Abstract
Lung cancer has a predilection to widely metastasize to the liver, bone, brain and adrenal glands. Metastasis of primary lung tumors to the stomach is infrequent, with only sporadic cases reported. Most cases are asymptomatic and diagnosed post-mortem on autopsy. The incidence of symptomatic gastrointestinal metastases is extremely rare. Herein, we describe a case of gastric metastasis by squamous cell lung carcinoma, presenting as melena and diagnosed by esophagogastroduodenoscopy. To the best of our knowledge, only twenty other cases in the English literature have reported symptomatic gastric metastasis of lung cancer diagnosed by endoscopic biopsy. A brief review of the literature shows gastric metastasis of lung cancer to have a predilection to occur most frequently in male smokers with the most common type of tumor likely to be squamous cell carcinoma.
Key words: Lung cancer, squamous cell lung carcinoma, metastasis to the stomach, GI metastasis, Esophagogastroduodenoscopy
Introduction
Lung cancer is the most common cancer worldwide and the leading cause of tumorrelated deaths. It has a predilection to widely metastasize to the liver, bone, brain and adrenal glands. Metastasis of primary lung tumors to the gastrointestinal tract is infrequent, with only sporadic cases reported. The incidence of symptomatic gastrointestinal metastases is extremely rare. In this report, we describe a case of a squamous cell lung carcinoma with metastasis to the stomach.
Case Report
A 90-year-old man with a history of left upper lobe pulmonary nodule on prior imaging presented with dark tarry stools, fatigue and repeated falls that progressively became worse over a one-month period. A week prior to presentation, he had a syncopal episode. He had not had an EGD or colonoscopy done in about 10 years. His social history is notable for a remote history of smoking.
Five months prior to this presentation, a 2.4 cm left upper lobe pulmonary nodule suspicious for neoplasm was incidentally found on CXR. The patient had declined any invasive procedures and opted to monitor the nodule thru serial chest computer tomography (CT) scans (Figure 1A). Two months later, new scattered 8 mm hepatic nodular hypodensities suspicious for metastatic lesions were found on a CT scan of the abdomen and pelvis (Figure 1B). A [18F] fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET)/CT (Figure 1C) showed a 4.4×2.9 cm FDG-avid lung mass (SUV max 12.3 g/mL) and 4 foci of increased radiotracer uptake corresponding to metastatic liver lesions; No FDG-avid mediastinal lymphadenopathy were identified. A CT head was negative for any metastases. Clinically, he appeared to have a T2aN0M1b stage IV primary lung neoplasm. On physical exam, the patient had pale conjunctivae and dry mucous membranes. His breath sounds were diminished on the left lower lobe. He had an ecchymosis over the anterior abdomen that was non-tender. FOBT was positive on rectal exam. His labs showed a hemoglobin of 5.7 g/dL and a hematocrit of 18.1%. His esophagogastroduodenoscopy (EGD) showed a nonobstructing, non-bleeding, cratered gastric ulcer at the greater curvature of the gastric body. The ulcer had a clean base, no stigmata of bleeding and no evidence of perforation. A gastric ulcer biopsy showed metastatic squamous carcinoma involving the base of the gastric mucosa without surface involvement on hematoxylin and eosin stain (Figure 2). Although the standard of care for stage IV Squamous Cell Lung Cancer is combination chemotherapy with platinum doublet, he was referred to palliative care given patient’s extremely poor functional status. He passed away 54 days after his presentation with GI bleed. The family declined an autopsy
Figure 1.
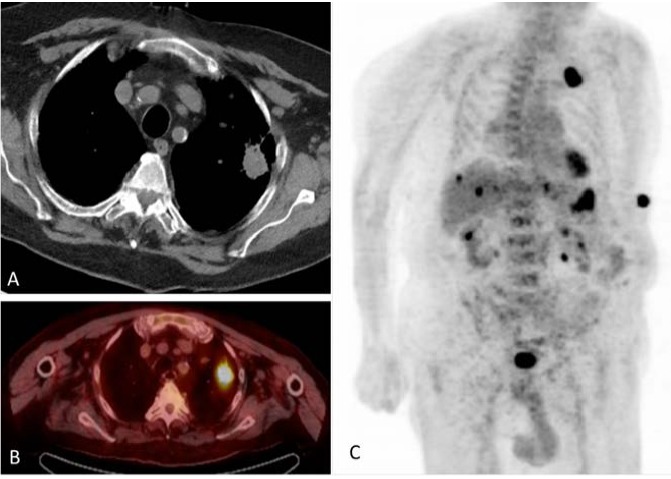
Computed tomography scan and [18F] fluoro-2-deoxy-D-glucose positron emission tomography. A solitary 2.4 cm Left Upper Lobe (LUL) nodule on CT scan (A) and FDG-PET/CT (B) C: [18F] fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET)/CT showing FDG-avid masses in the left upper lobe and right and left hepatic Lobes
Figure 2.
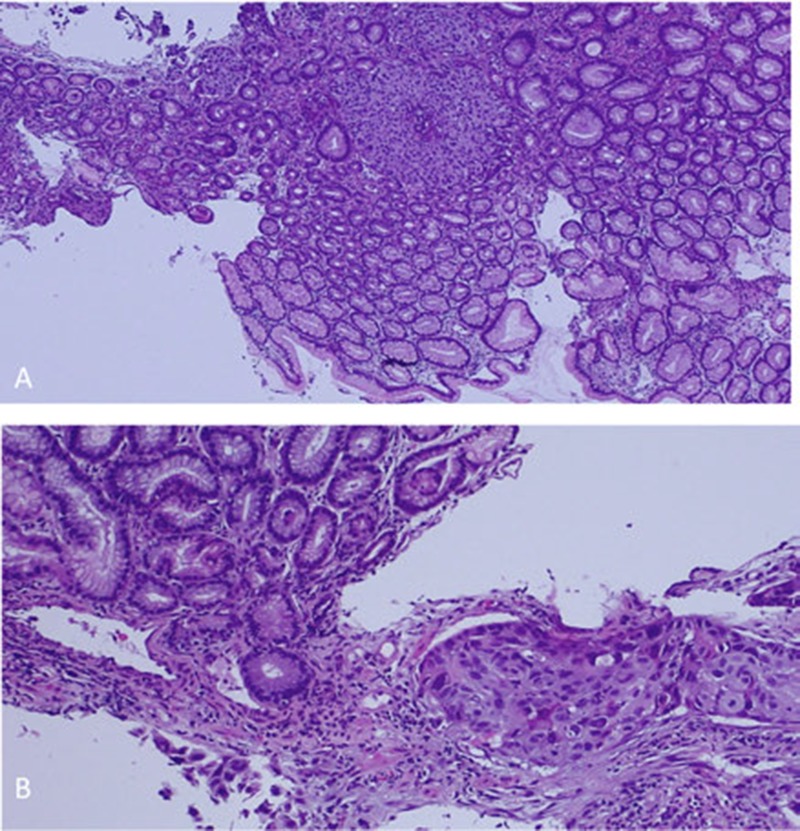
Histopathological examination: hematoxylin and eosin stain showing invasive squamous cell carcinoma under uninvolved gastric mucosa. Low (A) and High (B) magnification.
Discussion
Lung cancer most commonly metastasizes to liver, adrenal glands, bone and brain. Metastasis to the GI system is considered uncommon; although a higher prevalence has been reported on autopsies (14%).1 Symptomatic manifestations of GI metastasis are rare with only a few cases published. Of the GI sites where lung cancer metastasizes, stomach is an extremely rare site and is usually discovered on autopsies (<2%) 2,3 To the best of our knowledge, 20 cases in the English literature have reported symptomatic gastric metastasis of lung cancer diagnosed by endoscopic biopsy. Here, we report a case of squamous cell lung carcinoma metastasizing to the stomach along with a brief review of the cases reported in the literature (Table 1).
Table 1.
Reported cases of symptomatic metastatic squamous cell lung carcinoma to the stomach in the English literature.
| Author | Age | Sex | Smoking | Cancer cell type | Primary location | Clinical presentation | Gastric location | Other metastatic sites | Time between discovery and death |
|---|---|---|---|---|---|---|---|---|---|
| Azar | 90 | M | Y | Squamous cell | LUL | Melena | Greater curvature | Liver | 54 days |
| Yang 14 | 71 | M | Y | Squamous cell | LLL | Melena | - | None | 136 days |
| Yang 24 | 65 | M | Y | Squamous cell | RML | Melena | - | Pleural effusion, bone | 90 days |
| Yang 34 | 62 | M | Y | Adenocarcinoma | RUL | Melena | - | Bone | 371 days |
| Casella7 | 63 | M | Y | Small cell | LU hilar region | Epigastralgia, constipation | Gastric Corpus | LNs, pleural effusions, liver | 1 month |
| Suzaki11 | 45 | M | - | Adenocarcinoma | RML | Perforation | Fundus &, corpus at Greater curvature | None | 13 days |
| Fletcher9 | 70 | M | Y | Squamous cell | LLL | Perforation, epigastralgia | Greater curvature | None | 2 months |
| Kim12 | 71 | M | Y | Squamous cell | RLL | No abdominal Sx | Gastric corpus | LNs, spleen, pancreas | 11 months |
| Maeda8 | 60 | F | - | Small cell | RLL | Nausea, vomiting | Gastric corpus & greater curvature | ~ 80 Skin tumors | - |
| Kim 16 | 67 | M | N | Adenocarcinoma | LUL | Abdominal pain | - | Lung | 80 days |
| Kim 26 | 72 | M | Y | Large cell | RUL | No symptoms | - | Lung, brain, adrenal gland | 67 days |
| Alpar13 | 66 | M | Y | Squamous cell | RUL | Epigastralgia, vomiting | - | Liver, LNs | 2 months |
| Hamatake14 | 65 | M | Y | Adenocarcinoma | LLL | Hematemesis | Gastric corpus | Lingula, Chest wall | 147 days |
| Schmidt10 | 61 | M | - | Adenocarcinoma | Left hilum | Epigastralgia | Gastric fundus | LN, Brain | 21 days |
| Yamamoto15 | 80 | M | Y | Adenocarcinoma | Left lung | Epigastralgia | Upper stomach | Brain | 18 months |
| Kadakia 116 | - | M | - | Squamous cell | - | Acute GI bleed | Gastric corpus | - | - |
| Kadakia 216 | - | M/F | - | Squamous cell | - | Acute GI bleed | Gastric corpus | - | - |
| Kadakia 316 | - | M/F | - | Squamous cell | - | Anorexia, wt loss, IDA | Gastric Antrum | Duodenum | - |
| Aokage15 | 69 | M | - | Pleiomorphic | RUL | Fatigue, severe anemia | Anterial wasll of md-stomach | None | 5 years |
| Aokage25 | 62 | M | - | Pleiomorphic | LUL | Nos | Gastric fundus | None | 4 years |
| Miyazaki17 | 54 | M | - | Squamous cell | RUL | Epigastralgia, anemia | Gastric Antrum | Colon, liver | - |
-, unknown or not reported; Sx: Symptoms; LNs: Lymph nodes; M: Male; Y: Yes.
Squamous cell carcinoma has been reported as the most common type of lung cancer metastasizing to the entirety of the GI system.1-4 Our case, along with the majority of gastric metastases reported in literature (Table 1) support the case of Squamous cell carcinoma also being the most common type of lung cancer metastasizing to the stomach. Surprisingly, the second most common type is adenocarcinoma; a difficult pathological diagnosis to establish given the glandular epithelium of the stomach. Cases of pleiomorphic,5 large6 and small cell carcinoma7,8 have also been reported. From an epidemiological point of view, the vast majority of gastric metastases present in male smokers. One of the only 2 cases to report incidence in a female presented uniquely with small cell carcinoma metastasizing to 2 different sites of gastric metastases and over 80 cutaneous ones.8 Not a single case reported a non-smoker; although some cases did not report a smoking status. Interestingly, our case occurred in the eldest individual so far (age range: 45-90).
Metastatic spread to the GI system can present with symptoms including abdominal pain, GI bleeding, bowel obstruction, peritonitis and perforation. The two most common symptoms associated with gastric metastasis in our review were melena and epigastric pain (Table 1). Three cases presented with perforation,9-11 one of which was chemotherapy-induced.11 Only 3 reported cases5,6,12 presented with no abdominal symptoms, one of which was diagnosed by FDG-PET/CT.
Metastasis to the stomach can arise from any lobe of the lung (in our case LUL); but so far only 2 cases7,10 reported a gastric metastasis with a hilar primary. In contrast to esophageal metastases which is thought to be through direct extension, metastasis to the stomach, just like bowel is through hematogenous and lymphatic routes. Figure 2B suggests that, in our case, metastasis occurred hematogenously, either intravascularly or through lymphatics. The most common site of metastasis appears to be the gastric corpus; while our case’s site of metastasis was the greater curvature.
The higher prevalence of GI metastases found on autopsies compared to the reported cases diagnosed by endoscopy suggests metastasis to GI might be a late event in the evolution of the tumor. The presence of other sites of metastases in our case and most of the literature supports this hypothesis. Interestingly, while a bull’s eye target lesion is a well-established radiologic sign of metastasis, metastasis to the stomach does not show this sign on imaging.
Metastasis to the GI system is associated with poor prognosis.12 A study by Yang showed a relatively longer survival rate for metastasis to the stomach than other sites, especially in 2 cases of squamous cell carcinoma. By comparison, our patient had a much shorter time until death (54 days vs 136 and 90) which could be explained by his older age (90 y-o vs 71 and 65). Interestingly, the only 2 cases with a good prognosis (>4 years survival rate) were the pleiomorphic tumors reported by Aokage. 5
Conclusions
Overall, we report here a rare case of metastasis of Squamous Cell Lung Carcinoma to the stomach presenting as melena and review the literature on gastric metastases of lung cancers. While gastric metastasis of lung tumors is very rare, it should be considered in patients with known lung masses presenting with melena. We find gastric metastases of lung tumors to have a predilection to occur in male smokers with the most common type of tumor likely to be squamous cell carcinoma. The most common presentations are epigastric pain and melena. Our conclusions are limited by the small number of reported cases.
Acknowledgements
This material is the result of work supported with resources and the use of facilities at the Stratton Veterans Affairs Medical Center, Albany, NY, U.S.A
References
- 1.Antler AS, Ough Y, Pitchumoni CS, et al. Gastrointestinal metastases from malignant tumors of the lung. Cancer 1982;49:170-2. [DOI] [PubMed] [Google Scholar]
- 2.Berger A, Cellier C, Daniel C, et al. Small bowel metastases from primary carcinoma of the lung: clinical findings and outcome. Am J Gastroenterol 1999;94:1884-7. [DOI] [PubMed] [Google Scholar]
- 3.McNeill PM, Wagman LD, Neifeld JP. Small bowel metastases from primary carcinoma of the lung. Cancer 1987;59: 1486-9. [DOI] [PubMed] [Google Scholar]
- 4.Yang CJ, Hwang JJ, Kang WY, et al. Gastro-intestinal metastasis of primary lung carcinoma: clinical presentations and outcome. Lung Cancer J 2006;54: 319-23. [DOI] [PubMed] [Google Scholar]
- 5.Aokage K, Yoshida J, Ishii G, et al. Long-term survival in two cases of resected gastric metastasis of pulmonary pleomorphic carcinoma. J Thorac Oncol 2008;3:796-9. [DOI] [PubMed] [Google Scholar]
- 6.Kim MS, Kook EH, Ahn SH, et al. Gastrointestinal metastasis of lung cancer with special emphasis on a longterm survivor after operation. J Cancer Res Clin Oncol 2009;135:297-301. [DOI] [PubMed] [Google Scholar]
- 7.Casella G, Di BC Cambareri AR, et al. Gastric metastasis by lung small cell carcinoma. World J Gastroenterol 2006;12:4096-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maeda J, Miyake M, Tokita K, et al. Small cell lung cancer with extensive cutaneous and gastric metastases. Internal Med 1992;31:1325-8. [DOI] [PubMed] [Google Scholar]
- 9.Fletcher MS. Gastric perforation secondary to metastatic carcinoma of the lung: a case report. Cancer 1980;46:1879-82. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt G, Borsch G, Von Liebe S, Bohm E. Gastric perforation secondary to metastatic bronchogenic carcinoma. Hepato-gastroenterol 1985;32:103-5. [PubMed] [Google Scholar]
- 11.Suzaki N, Hiraki A, Ueoka H, et al. Gastric perforation due to metastasis from adenocarcinoma of the lung. Anticancer Res 2002;22:1209-12. [PubMed] [Google Scholar]
- 12.Kim YI, Kang BC, Sung SH. Surgically resected gastric metastasis of pulmonary squamous cell carcinoma. World J Gastrointest Surg 2013;5:278-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alpar S, Kurt OK, Ucar N, et al. A case of squamous cell lung carcinoma with gastric metastasis. South Med J 2006;99:1313-4. [DOI] [PubMed] [Google Scholar]
- 14.Hamatake M, Ishida T, Yamazaki K, et al. Lung cancer with p53 expression and a solitary metastasis to the stomach: a case report. Ann Thorac Cardiovasc Surg 2001;7:162-5. [PubMed] [Google Scholar]
- 15.Yamamoto M, Matsuzaki K, Kusumoto H, et al. Gastric metastasis from lung carcinoma. Case report. Hepatogastroenterol 2002;49:363-5. [PubMed] [Google Scholar]
- 16.Kadakia SC, Parker A, Canales L. Metastatic tumors to the upper gastrointestinal tract: endoscopic experience. Am J Gastroenterol 1992;87:1418-23. [PubMed] [Google Scholar]
- 17.Miyazaki J, Hirota S, Abe T. Metastasis of lung cancer to the gastrointestinal tract, presenting with a volcano-like ulcerated mass. Dig Endosc 2015;27: 397-8. [DOI] [PubMed] [Google Scholar]


