Foetal alcohol spectrum disorder (FASD) is a complex neurodevelopmental disorder caused by prenatal alcohol exposure (PAE). In some individuals, characteristic facial features result from the teratogenic effect of first trimester PAE.
In response to limited training opportunities in FASD, lack of a nationally adopted diagnostic instrument and confusion about diagnostic criteria, The Australian Guide to the Diagnosis of Fetal Alcohol Spectrum Disorder has been developed, funded by the Commonwealth Department of Health (DoH).
Building on a literature review of diagnostic criteria and guidelines from Canada and the USA,1, 2, 3, 4 Delphi surveys5, 6, 7, 8, 9 and a consensus workshop using the GRADE approach,10, 11 an Australian diagnostic instrument was developed in 2012. In 2015–2016, with additional funding from the DoH, a feasibility trial was conducted, and the instrument, guide and e‐learning modules were finalised and harmonised with the new Canadian guideline for diagnosis of FASD.12 The Australian Guide to the Diagnosis of Fetal Alcohol Spectrum Disorder and e‐learning modules were released in mid‐2016 and are freely available at http://alcoholpregnancy.telethonkids.org.au/australian‐fasd‐diagnostic‐instrument/australian‐guide‐to‐the‐diagnosis‐of‐fasd/. This includes clinical forms that can be used during evaluation.
A key recommendation in the guide is the adoption of FASD as a diagnostic term, with two subcategories: FASD with three sentinel facial features and FASD with less than three sentinel facial features. Diagnostic criteria relate to PAE, severe neurodevelopmental impairment in 3 out of 10 domains and sentinel facial features (small palpebral fissures, smooth philtrum and thin upper lip) (Table 1; Fig. 1). FASD with three sentinel facial features replaces the diagnosis of foetal alcohol syndrome, but without a requirement for growth impairment.11 FASD with less than three sentinel facial features encompasses the previous categories of partial foetal alcohol syndrome and neurodevelopmental disorder‐alcohol exposed.11 Co‐existing or alternative diagnoses including genetic conditions (e.g. microdeletions or duplications), effects of other teratogens and prenatal exposures, as well as the effects of postnatal exposures such as early life trauma and brain injury should be considered.
Table 1.
Diagnostic criteria and categories for foetal alcohol spectrum disorder (FASD)
| Diagnostic criteria | Diagnostic categories | |
|---|---|---|
| FASD with three sentinel facial features | FASD with less than three sentinel facial features | |
| Prenatal alcohol exposure | Confirmed or unknown | Confirmed |
Neurodevelopmental domains
|
Severe impairment† in at least three neurodevelopmental domains | Severe impairment† in at least three neurodevelopmental domains |
Sentinel facial features
|
Presence of three sentinel facial features | Presence of 0, 1 or 2 sentinel facial features |
Severe impairment is defined as either a global score or a major subdomain score on a standardised validated neurodevelopmental scale that is ≤2 standard deviation below the mean or <3rd percentile.
Figure 1.
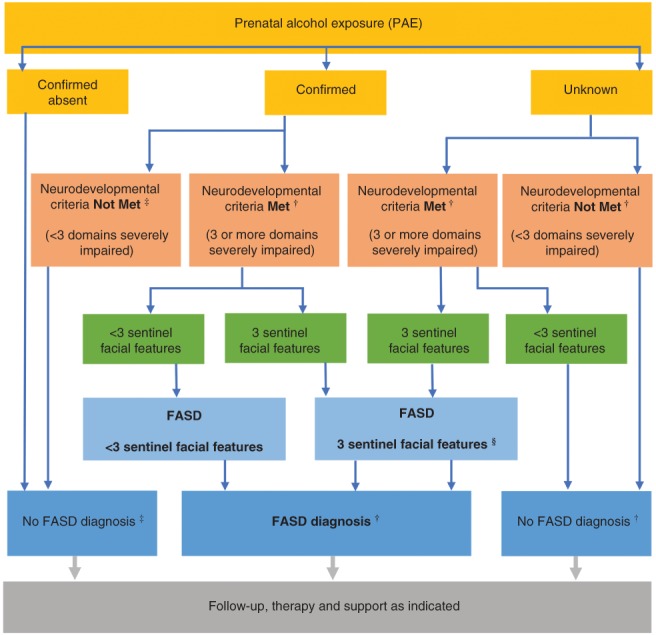
Australian diagnostic algorithm for foetal alcohol spectrum disorder (FASD). †Assessment fully completed and other diagnosis have been considered. Currency of assessment is also assumed. For infants and children under 6 years of age, severe global developmental delay meets criteria for neurodevelopmental impairment (in three or more domains) if it is confirmed on a standardised assessment tool (e.g. Bayley or Griffiths). ‡In the presence of confirmed PAE, reassessment of neurodevelopmental domains can be considered as clinically indicated (e.g. if there is a decline in an individual's functional skills or adaptive behaviour over time). §In infants and young children under 6 years of age with microcephaly and all three sentinel facial features, a diagnosis of FASD with three sentinel facial features can be made, whether PAE is confirmed or unknown, even without evidence of severe neurodevelopmental impairment in three domains based on standardised assessment. (Modified from Cook et al.,12 fig. 1, with permission.)
The diagnosis of FASD requires multidisciplinary assessment including comprehensive physical and developmental assessment, as well as psychometric testing, preferably by a multidisciplinary diagnostic team, and typically led by a medical specialist such as a paediatrician, psychiatrist or geneticist.
The assessment process may be confronting for the individual or caregiver who should provide informed consent beforehand, and receive appropriate support as required. This is particularly salient when biological parents or family are involved. An assessment report outlining the individual's strengths and difficulties, and recommendations should be provided to the family and referring clinician or agency. The value of sharing this information with relevant service providers (including teachers) should be discussed. If FASD is diagnosed, written information about the condition and contact details for the National Organisation for FASD (http://www.nofasd.org/) should be provided.
Dissemination of the guide and the e‐learning modules aims to standardise FASD diagnosis. We hope that it will provide clinicians with increased confidence to consider a diagnosis of FASD, the knowledge to refer for or make the diagnosis, and the information needed to manage and support individuals and families living with FASD. The guide will be updated as new evidence emerges, to ensure it reflects current knowledge and best practice in the evolving field of FASD. Having national, standardised criteria for diagnosis will also improve our ability to advocate for services, monitor FASD prevalence, and support efforts to reduce PAE and hence enable primary prevention of FASD.
Acknowledgements
The trial and implementation phase of the diagnostic instrument for foetal alcohol spectrum disorder (FASD) in Australia was funded through a contract from the Commonwealth Department of Health and benefited from the contribution of time, intellectual input and commitment by members of the Expert Review Panel (Professor EJ Elliott (Chair), Professor C Bower, Dr J Fitzpatrick, Ms V Russell, Dr D Shelton, Dr A Wilkins and Dr M Zimmet) and the Steering Group (Professor C Bower (Chair), Mr Scott Avery, Dr Felicity Collins, Dr Jennifer Delima, Professor EJ Elliott, Dr J Fitzpatrick, Ms Andrea Lammel, Ms V Russell, Dr D Shelton, Dr Lydia So, Dr David Thomas, Dr A Wilkins and Dr M Zimmet). We thank members of the Telethon Kids Institute's Alcohol, Pregnancy and FASD Research Program (Roslyn Giglia, Noni Walker, Heather Jones and Eliza Offereins). We are grateful to Dr Jocelynn Cooke and colleagues, who provided valuable advice and further detail on the Canadian Guidelines. The online modules were developed by Dr M Zimmet, Professor EJ Elliott, J Doorey and Professor C Bower. We acknowledge the technical expertise of Dr Rob Phillips, Dave Wheeler, Rob Bull and Pete Phillips in the development of the modules, and Melanie Hogan, Reverb Pty Ltd for use of her DVD ‘The Story of Alcohol Use in Pregnancy and Fetal Alcohol Spectrum Disorders’. We also thank the clinicians, parents and carers who participated in the trial. EJ Elliott is supported by an NHMRC Practitioner Fellowship (no. 1021480).
References
- 1. Astley SJ. Diagnostic Guide for Fetal Alcohol Spectrum Disorders: The 4‐Digit Diagnostic Code, 3rd edn. Seattle, WA: University of Washington, 2004. [Google Scholar]
- 2. Centers for Disease Control and Prevention . Fetal Alcohol Syndrome: Guidelines for Referral and Diagnosis. Atlanta, GA: National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Effect, 2004. [Google Scholar]
- 3. Chudley A, Conry J, Cook J, Loock C, Rosales T, LeBlanc N. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. Can. Med. Assoc. J. 2005; 172: S1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hoyme HE, May PA, Kalberg WO et al. A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: Clarification of the 1996 Institute of Medicine Criteria. Pediatrics 2005; 115: 39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jones HM, McKenzie A, Miers S et al. Involving consumers and the community in the development of a diagnostic instrument for fetal alcohol spectrum disorders in Australia. Health Res. Policy Syst. 2013; 11: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Watkins R, Elliott E, Halliday J et al. A modified Delphi study of screening for fetal alcohol spectrum disorders in Australia. BMC Pediatr. 2013; 13: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Watkins R, Elliott E, Mutch R et al. Health professionals’ perceptions about the adoption of existing guidelines for the diagnosis of fetal alcohol spectrum disorders in Australia. BMC Pediatr. 2012; 12: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Watkins RE, Elliott EJ, Mutch RC et al. Consensus diagnostic criteria for fetal alcohol spectrum disorders in Australia: A modified Delphi study. BMJ Open 2012; 2: e001918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Watkins RE, Elliott EJ, Wilkins A et al. Fetal alcohol spectrum disorder: Development of consensus referral criteria for specialist diagnostic assessment in Australia. BMC Pediatr. 2014; 14: 178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knotterus A. GRADE guidelines: A new series of articles in the Journal of Clinical Epidemiology. J. Clin. Epidemiol. 2011; 64: 380–2. [DOI] [PubMed] [Google Scholar]
- 11. Watkins R, Elliott E, Wilkins A et al. Recommendations from a consensus development workshop on the diagnosis of fetal alcohol spectrum disorders in Australia. BMC Pediatr. 2013; 13: 156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cook JL, Green CR, Lilley CM et al. Fetal alcohol spectrum disorder: A guideline for diagnosis across the lifespan. CMAJ 2016; 188: 191–7. [DOI] [PMC free article] [PubMed] [Google Scholar]


