Abstract
Objective
To evaluate the longitudinal impact of a 9-month text message intervention on participant adherence beyond the intervention to highly effective contraceptive methods among urban adolescent and young adult women enrolled in the DepoText randomized control trial (RCT).
Study Design
Retrospective longitudinal cohort study of long-term follow-up data from the DepoText RCT. Sixty-seven female participants (aged 13–21 years) using depot medroxyprogesterone acetate (DMPA) were recruited from an urban academic adolescent practice in Baltimore, Maryland. The principal outcome measured was a comparison of contraceptive method choice between the control and intervention groups during the 20 months postintervention.
Results
Intervention participants were 3.65 times more likely to continue using DMPA or a more efficacious method at the 20-month postintervention evaluation (odds ratio 3.65, 95% CI 1.26–10.08; P = .015).
Conclusion
Participation in the DepoText trial was associated with continued use of DMPA or a more effective contraceptive method almost 20 months after the intervention exposure ended.
Keywords: adolescent, DMPA, Depo-Provera, text messaging, family planning, adherence
Introduction
The unintended pregnancy rate among adolescents is one of the highest across all age groups—with Baltimore City’s teen birth rate higher than both the Maryland and US national rates.1 With 82% of teen pregnancies reported as unplanned, adolescents account for one-fifth of total annual unintended pregnancies.2,3 Urban minority youth have high rates of missed clinic appointments,4,5 but access to and use of text message technology is not associated with socioeconomic or racial/ethnic disparities.6,7 Recent federal health policy efforts have sought to incentivize improvements in safety and efficiency of patient care delivery through improved use of technology to target health disparities in areas such as those affecting adolescent populations. “Meaningful use of technology” through improved patient communication is one such initiative.
Over the past 15 years, the decline in US teen pregnancy rates has been primarily attributed to improved contraceptive use and adherence.8–10 Text messaging is a simple tool to communicate with teenagers who are at high risk for unintended pregnancy as a way of promoting healthy decisions related to contraceptive adherence and safe sexual practices. Youth-friendly text messages are a culturally relevant, convenient technology that can connect young, socially disadvantaged populations with the clinical setting to yield positive short-term health outcomes.12–14 Previous studies have demonstrated the use of texting as a health behavior modifier that improves short-term oral contraceptive pill continuation.15–19 To our knowledge, no study has been conducted to evaluate the longitudinal impact of a short-term, depot medroxyprogesterone acetate (DMPA) texting intervention on subsequent family planning behavior beyond the culmination of the text message intervention.
DMPA is a safe, effective, and commonly chosen contraceptive method by adolescents and young adults.20 Among young, urban women of color, DMPA has one of the highest rates of user satisfaction.21,22 These rates persist in the presence of documented risks, including a Black Box warning related to bone mineral density (BMD) loss with extended use. New recommendations to reevaluate women using DMPA after 24 months have been published and disseminated to address this concern. Recent studies also demonstrate that BMD loss dramatically slows after 24 months of use and is almost always completely reversed in adolescents within 2 to 3 years of discontinuation.23
DMPA is a unique contraceptive method that does not require male consent or cooperation and cannot be controlled, observed, or felt (eg rod beneath the arm, intrauterine device [IUD] strings) by male partners or others.24,25 Women often appreciate the “hidden” nature of DMPA, and freedom from daily compliance.26–28 In addition, as a progestin-only method, DMPA remains an important option for patients with medical contraindications for combined estrogen-progesterone contraceptive methods, and one that is supported by the American College of Obstetricians and Gynecologists and the World Health Organization.29,30
The purpose of this study is to evaluate long-term postintervention outcomes of the control and intervention participants in the DepoText trial to better understand the influence of text message interventions on participant adherence to highly effective methods such as DMPA or long-acting reversible contraception (LARC). We hypothesized that the effects of the original DepoText trial would be sustained, resulting in long-term adherence to or improvement in contraception choice.31
Materials and Methods
Original DepoText Trial
The DepoText trial was a randomized controlled pilot trial (RCT) conducted in an urban academic practice serving adolescent patients in Baltimore, Maryland between January 2011 and February 2012 (clinical trials registration #NCT01641380).31 The primary goals of the trial were to evaluate feasibility, acceptability, and preliminary efficacy of using a text message reminder system for family planning clinic appointments and delivery of positive sexual health messages during DMPA use. The messages were created to maintain patient privacy and empower adolescents by promoting self-management of their family planning decisions. Urban adolescents aged 13 to 21 years who were using DMPA and had a cell phone for personal use were eligible. One hundred participants were recruited and randomized into either the control or intervention arm. Each arm had 50 participants. Participants completed a baseline web-based survey during which demographic, parental, sexual, and use-of-technology histories were collected. Participants received $10 remuneration for completion of the survey and $5 for notifying the nurse case manager of changes in contact information over time. The major findings of the study support the feasibility, acceptability, and preliminary efficacy of the DepoText program for improving clinic attendance for family planning visits11. The Johns Hopkins Institutional Review Board approved this study.
DepoText Intervention
Participants in the intervention arm received text message reminders via the Compliance for Life (CFL) platform. Reminder messages for DMPA-specific family planning appointments were sent to all intervention participants 72 hours prior to the scheduled appointment time, and prompted the participant to reply. Additional reminders were sent at 48 and 24 hours prior to the appointment until the patient responded. One sample appointment reminder read, “Will you be going to your appointment on MM/DD/YYYY?—Nurse Kathy. If yes, reply 1. If no, reply 2”. A reply of “no” automatically sent an email alerting the nurse case manager to follow-up with the participant to reschedule the family planning clinic appointment. Communication was intentionally designed as 2-way; specific response categories were predetermined to result in flags being generated to the nurse case manager to contact the participant. Per the standard of care quality assurance DMPA clinical protocol, all participants in both study arms received a phone call from the clinic to their home phone reminding them of the clinic appointment as well as a call from the nurse case manager following missed appointments. Only intervention arm participants, however, received previsit text reminders.
Safe sexual health message content encouraged condom use and healthy eating using simple, teen-friendly language. Sample messages included, “Condoms prevent STDs. Stop by the clinic if you need some,” “Eat right and exercise to prevent weight gain on DEPO,” and “Call the clinic if you have questions or problems with DEPO.” Each message was delivered once during every 12-week DMPA injection cycles for 3 cycles. A total of 9 safe sexual health messages were delivered by completion of the trial.
Eligibility Criterion for Posttrial Follow-Up
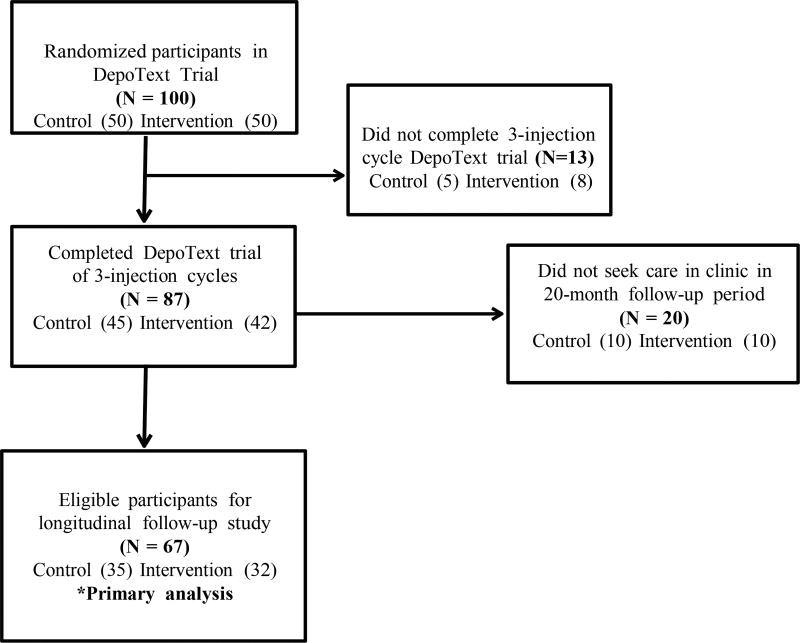
Eighty-seven participants from the original 100 enrolled participants completed all 3 injection cycles of DMPA for the DepoText trial. The primary analysis of this study, to determine the effect of the short-term DepoText intervention on long-term contraceptive use and behavior, involved a retrospective chart review to document participant continued adherence to DMPA or alternative contraceptive choice and compare results between control and intervention participants. Eligible participants for this posttrial follow-up analysis were therefore limited to those participants who completed all 3 injection cycles of the original DepoText trial and sought clinical follow-up care within the period selected for evaluation, February 2012 to October 2013 (Figure 1). Participants without a clinic visit in the electronic health record system between the end of the initial trial and the 20 months posttrial and/or participants who did not have a documented LARC placement, were categorized as not having returned to seek clinical care (N = 20).
Figure 1.
DepoText enrollment and eligibility for longitudinal follow-up study.
For those who did return to clinical care or had a documented LARC placement (N = 67), the method of contraception reported at the most recent visit within the 20-month cross-sectional time frame was used to evaluate contraceptive effectiveness in the follow-up analysis. The time from enrollment to the last clinical visit was documented to assess differences in clinic utilization between groups.
Outcome Measures and Statistical Analysis
The reviewers were blinded to the study arm designation of the participants for chart reviews. Data were evaluated using chi-square and logistic regression analysis in SPSS (version 22). A dichotomous variable was selected to classify the primary outcome of contraceptive method choice: “DMPA or more efficacious method” such as the implant or IUD (ie, LARC) or “less efficacious method” (ie, pill, patch, or ring) from the most recent family planning visit within the 20-month postintervention time frame. Published contraceptive failure rates for the percentage of women experiencing an unintended pregnancy during the first year of typical use and perfect use were used to classify method efficacy compared with DMPA.32
Confounding Variables
For this study, bivariate logistic regression analysis was used to evaluate the relationship between participation in the DepoText intervention and subsequent contraceptive behavior. Using the change-in-estimate method,33 age, race, living situation, parental education, status in school, insurance status, number of reported sexual partners in the past 3 months, history of prior sexually transmitted disease (STD) diagnosis, and history of pregnancy were evaluated as potential confounders or effect modifiers. However, the population of young women in this sample as a whole proved to be characteristically very similar. A chi-square analysis of demographic characteristics was performed to determine whether any statistically significant differences existed between the control and intervention groups for selected factors (Table 1). This served to isolate the impact of the DepoText intervention on decisions related to contraceptive choice.
Table 1.
Selected Demographics of Study Sample (N = 67).
| Characteristic | Intervention (n = 32), % | Control (n = 35), % | P |
|---|---|---|---|
| Age, years, mean (SD) | 17.41 (1.64) | 16.71 (1.69) | .582 |
| Adolescent 13–17 years | 56.2 | 62.9 | |
| Young adult 18–21 years | 43.8 | 37.1 | |
| Race | |||
| Race African American | 96.9 | 97.1 | .949 |
| Resides in single-female headed household | 65.5 | 60.0 | .559 |
| Parental education high school or less | 72.4 | 61.8 | .399 |
| In school at baseline | 82.8 | 94.1 | .153 |
| Had some form of insurance | 93.8 | 91.4 | .718 |
| Ideal age to have a child, 21 years or younger | 21.4 | 35.3 | .280 |
Post Hoc Analysis
In Baltimore, adolescents can seek contraceptive services in a variety of settings, including school-based health centers, the public health department, young adult transition clinics, and so on. Therefore, a post hoc analysis was performed on the 87 participants who completed the original DepoText trial to determine if there were any identifiable differences between those participants who had visits in the 20-month follow-up period (N = 67) and those for whom follow-up data were not available (N = 20).
Results
Sample Characteristics
The mean age of all participants was 17.1 (SD 1.67) years. Almost all the participants were African American (97%) residing in mother-headed households (63%). Most participants were in school (67%) at baseline and had some form of health insurance (93%). Notably, in both the intervention and control groups, only a minority of girls felt that the ideal age to have a child was at age 21 or younger (28%). A chi square analysis of demographic characteristics revealed no statistically significant differences between the control and intervention groups for selected factors (Figure 1).
The overall mean days from enrollment to last clinical visit were 837 (SD 181) days. There were no differences between the 2 groups (Intervention 843 [SD 134] days; Control 832 [SD 180] days; P = .4). Of participants who did not seek clinical care, 10 were from the control arm and 10 from the intervention arm, resulting in no proportional difference between study arms (odds ratio [OR] 0.64, 95% CI 0.24–1.67; P = .356). Those who did not return were also similar to those included in the post-trial follow-up analysis on other patient characteristics (age, race, living situation, parental education, status in school, insurance status, number of reported sexual partners in the past 3 months, history of prior STD diagnosis, and history of pregnancy).
Contraceptive Method Choices and Outcomes
Overall, of the 67 participants in the postintervention assessment, 33 adolescent and young adult women (49%) were classified as using “DMPA or a more efficacious method” based on the most recent clinic visit documented within 20 months postintervention. Within this group, 30 young women (91%) remained on DMPA and 3 switched to a contraceptive rod (9%). The remaining 34 adolescent and young adult women in the postintervention assessment (51%) were classified as using a “Less efficacious method.” Within this group, 5 switched to using condoms only (14%), 3 switched to oral contraceptive pills (8%), 2 switched to using the vaginal ring (5%), 1 switched to the transdermal patch (2%), and the remaining 24 participants reported not using any method of contraception (71%) at the most recent documented visit within the 20-month postintervention time frame.
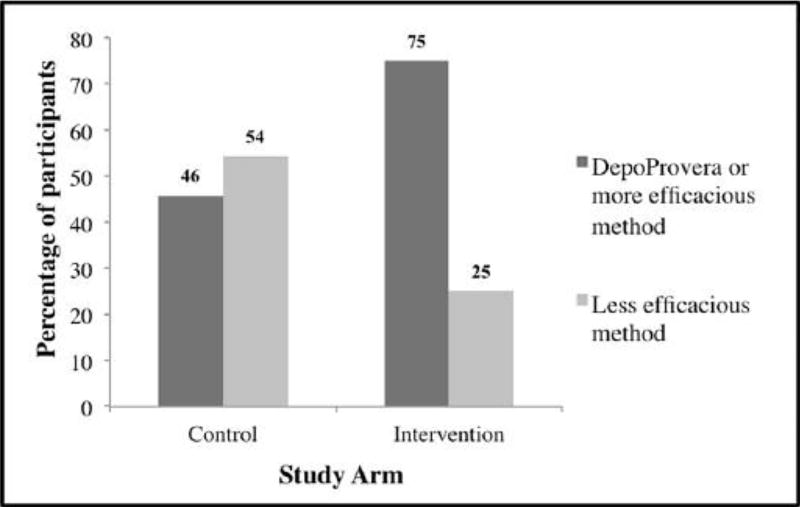
The bivariate logistic regression analysis to evaluate intervention and contraceptive method outcome yielded the results that 75% of young women in the DepoText intervention arm chose to either remain on DMPA or a more efficacious method compared with 46% of those in the control arm. Intervention participants were 3.65 times more likely to use DMPA or more effective intervention at 20 months (OR 3.65, 95% CI 1.26–10.08; P = .015) (Figure 2).
Figure 2.
Contraceptive method outcome by study arm 20 months postintervention (N = 67; odds ratio 3.56, 95% CI 1.26–10.08, P = .015).
Discussion
This study demonstrates that participants in the DepoText trial maintained prolonged adherence to DMPA or selected a more efficacious contraceptive method following completion of the trial. To our knowledge, this is the first study to demonstrate sustained improvement in long-term contraceptive adherence after short-term exposure to a contraceptive text messaging intervention. Intervention factors likely contributing to the positive effect on young women include the following: participant acceptance of text message timing and teen-friendly content, continuity and personalization of care from the nurse case manager, confidentiality of person-based communication, and development of a sense of clinical connectedness to the adolescent clinic practice as a home for contraception needs. The influence of personalized care with the clinic team is consistent with a preliminary review of positive participant feedback, which indicates the importance of having a specific person to contact in the clinic that was familiar with their contraceptive needs.34 Finally, the language of instructions in the text messages was simple, easy to understand and provided practical information. Over time, participants may have become more attuned to self-management of contraception.
Ongoing efforts to encourage LARC such as implant or IUD use among adolescents are important to enhance uptake of these highly effective methods.35 However, current data indicate that less than 5% of young women across the United States choose a LARC method.36–38 There are many obstacles to placement of LARC methods, including financial or insurance barriers, knowledge gaps in safety and efficacy, and parental support. In addition, waiting periods to coordinate LARC insertion can leave adolescents vulnerable to unintended pregnancy.39 Even when all the barriers are removed, one-third of adolescents still chose shorter acting methods and of that group, 20% chose DMPA.40,41 It is therefore critical to optimize support for existing methods chosen by young women for their contraceptive needs while progress is made on securing access, knowledge, and support for LARC methods.
Meaningful Use
The Centers for Medicare & Medicaid Services (CMS) is authorized to provide payments to eligible entities that demonstrate “meaningful use” of electronic health record (EHR) technology. “Meaningful use” is broadly defined as technology-based improvements in safety, efficiency, and health disparities that engage patients, improve coordination of care and maintain privacy and security of health information.42 Compliance with “meaningful use” initiatives is expected to improve clinical outcomes, increase efficiency, empower individuals and augment research data on health systems. The DepoText reminder system is an example of a text-based intervention that could be feasibly integrated into an EHR with texting capability. While many youth have access to email, texting is the preferred method of communication by low-income teens.6 Incorporation of programs like DepoText into an established EHR may foster effective, person-based communication between physicians and patients needing family planning support.
Limitations
The findings from this study should be considered in light of several general limitations. This study was limited to one geographic location with a largely homogenous sample, so generalizability may be limited. Approximately one-fifth of the sample did not seek clinical services within the 20-month postintervention follow-up time frame as per chart review in the EHR system. It is possible that unmeasured factors influenced return to the clinic or contributed to the observed contraceptive practices in the remaining cohort. Our analysis of the baseline traits, however, indicates similar demographic characteristics. The assessment of contraceptive practice also represents a cross-sectional view of former study participants and outcomes may be subject to prior study experiences and duration of time after study completion. Nonetheless, the results of our analysis suggest a similar follow-up period for participants in both arms and active care-seeking behavior by participants in the posttrial sample.
Conclusion
The DepoText intervention had sustained effects on contraceptive choice for intervention participants compared with controls. Among participants that sought ongoing clinical care, exposure to the DepoText intervention was associated with greater continued use of DMPA or more effective contraceptive methods. Until there is wide-spread uptake of LARC methods for adolescents, it is critical to support adolescent contraceptive choices. This intervention represents a promising strategy to encourage family planning appointment adherence, prevent unintended pregnancy, and promote “meaningful use” of technology for adolescents. Scaled up work to integrate this technology into EHR platforms and to evaluate impact on quality, outcomes, and cost-effectiveness is warranted.
Acknowledgments
We graciously acknowledge the Thomas Wilson Sanitarium Foundation for the Children of Baltimore City who funded the original trial, the DC-Baltimore Research Center on Child Health Disparities, and the National Institute of Nursing Research, which currently funds Cara Buchanan and Dr. Trent’s time (R01 NR013507, PI: Trent). We are especially grateful to the youth who participated in the trial.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Thomas Wilson Sanitarium Foundation for the Children of Baltimore City, DC-Baltimore Research Center on Child Health Disparities, National Institute of Nursing Research (R01 NR013507, PI: Trent).
Footnotes
Author Contributions
MET, KT CRMB :Study conceptualization:
MET :Funding
CRMB, KT, AR :Data Collection
CRMB, KT, MET, SC: Review and analysis of data
CRMB, KT, MET, SC, KKU, AR: Interpretation of data and manuscript development:
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Healthy Teen Network, Health Department Baltimore MD, JH Urban Health Institute, & Center for Adolescent Health. Executive summary: Reducing teen births in Baltimore City No. 1. Baltimore, MD: Baltimore City Health Department; 2008. [Google Scholar]
- 2.Guttmacher Institute. Unintended pregnancy in the United States. [Accessed October 13, 2014];2013 http://www.guttmacher.org/pubs/FB-Unintended-Pregnancy-US.html.
- 3.Guttmacher Institute. American teens’ sexual and reproductive health. [Accessed October 13, 2014];2014 http://www.guttmacher.org/pubs/FB-ATSRH.pdf.
- 4.Linn SW, Rieder J, Coupey SM, Bijur PE. Depot medroxyprogesterone acetate use in inner-city, minority adolescents: continuation rates and characteristics of long-term users. Arch Pediatr Adolesc Med. 1999;153:1068–1072. doi: 10.1001/archpedi.153.10.1068. [DOI] [PubMed] [Google Scholar]
- 5.Polaneczky M, Liblanc M. Long-term depot medroxyprogesterone acetate (DMPA) use in inner-city adolescents. J Adolesc Health. 1998;23:81–88. doi: 10.1016/s1054-139x(98)00014-7. [DOI] [PubMed] [Google Scholar]
- 6.Lindstrom Johnson S, Tandon SD, Trent M, Jones V, Cheng TL. Use of technology with health care providers: perspectives from urban youth. J Pediatr. 2012;160:997–1002. doi: 10.1016/j.jpeds.2011.11.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and technology 2013 (Teens and Tech No. 1) Pew Research Center’s Internet & American Life Project: Pew Research Center/Berkman Center for Internet & Society at Harvard University; 2013. [Google Scholar]
- 8.Santelli JS, Lindberg LD, Finer LB, Singh S. Explaining recent declines in adolescent pregnancy in the United States: the contribution of abstinence and improved contraceptive use. Am J Public Health. 2007;97:150–156. doi: 10.2105/AJPH.2006.089169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Santelli JS, Melnikas AJ. Teen fertility in transition: recent and historic trends in the United States. Annu Rev Public Health. 2010;31:371–834. doi: 10.1146/annurev.publhealth.29.020907.090830. [DOI] [PubMed] [Google Scholar]
- 10.Ammerman SD. The use of Norplant and Depo Provera in adolescents. J Adolesc Health. 1995;16:343–346. doi: 10.1016/S1054-139X(94)00009-4. [DOI] [PubMed] [Google Scholar]
- 11.Trent M, Tomaszewski K. Family planning appointment attendance among urban youth: results from the DepoText Trial. J Adolesc Health. 2013;52:S88. [Google Scholar]
- 12.Belzer ME, Naar-King S, Olson J, et al. The use of cell phone support for non-adherent HIV-infected youth and young adults: an initial randomized and controlled intervention trial. AIDS Behav. 2014;18:686–696. doi: 10.1007/s10461-013-0661-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matheson EC, Derouin A, Gagliano M, Thompson JA, Blood-Siegfried J. Increasing HPV vaccination series completion rates via text message reminders. J Pediatr Health Care. 2014;28:e35–e39. doi: 10.1016/j.pedhc.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 14.Narring F, Junod Perron N, Dominice Dao M, et al. Text-messaging to reduce missed appointment in a youth clinic: a randomized controlled trial. J Epidemiol Community Health. 2013;67:888–891. doi: 10.1136/jech-2013-202510. [DOI] [PubMed] [Google Scholar]
- 15.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36:165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 16.Free C, Knight R, Robertson S, et al. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single-blind, randomized trial. Lancet. 2011;378:49–55. doi: 10.1016/S0140-6736(11)60701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodgers A, Corbett T, Bramley D, et al. Do u smoke after txt? Results of a randomized trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14:255–261. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Castano PM, Bynum JY, Andres R, Lara M, Westhoff C. Effect of daily text messages on oral contraceptive continuation: a randomized controlled trial. Obstet Gynecol. 2012;119:14–20. doi: 10.1097/AOG.0b013e31823d4167. [DOI] [PubMed] [Google Scholar]
- 19.Hall KS, Westhoff CL, Castano PM. The impact of an educational text message intervention on young urban women’s knowledge of oral contraception. Contraception. 2013;87:449–454. doi: 10.1016/j.contraception.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertil Steril. 2012;98:893–897. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howard DL, Wayman R, Strickland JL. Satisfaction with and intention to continue DMPA versus the Mirena IUD among post-partum adolescents through 12 months of follow-up. J Pediatr Adolesc Gynecol. 2013;26:358–365. doi: 10.1016/j.jpag.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 22.Davis AJ. Use of depot medroxyprogesterone acetate contraception in adolescents. J Reprod Med. 1996;41(5 suppl):407–413. [PubMed] [Google Scholar]
- 23.Nelson AL. DMPA: battered and bruised but still needed and used in the USA. Obstet Gynecol. 2010;5:673–686. [Google Scholar]
- 24.Seth C, Kalichman EA, Cherry C, Belcher L, Nachimson D. Sexual coercion, domestic violence, and negotiating condom use among low-income African American women. J Womens Health. 1998;7:371–378. doi: 10.1089/jwh.1998.7.371. [DOI] [PubMed] [Google Scholar]
- 25.Cooper ML, Shapiro CM, Powers AM. Motivations for sex and risky sexual behavior among adolescents and young adults: a functional perspective. J Pers Soc Psychol. 1998;75:1528–1558. doi: 10.1037/0022-3514.75.6.1528. [DOI] [PubMed] [Google Scholar]
- 26.Cromer BA, Smith RD, Blair JM, Dwyer J, Brown RT. A prospective study of adolescents who choose among levonorgestrel implant (norplant), medroxyprogesterone acetate (DMPA), or the combined oral contraceptive pill as contraception. Pediatrics. 1994;94:687–694. [PubMed] [Google Scholar]
- 27.Matson SC, Henderson KA, McGrath GJ. Physical findings and symptoms of depot medroxyprogesterone acetate use in adolescent females. J Pediatr Adolesc Gynecol. 1997;10:18–23. doi: 10.1016/s1083-3188(97)70039-1. [DOI] [PubMed] [Google Scholar]
- 28.Allsworth JE, Secura GM, Zhao Q, Madden T, Peipert JF. The impact of emotional, physical, and sexual abuse on contraceptive method selection and discontinuation. Am J Public Health. 2013;103:1857–1864. doi: 10.2105/AJPH.2013.301371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.American College of Obstetricians and Gynecologists. Depot medroxyprogesterone acetate and bone effects: Committee Opinion No. 602. Obstet Gyecol. 2014;123:1398–1402. doi: 10.1097/01.AOG.0000450758.95422.c8. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. Medical Eligibility Criteria for Contraceptive Use. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 31.Trent M, Thompson C, Tomaszewski K. Text messaging support for urban adolescents and young adults using injectable contraception: outcomes of the DepoText pilot trial. J Adolesc Health. 2015;57:100–106. doi: 10.1016/j.jadohealth.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Trent ME, Rich M, Austin SB, Gordon CM. Quality of life in adolescent girls with polycystic ovary syndrome. Arch Pediatr Adolesc Med. 2002;156:556–560. doi: 10.1001/archpedi.156.6.556. [DOI] [PubMed] [Google Scholar]
- 34.Irons M, Tomaszewski K, Muñoz Buchanan CR, Trent M. Understanding adolescent nonresponsiveness to text messages: lessons from the DepoText trial. J Urban Health. 2015;92:502–512. doi: 10.1007/s11524-015-9950-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Potter J, Koyama A, Coles MS. Addressing the challenges of clinician training for long-acting reversible contraception. JAMA Pediatr. 2015;169:103–104. doi: 10.1001/jamapediatrics.2014.2812. [DOI] [PubMed] [Google Scholar]
- 36.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007–2009. Fertil Steril. 2012;98:893–897. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stanwood NL, Bradley KA. Young pregnant women’s knowledge of modern intrauterine devices. Obstet Gynecol. 2012;108:1417–1422. doi: 10.1097/01.AOG.0000245447.56585.a0. [DOI] [PubMed] [Google Scholar]
- 38.Whitaker AK, Johnson LM, Harwood B, Chiappetta L, Creinin MD, Gold MA. Adolescent and young adult women’s knowledge of and attitudes toward the intrauterine device. Contraception. 2008;78:211–217. doi: 10.1016/j.contraception.2008.04.119. [DOI] [PubMed] [Google Scholar]
- 39.Eisenberg D, McNicholas C, Peipert JF. Cost as a barrier to long-acting reversible contraceptive (LARC) use in adolescents. J Adolesc Health. 2013;52(4 suppl):S59–S63. doi: 10.1016/j.jadohealth.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 40.Mestad R, Secura G, Allsworth JE, Madden T, Zhao Q, Peipert JF. Acceptance of long-acting reversible contraceptive methods by adolescent participants in the contraceptive CHOICE project. Contraception. 2011;84:493–498. doi: 10.1016/j.contraception.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The contraceptive CHOICE project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203:115.e1–115.e7. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Centers for Medicare & Medicaid Services. 2014 definition stage 1 of meaningful use. [Accessed October 13, 2014];2014 http://www.cms.gov/Regulations-andGuidance/Legislation/EHRIncentivePrograms/Meaningful_Use.html.