Abstract
Past studies examining the relationship between preparedness for loss and bereavement voutcomes among caregivers of spouses/partners with life-limiting illness did not adequately account for preloss caregiver attributes that could potentially confound the relationship. Using a sample of spouse/partner cancer caregivers (N = 226), we examined how preloss caregiver attributes were associated with how prepared one felt for loss, and their role in the relationship between preparedness and later bereavement outcomes. Nearly half reported they were not emotionally prepared, and 35% were not prepared for the practical challenges associated with the loss. Although attributes such as depression, anxiety, competence in daily activities, and financial adequacy were associated with both preparedness and bereavement outcomes, regression analyses revealed that preparedness remained the strongest predictor in all models. We suggest that early interventions enhancing caregivers’ preparedness for loss may hold considerable promise for improved bereavement outcome.
Keywords: Spousal/partner loss, Preparedness, Caregiver anxiety, Cancer bereavement
While the news of a life-limiting cancer diagnosis is distressing and disruptive for patients, it also profoundly affects spouses or partners providing their care. The “assumptive world” (Parkes, 1971) regarding what was once considered reliable, predictable, and even controllable is forever changed and often replaced by uncertainty, anxiety, and dread about the impending loss of a future life together (Johansson & Grimby, 2012; Moon, 2015; Olson, 2014; Rando, 2000). In addition to emotional reactions, there are also significant daily living or practical life changes that occur (Hauksdottir, Steineck, Furst, & Valdimarsdottir, 2010; Hauksdottir, Valdimarsdottir, Furst, Onelov, & Steineck, 2010). Thus, a diagnosis of a life-limiting illness has a tremendous impact not only on the patient, but also the caregiver who is balancing the challenges of providing care while additionally expecting the loss that will follow (Barry, Kasl, & Prigerson, 2002; Fowler, Hansen, Barnato, & Garand, 2013).
Preparedness for Loss
The long-held view that anticipating an expected loss helps the griever to adjust more effectively after the death has been seriously challenged (Nielsen, Neergaard, Jensen, Bro, & Guldin, 2016). Having a forewarning period (the time between diagnosis of a life-limiting illness and death) does not necessarily mean that caregivers will prepare for the consequences (Clark, Brethwaite, & Gnesdiloff, 2011; Hebert, Dang, & Schulz, 2006). Indeed, past studies have reported that many bereaved caregivers reported being unprepared for the death and its aftermath (Caserta, Utz, & Lund, 2013; Clark et al., 2011; Hebert, Dang, et al., 2006; Nielsen et al., 2016; Tabler et al., 2015).
Preparedness is defined as “a caregiver’s perception of his/her readiness for the death” (Hebert, Prigerson, Schulz, & Arnold, 2006, pp. 1165-1166). In the case of a life-limiting illness, this would involve being ready to cope with the psychosocial, spiritual, and practical challenges of the patient’s illness, as well as managing medical concerns such as goals of care, treatment preferences, and end-of-life planning (Hauksdottir, Steineck, et al., 2010; Hauksdottir, Valdimarsdottir, et al., 2010; Hebert, Dang, et al., 2006). Carr (2012) suggests that readiness can consist of two components: emotional preparedness, which involves bracing for a broad range of emotions related to the loss itself and its finality; and practical preparedness, or readiness to address the necessary changes in daily life such as assuming new household, financial and other daily responsibilities, as well as making funeral arrangements and resolving estate matters.
A recent review (Nielsen et al., 2016) identified consistent evidence that a caregiver’s lack of preparedness was associated with poorer bereavement outcomes following the death of the patient (Hauksdottir, Valdimarsdottir, et al., 2010; Hebert, Dang, et al., 2006; Henriksson & Arestedt, 2013). Most notably, caregivers who felt less prepared reported greater levels of depressive symptoms (Hebert, Dang, et al., 2006; Schulz, Boerner, Klinger, & Rosen, 2015) and experienced a higher risk of complicated grief (Barry et al., 2002; Schulz et al., 2015; Tsai et al., 2015). These findings point to the need for a greater understanding of factors related to preparedness so that those at greatest risk for adverse consequences can be targeted for preparedness-focused intervention.
Preloss Caregiver Attributes
While existing empirical evidence has documented the effects of preparedness on bereavement outcomes, equally important are those preloss caregiver attributes that distinguish those who are more versus less prepared for the loss. For the purposes of this investigation, these attributes represent caregivers’ personal and psychoemotional characteristics and resources that are in effect prior to the loss. Many of these factors, however, could likewise have a role in bereavement outcomes.
Demographic comparisons in bereavement outcomes and bereavement experiences have been explored for some time (see Carr, Nesse, & Wortman, 2006). A recent body of literature, however, has begun to suggest demographic differences in how well caregivers are prepared for the loss of their ill spouse or partner. For example, being less prepared was more common among men (Henriksson & Arestedt, 2013) and the less educated (Hebert, Dang, et al., 2006). Reports from a Swedish study suggested that the adverse effects of low preparedness were more pronounced among widowers age 61 years or less versus those in the sample who were older (Asgeirsdottir, Valdimarsdottir, Furst, Steineck, & Hauksdottir, 2013; Hauksdottir, Valdimarsdottir, et al., 2010). This pattern is consistent with theoretical work suggesting that life experiences that were successfully navigated earlier in life could predispose one to be better equipped for the challenges posed by subsequent stressful situations (Aldwin & Levenson, 2004). It could also be argued that an inadequate financial situation is a potential predisposing factor to lower preparedness (Aneshensel, Botticello, & Yamamoto-Mitani, 2004). An important feature of practical preparedness is to ensure that household financial affairs are in order (Carr, 2012; Hauksdottir, Valdimarsdottir, et al., 2010; Steinhauser et al., 2001), which could be difficult if caregivers perceive their financial situation as inadequate and their future financial security as uncertain (Hebert, Schulz, Copeland, & Arnold, 2009).
In addition to demographic factors, preparedness may also be influenced by the extent to which tasks of daily living are shared between the caregiver and care recipient. The relationships between spouses or intimate partners, particularly among those in older cohorts who have been in long-standing relationships, are often characterized by fairly defined divisions of labor regarding household or familial responsibilities (Utz, 2006). As the disease progresses, it may become necessary for some caregivers to assume a greater share of responsibilities that were once those of their ill spouse or partner, which could require skills in time management, flexibility, and obtaining outside assistance if needed. This could be increasingly challenging for caregivers who depended on their ill companions to tend to these matters, and are thus less experienced in meeting these responsibilities themselves (Carr, 2004). In addition to adversely affecting caregivers’ preparedness, deficits in these skills could put them at risk for more problematic bereavement outcomes. Previous evidence has documented that widow(er)s who are less capable in a variety of daily living skills adjust more poorly to the loss of their spouse/partner (Lund, Caserta, Dimond, & Shaffer, 1989; Utz, Lund, Caserta, & de Vries, 2011).
Finally, the emotional and practical challenges, as well as the burden experienced by caregivers of those with life limiting illnesses such as cancer, may predispose them to high levels of depression and anxiety (Hudson, Thomas, Trauer, Remedios, & Clarke, 2011; Payne, Smith, & Dean, 1999; Schulz et al., 2003), which could exacerbate a lack of preparedness. In other words, those who are more distressed are less likely to take actions necessary for them to become more prepared (Hebert et al., 2009). Furthermore, a high level of distress during caregiving often persists beyond the patient’s death and becomes a risk factor itself for adverse bereavement outcomes (Nielsen et al., 2016; Romero, Ott, & Kelber, 2014).
As described above, preloss caregiver attributes arguably can be influential in both preparedness and the psychoemotional and daily living consequences associated with the loss. What is not yet determined is if this contributes to a spurious relationship between preparedness and outcomes. It is important, therefore, to disentangle the role of these preloss factors from this relationship – which past studies have not addressed.
Purpose of Study
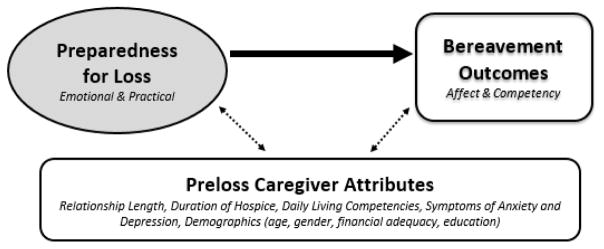
The purpose of this investigation, therefore, was two-fold (as illustrated in Figure 1): First, we examined the relative influence of preloss caregiver attributes on preparedness among cancer caregivers. Second, we examined to what extent preparedness explains early bereavement outcomes when accounting for these attributes. A better causal understanding of these relationships will help to provide more conceptual clarity regarding the role of preloss caregiver factors in preparedness as well as inform more effectively targeted interventions for those who are at greater risk for adverse bereavement outcomes.
Figure 1.
Conceptual Model Linking Preparedness, Preloss Caregiver Attributes, and Bereavement Outcomes
Methods
Data
The findings reported here used data from a subsample of spouse/partner cancer caregivers, ages 45 and older, from the Cancer Caregiver Study (CCS), a larger program-project study consisting of three interrelated projects focused on enhancing the well-being of cancer caregivers using hospice services (Mooney et al., 2013). One study examined the effectiveness of an automated telephone-delivered symptom management system on the well-being of the caregiver, while the second was an observational study examining communication patterns between caregivers and hospice staff during the in-home visits. The primary purpose of the third study, which included the subsample used in this investigation, was to test an individually tailored bereavement intervention after the patient had died (Caserta, Lund, Utz, & Tabler, 2016). The purpose of this investigation is addressed using data obtained from the caregivers while their spouses’/partners’ were receiving hospice care and then after 2–3 months following their deaths, but prior to when the intervention was administered.
Sampling Procedure
Potential participants were identified by hospices in 4 metropolitan areas spanning the northeastern United States, upper Midwest, the Intermountain West, and the Pacific Northwest. All participants were identified as the primary caregiver to a family member with a life limiting late-stage cancer diagnosis who was receiving hospice care. Caregivers needed to speak English and be cognitively able to participate in all aspects of the project. The subsample for this study consists of those CCS caregivers who were spouses/partners to the patient in the home. Those caregivers who were adult children, siblings, or friends to the dying patient, although part of the larger CCS, were not included in the bereavement study since several aspects of the bereavement experiences for spouses/partners compared to others can be notably different (Stroebe, Hansson, Schut, & Stroebe, 2008). Project staff contacted potential participants by phone to obtain a preliminary agreement for a home visit in order to obtain formal consent, enrollment, and a baseline assessment. Of the 7,419 potential caregivers the hospices initially screened, 868 spouses/partners were identified as eligible for this study. However, 123 were not contacted due to an invalid phone number, or the patient had already died or was actively dying. Of those who were contacted, 510 (68%) declined, resulting in 235 spouse/partners who were enrolled. The most common reasons for refusal were that the caregivers were too busy or overwhelmed to participate, or simply not interested. Nine of the 235 who were enrolled dropped prior to baseline resulting in an analytical sample of 226 caregivers who were spouses or partners to the patient (representing almost 50% of the entire CCS sample).
Measures
Unless otherwise indicated, data were obtained from self-administered questionnaires completed by the caregiver. Questionnaires were completed upon the caregivers’ enrollment into the study (approximately the time when the patient was admitted to hospice) and then approximately 2–3 months after the patient had died. These two time points define the caregiving and the bereavement phases, respectively.
Preparedness
Preparedness was assessed by two items obtained post death, each according to a 1 (very little if at all) to 5 (very prepared) Likert scale: “Emotionally, how prepared do you think you were for the death of your spouse/partner?” (Emotional preparedness) and “In terms of your daily life, how prepared were you for the death of your spouse/partner - for example, taking on new responsibility, planning ahead, funeral preparation, etc.?” (Practical preparedness). For most analyses the two items were combined to create an Overall preparedness scale ranging from 2 (low) to 10 (high), producing a Cronbach alpha equal to 0.81.
Demographic information
Demographic information was obtained from baseline surveys administered to caregivers upon their enrollment into the study. Variables included age, gender, length of marital/partner relationship, highest level of education completed, and perceived financial adequacy (1 = “not very good,” 2 = “comfortable,” and 3 = “more than adequate to meet my needs”). Because a previous study found that length of hospice stay was correlated with preparedness (Bradley et al., 2004), it was obtained from hospice records and accounted for in the analyses. We explored age as both a linear measurement (in years), as well as a dichotomous variable indicating those who experienced the transition from caregiving to bereavement at a younger age (from 45–65 years) and those who experienced it at a more normative age (65+ years). Results were substantively similar across these two measurement approaches; we use the linear measure of age in all analyses reported here.
Caregiver anxiety
Caregiver anxiety was measured using 7 items that comprise the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS - Zigmond & Snaith, 1983). Each item is scored along a 0 to 3 Likert format and then summed for a total score with a possible range of 0 to 21, where a higher value is indicative of a greater level of anxiety. Scores that are 11 or higher indicate a clinical level of anxiety. Multiple studies have demonstrated evidence of reliability (mean alpha = .83) and concurrent validity; psychological function among cancer caregivers has been predicted with a specificity of 0.78 and a sensitivity of 0.9 (Bjelland, Dahl, Haug, & Neckelmann, 2002).
Perceived daily living skills
Perceived daily living skills were assessed both at baseline and post death using two subscales from the Perceived Self-Care and Daily Living Competencies Scale: (1) active coping, which refers to ability to address the challenges of daily living such as adapting to change, organizing time, planning ahead, and identifying and utilizing sources of help to meet one’s needs, and (2) managing household affairs, which includes the typical skills needed to maintain a home and manage household finances (Caserta, Lund, & Obray, 2004; Utz et al., 2011). For each item, the caregivers reported their perceived ability in a particular skill ranging from 1 (not at all) to 3 (a lot). The active coping subscale (7 items) ranged from 7 to 21and managing household affairs (10 items) ranged from 10 to 30, with a higher score indicating a greater perceived competency level. Utz et al. (2011) reported an alpha coefficient equal to .85 for each subscale.
Depression
Depression was assessed at both baseline and post-death data collections, using the Geriatric Depression Scale Short Form (GDS-SF - Sheikh & Yesavage, 1986). The GDS-SF consists of 15 yes/no items that were summed for a total score ranging from 0 to 15. A higher score indicates a greater level of depressive symptomatology; a score greater than 4 has been established as a clinical cut-off.
Complicated/prolonged grief symptoms
Complicated/prolonged grief symptoms were obtained at the post death data collection by summing 11 symptom distress items from the Prolonged Grief -13 (PG-13) Scale (Prigerson et al., 2009) for a total score ranging from 11 to 55. A higher score corresponds to a greater level of prolonged or complicated grief symptoms (Thomas, Hudson, Trauer, Remedios, & Clarke, 2014; Tomarken et al., 2012). Prigerson et al. (2009) reported an alpha equal to .82 for these items. Although a clinical diagnosis of prolonged grief disorder is typically not made until after 6 months since a loss has passed (Boelen & Prigerson, 2013; Prigerson et al., 2009), prolonged grief symptoms assessed by the PG-13 items prior to that time are highly predictive of whether or not prolonged grief disorder emerges later (Thomas et al., 2014).
Analytic Strategy
After performing descriptive analyses on the variables, we explored the correlations between preloss caregiver attributes, bereavement outcomes, and preparedness. We then used those bivariate results to inform a series of multivariate regression equations for each of the four bereavement outcomes, where each bereavement outcome was first regressed on perceptions of overall preparedness (Model 1), and again while controlling for the caregiver-related factors (Model 2). Comparison of the coefficients across Models 1 and 2 was able to show how much of the relationship between preparedness and bereavement outcomes was potentially explained by preloss caregiver attributes. All regression analyses were estimated using both least squares and maximum likelihood estimation techniques. Because these data supported normality of responses and errors, the two sets of estimates are identical. We present the least squares estimates here, given a meaningful interpretation of the R-squared values as the amount of explained variation in the outcome variables.
Attrition
Thirty-three (14.6%) caregivers were lost to attrition following baseline. T-tests revealed no statistically significant differences between this group of caregivers and those who completed the post-death data collection with the exception of length of hospice stay (t = −2.74, p < 0.01). Those who were lost to attrition used hospice for a longer period of time (M = 103 days; SD = 194.19) than those who remained in the study (M =54 days; SD = 74.69). Many of the patients who were in hospice for a longer period of time were still alive at the end of the study period. Consequently, there was no opportunity to obtain a post-death data collection from their caregivers. Other reasons for attrition included moving out of the study area and no longer interested in participating.
Results
Descriptive Findings
Table 1 presents descriptive data pertaining to preparedness, bereavement outcomes, and preloss caregiver attributes, including demographic characteristics. Sixty-two percent of the caregivers were women with a mean age equal to 65.2 years (SD = 10.5; Range = 45 – 90). They were married or had been in a relationship with their care recipients for an average of 35.3 years (SD = 17.0. Range = 1 – 68) when they entered the study. Ninety-eight percent completed high school, including 40% college graduates. Most (81%) reported that their financial situation was either comfortable or more than adequate to meet their needs. Mean anxiety scores indicated that a notable proportion of the sample was experiencing anxiety as caregivers. In fact, 33% of the sample had scores ≥ 11, indicating very high anxiety levels.
Table 1.
Descriptive Statistics on Key Variables
| Mean or Percent | SD | Range | |
|---|---|---|---|
| Preparedness for Loss | |||
| Emotional | 3.42 | 1.15 | 1–5 |
| Practical | 3.67 | 1.15 | 1–5 |
| Overall (Emotional + Practical) | 7.09 | 2.11 | 2–10 |
| Bereavement Outcomes1 | |||
| Grief | 26.70 | 9.09 | 11–55 |
| Depressive Symptoms | 4.28 | 3.82 | 0–14 |
| Active Coping | 17.50 | 3.12 | 7–21 |
| Managing Household Affairs | 26.89 | 3.54 | 11–30 |
| Preloss Caregiver Attributes1 | |||
| Depressive Symptoms | 4.54 | 3.39 | 0–14 |
| Anxiety Symptoms | 8.46 | 4.52 | 0–20 |
| Active Coping | 17.38 | 3.05 | 9–21 |
| Managing Household Affairs | 26.44 | 3.39 | 15–30 |
| Hospice Duration (in days) | 67.71 | 122.48 | 0–1455 |
| Age (in years) | 65.22 | 10.52 | 45–90 |
| Gender (female) | 62% | ||
| Length of relationship (in years) | 35.33 | 17.05 | 1–68 |
| Education (college degree or more) | 40% | ||
| Perceived financial adequacy | |||
| not adequate | 18% | ||
| adequate | 61% | ||
| more than adequate | 20% | ||
Notes:
Bereavement Outcomes are measured at 2–3 months post-death. Caregiver Attributes are measured at baseline/enrollment, approximately the time of hospice admission.
As seen in the Table 1, there was variability in how participants rated their emotional, practical, and overall preparedness. Using a cut-off of 3 or less, nearly half (49%) of the caregivers reported they were not prepared emotionally for the deaths of their spouses or partners; more than one-third (35%) reported they were not prepared for the practical challenges associated with the loss. Fifty-three percent had scores ≤ 7 on the overall preparedness scale.
Finally, Table 1 shows the average bereavement responses for this sample. Three (of the four) outcome measures were assessed at both time points - baseline/caregiving and post-death/bereavement - providing a sense of how these measures of affect and competency change over the transition from caregiving to bereavement. The fourth measure – grief – was not measured at baseline/caregiving, since grief is typically associated with bereavement and loss. Although the mean levels of perceived competency, as measured by active coping and household management skills, tended to fall within the higher end of the ranges for both scales at each time point, there were individuals who clearly perceived themselves as not adequately skilled in these daily living competencies at either the caregiving or bereavement stages. Similarly, the mean scores for depression fell just below the cut-off indicating clinical depressive symptoms (≥ 5); yet, approximately 40% of the sample reported depressive symptoms in the clinical range at each of the two time points. Finally, although the mean score for grief symptoms fell below the potential midpoint of the scale (33), participant scores covered the full possible range for that scale, suggesting there were some who were experiencing the more adverse or complicated grief symptoms.
Correlational Findings
Table 2 shows that several preloss caregiver attributes were associated with both bereavement outcomes and perceptions of preparedness. For example, caregivers with greater anxiety and depressive symptoms felt less prepared for the loss. Those same caregivers with higher anxiety and depressive symptoms also exhibited greater post-death depressive symptoms, higher levels of grief, and lower daily competencies. Similarly, caregivers who reported greater competence in daily living activities (active coping and management of household affairs) had greater perceptions of preparedness and more favorable bereavement outcomes. Those with greater financial sufficiency were also associated with higher levels of preparedness and more favorable bereavement outcomes.
Table 2.
Pearson Correlation: Preloss Caregiver Attributes, Bereavement Outcomes, & Preparedness
| Bereavement Outcomes | Preparedness for Loss | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Grief | Depression | Managing Household Affairs | Active Coping | Emotional Preparedness | Practical Preparedness | Overall Preparedness | |
|
Preloss Caregiver Attributes
|
|||||||
| Depressive Symptoms | 0.48 *** | 0.64 *** | −0.34** | −0.39** | −0.29 ** | −0.24* | −0.28** |
| Anxiety Symptoms | 0.55*** | 0.52*** | −0.31** | −0.42*** | −0.32** | −0.31** | −0.34** |
| Active Coping | −0.49*** | −0.52*** | 0.53*** | 0.65*** | 0.27* | 0.23* | 0.27** |
| Managing Household Affairs | −0.31** | −0.35** | 0.63** | 0.55** | 0.09 | 0.24** | 0.18 |
| Hospice Duration | −0.04 | 0.05 | −0.04 | 0.03 | 0.05 | 0.03 | 0.04 |
| Age | −0.20** | −0.16* | 0.12 | 0.14 | 0.07 | 0.16 | 0.12 |
| Gender | −0.07 | −0.08 | −0.13 | 0.00 | 0.04 | 0.01 | 0.02 |
| Length of Relationship | −0.25** | −0.25** | 0.20* | 0.21** | 0.14 | 0.15 | 0.16 |
| Perceived Financial Adequacy | −0.32** | −0.26** | 0.24** | 0.28** | 0.20* | 0.25** | 0.25** |
| Education | −0.14 | −0.13 | 0.06 | 0.07 | 0.16 | 0.08 | 0.13 |
Notes: Pearson Correlation is statistically significant (2-tailed),
p<.05,
p<.01,
p<.001
Age and length of relationship were associated with bereavement outcomes, suggesting that those who are older and those who are in longer relationships may have more favorable bereavement outcomes. Yet, age and length of relationship were not associated with how prepared one felt. The other caregiver attributes including gender, education, and length of hospice stay were not associated with preparedness or bereavement outcomes. These bivariate results illustrate the importance of accounting for preloss caregiver attributes in understanding the relationship between preparedness and bereavement outcomes.
Regression Results
Table 3 shows results from the regression analyses estimating the effect of preparedness on four different bereavement outcomes (Model 1), and then whether this relationship exists after controlling for the preloss caregiver attributes (Model 2). To be included as a control variable, the preloss caregiver attribute had to have at least one significant bivariate correlation with either an outcome measure or a preparedness measure, as shown previously in Table 2 (i.e., gender, education, and length of hospice stay were consequently excluded). Table 3 provides the coefficients estimating “overall” preparedness; additional models looking individually at “emotional” versus “practical” preparedness (not shown here) produced nearly identical results as those reported in Table 3.
Table 3.
Least Squares Regression Coefficients Estimating the Effect of Preparedness on Bereavement Outcomes
| Bereavement Outcomes
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Grief | Depression | Household Affair Mgmt | Active Coping | |||||
| Model 1 | Model 2a | Model 1 | Model 2a | Model 1 | Model 2a | Model 1 | Model 2a | |
|
| ||||||||
| Preparedness for Loss ∞ | −2.6 *** | −1.79 *** | −0.96 *** | −0.66 *** | 0.72 *** | 0.43 ** | 0.70 *** | 0.41 ** |
| (0.40) | (0.41) | (0.17) | (0.17) | (0.17) | (0.14) | (0.14) | (0.13) | |
| Preloss Caregiver Attributes | ||||||||
| Depressive Symptoms | 0.30 | 0.50 *** | 0.07 | 0.08 | ||||
| (0.32) | (0.14) | (0.08) | (0.11) | |||||
| Anxiety Symptoms | 0.50 * | 0.05 | 0.07 | −0.03 | ||||
| (0.23) | (0.10) | (0.08) | (0.08) | |||||
| Active Coping | 0.02 | −0.03 | 0.18 | 0.40 ** | ||||
| (0.43) | (0.18) | (0.15) | (0.14) | |||||
| Managing Household Affairs | −0.30 | −0.07 | 0.58 *** | 0.19 * | ||||
| (0.29) | (0.12) | (0.10) | (0.09) | |||||
| Age | −0.01 | 0.02 | −0.01 | −0.01 | ||||
| (0.10) | (0.04) | (0.03) | (0.03) | |||||
| Length of relationship | −0.02 | −0.03 | 0.02 | 0.02 | ||||
| (0.06) | (0.03) | (0.02) | (0.02) | |||||
| Perceived Financial Adequacy | −0.95 | 0.48 | 0.27 | 0.35 | ||||
| (1.38) | (0.58) | (0.49) | (0.46) | |||||
| Constant | 45.30 | 44.27 | 11.36 | 7.54 | 21.51 | 3.25 | 12.14 | 2.70 |
| Adjusted R-Squared | 0.34 | 0.45 | 0.27 | 0.46 | 0.18 | 0.53 | 0.22 | 0.45 |
Notes: Unstandardized coefficients, B, and (standard errors) are reported in cells.
p≤.10,
p<.05,
p<.01.
p<.001
Significant F-Change from Model 1 to Model 2, p<.05.
A measure of Overall Preparedness (emotional + practical) was used in these equations as the primary independent variable.
A similar finding emerged across all eight models that were estimated: Preparedness was significantly associated with more favorable bereavement outcomes. More specifically, higher levels of perceived preparedness had a predicted inverse effect on the two affective outcomes (depressive and grief symptoms) and an expected positive effect on the two daily living competency measures (active coping and household management). A comparison of Models 1 and Models 2 reveal two additional important findings: First, the significant F-change noted for each of the four outcomes (p < .05) suggests that the addition of the caregiver attribute variables in Model 2 significantly improved the overall model fit. Similarly, the higher adjusted R-squared values for Model 2, compared to Model 1, revealed that a greater proportion of variance was explained by the consideration of preparedness together with preloss caregiver attributes. Second, the comparison of the estimated b coefficient for preparedness was consistently larger in Model 1 than Model 2, suggesting that some of preparedness’ effect on outcomes was explained by variations in the caregiver factors examined. Yet, in each of the four models, preparedness remained significant (p < .01). A final notable and expected relationship emerged showing higher levels of daily-life competency during bereavement among those who had higher competency during caregiving; and lower levels of grief and post-loss depression among those who had lower levels of anxiety or depressive symptoms as a caregiver. None of the demographic characteristics were significant in these multivariate models.
Discussion
In addition to determining the levels of emotional and practical preparedness among cancer caregivers, the purpose of this investigation was to examine the relationship between preparedness and bereavement outcomes while accounting for the influence of preloss caregiver attributes. Controlling for these characteristics allowed us to determine to what extent preparedness has a unique influence on bereavement outcomes or is a function of a spurious relationship involving those attributes.
Consistent with other reports (Clark et al., 2011; Hebert, Dang, et al., 2006; Nielsen et al., 2016; Tabler et al., 2015), we found a significant proportion of bereaved spouses/partners reported they were not adequately prepared emotionally, and to a lesser extent, in a practical way for their loss, even with an apparent period of forewarning. Lower levels of perceived preparedness were common among caregivers who were more anxious and depressed, less competent in daily living tasks, and who reported lower financial adequacy.
Similarly, and as expected, aspects of the caregivers’ situation were also correlated with bereavement outcomes. Higher levels of anxiety and depression during caregiving were associated with more adverse consequences post loss. This is consistent with reports in the literature indicating a relationship between caregiver distress and bereavement outcomes (Nielsen et al., 2016; Romero et al., 2014). As well, lower perceived daily living competencies and lower financial adequacy during caregiving were associated with more adverse bereavement outcomes (especially pertaining to managing a household). Having adequate skills and resources during caregiving may persist into bereavement, which could place some bereaved spouses/partners at an advantage to be better prepared to address some of the practical matters that arise as an outcome of the loss.
As suggested earlier, the fact that these preloss caregiver attributes produced significant correlations with both preparedness and bereavement outcomes could suggest a spurious relationship. The multivariate regression analyses revealed, however, that preparedness emerged as a significant and strong predictor of both affective and daily living bereavement outcomes but most importantly, remained so after controlling for caregiver-related attributes. Lower levels of preparedness were associated with more depression, a greater likelihood of experiencing complicated/prolonged grief symptoms, and with lower levels of daily living competencies during early bereavement. The overarching conclusion from these analyses, therefore, is that while one’s preloss caregiving characteristics do contribute to the strength of the relationship between preparedness and bereavement outcomes, the effect of preparedness remains the strongest predictor of those outcomes.
Implications for Intervention
Although it is not possible to rule out all potential spurious relationships regarding the connection between preparedness and bereavement outcomes, the robustness of these findings point to a promising focus for future intervention. The findings associated with emotional versus practical preparedness follow similar patterns with both antecedent and outcome variables, so a dual focus on both (overall preparedness) is an important way to support caregivers who are facing the transition from caregiving to bereavement. Especially important is to intervene early within the caregiving phase. Preparedness necessitates an active effort that encompasses planning, communication, problem solving and decision-making as well as coming to terms with an uncertain future (Carr, 2012; Hebert, Prigerson, et al., 2006; Hebert et al., 2009). These findings suggest that activities that foster preparedness are beneficial earlier in the disease trajectory prior to the need for hospice care where the focus tends to be almost exclusively on symptom management and comfort care of the patient (Schulz et al., 2015; Tabler et al., 2015).
A well-known theoretical framework in bereavement is the dual process model (DPM) (Stroebe & Schut, 1999, 2010). The DPM posits that individuals adapt to a loss by oscillating between loss-oriented (LO) coping, which addresses those stressors related to the loss itself and restoration-orientation (RO), in which the bereaved individual copes with life changes and related stressors consequential to the loss that has occurred (for example, taking on new responsibilities). Those who adapt the most effectively are able to engage in that form of coping needed to address the “stressor at hand.” Given the influence preparedness has on outcomes along with a recognition of the value of supporting caregivers earlier within the illness trajectory, we argue that the dual process model and its application to intervention can be “upstreamed.”
The focus of an upstreamed DPM would be on preparatory coping, in which caregivers turn their attention to various facets of being emotionally and practically prepared to address immediate concerns but also what lies ahead as they eventually transition from caregiving to bereavement. In this application of the model, preparatory loss-orientation (P-LO) includes coping with the expected thoughts and feelings of grief and loneliness surrounding the loss of the person and a shared future, while preparatory restoration-orientation (P-RO, or what can be coined as “pre-storation”) is a recognition that caregivers must cope with the concomitant daily living issues related to the uncertainties of the path the disease takes and how they will manage the challenges of daily life after the patient dies. Recently, Stroebe and Schut (2016) introduced overload as a “missing link” in the DPM. Overload is an outcome of experiencing an array of stressors - including those not related to the bereavement experience - that exceeds an individual’s ability to effectively engage in loss- or restoration-oriented coping processes. Given the demands confronting cancer caregivers during the end stages of the patients’ disease, they could be especially susceptible to overload, which further underscores the value of engaging in preparatory coping earlier in the disease trajectory.
Without encouragement from others, cancer caregivers often find it difficult to think about the future beyond their current caregiving situation and might lack the time and energy to engage in any form of preparation (Tabler et al., 2015). Each caregiver may have his or her own unique needs regarding how to best prepare emotionally or on a practical level. Therefore, the role of an intervention focused on preparatory coping would be to help caregivers identify emotional and/or practical areas where they need to place their attention and then engage in the necessary preparation to engender a greater sense of readiness. Those experiencing higher levels of depression and anxiety and who are less capable in meeting daily living tasks should be particularly targeted for this type of intervention.
Limitations and Future Directions
Our longitudinal design provided the opportunity to obtain both caregiving and bereavement assessments, which was a notable strength of this study. Still, there are limitations that need to be taken into account in interpreting the findings, most notably regarding how preparedness was measured. Like most research on preparedness, the bereaved spouses/partners were asked to retrospectively report on how prepared they were for the death after it happened, which could be a source of recall bias (Nielsen et al., 2016). Only a study by Schulz et al. (2015) assessed preparedness prospectively. In that study, preparedness was inversely related to complicated grief, which is consistent with our findings, partially supporting the validity of the retrospective reports of the bereaved caregivers soon after the loss. Clearly, however, we agree with Schulz and his colleagues that future studies investigating preparedness should incorporate prospective measures into their designs.
Furthermore, while our study was able to separate how emotionally versus practically prepared caregivers felt (Carr, 2012), preparedness has been described in the literature as a multifaceted concept involving psychosocial, spiritual, as well as practical dimensions (Hauksdottir, Steineck, et al., 2010; Hauksdottir, Valdimarsdottir, et al., 2010). In addition to making preparedness the focal point of pre-bereavement interventions, future research needs to devote greater attention to how this concept is defined and how it is measured empirically (Nielsen et al., 2016). Until this is pursued, findings pertaining to preparedness for loss will be limited and the field will be slow to advance. We suggest considering how preparedness is related to the larger caregiving context and dynamics. For example, are those caregivers who receive help from family and friends more prepared, and in what facets are they most prepared? Do the different facets of preparedness differ across the stages of death trajectory, and/or by the relationship among the caregiver and patient? Are the facets of preparedness static or dynamic over time, and do they vary with each other? Moreover, the extent to which caregivers are able to grasp the implications of their spouses’ or partners’ prognosis and cope with distressing symptoms, for instance, may align with Stroebe and Schut’s (2016) conceptualization of “overload” and merit examination in a larger conceptual model of preparedness. Given the current data, we were unable to capture the full array of dynamics and facets associated with preparedness, but encourage future research to continue to explore novel ways to conceptualize and operationalize it.
Finally, the sample of caregivers in our study consisted exclusively of bereaved spouses or partners. It is yet to be determined to what extent the findings uncovered here would apply to those in other caregiver relationships, such as adult children. Although there are arguably some common elements independent of relationship type, both emotional and practical preparedness could be qualitatively different for those who are caring for a parent dying from cancer. In other words, some issues for which spousal caregivers need to be prepared (for example, being alone after many years in a married/partnered relationship, or taking on new responsibilities that were once the deceased spouse’s/partner’s) may not always be as relevant for adult children.
Even with these limitations, this study adds to our understanding of the role of preparedness in predicting outcomes among bereaved caregivers while taking into account caregiver-related attributes identified in the literature. Disentangling potential spurious effects among preparedness, selected preloss caregiver attributes, and bereavement outcomes revealed preparedness as a promising as well as potentially feasible target for early intervention with those caregivers who would be at greatest risk for adverse outcomes later in bereavement.
Acknowledgments
Research reported in this publication was supported by a grant from the National Cancer Institute (P01 CA138317). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
References
- Aldwin CM, Levenson MR. Posttraumatic growth: A developmental perspective. Psychological Inquiry. 2004;15(1):9–22. [Google Scholar]
- Aneshensel CS, Botticello AL, Yamamoto-Mitani N. When caregiving ends: the course of depressive symptoms after bereavement. Journal of Health & Social Behavior. 2004;45(4):422–440. doi: 10.1177/002214650404500405. [DOI] [PubMed] [Google Scholar]
- Asgeirsdottir HG, Valdimarsdottir U, Furst CJ, Steineck G, Hauksdottir A. Low preparedness before the loss of a wife to cancer and the widower’s chronic pain 4–5 years later-a population-based study. Psychooncology. 2013;22(12):2763–2770. doi: 10.1002/pon.3345. [DOI] [PubMed] [Google Scholar]
- Barry LC, Kasl SV, Prigerson HG. Psychiatric disorders among bereaved persons: the role of perceived circumstances of death and preparedness for death. American Journal of Geriatric Psychiatry. 2002;10(4):447–457. [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research. 2002;52(2):69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Boelen P, Prigerson H. Prolonged grief disorder as a new diagnostic category in DSM-5. In: Stroebe M, Schut H, van den Bout J, editors. Complicated grief: Scientific foundations for health care professionals. New York, NY: Routledge; 2013. pp. 85–98. [Google Scholar]
- Bradley EH, Prigerson H, Carlson MD, Cherlin E, Johnson-Hurzeler R, Kasl SV. Depression among surviving caregivers: does length of hospice enrollment matter? American Journal of Psychiatry. 2004;161(12):2257–2262. doi: 10.1176/appi.ajp.161.12.2257. [DOI] [PubMed] [Google Scholar]
- Carr D. Gender, preloss marital dependence, and older adults’ adjustment to widowhood. Journal of Marriage and the Family. 2004;66:220–235. [Google Scholar]
- Carr D. Death and dying in the contemporary United States: What are the psychological implications of anticipated death? Social and Personality Psychology Compass. 2012;6(2):184–195. [Google Scholar]
- Carr D, Nesse RM, Wortman CB, editors. Spousal bereavement in late life. New York, NY: Springer; 2006. [Google Scholar]
- Caserta M, Lund D, Obray SJ. Promoting self-care and daily living skills among older widows and widowers: Evidence from the Pathfinders demonstration project. Omega: Journal of Death & Dying. 2004;49(3):217–236. [Google Scholar]
- Caserta M, Lund D, Utz R, Tabler JL. “One size doesn’t fit all” - Partners in Hospice Care, an individualized approach to bereavement intervention. Omega (Westport) 2016;73(2):107–125. doi: 10.1177/0030222815575895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caserta MS, Utz RL, Lund DA. Spousal bereavement following cancer death. Illness, Crisis and Loss. 2013;21(3):185–202. doi: 10.2190/IL.21.3.b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark PG, Brethwaite DS, Gnesdiloff S. Providing support at time of death from cancer: Results of a 5-year post-bereavement group study. Journal of Social Work in End-of-Life & Palliative Care. 2011;7(2–3):195–215. doi: 10.1080/15524256.2011.593156. [DOI] [PubMed] [Google Scholar]
- Fowler NR, Hansen AS, Barnato AE, Garand L. Association between anticipatory grief and problem solving among family caregivers of persons with cognitive impairment. Journal of Aging and Health. 2013;25(3):493–509. doi: 10.1177/0898264313477133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauksdottir A, Steineck G, Furst CJ, Valdimarsdottir U. Long-term harm of low preparedness for a wife’s death from cancer--a population-based study of widowers 4–5 years after the loss. American Journal of Epidemiology. 2010;172(4):389–396. doi: 10.1093/aje/kwq147. [DOI] [PubMed] [Google Scholar]
- Hauksdottir A, Valdimarsdottir U, Furst CJ, Onelov E, Steineck G. Health care-related predictors of husbands’ preparedness for the death of a wife to cancer--a population-based follow-up. Annals of Oncology. 2010;21(2):354–361. doi: 10.1093/annonc/mdp313. mdp313. [DOI] [PubMed] [Google Scholar]
- Hebert RS, Dang Q, Schulz R. Preparedness for the death of a loved one and mental health in bereaved caregivers of patients with dementia: findings from the REACH study. Journal of Palliative Medicine. 2006;9(3):683–693. doi: 10.1089/jpm.2006.9.683. [DOI] [PubMed] [Google Scholar]
- Hebert RS, Prigerson HG, Schulz R, Arnold RM. Preparing caregivers for the death of a loved one: a theoretical framework and suggestions for future research. Journal of Palliative Medicine. 2006;9(5):1164–1171. doi: 10.1089/jpm.2006.9.1164. [DOI] [PubMed] [Google Scholar]
- Hebert RS, Schulz R, Copeland VC, Arnold RM. Preparing family caregivers for death and bereavement. Insights from caregivers of terminally ill patients. Journal of Pain and Symptom Management. 2009;37(1):3–12. doi: 10.1016/j.jpainsymman.2007.12.010. [DOI] [PubMed] [Google Scholar]
- Henriksson A, Arestedt K. Exploring factors and caregiver outcomes associated with feelings of preparedness for caregiving in family caregivers in palliative care: a correlational, cross-sectional study. Palliative Medicine. 2013;27(7):639–646. doi: 10.1177/0269216313486954. [DOI] [PubMed] [Google Scholar]
- Hudson PL, Thomas K, Trauer T, Remedios C, Clarke D. Psychological and social profile of family caregivers on commencement of palliative care. Journal of Pain and Symptom Management. 2011;41(3):522–534. doi: 10.1016/j.jpainsymman.2010.05.006. [DOI] [PubMed] [Google Scholar]
- Johansson AK, Grimby A. Anticipatory grief among close relatives of patients in hospice and palliative wards. American Journal of Hospice & Palliative Care. 2012;29(2):134–138. doi: 10.1177/1049909111409021. [DOI] [PubMed] [Google Scholar]
- Lund D, Caserta M, Dimond M, Shaffer S. Competencies, tasks of daily living, and adjustments to spousal bereavement in later life. In: Lund DA, editor. Older bereaved spouses: Research with practical applications. Washington, DC: Taylor-Francis/Hemisphere Press; 1989. pp. 135–156. [Google Scholar]
- Moon PJ. Anticipatory Grief: A Mere Concept? American Journal of Hospice & Palliative Medicine. 2015;32:1–4. doi: 10.1177/1049909115574262. [DOI] [PubMed] [Google Scholar]
- Mooney K, Berry P, Caserta M, Ellington L, Clayton M, Lund D, Utz R. Partners in Hospice Care: A program project grant exploring and supporting family caregivers during hospice care through bereavement. Journal of Pain and Symptom Management. 2013;45(2):394–395. doi: 10.1016/j.jpainsymman.2012.10.247. [DOI] [Google Scholar]
- Nielsen MK, Neergaard MA, Jensen AB, Bro F, Guldin MB. Do we need to change our understanding of anticipatory grief in caregivers? A systematic review of caregiver studies during end-of-life caregiving and bereavement. Clinical Psychology Review. 2016;44:75–93. doi: 10.1016/j.cpr.2016.01.002. [DOI] [PubMed] [Google Scholar]
- Olson RE. Indefinite loss: the experiences of carers of a spouse with cancer. Eur J Cancer Care (Engl) 2014;23(4):553–561. doi: 10.1111/ecc.12175. [DOI] [PubMed] [Google Scholar]
- Parkes CM. Psycho-social transitions: A field for study. Social Science & Medicine. 1971;5:101–115. doi: 10.1016/0037-7856(71)90091-6. [DOI] [PubMed] [Google Scholar]
- Payne S, Smith P, Dean S. Identifying the concerns of informal carers in palliative care. Palliative Medicine. 1999;13(1):37–44. doi: 10.1191/026921699673763725. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Horowitz MJ, Jacobs SC, Parkes CM, Aslan M, Goodkin K, … Maciejewski PK. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-V and ICD-11. PLoS Med. 2009;6(8):e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rando TA. Clinical dimensions of anticipatory mourning. Champaign, IL: Research Press; 2000. [Google Scholar]
- Romero MM, Ott CH, Kelber ST. Predictors of grief in bereaved family caregivers of person’s with Alzheimer’s disease: a prospective study. Death Studies. 2014;38(6–10):395–403. doi: 10.1080/07481187.2013.809031. [DOI] [PubMed] [Google Scholar]
- Schulz R, Boerner K, Klinger J, Rosen J. Preparedness for death and adjustment to bereavement among caregivers of recently placed nursing home residents. Journal of Palliative Medicine. 2015;18(2):127–133. doi: 10.1089/jpm.2014.0309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Mendelsohn AB, Haley WE, Mahoney D, Allen RS, Zhang S, Thompson L, Belle SH. End-of-life care and the effects of bereavement on family caregivers of persons with dementia. New England Journal of Medicine. 2003;349(20):1936–1942. doi: 10.1056/NEJMsa035373. [DOI] [PubMed] [Google Scholar]
- Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): Recent evidence and development of a shorter version. In: Brink TL, editor. Clinical gerontology: A guide to assessment and intervention. New York, NY: Haworth Press; 1986. pp. 165–173. [Google Scholar]
- Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, Grambow S, Parker J, Tulsky JA. Preparing for the end of life: preferences of patients, families, physicians, and other care providers. Journal of Pain and Symptom Management. 2001;22(3):727–737. doi: 10.1016/s0885-3924(01)00334-7. [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H. The dual process model of coping with bereavement: Rationale and description. Death Studies. 1999;23:197–224. doi: 10.1080/074811899201046. [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H. The dual process model of coping with bereavement: A decade on. Omega Journal of Death and Dying. 2010;61(4):273–289. doi: 10.2190/OM.61.4.b. [DOI] [PubMed] [Google Scholar]
- Stroebe M, Schut H. Overload: A missing link in the dual process model. Omega (Westport) 2016;74(1):96–109. [Google Scholar]
- Stroebe MS, Hansson RO, Schut H, Stroebe W. Handbook of bereavement research and practice: Advances in theory and intervention. Washington, DC: American Psychological Association; 2008. [Google Scholar]
- Tabler JL, Utz R, Ellington L, Reblin M, Caserta M, Clayton M, Lund D. Missed opportunity: Hospice care and the family. Journal of Social Work in End-of-Life and Palliative Care. 2015;11(3/4):224–243. doi: 10.1080/15524256.2015.1108896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas K, Hudson P, Trauer T, Remedios C, Clarke D. Risk factors for developing prolonged grief during bereavement in family carers of cancer patients in palliative care: a longitudinal study. Journal of Pain and Symptom Management. 2014;47(3):531–541. doi: 10.1016/j.jpainsymman.2013.05.022. [DOI] [PubMed] [Google Scholar]
- Tomarken A, Roth A, Holland J, Ganz O, Schachter S, Kose G, … Nelson CJ. Examining the role of trauma, personality, and meaning in young prolonged grievers. Psychooncology. 2012;21(7):771–777. doi: 10.1002/pon.1983. [DOI] [PubMed] [Google Scholar]
- Tsai WI, Prigerson HG, Li CY, Chou WC, Kuo SC, Tang ST. Longitudinal changes and predictors of prolonged grief for bereaved family caregivers over the first 2 years after the terminally ill cancer patient’s death. Palliative Medicine. 2015 doi: 10.1177/0269216315603261. [DOI] [PubMed] [Google Scholar]
- Utz R. Economic and practical adjustments to late life spousal loss. In: Carr D, Neese RM, Wortman CB, editors. Spousal bereavement in late life. New York, NY: Springer; 2006. pp. 167–192. [Google Scholar]
- Utz RL, Lund DA, Caserta MS, de Vries B. Perceived self-competency among the recently bereaved. Journal of Social Work in End-of-Life and Palliative Care. 2011;7(2–3):173–194. doi: 10.1080/15524256.2011.593154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]