |
Abbreviation: ICC, intraclass correlation coefficient.
Table 3. Intraobserver reliability analysis using ICC for two attending surgeons' photography-based wrist range of motion measurements.
| Measurement | ICC (Attending 1) |
P value | ICC (Attending 2) |
p Value |
|---|---|---|---|---|
| Wrist flexion (active) | 0.98 | < 0.01 | 0.98 | < 0.01 |
| Wrist extension (active) | 0.91 | < 0.01 | 0.96 | < 0.01 |
| Wrist flexion (passive) | 0.93 | < 0.01 | 0.98 | < 0.01 |
| Wrist extension (passive) | 0.91 | < 0.01 | 0.96 | < 0.01 |
| Ulnar deviation | 0.93 | < 0.01 | 0.91 | < 0.01 |
| Radial deviation | 0.92 | < 0.01 | 0.94 | < 0.01 |
Abbreviation: ICC, intraclass correlation coefficient.
Discussion
The purpose of this study was to test the reliability of WROM measurements based on digital photographs taken by patients at home. We demonstrated excellent agreement between photography-based WROM measurements and traditional clinical goniometry measurements. It should be noted that passive WROM was more accurately measured from photographs than active WROM. Inter- and intraobserver agreement was excellent for all WROM measurements for both the attending surgeons. Thus, our study validates a protocol allowing accurate and reliable WROM measurements without direct physician contact.
ROM measurements via traditional clinical goniometry may be limited for reasons such as incorrect goniometer placement. 4 5 Alternative goniometry techniques have been studied to achieve improved accuracy, precision, and/or convenience, including radiograph-based measurements, visual estimation, 3D motion-capture registration, smartphone-assisted measurements, and photography-based measurements. 4 6 7 8 9 12 Photography-based goniometry is particularly appealing given the potential to be performed independently by patients. Previous studies validating photography-based goniometry for the elbow, knee, and wrist utilized photographs taken by members of the clinical research team in the office setting. 10 11 13 Thus, our ability to extrapolate these studies' conclusions is limited by the fact that the photographs were taken by researchers with relevant clinical knowledge. This study is the first to assess patient-performed photography-based goniometry based on written instructions as a potential alternative to traditional clinical goniometry.
This study has several important limitations. First, our response rate was 43%; thus, the success of our study protocol may have been overestimated via selection bias. However, patients had no incentive to follow the research protocol and our IRB limited contact after the office visit to two phone calls (which sometimes only resulted in a voicemail message). Second, the mean time interval between clinical examination and photograph receipt was 4 weeks (ranging from 1 day to 16 weeks). This delay may have led to an underestimation of agreement between clinical and photography-based measurements due to potential WROM changes with time. Third, pronation and supination are important components of WROM, but they were not included in this study. Interestingly, unlike flexion/extension and radial/ulnar deviation, goniometric measurement techniques for pronation and supination have not been formally studied and have been described as relatively error-prone. 3 14 That being said, pronation and supination have been reliably measured in recent studies using photography-based goniometry and smartphone-assisted measurements. 8 13 Finally, the illustrated instruction sheet provided to patients has room for further optimization. In particular, integration of video displays, online accessibility, and/or smartphone accessibility may have improved patient response rate and/or protocol accuracy.
In summary, this study validates a patient-performed photography-based goniometry protocol to enable accurate and reliable WROM measurements from a remote location. Interestingly, a remote hand therapy program for patients with chronic hand conditions, such as systemic sclerosis, has been previously described. 17 Such protocols may have significant benefits over traditional in-office alternatives enabling longer-term (or more frequent) patient follow-up, enhanced patient convenience, the ability to overcome travel or insurance impediments to follow-up, and the potential for cost savings.
Acknowledgment
The authors wish to thank Joseph T. Nguyen, BS, MPH (Healthcare Research Institute, Hospital for Special Surgery), for statistical support.
Funding None. Conflict of Interest None.
Note
The study was approved by Hospital for Special Surgery Institutional Review Board (#2013–129).
Supplementary Material
References
- 1.Ryu J Y, Cooney W P, III, Askew L J, An K N, Chao E Y. Functional ranges of motion of the wrist joint. J Hand Surg Am. 1991;16(03):409–419. doi: 10.1016/0363-5023(91)90006-w. [DOI] [PubMed] [Google Scholar]
- 2.Boone D C, Azen S P, Lin C M, Spence C, Baron C, Lee L. Reliability of goniometric measurements. Phys Ther. 1978;58(11):1355–1360. doi: 10.1093/ptj/58.11.1355. [DOI] [PubMed] [Google Scholar]
- 3.Flowers K R, Stephens-Chisar J, LaStayo P, Galante B L. Intrarater reliability of a new method and instrumentation for measuring passive supination and pronation: a preliminary study. J Hand Ther. 2001;14(01):30–35. doi: 10.1016/s0894-1130(01)80022-3. [DOI] [PubMed] [Google Scholar]
- 4.Blonna D, Zarkadas P C, Fitzsimmons J S, O'Driscoll S W. Accuracy and inter-observer reliability of visual estimation compared to clinical goniometry of the elbow. Knee Surg Sports Traumatol Arthrosc. 2012;20(07):1378–1385. doi: 10.1007/s00167-011-1720-9. [DOI] [PubMed] [Google Scholar]
- 5.Fish D R, Wingate L. Sources of goniometric error at the elbow. Phys Ther. 1985;65(11):1666–1670. doi: 10.1093/ptj/65.11.1666. [DOI] [PubMed] [Google Scholar]
- 6.Chapleau J, Canet F, Petit Y, Laflamme G Y, Rouleau D M. Validity of goniometric elbow measurements: comparative study with a radiographic method. Clin Orthop Relat Res. 2011;469(11):3134–3140. doi: 10.1007/s11999-011-1986-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferriero G, Vercelli S, Sartorio F et al. Reliability of a smartphone-based goniometer for knee joint goniometry. Int J Rehabil Res. 2013;36(02):146–151. doi: 10.1097/MRR.0b013e32835b8269. [DOI] [PubMed] [Google Scholar]
- 8.Kim T S, Park D D, Lee Y B et al. A study on the measurement of wrist motion range using the iPhone 4 gyroscope application. Ann Plast Surg. 2014;73(02):215–218. doi: 10.1097/SAP.0b013e31826eabfe. [DOI] [PubMed] [Google Scholar]
- 9.Hillstrom H J, Garg R, Kraszewski A et al. Development of an anatomical wrist joint coordinate system to quantify motion during functional tasks. J Appl Biomech. 2014;30(04):586–593. doi: 10.1123/jab.2011-0094. [DOI] [PubMed] [Google Scholar]
- 10.Blonna D, Zarkadas P C, Fitzsimmons J S, O'Driscoll S W. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21(01):29–35. doi: 10.1016/j.jse.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 11.Naylor J M, Ko V, Adie Set al. Validity and reliability of using photography for measuring knee range of motion: a methodological study BMC Musculoskelet Disord 20111277. Doi: 10.1186/1471-2474-12-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garg R, Kraszewski A P, Stoecklein H H et al. Wrist kinematic coupling and performance during functional tasks: effects of constrained motion. J Hand Surg Am. 2014;39(04):634–6420. doi: 10.1016/j.jhsa.2013.12.031. [DOI] [PubMed] [Google Scholar]
- 13.Crasto J A, Sayari A J, Gray R R, Askari M. Comparative analysis of photograph-based clinical goniometry to standard techniques. Hand (NY) 2015;10(02):248–253. doi: 10.1007/s11552-014-9702-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carter T I, Pansy B, Wolff A L et al. Accuracy and reliability of three different techniques for manual goniometry for wrist motion: a cadaveric study. J Hand Surg Am. 2009;34(08):1422–1428. doi: 10.1016/j.jhsa.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Trehan S K, Shifflett G D, Johnsen P H, Lee S K, Wolfe S W.Photography-based goniometric method for measuring wrist range of motion: Feasibility Study, AAHS 2015 Annual Meeting (poster presentation)Atlantis Paradise Island, BAH. January 21–24, 2015
- 16.Landis J R, Koch G G. The measurement of observer agreement for categorical data. Biometrics. 1977;33(01):159–174. [PubMed] [Google Scholar]
- 17.Wolff A, Weinstock-Zlotnick G, Gordon J. SSc management—in person appointments and remote therapy (SMART): a framework for management of chronic hand conditions. J Hand Ther. 2014;27(02):143–150. doi: 10.1016/j.jht.2013.11.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


