Abstract
The current study aimed to investigate whether the increased expression of long chain acyl-coenzymeA synthetase 1 (ACSL1) in peripheral blood leukocytes (PBL) may be a molecular marker for the genetic evaluation of acute myocardial infarction (AMI). The mechanism of action of ACSL1 in the pathogenesis of AMI was also investigated. A total of 75 patients with AMI and 70 individuals without coronary heart disease were selected to participate in the present study. The demographic and clinical information of the enrolled subjects was recorded. Reverse transcription quantitative polymerase chain reaction and western blot analysis were applied to measure the expression of ACSL1 at the mRNA and protein levels. It was demonstrated that the expression of ACSL1 mRNA and protein in PBL was increased in patients with AMI compared with controls. Logistic regression analysis indicated that ACSL1 expression in PBL was an independent risk factor of AMI. There was a significant positive association between the level of ACSL1 expression and the degree of atherosclerosis in the coronary artery. Furthermore, patients with AMI exhibited an increased risk of atherosclerosis due to increased fasting blood glucose, total cholesterol, triglyceride and lipoprotein levels and decreased high-density lipoprotein levels, compared with controls. Therefore, the current study demonstrated that ACSL1 expression was increased in the PBLs of patients with AMI. The elevated expression of ACSL1 acts an independent risk factor of AMI and may act as a potential biomarker when determining the risk of AMI.
Keywords: long-chain acyl-coenzyme A synthetase 1, acute myocardial infarction, gene expression, Han people of Northern China
Introduction
Acute myocardial infarction (AMI) refers to myocardial necrosis resulting from acute, persistent ischemia and hypoxia due to coronary atherosclerosis and poses a serious threat to patients. The incidence of AMI is rising due to the rapidly increasing population (1,2). Therefore, it is essential to reduce the morbidity and mortality rates of AMI and improve the prognosis of patients.
AMI is caused by the interaction of multiple factors, including immunity, the environment and genetics (3). The risk factors of AMI include age, sex, smoking, dyslipidemia, hypertension, diabetes, abdominal obesity and chronic inflammation (4). Furthermore, the incidence of AMI exhibits clear familial aggregation and a large number of associated genes serve important roles in its onset and development (5). Gene-chip technology facilitates the identification of differentially expressed genes in patients with AMI and may potentially be used as an auxiliary means during the evaluation and diagnosis of patients with AMI (6). Abnormally expressed genes may contribute to early identification of high-risk groups and may potentially be used as an early warning marker or therapeutic target of AMI.
Fatty acids are an important source of energy for mammals. They are broken down into carbon dioxide and water under aerobic conditions, during which a large amount of energy is released in the form of adenosine triphosphate (ATP) (7). The long-chain acyl-coenzymeA synthetase (ACSL) family is a key enzyme family for the biosynthesis and catabolism of fatty acids (8). ACSL1 serves a role in multiple anabolic and catabolic lipid pathways, including those making cholesterol esters, triglycerides and phosphate esters (9). Disruptions in these pathways can cause various metabolic diseases, including hepatic steatosis, hyperlipoidemia and insulin resistance (10). ACSL1 is the major subtype of ACSL in the liver; however the association between the expression of ACSL1 in peripheral blood leukocytes (PBL) and AMI remains unclear. The results of our previous study investigating the differential gene expression profile of AMI indicated that the expression of certain genes in PBL differs significantly between patients with AMI and healthy controls (11). Among differentially expressed genes, the expression of ACSL1 is significantly increased in AMI (LogFC=2.590, P=0.04) (11). Based on this pattern of expression, the present study hypothesized that the ACSL1 gene is involved in the pathogenesis of AMI and an investigation was conducted into the potential of using ACSL1 expression in PBL as a biomarker for assessing AMI risk.
Patients and methods
Patients
The patient group (AMI group) consisted of 75 inpatients (45 male and 30 female; mean age, 58.96 years) from the Han population of Northern China. Patients were admitted into the Department of Cardiology of The China-Japan Union Hospital of Jilin University (Jilin, China) between November 2014 and March 2016. Diagnosis of AMI was confirmed according to the Universal Definition of Myocardial Infarction (12) and coronary angiography was performed to confirm that narrowing of >70% was exhibited in ≥1 of the main branches (left main, left anterior descending, circumflex and right) of the coronary arteries. Non-coronary atherosclerotic heart disease was confirmed when narrowing of <50% was exhibited in the main branches of the coronary arteries (left main, left anterior descending, circumflex and right coronary arteries) using coronary angiography. This was present in 70 cases (39 male and 31 female; mean age, 58.13 years), which were subsequently selected as controls (Control group). They were admitted into the Department of Cardiology of The China-Japan Union Hospital of Jilin University between November 2014 and March 2016. The exclusion criteria of patients in the current study were as follows: i) AMI induced by percutaneous coronary intervention or coronary artery bypass grafting; ii) an imbalance between supply and demand secondary to the myocardial injury, including coronary endothelial dysfunction with no significant coronary artery disease, coronary artery spasm, coronary embolism, fast/slow arrhythmia, severe anemia, severe respiratory failure, aortic dissection or severe aortic valve disease and hypertrophic cardiomyopathy; iii) non-ischemic myocardial injury, including cardiac contusion, surgery, ablation, pacemaking or defibrillation, rhabdomyolysis with cardiac involvement, myocarditis and taking cardiotoxic drugs; iv) myocardial injury induced by multifactor or uncertain factors including severe heart failure, stress cardiomyopathy, severe pulmonary hypertension or pulmonary embolism, sepsis and critically ill patients, renal failure, severe acute neurological diseases, including stroke, subarachnoid hemorrhage, invasive diseases, including amyloidosis, sarcoidosis and intense exercise; v) patients exhibiting severe infectious diseases or malignant tumors; vi) patients suffering from chronic infectious diseases or with a history of recurrent infectious disease; vii) active or latent Tuberculosis infection history; viii) patients with immune system diseases and/or taking hormones and suspected or confirmed immunodeficiency; ix) patients with incomplete angiographic or clinical data. The exclusion criteria (v-ix) were also applicable to the control group.
Ethical approval
The current study was approved by the Ethics Committee of the China-Japan Union Hospital of Jilin University (Jilin, China). Written informed consent was obtained from all subjects prior to enrollment in the study. Detailed clinical data were recorded, including medication history, blood lipids, fasting blood glucose, markers of myocardial damage, blood pressure while seated, body mass index (BMI), coronary angiography information, family history of premature coronary heart disease, smoking history and history of other clinical diseases.
Blood collection
A total of 4 ml peripheral blood was drawn into EDTA anticoagulant-coated tubes from all fasting subjects in the morning and stored at 4°C. All blood samples were used within 2 h of collection. Each peripheral blood sample was equally divided for total RNA or protein extraction from peripheral blood mononuclear cells.
Total RNA extraction and cDNA synthesis
Peripheral blood mononuclear cells were isolated from fresh blood samples by Ficoll density gradient centrifugation (Lymphocyte Separation Medium; Hao Yang Biological Technology Co., Ltd., Tianjin, China) according to the manufacturer's protocol. Total RNA from peripheral blood mononuclear cells was extracted using the RNA simple Total RNA kit (Beijing Bio-tech Co Ltd, Beijing, China) following the manufacturer's instructions. RNA purity and concentration were measured using a NanoDrop spectrophotometer (NanoDrop 2000; Thermo Fisher Scientific Inc., Wilmington, DE, USA) with a sample volume of 1 µl. RNA purity was assessed according to A260/A280 and A260/A230 absorbance ratios. RNA samples are required to have an absorbance reading of 1.9–2.1 for the A260/A280 ratio and >2 for the A260/A230 ratio. RNA integrity was verified based on the 28S and 18S ribosomal RNA bands following electrophoresis on a 1.5% agarose gel, staining with ethidium bromide (20–30 min at room temperature) and visualization with UV light. A total of 1 µg qualified total RNA was used for cDNA synthesis with a ReverTra Ace® RT-qPCR kit (Toyobo Co., Ltd., Osaka, Japan) following the manufacturer's protocol. cDNA samples were stored at −20°C prior to qPCR.
Total protein extraction
Peripheral blood mononuclear cells were lysed with radioimmunoprecipitation assay lysis buffer (Beyotime Institute of Biotechnology, Haimen, China) and total protein was collected from the supernatant following centrifugation at 13,400 × g for 20 min at 4°C. Protein concentration was measured using the bicinchoninic acid method using a spectrophotometer (Nanodrop 2000; Thermo Fisher Scientific, Inc.). Protein samples were stored at −80°C prior to western blot analysis.
qPCR detection
A cDNA sample (1 µg; ×10 dilution) was used for qPCR with SYBR® Premix Ex Taq™ (Takara Biotechnology Co., Ltd., Dalian, China). qPCR amplification was conducted in a 20 µl reaction mixture containing 10 µl SYBR® Premix Ex Taq™, 0.5 µl upstream and downstream primers with a concentration 10 µmol/l and 8 µl nuclease-free double-distilled water in the Mx3005P RT-qPCR System (Stratagene; Agilent Technologies Inc., Santa Clara, CA, USA). The thermocycling conditions were as follows: 95°C for 10 min; 40 cycles of 95°C for 15 sec, 60°C for 20 sec, 72°C for 20 sec and 95°C for 1 min, 55°C for 30 sec and 95°C for 30 sec. Following the reaction, 10 µl assay mixture was used for 1.5% agarose gel electrophoresis using Tris, acetic acid and EDTA buffer (1x), following a standard procedure. GAPDH was used as the reference gene and each sample was run at least in triplicate. The results were quantified using the 2−∆∆Cq method (13). All PCR primers were designed with Primer Premier 6.0 (VoyaGene Biotech Co., Ltd., Hangzhou, China) according to the mRNA sequence from the National Centre for Biotechnology Information (https://www.ncbi.nlm.nih.gov/; ACSL1, NM_001995; GAPDH, NM_001256799) and synthesized by Shanghai Biological Technology Ltd. (Shanghai, China) and the sequences are presented in Table I.
Table I.
Primer sequences.
| Gene names | Primer sequences (5′-3′) |
|---|---|
| ACSL1 | |
| F | CCATGAGCTGTTCCGGTATTT |
| R | CCGAAGCCCATAAGCGTGTT |
| GAPDH | |
| F | GGAGCGAGATCCCTCCAAAAT |
| R | GGCTGTTGTCATACTTCTCATGG |
ACSL1, acyl-coenzymeA synthetase 1; F, forward; R, reverse.
Western blot analysis
Total protein (30 µg per lane) underwent 10% SDS-PAGE and was transferred onto a polyvinylidene fluoride membrane with a semi-dry transfer device (Bio-Rad Laboratories, Inc., Hercules, CA, USA) for 10 min. The membrane was blocked with blocking buffer (TBS with 0.1% Tween-20 and 5% skim milk powder) at room temperature for 1 h. The blocked membrane was incubated with a primary antibodies in TBST at 4°C overnight (ACSL1 monoclonal antibodies, 1:1,000, cat. no. ab177958; β-actin polyclonal antibody antibodies, 1:1,000, cat. no. ab8227; Abcam, Cambridge, MA, USA) Following washing, the membrane was incubated with secondary antibodies (Hydroxypyruvate reductase conjugated sheep anti-rabbit immunoglobulin G; 1:3,000; cat. no. ab 97051; Abcam) at 4°C for 1 h. The membrane was developed using an enhanced chemiluminescence kit (Thermo Fisher Scientific, Inc.). To analyze the relative expression level of each protein, densitometric analysis was performed using Image Lab 4.1 software (Bio-Rad Laboratories, Inc.).
Statistical analysis
All data were statistically analyzed with SPSS 22.0 software (IBM Corp., Armonk, NY, USA) and expressed as mean ± standard error. When comparing differences between groups, data with a normal distribution were analyzed using an independent T test and non-normal distribution data were analyzed using a Wilcoxon signed rank test. Count data were expressed as frequency for statistical description and differences between groups were analyzed with a χ2 test; AMI-associated risk factors were analyzed using binary logistic regression analysis. Blood vessel lesions between groups were compared with the Mann-Whitney U test. The correlation between the relative expression of ACSL1 and cardiac troponin I (cTnI) was measured using bivariate correlation analysis. Data of relative ACSL1 expression were used to construct a receiver operating characteristic (ROC) curve and the area under the curve and standard error were calculated to deduce the threshold value. P<0.05 was considered to indicate a statistically significant difference.
Results
Analysis of clinical data
There were no significant differences between the AMI and control groups in age, sex, BMI, family history of coronary heart disease, smoking history, incidence of hypertension and diabetes (Table II). However, there were significant differences between serum lipid and glucose levels in the AMI and control groups. The fasting glucose, total plasma cholesterol, plasma triglycerides and plasma low-density lipoprotein (LDL) levels in the AMI group were significantly increased compared with the control group (all P<0.01; Table III), whereas plasma high-density lipoprotein (HDL) levels were significantly decreased compared with the control group (P<0.05; Table III).
Table II.
Clinical data comparison between the AMI and control groups.
| Data | AMI group (n=75) | Control group (n=70) | t/χ2 | P-values |
|---|---|---|---|---|
| Age (year) | 58.96±9.05 | 58.13±6.68 | −0.63 | 0.53 |
| Sex | 0.27 | 0.60 | ||
| Male | 45 (60.00) | 39 (55.71) | ||
| Female | 30 (40.00) | 31 (44.29) | ||
| BMI (kg/m2) | 25.10±3.44 | 25.56±3.90 | 0.76 | 0.45 |
| Hypertension | 37 (49.33) | 26 (37.14) | 2.19 | 0.14 |
| Diabetes | 15 (20.00) | 10 (14.29) | 0.83 | 0.36 |
| Family history | 6 (8.00) | 5 (7.14) | 0.04 | 0.85 |
| Smoking history | 38 (50.67) | 26 (37.14) | 2.69 | 0.10 |
Data are presented as the mean ± standard deviation or as n (%). AMI, acute myocardial infarction; BMI, body mass index.
Table III.
Comparison of the levels of blood glucose and blood lipid between the AMI and control groups.
| Index (mmol/l) | AMI group (n=75) | Control group (n=70) | t | P-values |
|---|---|---|---|---|
| Fasting blood-glucose | 6.73±2.10 | 5.76±1.53 | −3.08 | 0.003a |
| Total cholesterol | 4.96±1.24 | 4.43±1.02 | −2.79 | 0.01a |
| Triglycerides | 2.48±1.34 | 1.77±0.98 | −3.61 | <0.001a |
| LDL | 3.34±1.03 | 2.86±0.81 | −3.11 | 0.002a |
| HDL | 0.98±0.29 | 1.07±0.27 | 2.06 | 0.04a |
P<0.05. Data are presented as mean ± standard deviation. AMI, acute myocardial infarction; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
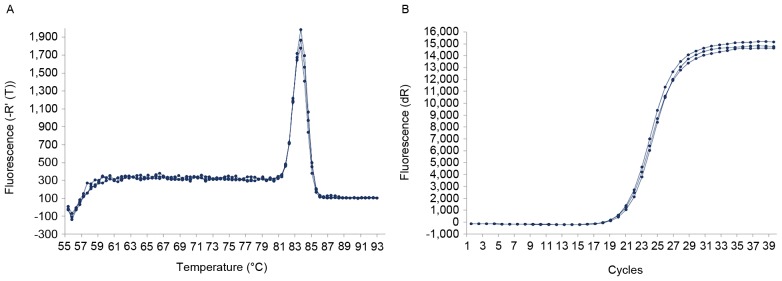
RT-qPCR
The dissolution curve of the ACSL1 gene exhibited a single dissolution peak with high PCR specificity (Fig. 1A) and the amplification curve was clearly sigmoid (Fig. 1B). PCR products were checked for the presence of the objective band on the 1.5% agarose gel. The PCR products were used to measure ACSL1 expression and exhibited the target band with the expected size of ~93-bp (Fig. 2). The ΔΔCq value of RT-qPCR from each sample was the mean ± standard deviation of three repeats within the required range. There was a significant difference in the 2−ΔΔCq value of the ACSL1 gene between the AMI 0.18±0.08 and control groups (0.06±0.04; t=−11.48, P<0.01). The relative expression of ACSL1 gene was calculated by 2−∆∆Cq method. The results showed that the relative expression of ACSL1 gene was 2.84±1.18 times of the control group (Fig. 3). These results demonstrate that the level of ACSL1 mRNA in the PBL of patients with AMI is significantly increased.
Figure 1.
Acyl-coenzymeA synthetase 1 (A) dissolution curve and (B) amplification curve.
Figure 2.
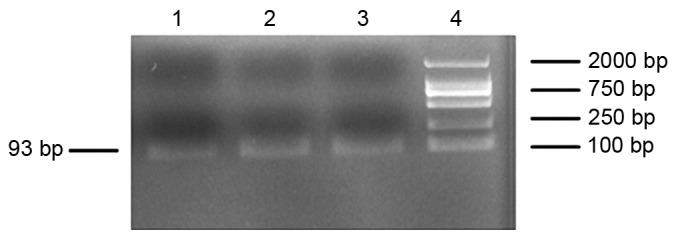
Agarose gel electrophoresis of the RT-qPCR products. Lanes 1, 2 and 3, RT-qPCR products; lane 4, DL2000 DNA ladder marker. RT-qPCR, reverse transcription quantitative polymerase chain reaction; bps, base pairs.
Figure 3.
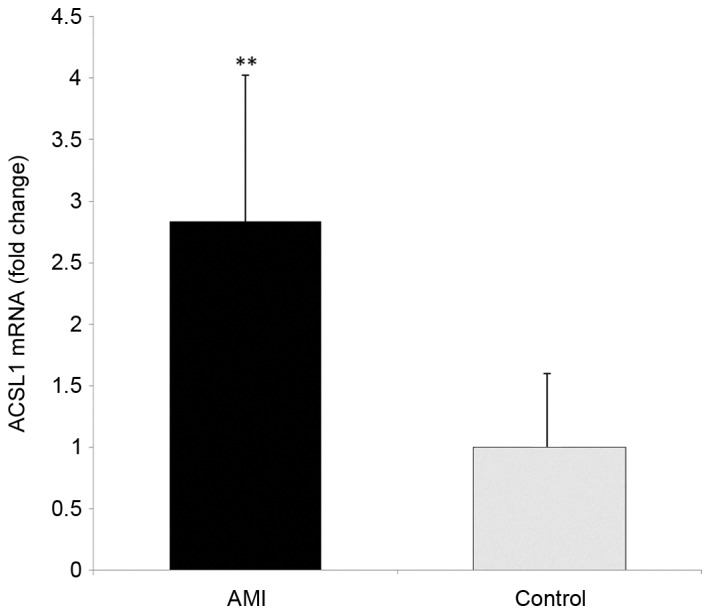
Levels of ACSL1 mRNA. **P<0.01 vs. Control. AMI, acute myocardial infarction group; ACSL1, acyl-coenzymeA synthetase 1.
Western blot analysis
The expression of ACSL1 protein in the AMI group was significantly increased compared with the control group (P<0.01; Fig. 4).
Figure 4.
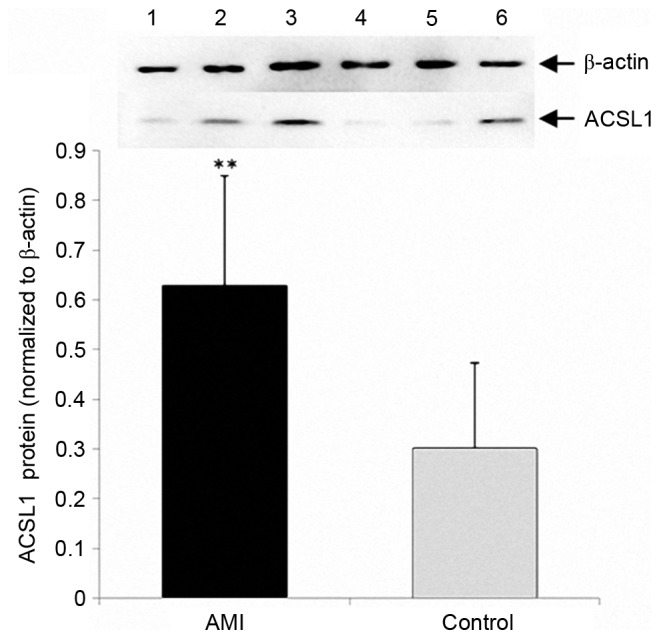
Results of western blot analysis. **P<0.01. AMI, acute myocardial infarction group (samples numbered 1, 2 and 3); Control, control group (sample numbered 4, 5 and 6); ACSL1, acyl-coenzymeA synthetase 1.
Logistic regression analysis assessing the association between expression of ACSL1 and AMI
To further analyze whether increased expression of ACSL1 was a risk factor of AMI, the 145 subjects were divided into a low expression group (2−ΔΔCq ≤0.11) and a high expression group (2−Δ∆Cq>0.11), according to the median relative level of ACSL1 expression (Table IV). The associations between AMI and the relative expression of ACSL1, age, sex, BMI, smoking history, family history of premature coronary heart disease, hypertension, diabetes, blood sugar and blood cholesterol were analyzed using stepwise logistic regression analysis. The results demonstrated that increased gene expression of ACSL1 (P<0.01) and increased total blood cholesterol levels (P=0.01) were independent risk factors for AMI (Table V).
Table IV.
Clinical data comparison between the low expression and high expression groups.
| Data | Low expression (n=73) | High expression (n=72) | t/χ2 | P-value |
|---|---|---|---|---|
| Age (year) | 57.62±6.87 | 59.51±8.90 | −1.43 | 0.15 |
| Sex | 0.19 | 0.66 | ||
| Male | 41 (56.16) | 43 (59.72) | ||
| Female | 32 (43.84) | 29 (40.28) | ||
| BMI (kg/m2) | 25.88±3.91 | 24.76±3.33 | 1.86 | 0.06 |
| Hypertension | 28 (38.36) | 35 (48.61) | 1.55 | 0.21 |
| Diabetes | 12 (16.44) | 13 (18.066) | 0.07 | 0.79 |
| Family history | 8 (10. 96) | 3 (4.17) | 2.38 | 0.12 |
| Smoking history | 29 (39.73) | 35 (48.61) | 1.16 | 0.28 |
| FBG (mmol/l) | 5.82±1.54 | 6.79±1.98 | −3.22 | 0.002a |
| TC (mmol/l) | 4.59±1.17 | 4.82±1.15 | −1.22 | 0.22 |
| TG (mmol/l) | 1.80±0.94 | 2.48±1.39 | −3.44 | 0.001a |
| LDL (mmol/l) | 2.95±0.97 | 3.27±0.91 | −1.98 | 0.04a |
| HDL (mmol/l) | 1.08±0.27 | 0.97±0.28 | 2.23 | 0.03a |
P<0.05. Data are presented as the mean ± standard deviation or as n (%). BMI, body mass index; FBG, fasting blood-glucose; TC, total cholesterol; TG, triglycerides; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
Table V.
Logistic regression analysis indicating independent risk factors of AMI.
| Variables | Regression coefficient | Standard error | Wald | P-values | OR | 95% CI |
|---|---|---|---|---|---|---|
| Relative expression level of ACSL1 | 4.07 | 0.56 | 52.35 | <0.001a | 58.66 | 19.47–176.74 |
| Total cholesterol | 0.61 | 0.23 | 7.20 | 0.01a | 1.84 | 1.18–2.88 |
P<0.05. AMI, acute myocardial infarction; CI, confidence interval; OR, odd ratio; ACSL1, acyl-coenzyme A synthetase 1.
The association between the expression of ACSL1 in patients with AMI and the severity of coronary artery lesions
The 75 patients with AMI were divided into a ACSL1 low expression level group (2−∆∆Cq≤0.17) and a ACSL1 high expression level group (2−∆∆Cq>0.17) according to the median relative expression levels in the AMI group. The numbers of blood vessel lesions were counted in the two groups. Lesions were identified where angiography confirmed coronary artery stenosis of >70%. The severity of lesions between the AMI and control groups was compared using the Mann-Whitney U test and the results demonstrated that high expression of ACSL1 was significantly associated with the numbers of lesions in the main branches of the coronary artery (P=0.03; Table VI), suggesting that the expression of ACSL1 may reflect the severity of coronary arteriosclerosis.
Table VI.
Comparison of the number of vessel lesions between patients with different levels of ACSL1 expression.
| Group | Single vessel lesion | Double vessel lesion | Three vessel lesion | Z value | P-value |
|---|---|---|---|---|---|
| Low ACSL1 expression level (n=38) | 16 (42.11) | 12 (31.58) | 10 (26.31) | −2.16 | 0.03a |
| High ACSL1 expression level (n=37) | 6 (16.22) | 16 (43.24) | 15 (40.54) |
P<0.05. Data are presented as n (%). ACSL1, acyl-coenzyme A synthetase 1.
Bivariate correlation analysis on serum cTnI and relative expression of ACSL1 in patients with AMI
The median cTnI concentration of the AMI group was 0.56 (0.11–7.52) ng/ml (data not shown). Bivariate correlation analysis on cTnI and the relative gene expression of in AMI patients gave an Spearman's rank correlation coefficient (rs) of value 0.20 (P=0.16), indicating that there was no correlation between ACSL1 expression and the concentration of serum cTnI. Although the increased gene expression of ACSL1 increases the morbidity of AMI, the expression of ACSL1 is not associated with the size of the myocardial injury.
ROC curves and cut off value of the relative expression of ACSL1 in patients with AMI
Levels of ACSL1 expression exhibited diagnostic accuracy for AMI and the area under the curve was 0.93±0.02 with a cutoff value of 0.112 as determined by the maximum value of Youden's index (14) (P<0.01; Fig. 5)/This indicates that high expression of ACSL1 results in a high likelihood of AMI. The sensitivity and specificity were 84 and 90%, respectively. The positive and negative prediction rates were 90 and 84%, respectively.
Figure 5.
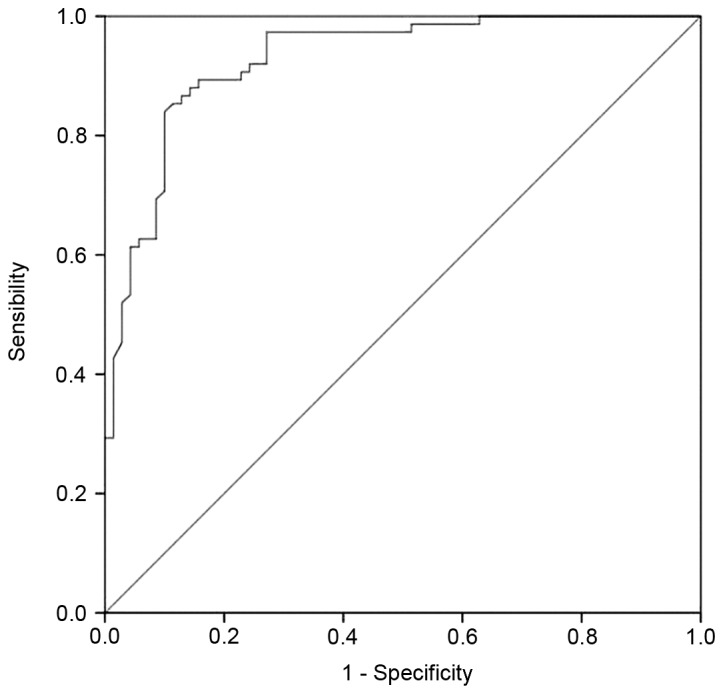
Receiver operating characteristic curve of the relative level of expression of acyl-coenzymeA synthetase.
Discussion
Coronary atherosclerotic heart disease is the most common cardiovascular disease and is caused by the interaction between genetic and environmental factors (15–17). AMI refers to myocardial necrosis induced by acute, persistent ischemia and hypoxia, which can result in further life-threatening complications, including arrhythmia, cardiogenic shock and acute heart failure. A previous study has demonstrated that changes in the expression of various genes (including ALOX5, MGST1, CREB5, IL1RN, CSF2R, VCAN are CSF3R) are correlated with susceptibility of patients to coronary heart disease (18,19). Furthermore, a previous study on the differential gene expression profile of AMI determined that the expression of ACSL1 in the peripheral blood of patients with AMI is significantly increased (11). The present study expanded the sample size and confirmed that the expression of ACSL1 mRNA and protein was significantly increased in the PBL of patients with AMI from Northern China.
Fatty acids are an important source of energy for mammals. Fatty acids and their products exert many different functions in metabolism and signal transduction. Long-chain acyl-coenzyme A synthetase catalyzes the first step of the reaction in fatty acid metabolism and is one of the key enzymes in fat synthesis and catabolism (20). ACSL1, a major subtype of ACSL, catalyzes the synthesis of bioactive acyl-coenzyme A esters using long-chain fatty acids, ATP and coenzyme A as substrates (21). Acyl-coenzyme A ester is an important fuel for fatty acid catabolism and participates in the synthesis of phospholipids, cholesterol esters, ceramide, triglycerides and other complex lipids (22). Increased levels of ACSL1 are expressed in the liver, cardiac muscle, fat and endothelial cells and monocytes-macrophages (23). It has been demonstrated that the expression of ACSL1 is correlated with increased lipid loading and insulin sensitivity and that decreased gene expression of ACSL1 can reduce the lipid loading and glucose uptake in cells (24). In mice with high-fat diets, the expression of ACSL1 is consistent with the severity of obesity, suggesting that ACSL1 is involved in the regulation of insulin sensitivity and lipids in cells (25).
ACSL1 is actively involved in the synthesis and oxidation of fat in liver cells (26). Disorders in metabolic pathways can trigger a variety of metabolic diseases. However, to the best of our knowledge, the association between ACSL1 expression and AMI remains unclear. In the present study, logistic regression analysis demonstrated that ACSL1 expression in PBL was an independent risk factor for AMI. Furthermore, ACSL1 expression is correlated with the number of lesions on the main branches of the coronary artery. Therefore, the increased expression of ACSL1 suggests more severe atherosclerosis.
Cardiac troponin is currently recognized as an indicator with high specificity and sensitivity for necrotic myocardial cell injury (27). cTnI released from myocardial cells during AMI is positively correlated with the scope of myocardial cell damage (28). The present study indicated that ACSL1 expression was not significantly correlated with serum cTnI levels in patients with AMI, suggesting that the expression of ACSL1 promotes the onset of AMI, not the scope of myocardial infarction.
The ROC curves indicated that the relative expression of ACSL1 exhibited high sensitivity, specificity and positive and negative prediction values in the diagnosis of AMI. Therefore, the relative expression of ACSL1 may be used as a genetic marker for assessing the risk of AMI.
Clinical data analysis identified that patients with AMI had significantly increased fasting blood glucose, total cholesterol, triglyceride and LDL, which are risk factors of atherosclerosis but exhibited decreased levels of HDL compared with the control group. ACSL1 is broadly involved in the synthesis and oxidation of fatty acids; therefore it is possible that increased ACSL1 expression influences blood glucose and lipid levels, leading to atherosclerosis of the arteries, thus stimulating the development of AMI.
Apart from glucose and lipid metabolism disorders, chronic inflammation serves an important role in atherosclerosis and AMI. Previous studies have indicated that ACSL1 expression may affect the expression of inflammatory chemokines and it has been demonstrated that levels of ACSL1 expression are significantly increased in monocyte-macrophages in a type I diabetic mouse model and in humans with type I diabetes (29–31). Furthermore, specific inhibition of ACSL1 expression in type I diabetic mice selectively reduces the inflammatory response of the cells and the effects of diabetic atherosclerosis (32). This suggests that the expression of ACSL1 is closely associated with chronic inflammation in patients with diabetes, which contributes to the initiation and progression of atherosclerosis. However, further studies are required to determine whether ACSL1 expression promotes the pro-inflammatory response in individuals with normal blood sugar levels. The current study was limited as the inflammatory markers were not measured and recorded.
In conclusion, the current study demonstrated that ACSL1 expression was significantly increased in the peripheral blood mononuclear cells of patients with AMI and it was determined that increased expression of ACSL1 is an independent risk factor for AMI. ACSL1 expression was positively correlated with the severity of atherosclerosis. However, the expression of ACSL1 was not correlated with the scope of AMI. ACSL1 may promote the onset of AMI by affecting the metabolism of fat and glucose. Thus, the increased expression of ACSL1 in peripheral blood mononuclear cells may potentially be used as a molecular marker for the early diagnosis of AMI.
Acknowledgements
The authors would like to thank Professor Zhihui Zhao and his team in Jilin University School of Animal Husbandry and Veterinary Medicine (Jilin, China) for their excellent technical guidance in the current study.
References
- 1.Lopez AD, Mathers CD. Measuring the global burden of disease and epidemiological transitions: 2002–2030. Ann Trop Med Parasitol. 2006;100:481–499. doi: 10.1179/136485906X97417. [DOI] [PubMed] [Google Scholar]
- 2.Moran AE, Forouzanfar MH, Roth GA, Mensah GA, Ezzati M, Flaxman A, Murray CJ, Naghavi M. The global burden of ischemic heart disease in 1990 and 2010: The global burden of disease 2010 study. Circulation. 2014;129:1493–1501. doi: 10.1161/CIRCULATIONAHA.113.004046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moreira DM, da Silva RL, Vieira JL, Fattah T, Lueneberg ME, Gottschall CA. Role of vascular inflammation in coronary artery disease: Potential of anti-inflammatory drugs in the prevention of atherothrombosis. Inflammation and anti-inflammatory drugs in coronary artery disease. Am J Cardiovasc Drugs. 2015;15:1–111. doi: 10.1007/s40256-014-0094-z. [DOI] [PubMed] [Google Scholar]
- 4.White HD, Chew DP. Acute myocardial infarction. Lancet. 2008;372:570–584. doi: 10.1016/S0140-6736(08)61237-4. [DOI] [PubMed] [Google Scholar]
- 5.Zdravkovic S, Wienke A, Pedersen NL, de Faire U. Genetic susceptibility of myocardial infarction. Twin Res Hum Genet. 2007;10:848–852. doi: 10.1375/twin.10.6.848. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Y, Lin P, Jiang H, Xu J, Luo S, Mo J, Li Y, Chen X. Extensive serum biomarker analysis in patients with ST segment elevation myocardial infarction (STEMI) Cytokine. 2015;76:356–362. doi: 10.1016/j.cyto.2015.06.015. [DOI] [PubMed] [Google Scholar]
- 7.Yan S, Yang XF, Liu HL, Fu N, Ouyang Y, Qing K. Long-chain acyl-CoA synthetase in fatty acid metabolism involved in liver and other diseases: An update. World J Gastroenterol. 2015;21:3492–3498. doi: 10.3748/wjg.v21.i12.3492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Coleman RA, Lewin TM, Muoio DM. Physiological and nutritional regulation of enzymes of triacylglycerol synthesis. Annu Rev Nutr. 2000;20:77–103. doi: 10.1146/annurev.nutr.20.1.77. [DOI] [PubMed] [Google Scholar]
- 9.Soupene E, Kuypers FA. Mammalian long-chain acyl-CoA synthetases. Exp Biol Med (Maywood) 2008;233:507–521. doi: 10.3181/0710-MR-287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li LO, Mashek DG, An J, Doughman SD, Newgard CB, Coleman RA. Overexpression of rat long chain acyl-coa synthetase 1 alters fatty acid metabolism in rat primary hepatocytes. J Biol Chem. 2006;281:37246–37255. doi: 10.1074/jbc.M604427200. [DOI] [PubMed] [Google Scholar]
- 11.Xudong Guo, Lin Fan, Xiangdong Li, Fanbo Meng. Microarray analysis of differential gene expression profile in the peripheral blood cells of the patients with myocardial infarction. ResearchGate. DOI: 10.1016/j.jacc.2015.06.596. [Google Scholar]
- 12.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD. Writing Group on the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction. Thygesen K, Alpert JS, White HD, et al., editors. Third universal definition of myocardial infarction. 2012;33:2551–2567. Eur Heart J. [Google Scholar]
- 13.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 14.Hughes G. Youden's index and the weight of evidence. Methods Inf Med. 2015;54:198–199. doi: 10.3414/ME14-04-0003. [DOI] [PubMed] [Google Scholar]
- 15.Zeller T, Blankenberg S, Diemert P. Genomewide association studies in cardiovascular disease-an update 2011. Clin Chem. 2012;58:92–103. doi: 10.1373/clinchem.2011.170431. [DOI] [PubMed] [Google Scholar]
- 16.Kullo IJ, Ding K. Mechanisms of disease: The genetic basis of coronary heart disease. Nat Clin Pract Cardiovasc Med. 2007;4:558–569. doi: 10.1038/ncpcardio0982. [DOI] [PubMed] [Google Scholar]
- 17.Joehanes R, Ying S, Huan T, Johnson AD, Raghavachari N, Wang R, Liu P, Woodhouse KA, Sen SK, Tanriverdi K, et al. et al. Gene expression signatures of coronary heart disease. Arterioscler Thromb Vasc Biol. 2013;33:1418–1426. doi: 10.1161/ATVBAHA.112.301169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friede KA, Ginsburg GS, Voora D. Gene expression signatures and the spectrum of coronary artery disease. J Cardiovasc Transl Res. 2015;8:339–352. doi: 10.1007/s12265-015-9640-6. [DOI] [PubMed] [Google Scholar]
- 19.Ogawa N, Imai Y, Morita H, Nagai R. Genome-wide association study of coronary artery disease. Int J Hypertens. 2010;21:790539. doi: 10.4061/2010/790539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang YL, Guo W, Zang Y, Yaney GC, Vallega G, Getty-Kaushik L, Pilch P, Kandror K, Corkey BE. Acyl coenzyme a synthetase regulation: Putative role in long-chain acyl coenzyme a partitioning. Obes Res. 2004;12:1781–1788. doi: 10.1038/oby.2004.221. [DOI] [PubMed] [Google Scholar]
- 21.Parkes HA, Preston E, Wilks D, Ballesteros M, Carpenter L, Wood L, Kraegen EW, Furler SM, Cooney GJ. Overexpression of acyl-CoA synthetase-1 increases lipid deposition in hepatic (HepG2) cells and rodent liver in vivo. Am J Physiol Endocrinol Metab. 2006;291:E737–E744. doi: 10.1152/ajpendo.00112.2006. [DOI] [PubMed] [Google Scholar]
- 22.Li LO, Klett EL, Coleman RA. Acyl-CoA synthesis, lipid metabolism and lipotoxicity. Biochim Biophys Acta. 2010;1801:246–251. doi: 10.1016/j.bbalip.2009.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanter JE, Tang C, Oram JF, Bornfeldt KE. Acyl-CoA synthetase 1 is required for oleate and linoleate mediated inhibition of cholesterol efflux through ATP-binding cassette transporter A1 in macrophages. Biochim Biophys Acta. 2012;1821:358–364. doi: 10.1016/j.bbalip.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ellis JM, Li LO, Wu PC, Koves TR, Ilkayeva O, Stevens RD, Watkins SM, Muoio DM, Coleman RA. Adipose acyl-CoA synthetase-1 directs fatty acids toward beta-oxidation and is required for cold thermogenesis. Cell Metab. 2010;12:53–64. doi: 10.1016/j.cmet.2010.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Joseph R, Poschmann J, Sukarieh R, Too PG, Julien SG, Xu F, Teh AL, Holbrook JD, Ng KL, Chong YS, et al. ACSL1 is associated with fetal programming of insulin sensitivity and cellular lipid content. Mol Endocrinol. 2015;29:909–920. doi: 10.1210/me.2015-1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhan T, Poppelreuther M, Ehehalt R, Füllekrug J. Overexpressed FATP1, ACSVL4/FATP4 and ACSL1 increase the cellular fatty acid uptake of 3T3-L1 adipocytes but are localized on intracellular membranes. PLoS One. 2012;7:e45087. doi: 10.1371/journal.pone.0045087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zimmerman J, Fromm R, Meyer D, Boudreaux A, Wun CC, Smalling R, Davis B, Habib G, Roberts R. Diagnostic marker cooperative study for the diagnosis of myocardial infarction. Circulation. 1999;99:1671–1677. doi: 10.1161/01.CIR.99.13.1671. [DOI] [PubMed] [Google Scholar]
- 28.Boden H, Ahmed TA, Velders MA, van der Hoeven BL, Hoogslag GE, Bootsma M, le Cessie S, Cobbaert CM, Delgado V, van der Laarse A, Schalij MJ. Peak and fixed-time high-sensitive troponin for prediction of infarct size, impaired left ventricular function and adverse outcomes in patients with first ST-segment elevation myocardial infarction receiving percutaneous coronary intervention. Am J Cardiol. 2013;111:1387–1393. doi: 10.1016/j.amjcard.2013.01.284. [DOI] [PubMed] [Google Scholar]
- 29.Kanter JE, Kramer F, Barnhart S, Averill MM, Vivekanandan-Giri A, Vickery T, Li LO, Becker L, Yuan W, Chait A, et al. et al. Diabetes promotes an inflammatory macrophage phenotype and atherosclerosis through acyl-CoA synthetase 1. Proc Natl Acad Sci USA. 2012;109:E715–E724. doi: 10.1073/pnas.1111600109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Renard CB, Kramer F, Johansson F, Lamharzi N, Tannock LR, von Herrath MG, Chait A, Bornfeldt KE. Diabetes and diabetes-associated lipid abnormalities have distinct effects on initiation and progression of atherosclerotic lesions. J Clin Invest. 2004;114:659–668. doi: 10.1172/JCI200417867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol. 2011;31:986–1000E7. doi: 10.1161/ATVBAHA.110.207449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kanter JE, Bornfeldt KE. Inflammation and diabetes-accelerated atherosclerosis: Myeloid cell mediators. Trends Endocrinol Metab. 2013;24:137–144. doi: 10.1016/j.tem.2012.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]