Abstract
A 77-year-old Japanese woman presented to an ophthalmologist with an erythematous swollen upper eyelid and diplopia which was initially diagnosed to be idiopathic dacryoadenitis on the basis of a histological evaluation of an orbital mass that was in remission following a 3.5-month period of systemic corticosteroid therapy. She subsequently developed respiratory symptoms, and was finally diagnosed with systemic granulomatosis with polyangiitis (GPA) based on the clinical and histological features. She was successfully treated with corticosteroids and azathioprine. Dacryoadenitis in the form of an orbital inflammatory pseudotumor may be an initial presenting feature of GPA, sometimes as the limited phenotype, and occasionally progressing to systemic disease.
Keywords: idiopathic orbital inflammation, inflammatory pseudotumor, magnetic resonance imaging, orbital, Wegener's granulomatosis
Introduction
Granulomatosis with polyangiitis (GPA), which was first described by Heintz Klinger in 1931, was formerly known as Wegener's granulomatosis because of the detailed description of the disease by Friedrich Wegener in 1936. GPA is an autoimmune small-to-medium vessel vasculitis that is characterized by necrotizing granulomatous inflammation. In 1990, the diagnostic criteria of GPA was established by the American College of Rheumatology with 88% sensitivity and 92% specificity in cases in which two or more the following criteria are present: (1) nasal or oral inflammation, (2) respiratory radiographic abnormalities consistent with respiratory tissue destruction, (3) abnormal urinary sediment, and (4) granulomatous inflammation within the artery wall or in the perivascular or extravascular area. Proteinase 3-anti-neutrophil cytoplasmic antibody (PR3-ANCA) was subsequently established as a diagnostic marker of GPA.
Recently, the diagnosis of GPA has been based on clinicopathological findings. The possibility of GPA is increased in patients who are seropositive for ANCA; however, GPA can occur in ANCA-negative individuals. The clinical features of classic, systemic GPA include upper respiratory tract, lung, and kidney symptoms; however, the disease can affect almost any organ. Sometimes only the upper or lower respiratory tract or the eye is involved; this is known as the limited phenotype. We herein report a rare case of myeloperoxidase-ANCA (MPO-ANCA)-positive GPA that initially presented as dacryoadenitis with ptosis and diplopia, but which was followed by the systemic involvement of the upper respiratory tract, lung, and kidney. The patient was successfully treated with corticosteroids and azathioprine.
Case Report
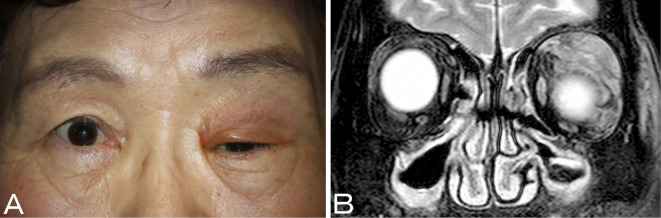
A 77-year-old Japanese woman with underlying hypertension had visited a number of ophthalmic clinics with complaints of left periorbital swelling and pain, visual disturbance, and diplopia. An ophthalmological examination revealed a left-sided erythematous and swollen upper eyelid, ptosis, and medial-inferior primary eye position with restricted upward eye movement (Fig. 1A). The patient's pupil size and pupillary light reflex were normal. A magnetic resonance imaging (MRI) study revealed a left orbital tumor-like mass (Fig. 1B), which involved the neighboring levator palpebrae superioris muscle and superior rectus muscle without the other extraocular muscles. The patient's complete blood counts and blood chemistry were almost normal. Serological tests revealed a slightly elevated C-reactive protein level of 0.14 mg/dL (normal: <0.03 mg/dL) with normal levels of immunoglobulin (Ig)G, IgA, IgM, IgG4, soluble interleukin-2 receptor (sIL-2R), and angiotensin-converting enzyme (ACE), which were not suggestive or diagnostic. She was referred to a cancer hospital 2 months after her initial examination for further investigation.
Figure 1.
Left dacryoadenitis presenting as an erythematous swollen upper eyelid and ptosis (A). Coronal T2-weighted orbital magnetic resonance imaging with spectral presaturation and inversion recovery showing localized, tumor-like left lacrimal gland enlargement with the involvement of the neighboring levator palpebrae superioris muscle and the superior rectus muscle without the other extraocular muscles (B).
During the following month, a diagnostic incisional biopsy of the left orbital mass was performed under the presumptive diagnosis of malignant lymphoma. A histopathological evaluation of a biopsy specimen showed polymorphic inflammatory infiltration by lymphocytes, plasmacytes, and neutrophils, with mild eosinophilia and tissue fibrosis in the lacrimal gland. An immunohistochemical analysis of the specimen was negative for IgG4 and single light chain isotypes (κ and λ). Flow cytometry of the specimen revealed a reactive pattern with no evidence of monoclonal lymphoproliferation. Based on these pathological findings, the patient was diagnosed with dacryoadenitis in the form of an orbital inflammatory pseudotumor, also known as idiopathic orbital inflammation.
After the biopsy procedure, prednisolone (40 mg/day; 1 mg/kg/day) was administered due to the worsening swelling of the upper eyelid, ptosis, and diplopia. Her symptoms gradually improved, and the corticosteroid therapy was tapered within 3.5 months. At two weeks after the cessation of corticosteroids, she gradually developed a non-productive cough. At this point, 8 months after the initial examination, she was referred to our respiratory department with a 2-week history of respiratory symptoms to undergo further investigation and treatment.
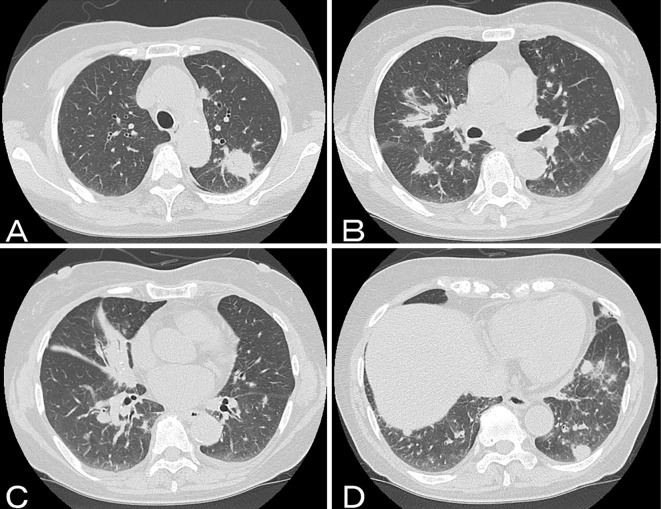
Her vital signs were within the normal limits, and a physical examination, which included an eye examination, revealed no abnormalities. The patient denied any fever, weight loss, appetite loss, general fatigue, or other symptoms apart from the dry cough. A chest roentgenogram revealed bilateral masses and infiltration. A high-resolution computed tomography (CT) scan of the lungs revealed multiple nodules, mass-like consolidation, peribronchial consolidation, and peribronchovascular thickening with atelectasis (Fig. 2). These radiological findings suggested the possibility of perilymphatic distributed disease, including malignancies such as malignant lymphoma, and benign lymphoproliferative disorders such as sarcoidosis, multicentric Castleman disease, and IgG4-related disease. The patient's complete blood counts and blood chemistry were almost normal. Serological tests revealed the following: C-reactive protein, 9.82 mg/dL; sIL-2R, 992 U/mL (normal: <499 U/mL); interleukin-6, 45 pg/mL (normal: <7.9 pg/mL), lysozyme, 13.0 μg/mL (normal: <10.0 μg/mL), and ACE, 15.3 U/L (normal: <25 U/L). Chemiluminescence enzyme immunoassays were negative for PR3-ANCA, but positive for MPO-ANCA (4.4 IU/mL; normal <3.5 IU/mL). A urinalysis revealed microhematuria with 20-29 red blood cells per high power field, and mild proteinuria with a urine protein to urine creatinine ratio of 0.15 g/gcr. Five months before admission to our department, a urinalysis performed at a previous hospital for a preoperative examination revealed microhematuria with red blood cell casts and dysmorphic red blood cells.
Figure 2.
Axial computed tomography of the chest showing a mass-like consolidation (A), peribronchial consolidation (B), peribronchovascular thickening with atelectasis (C), and multiple nodules (D).
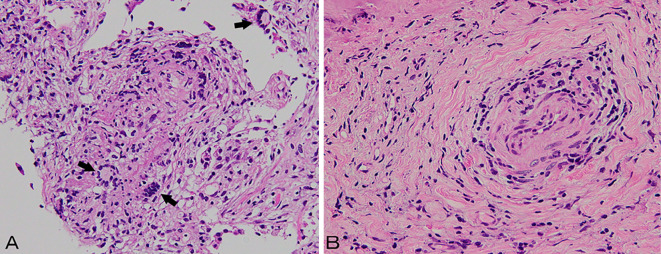
An examination of the patient's bronchial lavage fluid revealed no infectious organisms or malignant cells. The patient's severe cough precluded the collection of an adequate amount of transbronchial lung biopsy tissue for histopathological assessment. We therefore performed a CT-guided lung biopsy instead. This revealed pleomorphic inflammatory infiltration with lymphocytes, plasmacytes, and neutrophils, with mild eosinophilia and organizing pneumonia-like fibrosis; this was similar to the findings of the lacrimal tissue samples that were biopsied at a previous hospital. Neutrophil-infiltrated microabscesses and necrotizing vasculitis with multinucleated giant cells were also observed. We re-investigated the previously biopsied lacrimal tissue samples and detected the presence of necrotizing vasculitis without granulomatosis (Fig. 3). Follow-up orbital and face MRI only revealed sinus mucosal thickening, which was compatible with chronic sinusitis without orbital involvement. Based on these clinical and pathological features, we diagnosed the patient with classic, systemic GPA initially presenting as dacryoadenitis followed by the systemic involvement of the lung and kidney in the subsequent 8 months.
Figure 3.
Histological images: a computed tomography-guided percutaneous lung biopsy specimen revealing pleomorphic inflammatory infiltration of lymphocytes, plasmacytes, and neutrophils with mild eosinophilia, organizing pneumonia-like fibrosis, and neutrophil-infiltrated microabscesses; necrotizing vasculitis with multinucleated giant cells (A: arrow) [Hematoxylin and Eosin (H&E) staining, 200x]; and an incisional biopsy specimen of an orbital mass revealing necrotizing vasculitis (B) with polymorphic inflammatory infiltration and tissue fibrosis in the lacrimal gland (H&E staining, 400x).
At 14 days after admission, the patient developed right-sided conjunctivitis. Her MPO-ANCA titer was increased to 11.5 IU/mL, and oral prednisolone (40 mg daily) was initiated. The patient's dry cough, abnormal radiological findings, and conjunctivitis resolved rapidly, and remission was achieved within 3 weeks. Her urinary parameters slowly normalized over the course of 8 weeks. Oral steroid therapy was tapered on an outpatient basis. At 8 weeks after treatment initiation, her prednisolone dose was tapered to 20 mg daily and azathioprine was added for maintenance therapy. The patient currently remains asymptomatic with no further radiological or urinalysis abnormalities.
Discussion
We confirmed a clinical triad of GPA symptoms and findings in our patient: upper respiratory tract, lung, and kidney abnormalities with pathological findings that were consistent with GPA (microabscesses, necrotizing vasculitis, multinucleated giant cells, polymorphic inflammatory infiltration, and tissue fibrosis). The patient satisfied all of the diagnostic criteria for GPA according to the American College of Rheumatology (1), Chapel Hill Consensus Conference (2), and European Medicines Agency (3).
GPA is an ANCA-associated vasculitis, in which the diagnostic marker is PR3-ANCA. The sensitivity and specificity of this marker are influenced by the disease activity, and the overall sensitivity of PR3-ANCA for GPA ranges from 34-92%, with a specificity of 88-100%. In patients with active disease, the pooled sensitivity and specificity are 91% [confidence interval (CI), 87-95%] and 99% (CI, 97-99.9%), respectively. In those with inactive disease, the pooled sensitivity and specificity are 63% and 99.5%, respectively (4). MPO-ANCA can be positive in less than 10% of patients with GPA (5). The presence of MPO-ANCA without PR3-ANCA in the present patient was somewhat atypical but was still compatible with the above-mentioned criteria.
Orbital involvement occurs in 45-60% of patients with GPA during the course of the disease and is the presenting feature in 16% of patients (6). Conjunctivitis and episcleritis are common manifestations that are seen in 52.1% and 39.3% of cases, respectively (7). Orbital inflammatory disease develops in 19.7% of patients with GPA and is therefore considered a relatively rare presentation (7).
Orbital GPA may occur in a limited form with isolated orbital involvement or a component of the systemic form and can develop within the orbital tissue itself or from the adjacent paranasal sinuses or the nasal cavity. Among the orbital tissues, the lacrimal gland is rarely affected and is especially uncommon as the initial presenting location (8-14). In addition, a recent report discussed the retrospective analysis of orbital biopsies in 247 cases, in which 69 patients were found to have orbital inflammatory disease with lacrimal gland involvement, and 7 patients had a final diagnosis of GPA (15).
Among the 7 previously reported cases (8-14) with dacryoadenitis as the initial presenting feature of GPA, no cases were positive for MPO-ANCA; 4 cases were positive for PR3-ANCA (10, 11, 13, 14), 1 case was negative for ANCA (9), and 2 cases were unknown. Thus, the present case is, to the best of our knowledge, the world's first case of MPO-ANCA-positive GPA that initially presented as dacryoadenitis.
Regarding the orbital manifestation in our patient, ptosis and diplopia were caused by dysfunction of the levator palpebrae superioris muscle and the superior rectus muscle, respectively. The pathophysiology was considered to be lacrimal gland inflammation, also known as dacryoadenitis, involving the two above-mentioned muscles themselves and a superior branch of the oculomotor nerve, which innervates the two muscles.
It is difficult to diagnose orbital GPA, and the interval from presentation to a definitive diagnosis ranges from 3-20 months (mean, 12.1) (15). One reason for this is that the diagnostic criteria for systemic GPA are not adaptable to limited GPA or systemic GPA with isolated orbital involvement before the progression to systemic disease. The second is the low sensitivity of a histological diagnosis of biopsy specimens of orbital tissue; the histopathological changes may be subtle and can be overlooked; furthermore, the classic histopathological triad of vasculitis, tissue necrosis, and granulomatous inflammation is only present in 25-50% of orbital biopsies (16).
In some cases of orbital GPA, the disease is locally destructive with irreversible functional loss or progression to fatal systemic disease. In order to promptly initiate advanced immunosuppressive therapy, it is important to perform a systemic work-up that includes an imaging study of the chest, urinalysis, and serological studies for ANCA and to make an early diagnosis. In the present case, had abnormal urinalysis results raised the suspicion of the possibility of GPA, the diagnosis of GPA could have been made before the development of symptomatic systemic disease.
In conclusion, we herein described a rare case of MPO-ANCA-positive GPA initially presenting as dacryoadenitis in the form of an orbital inflammatory pseudotumor with ptosis and diplopia followed by the systemic involvement of the upper respiratory tract, lung, and kidney. It is difficult to make an early diagnosis in cases of atypical and orbital-onset GPA because of the distribution of symptomatic lesions (in both time and space) and the low sensitivity of pathological diagnostic methods. Collaborative multidisciplinary diagnostic efforts are required for timely treatment, and clinicians should be aware of the possibility of orbital-onset GPA.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We would like to thank Dr. Tamiko Takemura of the Department of Pathology at the Japanese Red Cross Medical Center for evaluating the pathological findings, Dr. Tetsumasa Kamei of the Department of Neurology at the Shonan Fujisawa Tokushukai Hospital for performing the neuro-ophthalmological evaluation, and Orimpiakai Olympia Ophthalmology Hospital and National Cancer Center Hospital for providing valuable data and the biopsy samples of lacrimal tissues.
References
- 1.Leavitt RY, Fauci AS, Bloch DA, et al. The American College of Rheumatology 1990 criteria for the classification of Wegener's granulomatosis. Arthritis Rheum 33: 1101-1107, 1990. [DOI] [PubMed] [Google Scholar]
- 2.Jennette JC, Falk RJ, Bacon PA, et al. 2012 Revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 65: 1-11, 2013. [DOI] [PubMed] [Google Scholar]
- 3.Watts R, Lane S, Hanslik T, et al. Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis 66: 222-227, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rao JK, Weinberger M, Oddone EZ, Allen NB, Landsman P, Feussner JR. The role of antineutrophil cytoplasmic antibody (c-ANCA) testing in the diagnosis of Wegener granulomatosis. A literature review and meta-analysis. Ann Intern Med 123: 925-932, 1995. [DOI] [PubMed] [Google Scholar]
- 5.Kallenberg CG, Heeringa P, Stegeman CA. Mechanisms of Disease: pathogenesis and treatment of ANCA-associated vasculitides. Nat Clin Pract Rheumatol 2: 661-670, 2006. [DOI] [PubMed] [Google Scholar]
- 6.Hoffman GS, Kerr GS, Leavitt RY, et al. Wegener granulomatosis: an analysis of 158 patients. Ann Intern Med 116: 488-498, 1992. [DOI] [PubMed] [Google Scholar]
- 7.Rothschild PR, Pagnoux C, Seror R, Brézin AP, Delair E, Guillevin L. Ophthalmologic manifestations of systemic necrotizing vasculitides at diagnosis: a retrospective study of 1286 patients and review of the literature. Semin Arthritis Rheum 42: 507-514, 2013. [DOI] [PubMed] [Google Scholar]
- 8.Leavitt JA, Butrus SI. Wegener's granulomatosis presenting as dacryoadenitis. Cornea 10: 542-545, 1991. [DOI] [PubMed] [Google Scholar]
- 9.Lanza JT, Ku Y, Lucente FE, Har-El G. Wegener's granulomatosis of the orbit: lacrimal gland involvement as a major sign. Am J Otolaryngol 16: 119-122, 1995. [DOI] [PubMed] [Google Scholar]
- 10.Soheilian M, Bagheri A, Aletaha M. Dacryoadenitis as the earliest presenting manifestation of systemic Wegener's granulomatosis. Eur J Ophthalmol 12: 241-243, 2002. [DOI] [PubMed] [Google Scholar]
- 11.Danda D, Mathew AJ, Mathew J. Wegener's granulomatosis: a rare presentation. Clin Rheumatol 27: 273-275, 2008. [DOI] [PubMed] [Google Scholar]
- 12.Kiratli H, Sekeroğlu MA, Soylemezoğlu F. Unilateral dacryoadenitis as the sole presenting sign of Wegener's granulomatosis. Orbit 27: 157-160, 2008. [DOI] [PubMed] [Google Scholar]
- 13.Khanna D, Shrivastava A. Suppurative dacroadenitis causing ocular sicca syndrome in classic Wegener's granulomatosis. Indian J Ophthalmol 59: 151-153, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lopes Caçola R, Morais SA, Carvalho R, Môço R. Bilateral dacryoadenitis as initial presentation of a locally aggressive and unresponsive limited form of orbital granulomatosis with polyangiitis. BMJ Case Rep 2016(Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan LT, Davagnanam I, Isa H, et al. Clinical and imaging features of lacrimal gland involvement in granulomatosis with polyangiitis. Ophthalmology 122: 2125-2129, 2015. [DOI] [PubMed] [Google Scholar]
- 16.Kalina PH, Lie JT, Campbell RJ, Garrity JA. Diagnostic value and limitations of orbital biopsy in Wegener's granulomatosis. Ophthalmology 99: 120-124, 1992. [DOI] [PubMed] [Google Scholar]