Abstract
Introduction
Rift Valley fever (RVF) is a mosquito-borne zoonotic viral disease endemic to Africa and the Arabian Peninsula. High rates of abortion among infected ruminants and hemorrhagic fever in infected humans are major public health concerns. Commercially available veterinary RVF vaccines are important for preventing the spread of the Rift Valley fever virus (RVFV) in endemic countries; however, RVFV outbreaks continue to occur frequently in endemic countries in the 21st century. In the U.S., the live-attenuated MP-12 vaccine has been developed for both animal and human vaccination. This vaccine strain is well attenuated, and a single dose induces neutralizing antibodies in both ruminants and humans.
Areas covered
This review describes scientific evidences of MP-12 vaccine efficacy and safety, as well as MP-12 variants recently developed by reverse genetics, in comparison with other RVF vaccines.
Expert commentary
The containment of active RVF outbreaks and long-term protection from RVF exposure to infected mosquitoes are important goals for RVF vaccination. MP-12 vaccine will allow immediate vaccination of susceptible animals in case of an unexpected RVF outbreak in the U.S., whereas MP-12 vaccine may be also useful for the RVF control in endemic regions.
Keywords: Rift Valley fever, MP-12 vaccine, reverse genetics, efficacy, safety
1. Introduction
In 1930, an outbreak of Rift Valley fever (RVF) involving sheep, cattle, goats, and humans was reported in Kenya [1]. This disease was characterized by a high mortality rate (more than 90%) of newborn lambs and high abortion rates among pregnant ewes, cattle, and goats. Daubney and Hudson proposed that Rift Valley fever virus (RVFV) is transmitted by mosquitoes, and in the 1940s, Smithburn et al. accidentally isolated RVFV (Entebbe strain) from a pool of Aedes and Eretmapodites spp. mosquitoes, which were caught for the investigation of Yellow fever, in a forest uninhabited by humans in Uganda [2]. From the 1950s to the 1990s, RVF outbreaks occurred in various countries throughout the African continent, such as Kenya, South Africa, Zimbabwe, Namibia, Mozambique, Madagascar, Mauritania, Senegal, Egypt, and Sudan [3]. During this period, it became evident that human infection with RVFV can occasionally lead to hemorrhagic fever, encephalitis, or retinitis with partial or complete blindness, in addition to febrile illness [4,5]. In the 21st century, a RVF outbreak occurred for the first time in Saudi Arabia and Yemen on the Arabian Peninsula [6], and major RVF outbreaks continued to occur in Kenya, Tanzania, and Somalia in 2006, Namibia and South Africa from 2009 – 2011, Sudan in 2007 and 2010, Madagascar in 2008, Mauritania in 2010 and from 2012 – 2015, and both Uganda and Niger in 2016 [7]. Over the last 80 years, frequent RVFV outbreaks have affected agriculture and public health in various African countries, as well as Saudi Arabia and Yemen. In 2016, a man who was suspected to have become infected with yellow fever in Angola traveled back to China and RVFV RNA was detected via deep sequencing [8]. Because this patient had mosquito bites but did not have close contact with animals before the onset of febrile illness, sporadic RVFV infection via infected mosquitoes may also occur in countries such as Angola, where active RVF outbreaks are not apparently ongoing. The transmission of RVFV occurs via mosquito vectors or body fluid of infected animals, and a lack of mosquito bites during the viremic period or appropriate quarantine of animals might prevent the spread of disease into other countries outside the endemic area [9]. Vaccination of sheep, cattle, and goats is the most important countermeasure with which to contain RVFV spread. To protect highly susceptible pregnant ewes or newborn lambs, the RVF vaccine must rapidly induce protective immunity, and remain sufficiently safe for vulnerable animal populations. The live-attenuated Smithburn vaccine, which was made in 1940s [10], causes considerable abortion risk in pregnant animals and is therefore only used for non-pregnant ruminants in endemic countries [11,12]. On the other hand, a formalin-inactivated RVF vaccine derived from the Entebbe strain was not efficacious for protecting pregnant ewes with a single dose [13]. In the U.S., a live-attenuated MP-12 vaccine strain was developed in the 1980s and was conditionally licensed for animal vaccination. This strain is attenuated, and requires only a single dose to elicit protective immune responses in ruminants and humans. In order to develop effective countermeasures against RVF, it is important to correctly understand the need for RVF vaccines. Since informative RVF vaccine reviews have previously been described elsewhere [14–17], this review will describe the update of the safety and immunogenicity of MP-12 vaccine candidate for animal and human applications.
2. Development of the MP-12 vaccine
The MP-12 strain was developed from the pathogenic ZH548 strain, which was originally isolated from a febrile human in Egypt in 1978 via 12 serial mutageneses [18]. Monolayers of human fetal lung diploid (MRC-5) cells were infected with uncloned ZH548 strain at 0.1 multiplicity of infection (moi). After repeated washes, cells were incubated with media containing 200 μg/ml of 5-fluorouracil (5-FU) at 37.5°C. Residual viruses were again removed at 3 – 4 hours post infection (hpi), and cells were further incubated with fresh media containing 5-FU for 45 to 65 hours. A plaque assay was then performed on MRC-5 cells, and viruses were isolated from the two largest well-separated plaques. Plaque-isolates were further amplified using media without 5-FU, and harvested at 48 to 72 hpi. One of the two stocks was selected based on larger plaque phenotype and/or high titers. Following this, mutagenesis cycles were initiated in the same experimental method. As a result, a mutant of the ZH548 strain was isolated after each mutagenesis cycle: i.e., 16 mutant strains (the MP-1 to the MP-16 strains) during 16 mutagenesis cycles. The lethal doses (LD50; log10 pfu) of those strains in 4- to 6-week-old outbred mice via intraperitoneal route infection (i.p.) were 1.8 (MP-1), 2.8 (MP-3), 4.8 (MP-6), ≥ 6.7 (MP-7), ≥ 6.3 (MP-12), and ≥ 5.7 (MP-16), respectively [18]. Due to the attenuation, the MP-12 strain was selected for further production of vaccine master seed and vaccine lot in the Salk Institute Government Service Division GMP facility (MP-12 vaccine, TSI-GSD-223). The preparation of MP-12 vaccine was described in the Investigational New Drug application (IND BB-4307), and the protocol was previously summarized by Lokugamage et al. [19]. The original MP-12 strain was amplified once in certified MRC-5 cells in 40 flasks (150 cm2) at 37°C for 51 hours, which was stocked as master seed (860 ml, >6.0 log10 pfu/ml). Master seed was then amplified once in certified MRC-5 cells in 60 flasks (150 cm2) at 37°C for 50 hours, and this was stocked as production seed (1,750 ml, >6.0 log10 pfu/ml). In 1988, a vaccine lot was made from the production seed using 1,239 flasks (58,120 ml), which resulted in 9,360 vials of filtrated and lyophilized vaccine lot 7-2-88 (stored at -30°C). The MP-12 vaccine lot has been used for various vaccine safety and efficacy studies using different animal models, including mice, sheep (adult, pregnant ewes, young, and newborn lambs), cattle (adult, lactating cows, pregnant cows, newborn, and young calves), and rhesus macaques [18,20–32]. The MP-12 vaccine is an Investigational New Drug to be tested in humans, and its safety and immunogenicity have been tested in clinical trials, including healthy adults [33,34]. In 2013, the MP-12 vaccine was conditionally licensed to Zoetis Inc. for animal vaccination in the U.S. without specific descriptions in the issuance of a conditional license in terms of applied animal species, pregnancy, or age [35], and new vaccine master seed has been generated accordingly by additional amplification of TSI-GSD-223 in MRC-5 cells [27,36].
3. Efficacy and safety of the MP-12 vaccine in sheep and cattle
Morrill et al. demonstrated the efficacy and attenuation of the MP-12 vaccine in pregnant ewes, which are one of the most susceptible animal populations to RVFV infection [20]. Ewes in the second trimester of pregnancy (90 to 110 days pregnancy) were subcutaneously (s.c.) vaccinated with a 1×105 pfu dose of MP-12 vaccine and challenged with the pathogenic ZH501 strain at 63 days post vaccination (dpv). Ewes developed viremia of 0.7 to 1.4 log10 pfu at 1 dpv, and Plaque Reduction Neutralization Test 80 (PRNT80) titer of ≥ 1:320 were raised by 14 dpv. All vaccinated and challenged ewes delivered healthy lambs, and no neutralizing antibodies were detected in those lambs at birth, indicating that the MP-12 vaccine did not cross the placenta. In this vaccination study [20], newborn lambs rapidly gained neutralizing antibodies after ingesting colostrum from vaccinated ewes.
Newborn lambs are highly susceptible to RVFV infection, with mortality reaching 100%. Because RVF vaccination should include vulnerable populations, Morrill et al. also tested the safety of the MP-12 vaccine in newborn lambs [21]. Six out of 12 lambs (≤ 7 days old) vaccinated with the MP-12 vaccine (5×105 pfu, i.p.) experienced transient febrile response (≥ 40°C) at 3 to 5 dpv. Histopathological examination showed one to several foci of hepatocellular necrosis in three of the 12 lambs at 2, 3, and 4 dpv. Two- to seven-day-old lambs were overall resistant to MP-12 vaccination, however, and the elevated liver enzyme Gamma-Glutamyl Transferase (GGT) in sera could return to normal within 10 days. Subcutaneous vaccination with the MP-12 vaccine (5×103 pfu or 5×103 pfu) induced transient viremia (≤ 0.7 to 2.8 log10 pfu/ml) at 1 to 4 dpv, and vaccinated two- to seven-day-old lambs were fully protected from the pathogenic ZH501 strain (5×105 pfu, s.c.) when challenged at 14 dpv. Hubbard et al. also tested the efficacy of the MP-12 vaccine (102, 103, 104, 105, and 106 pfu doses) in two-week-old lambs [25]. Although lambs vaccinated with a 102 or 103 dose of MP-12 vaccine showed transient pyrexia after ZH501 strain challenge (1×106 pfu, s.c.), a higher dose protected lambs from pyrexia. These studies demonstrated the efficacy and attenuation of the MP-12 vaccine in ewes at 90 to 110 days pregnancy, as well as in newborn and young lambs.
Efficacy and attenuation of the MP-12 vaccine were also demonstrated in cows and calves. Cows in their third, fifth, or eighth month of pregnancy were subcutaneously vaccinated with 1×105 pfu of MP-12 vaccine [22]. Vaccination induced viremia of 0.7 to 2.5 log10 pfu at 2 to 4 dpv. Neutralizing antibodies were detectable at 7 dpv, and increased to the PRNT80 titers of ≥ 1:40 by 10 dpv. One cow died from watery diarrhea that persisted from 86 dpv to 164 dpv. Although mild inflammation in the small intestine and a necrogranuloma in a mesenteric lymph node were found in the cow, no histologic lesions associated with RVFV antigens were detected in the histological examination. All other cows delivered healthy calves with no detectable anti-RVFV antibody in precolostrum sera. A lactating dairy cow was also subcutaneously vaccinated with 1×105 pfu of MP-12 vaccine. A low level of viremia occurred at 1 dpv, whereas neutralizing antibody titers (PRNT80) of 1:80 to 1:1,280 were detected in milk by 10 dpv. A dose escalation study using yearling steers showed that the MP-12 vaccine has full protective efficacy from the pathogenic ZH501 strain challenge, at least with a 1×103 pfu vaccine dose (s.c.). Another safety study tested direct intramuscular (i.m.) vaccination of three- or five-month-old fetuses with 1×105 pfu of MP-12 vaccine through laparotomy of pregnant cows [23]. In the experiment, several abortions occurred, including within the control group, likely due to surgical trauma. Newborn calves that had been vaccinated as fetuses were healthy and had neutralizing antibody titers of 1:20 to 1:1,280 at birth. A recently conducted study showed that four-month-old calves vaccinated with 2.9×106 pfu of MP-12 vaccine, however, suffered multifocal hepatocellular necrosis (0.3 – 0.7 mm in diameter) in the liver at 2, 3, 4, and 10 dpv, and a viral antigen was detected associated with the necrotic lesions [37]. Those calves had suppurative bronchopneumonia irrelevant to the MP-12 vaccination, and systemic stress derived from respiratory disease may affect the pathogenesis of liver lesions in calves of this age. Taken together with a previous study [21], young animals are more susceptible to MP-12 vaccine infection and tend to incur transient hepatitis dependent on their immunological condition. Another study also showed that 6 month-old alpacas (Vicugna pacos) vaccinated with 106 TCID50 dose of MP-12 strain via s.c. resulted in mild focal lymphohistiocytic hepatitis with viral infection in hepatocytes, in one of three animals [38]. Because livestock animals may have various health conditions, further evaluation of vaccine safety in immunosuppressed animals will be meaningful to assess the vaccine safety in field use.
The safety of the MP-12 vaccine in immunosuppressed human individuals, pregnant women, or children has never been established. Thus, exposure of the MP-12 vaccine to those populations is a potential safety concern. No evidence of viral transmission from vaccinated animals to sentinel animals has yet been shown [36]. MP-12-vaccinated lactating cows did not shed viruses in milk, although viremia occurred at 2 to 4 dpv [22]. Conversely, the MP-12 vaccine was isolated from oropharyngeal swabs taken from two vaccinated rhesus macaques (6×103 pfu dose, i.m.) at 4 or 7 dpv [31], whereas no virus was recovered from oropharyngeal swabs taken from vaccinated two- to seven-day-old lambs (5×105 pfu dose, i.p. or s.c.) [21]. Future studies should elucidate the mechanism of oral shedding of the MP-12 vaccine in nonhuman primates because it may play a role in strong mucosal immunity elicited by this vaccine.
4. Adverse effects of RVF vaccination in pregnant animals
A study by Hunter et al. indicated adverse effects of the MP-12 vaccine in the fetuses of ewes [39]. Ewes in the first trimester (28, 35, and 42 days of pregnancy) or the second trimester (49 and 56 days of pregnancy) were vaccinated with 1×106 pfu of MP-12 vaccine. As a result, 13 to 19 viable lambs were delivered from each gestation group (n = 9 to 11), with a few abortions occurring due to dystocia. Overall, 0% (28 days), 30% (35 or 42 days), 20% (49 days), and 27% (56 days) of lambs were mildly to severely malformed at birth, including domed head (35 days), scoliosis (35, 42, 49, and 56 days), lordosis (49 and 56 days), kyphosis (42, 49, and 56 days), hydranencephaly and spinal hypoplasia (42, 49, and 56 days), and cerebellar hypoplasia (56 days). Morrill et al. performed a vaccination of ewes at 30 to 50 days of pregnancy with the MP-12 vaccine (1×105 pfu, s.c.) [24]. One of four vaccinated ewes delivered a dead and autolyzed fetus at 18 to 20 weeks of gestation, and viral RNA was detected in the fetus brain by PCR. These studies indicate a potential risk of fetal malformation due to vaccination during the first and second trimester of pregnancy. Considering that the pathogenic RVFV 35/74 strain (10 TCID50 dose, intraperitoneal injection) causes viral transmission into the fetus in sheep, even without detectable viremia [40], there should be an unidentified transmission route taken by RVFV to reach fetus.
Live-attenuated RVF vaccines other than the MP-12 vaccine have similar adverse effects in pregnant ewes. Coetzer et al. reported that vaccination of ewes at 42 to 74 days of pregnancy with the Smithburn vaccine resulted in abortion or malformation in three out of seven fetuses [41]. Moreover, vaccination of non-indigenous cattle of European breed with the Smithburn vaccine resulted in abortion of 28% of pregnant cows, with at least three cases of early fetal death or mummifications, and virus isolated from the fetus showed a RVFV sequence distantly related to the Smithburn strain [11]. Vaccination of does in the third month of pregnancy with the Smithburn vaccine resulted in abortion of the fetus in two of three animals at 10 to 28 dpv [42]. Due to such adverse effects, the Smithburn vaccine has never been recommended for pregnant animals.
The recently developed Clone 13 vaccine, which lacks 69% of the non-structural protein S (NSs) gene, also possesses a risk of vertical transmission of the virus into the fetus [43]. Ewes at 50 days of pregnancy were vaccinated with an overdose of Clone 13 vaccine (6.8 log10 TCID50, s.c.) to evaluate the vaccine’s safety. Among the subjects, seven lambs from five different ewes showed malformation of the central nervous system (e.g., hydranencephaly, hypoplasia of cerebrum, cerebellum, and spinal cord, brachygnathia, arthrogryposis, and/or scoliosis). No malformation occurred in lambs when ewes at 120 days of pregnancy were vaccinated with the Clone 13 vaccine (7.0 log10 TCID50, s.c.); however, in newborn lambs in both the 50 and 120 day groups, viral RNA was detected in blood or other organs, and precolostrum sera had RVFV-specific antibodies. In contrast, evaluation of the Clone 13 vaccine in field trials using sheep, goats, and cattle indicated that the vaccine did not cause notable abortion or fetal malformation [44,45], indicating that the adverse effects of the Clone 13 vaccine in pregnant animals were not notable with a directed dose.
Taken together, live-attenuated RVF vaccines have some risk of adverse effects in pregnant animals. The pathogenic RVFV strain is highly abortogenic, and most infected animals abort fetuses due to inflammation and necrosis of maternal caruncles and fetal cotyledons [26]. Apparently, the Smithburn vaccine has residual virulence in fetuses, and abortion and fetal death, rather than fetal malformation, can occasionally occur. The MP-12 and Clone 13 vaccines have potential risks of mild to severe teratogenicity of developing fetuses, rather than abortion, only when vaccination is performed early in pregnancy. The inactivated RVF vaccine is safe, and no abortion or fetal malformation may occur; however, formalin-inactivated RVF vaccine did not protect fetuses of ewes and cows from the pathogenic ZH501 challenge, and resulted in abortion of dead fetuses [13]. Attenuated, but efficacious RVF vaccines, such as the MP-12 or Clone 13 vaccines, are useful for rapidly inducing protective immunity in susceptible ruminants, which may minimize the impact of RVF outbreaks in ruminants. At the same time, it will be important to prepare alternative safe and efficacious vaccines to cover animals early in pregnancy, in order to avoid the above-mentioned problems associated with vaccination.
5. Application of the MP-12 vaccine to human use
RVFV is pathogenic to both animals and humans, and vaccination is one of the most effective measures to prevent the disease. Pathogenesis of RVF in human patients is different from that in ruminants, and is characterized by febrile illness, hemorrhagic fever, encephalitis, and blindness, rather than abortion or fetal malformation. The formalin-inactivated RVF vaccine (TSI-GSD-200) was developed from the pathogenic Entebbe strain, and the vaccine requires three repeated vaccinations and periodical boosters to maintain its protective efficacy [46]. The MP-12 vaccine is an Investigational New Drug, and its safety and immunogenicity have been tested in clinical trials [32].
In the initial human trial, three out of four volunteers administered with the MP-12 vaccine (104.4 pfu dose, s.c.) developed neutralizing antibodies, whereas all four showed transient mild to moderate elevation of serum alanine aminotransferase (ALT) and/or aspartate aminotransferase (AST) [33]. In a subsequent dose escalation study, 22 humans were administered with the MP-12 vaccine (either 104.4, 103.4, 102.4, or 101.4 pfu dose, s.c.) [33]. Within the 104.4 pfu dose group, seroconversion (positive for IgM or IgG via either PRNT50 or PRNT80, or ELISA) occurred in two of four individuals, in addition to injection site tenderness (3 of 4), severe AST elevation (1 of 4), or elevated creatine phosphokinase (CPK) (3 of 4).
In another clinical trial for dose escalation and route comparison, a comparative analysis of MP-12 vaccination in humans via the s.c. route (104.7 pfu, n = 10) or i.m. route (103.4 pfu, n = 6, or 104.4 pfu, n = 27) was performed [33]. Overall, 93% of subjects (40 of 43) showed an increase in neutralizing antibody titers (PRNT80 ≥20) from 14 to 21 dpv. Peak IgM and IgG ELISA titers were higher in the s.c. injection group than in the i.m. group, whereas PRNT50 and PRNT80 titers were higher and more sustained in the i.m. (104.4 pfu dose) injection group (peak geometric PRNT80 titer was 1:277) than in the s.c. injection group. PRNT50 and PRNT80 titers of ≥ 1:20 were maintained in 87% of individuals in the i.m. group with 104.4 pfu dose for one year, indicating a better vaccine immunogenicity than that of TSI-GSD-200 (formalin-inactivated Entebbe strain) [46,47]. One volunteer (i.m, 104.4 pfu) developed viremia of 1.3 pfu/ml at 9 dpv. Adverse effects within the i.m. group (104.4 pfu) were mild to moderate: chills (7.4%), dizziness (11.1%), fever (3.7%), headache (29.6%), malaise (22.2%), or vomiting (7.4%). According to the guideline of the U.S. Food and Drug Administration [48], the abnormality grading of liver enzymes (ALT and AST) is defined as the relative increase compared to the upper limit of the normal range: i.e., 1.1× – 2.5× (mild, Grade 1), 2.6× – 5.0× (moderate, Grade 2), 5.1× – 10× (severe, Grade 3), >10× (potentially life threatening, Grade 4), and that of CPK as 1.25× – 1.5× (mild, Grade 1), 1.6× – 3.0× (moderate, Grade 2), 3.1× – 10× (severe, Grade 3), >10× (potentially life threatening, Grade 4). Symptomatic transient elevation of serum ALT, AST, CPK, and lactate dehydrogenase (LDH) were found in all groups (40% in s.c. group, 50% in i.m. 103.4 pfu dose group, and 44% in i.m. 104.4 pfu dose group). Although most cases were mild or moderate (Grade 1 or 2) increases, one vaccinee in the i.m. 103.4 pfu dose group had 4,139 U/L of LDH (Grade 3) and 587 U/L of AST (Grade 4). Grade 4 CPK elevation was also recorded in one in the i.m. 103.4 pfu dose group and two in the placebo group, all of which were recorded after physical exercise with muscle fatigue. The values of CPK, AST, ALT, and LDH were returned to normal within a few days without clinical significance in all cases. Further evaluation will be required to ensure the safety of MP-12 vaccine candidate in humans.
Since vaccination via the i.m. route induced higher neutralizing titers than that via the s.c. route, further clinical trials for vaccine immunogenicity and viral genetic stability were performed. A total of 19 volunteers were vaccinated with the MP-12 vaccine (1×105 pfu, i.m.) and 18 (95%) had increased PRNT80 titers of ≥ 1:20 by 28 dpv, and maintained 1:20 or higher titers for 12 months afterwards [34]. Follow-up evaluation of those volunteers showed that eight of nine tested sera still maintained neutralizing antibodies of ≥ 1:20 at five years post vaccination. Adverse effects were reported including headache (58%), fatigue (42%), nausea (26%), flu-like symptoms (21%), fever (16%), and local tenderness (48%). Ophthalmologic examination (28 dpv) or electrocardiogram (three months post vaccination) showed normal results. Virus isolation was attempted from plasma (1 ml) and buffy coat (0.2 ml) specimens collected at 1 to 14 dpv. Vero cells were adsorbed with those clinical specimens in T-25 flasks at 37°C for one hour, and further incubated with fresh media for five days. After additional medium replacement, cells were incubated for an additional five days. The freeze-thawed cells were added into fresh Vero cells, and a second 10-day incubation was performed with medium replacement at 5 dpi. All negative flasks were tested for viral RNA via RT-PCR. When cells showed cytopathic effects (CPE), the supernatants derived from freeze-thawed cell samples containing viruses were further amplified in fresh Vero cells. Virus titers of culture supernatants were measured by plaque assay. As a result, nine MP-12 isolates were amplified from the plasma samples of five vaccinees at 4 to 9 dpv, and two isolates were made from buffy coat samples at 7 and 8 dpv. A total of 10 mutations (two silent mutations and eight amino acid substitutions) were found, yet none were reversion mutations. LD50 of each of the 11 isolates in 19-day-old CD1 mice, a mouse model susceptible to MP-12 in an age-dependent manner, was greater than 1×101.88 pfu/ml, indicating no increase in the virulence of the MP-12 strain due to those mutations. Overall, clinical trials demonstrated that the MP-12 vaccine induces neutralizing antibodies with a single dose for at least several years. Due to a lack of RVF in the U.S., the vaccine efficacy study in humans is difficult. Thus, an alternative approach to claim a valid efficacy may be applicable using more than one appropriate animal models under Good Laboratory Practice and the Animal Welfare Act under the Animal Rule of the FDA [49–51].
6. Protective efficacy of the MP-12 vaccine against aerosol exposure to the pathogenic RVFV strain
Because RVFV exposure via aerosol (e.g., bioterrorism, laboratory exposure) may alter the pathogenesis of disease, it is important to evaluate the protective efficacy of the MP-12 vaccine against aerosol exposure challenge. Rhesus monkeys were vaccinated with the MP-12 vaccine (6×103 pfu, i.m.) and challenged with a small particle (<5 μm) aerosol exposure of the pathogenic ZH501 strain (~ 5×105 pfu) [31]. Viremia of <2.0 log10 pfu/ml was detected in three of nine vaccinated monkeys, and the virus was also isolated from oropharyngeal swabs at 4 or 7 dpv. Neutralizing antibody titers (PRNT80) of ≥ 1:20 were detected at 7 dpv, and increased to between 1:320 and 1:2,560 by 126 dpv. Slight increases in AST and CK were observed in vaccinated animals from 1 to 3 dpv, but all vaccinated animals survived the challenge without detectable clinical signs or viremia, whereas all control animals developed viremia after the challenge. Thus, vaccination of MP-12 via the i.m. route was shown to be efficacious to protect against aerosol exposure.
Another study also showed the efficacy of the MP-12 vaccine via the aerosol or intranasal vaccination route [30]. Rhesus monkeys were vaccinated with MP-12 (~ 1×105 pfu via aerosol, or 5×104 pfu via intranasal vaccination route) and challenged with a small particle (<5 μm) aerosol exposure of the pathogenic ZH501 strain at 56 dpv. Vaccinated monkeys did not develop viremia, and increased titers of neutralizing antibody to 1:40 or more by 28 dpv. Vaccinated monkeys were fully protected from aerosol challenge of the ZH501 strain. Thus, this study demonstrated the efficacy of the MP-12 vaccine via the aerosol or intranasal route. Because none of the vaccinated monkeys showed clinical signs, safe vaccination with the MP-12 vaccine via the mucosal route could now be considered for massive vaccination without using a needle.
7. Attenuation mechanism of the MP-12 vaccine and the risk of gaining virulence
Since the RVFV genome is comprised of three RNA segments, co-infection of the vaccine strain and the pathogenic strain may generate RVFV strains encoding one or two RNA segments of the vaccine strain (reassortant strain). This likely occurs when animals are vaccinated with live-attenuated vaccine during a RVF outbreak. During the 2010 RVF outbreak in South Africa, a reassortant RVFV strain was isolated from a febrile patient who had self-injected using an automatic syringe during sheep vaccination with a live-attenuated Smithburn vaccine [12]. Mosquito vectors may be infected with reassortant strains by ingesting a viremic blood meal, if the blood contains sufficient titers of reassortant viruses. This scenario is thought to be rare, however, as long as vaccination is conducted appropriately by excluding potentially viremic animals. Most vaccinated animals are not infected with the pathogenic RVFV strain, and mosquitoes cannot be infected with the vaccine strain by feeding on vaccinated animals with low viremia, such as ≤3.0 log10 pfu/ml [27,52,53]. Field use of a live-attenuated vaccine will require special caution, however, to avoid vaccination of already infected animals [36], because MP-12 infection and dissemination rates of mosquito populations in endemic areas may not be the same as those found in mosquito colonies available in laboratories. Another concern is the emergence of reassortant strains between RVFV and other bunyaviruses, which may have novel virological or pathological phenotypes. For example, Ngari virus (genus Orthobunyavirus), which caused a large outbreak in East Africa in 1997 – 1998, is a natural reassortant encoding Bunyamwera virus S- and L-segments, and a Batai virus M-segment [54,55]. Similarly, Potosi virus and Main Drain virus (both belonging to the genus Orthobunyavirus) encode the M-segment, clustering into a distant phylogenetic clade [56]. Thus, an incorporation of the M-segment from other bunyavirus species may contribute to the evolution of bunyaviruses. African phleboviruses, such as Arumowot virus (vector: Culex spp., Mansonia spp.; host animals: rodents and birds) or Gabek forest virus (vector: Phlebotomine sandfly sp.; host animals: rodents) [57–60] may serve as potential donors of heterogeneous viral genomic RNA segments to form a novel reassortant virus with RVFV, although the viability of such presumable reassortant strains has not yet been evaluated.
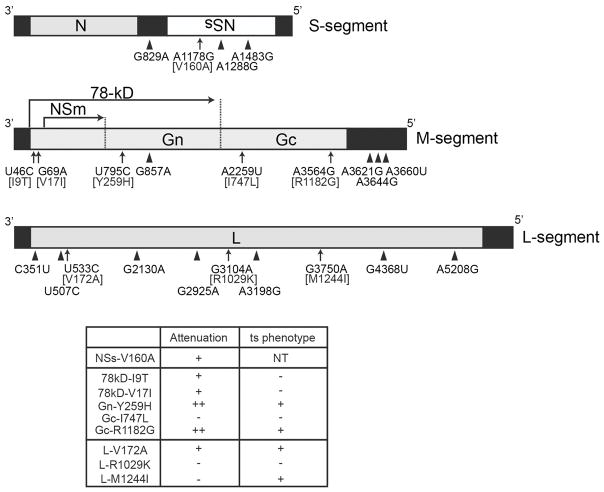
The MP-12 vaccine encodes 23 mutations in the genome from the pathogenic ZH548 strain (Fig. 1): four in the S-segment, nine in the M-segment, and 10 in the L-segment. It was not known how the MP-12 strain could be attenuated by those mutations and thus, evaluation of attenuation level for each segment or mutation was performed using reverse genetics. Outbred mice were infected with 1×103 pfu (i.p.) of reassortant RVFV resulting from a combination of the pathogenic ZH501 strain (Z) and MP-12 strain (M): i.e., Z/Z/M, Z/M/Z, and M/Z/Z (in the order of L/M/S) [61]. Mortality caused by Z/Z/M, Z/M/Z, and M/Z/Z was 100%, 60%, and 80%, respectively. All infected mice survived for at least five days before clinical signs became evident, however, indicating that those reassortant RVFV were more attenuated than the parental ZH501 strain. Thus, any reassortant strains derived from the MP-12 vaccine are more attenuated than pathogenic RVFV strains. A previous study showed that NSs-V160A is likely responsible for the attenuation of the MP-12 S-segment [62]. Another mutagenesis study identified two major mutations in the MP-12 M-segment, which can independently contribute to the attenuation of the ZH501 strain (Gn-Y259H and Gc-R1182G) [61]. None of the individual MP-12 L-segment mutations could affect mortality caused by the ZH501 strain in mice [61] and thus, the L-segment could be attenuated by a combination of those mutations. Saluzzo et al. showed that the MP-12 strain displays a temperature-sensitive (ts) phenotype independent of the M- and L-segments [63]. The restriction temperature of the MP-12 strain was 38°C, and viral replication was shut-off at 40°C and above [64]. Reassortant RVFV strains (Z/Z/M, Z/M/Z, and M/Z/Z) showed that MP-12 L-, M-, and S-segments independently contribute to the ts phenotype (L > M > S) [64]. This study also identified four independent ts mutations: Gn-Y259H, Gc-R1182G, L-V172A, and L-M1244I. In particular, L-M1244I partially inhibited viral RNA synthesis at 37°C and reduced the size of plaques in Vero E6 cells at 37°C, although the generation of infectious progeny viruses of the ZH501 strain encoding L-M1244I continued to occur efficiently at 37°C. Because the body temperatures of sheep or cattle are normally 38°C or above, those four ts mutations should redundantly limit viral replication in ruminants. High throughput sequencing of the MP-12 vaccine lot (TSI-GSD-223) did not detect any parental ZH548 strain sequence at those four ts mutation sites [19]. Furthermore, viral isolates from MP-12 vaccinees during a clinical trial did not show any reversion mutations at any of the key mutation sites [34]. Overall, it is unlikely that a highly pathogenic RVFV strain can be formed from the MP-12 vaccine strain during the manufacturing of MP-12 vaccine or during the limited viral replication in vivo.
Figure 1. Schematic representation of RVFV MP-12 strain genome structure.
Negative-sense RNA genome of the MP-12 vaccine is shown, including Small (S)-, Medium (M)-, and Large (L)-segments. A total of 23 mutations of the MP-12 strain compared to the parental ZH548 strain are also specified. When individual MP-12 mutations were introduced into the pathogenic ZH501 strain, the resulting mutant viruses displayed attenuation and/or temperature-sensitivity (ts) phenotypes, as summarized in the box under the genome schematics [61,98].
8. Modification of the MP-12 vaccine for future applications
Although the MP-12 vaccine is highly efficacious in animals and humans, reverse genetics for RVFV could generate several novel variants of the MP-12 strain with improved vaccine safety [62,65–67]. A recombinant MP-12 strain (rMP-12) was initially generated with silent mutations (Xho I sites) in the L-, M-, and S-segments [65]. For further vaccine development, those silent mutations were removed, and designated as authentic recombinant MP-12 (arMP-12). In this review, all recombinant MP-12 strains will be just described as rMP-12, to avoid a confusion. The rMP12-ΔNSm21/384 variant lacks expression of both the 78kD protein and the NSm protein from the M-segment [68]. Because a lack of 78kD and NSm affects the systemic viral dissemination from midgut in mosquitoes [69–71], rMP12-ΔNSm21/384 is less likely to be transmitted by mosquito vectors. In addition, antibodies against the NSm protein can be raised in animals infected with pathogenic RVFV [72], and a lack of the anti-NSm antibody may be useful as a marker for the differentiation of infected animals from vaccinated animals (DIVA). The rMP12-ΔNSm21/384 variant was as efficacious as the MP-12 vaccine in pregnant ewes, lambs, and calves [24,73,74]. The truncation of the 78kD and NSm proteins can only weakly attenuate RVFV [71,75,76], and there was still a potential risk of viral infection of fetuses when vaccination was performed at 30 to 50 days of pregnancy [24].
The rMP12-ΔNSs16/198 (rMP12-C13type) variant encodes an in-frame 69% truncation of the NSs gene in the S-segment. Due to the shortened NSs gene, this strain shows impaired viral replication in type-I interferon (IFN)-competent cells [65]. Although rMP12-ΔNSs16/198 was shown to be highly efficacious in mice [28], the immunogenicity was not as strong as that of the parental MP-12 vaccine or rMP12-ΔNSm21/384 in ruminants [24]. A shortened NSs gene cannot completely attenuate RVFV, and mouse encephalitis can occur in some infected mice [75]. The rMP12-ΔNSs16/198 is highly safe vaccine, however, due to significant attenuation in all three segments, and no viremia or diseases have been found to occur in vaccinated mice [77]. This vaccine may be an alternative human RVF vaccine candidate with an additional attenuation in MP-12 vaccine candidate.
Because deletion of the NSs gene in the S-segment might over-attenuate the MP-12 vaccine for practical use, replacement of the MP-12 NSs gene with other functional genes, which can contribute to the immunogenicity of the vaccine, was evaluated. The rMP12-PKRΔE7 variant encodes human dominant-negative protein kinase R (PKR), in place of MP-12 NSs [78]. The recombinant MP-12 strain encoding the mouse analog of PKRΔE7 protein, mPKRN167 [79] was shown to express more accumulation of N proteins than rMP12-ΔNSs16/198 at the draining lymph node in vaccinated mice by antigen-capture ELISA for the detection of RVFV N proteins, and all vaccinated mice were protected from pathogenic ZH501 strain challenge [28]. The pathogenic RVFV ZH501 strain was significantly attenuated by the replacement of NSs gene with the PKRΔE7 [75]. Chimeric MP-12 strains encoding other phlebovirus NSs genes in place of the MP-12 NSs gene were also tested for attenuation and efficacy in mice: i.e., NSs genes derived from Toscana virus (TOSV), Sandfly fever Sicilian virus (SFSV), Punta Toro virus (PTV) Adames strain, or PTV Balliet strain. Those recombinant MP-12 strains were designated as rMP12-TOSNSs, rMP12-SFSNSs, rMP12-PTANSs, or rMP12-PTBNSs, respectively. Due to frequent occurrence of viral encephalitis in mice, rMP12-TOSNSs was not considered for further vaccine efficacy in mice [80]. The rMP12-PTANSs and rMP12-SFSNSs were both highly immunogenic in mice, and did not cause disease more than did parental MP-12 [29]. In addition, the pathogenic ZH501 strain was attenuated through the chimeric S-segment encoding either the NSs of PTV Adames strain or SFSV [75]. The protective efficacy and adverse effects of those chimeric strains in pregnant ewes or fetuses have not been evaluated.
9. Commercially available veterinary RVF vaccine in endemic countries and novel vaccine candidates
Two live-attenuated RVF vaccines are available for veterinary use in endemic area. The Smithburn vaccine is available from Onderstepoort Biological Product (OBP) or Kenya Veterinary Vaccine Producing Institute (sold as RIFTVAX TM), whereas the Clone 13 vaccine is available from OBP [81]. On the other hand, three different inactivated RVF vaccines are also available in endemic regions. The binary ethylenamine-inactivated RVF ZH501 strain vaccine is available from Veterinary Serum and Vaccine Research Institute (VSVRI) in Egypt, the formalin-inactivated RVF Menya strain (Menya/Sheep/258) vaccine is available from the holding company for biological products and vaccines (VACSERA) in Egypt [82]. Another formalin-inactivated vaccine derived from a field strain isolated from a cow, is available from OBP [83,84]. Both the inactivated RVF vaccine and Clone 13 vaccine, but not Smithburn vaccine, may be used for pregnant animals. RVF vaccines may not be always available from above manufacturers due to unforeseen circumstances. It is an important issue how to increase the coverage of RVF vaccination in livestock animals in Africa [12,81,85]. In Saudi Arabia, approximately 10 million ruminants (mostly sheep and goats, six months of age and older) received the Smithburn vaccine in 2001; although no large outbreak has occurred in Saudi Arabia since 2001, eradication of RVF has not been successful, and a few animal and human RVF cases were still confirmed in 2010 [86].
With the limitation of efficacy or safety of currently available RVF vaccines, novel RVF vaccines with better safety and efficacy may replace traditional RVF vaccines [15]. The DDvax vaccine (recombinant ZH501 strain encoding deletions of both NSs and NSm genes [rZH501-ΔNSs-ΔNSm], 1×103 to 1×105 pfu dose, s.c.) showed protective efficacy in pregnant ewes at 42 days of pregnancy, without detectable adverse effects in newborn lambs [72]. The CDC, Deltamune, and Merial supported further evaluation of vaccine efficacy in cattle or marmosets toward the development of safe DIVA vaccine for RVF [15]. The R566 vaccine, which was isolated from co-infection of the Clone 13 and MP-12 vaccines, encodes the Clone 13 S-segment and MP-12 M- and L-segments. Although the R566 vaccine is less immunogenic than the Clone 13 vaccine, this vaccine could sufficiently protect lambs from pathogenic RVFV challenge [15,87]. Non-spreading RVFV (NSR) consisting of only the S- and L-segments [88], in which the Gn protein can be expressed in place of the NSs gene in the S-segment (NSR-Gn), was also shown to be efficacious in lambs with a single dose, and is under development [15,87]. Most recently, a chimpanzee adenovirus vaccine expressing RVFV GnGc (ChAdOx1-GnGc) was developed as a veterinary vaccine candidate, and its protective efficacy (1×109 infectious units [IU], i.m., single dose) was shown in four- to six-month-old cattle, goats, and sheep, whereas thermostabilized ChAdOx1-GnGc was resistant to 25, 37, or 45°C for six months with retained vaccine potency [89–91]. In the U.S., glycoprotein subunit RVF vaccine (Gn ectodomain: Gne, and Gc, each 50 μg), which was purified from the lysates of insect Sf9 cells infected with recombinant baculovirus, was developed for veterinary vaccination [92–94]. With adjuvant (ISA25, Seppic, France) and one booster dose at 21 dpv, this vaccine could protect sheep from pathogenic RVFV challenge at 35 dpv. The glycoprotein subunit vaccine is safe and applicable to DIVA due to a lack of antibody responses to viral proteins other than Gn and Gc. In addition to those described, other various RVF vaccine candidates are also being studied for further development, which is important for future vaccination and eradication strategy in endemic countries [14,16,17].
10. Expert commentary
In endemic countries, mosquitoes potentially harbor pathogenic RVFV, regardless of any ongoing RVF outbreak [8,95]. In such an environment, RVF vaccination may be focused on: (1) the containment of active RVF outbreaks and (2) long-term protection from RVF exposure to infected mosquitoes. Because RVF vaccination performed during a RVF outbreak increases the risk of co-infection of the pathogenic RVFV strain and live-attenuated RVFV strain in animals, it is ideal that endemic countries continue regular vaccination of susceptible animals with commercially available efficacious RVF vaccines before new outbreaks start. Although the Smithburn vaccine has been used for a long period of time in endemic areas, residual virulence in pregnant animals hampers safe vaccination of highly susceptible animal populations. Unfortunately, mosquitoes transmit RVFV into offspring without the involvement of animals and thus, regular vaccination may be the only practically effective approach to protect susceptible livestock animals from continuous RVFV exposure by infected mosquitoes, unless infected mosquitoes can be eradicated in the endemic area. Further safe vaccines, including other live-attenuated vaccines, subunit vaccines, or replicon/vector vaccines, can better support the safe vaccination of ruminants in endemic countries. It will therefore be important to accelerate the communication between vaccine manufacturers in endemic countries and vaccine stakeholders, to facilitate the introduction of better RVF vaccines in endemic countries. The MP-12 vaccine has never been used in endemic countries; however, if the MP-12 vaccine were to become available in such places, the long-term protection of ruminants, including newborn animals through colostrum, as well as viral spill-over into mosquitoes, should be evaluated on a large scale. In non-endemic countries, including the U.S., Canada, and European countries, no vaccination will be required until the first RVFV case is confirmed, as early containment of viral spread will be important for minimizing the impact on society. A national stockpile vaccine, such as the MP-12 vaccine in the U.S., will allow immediate vaccination of susceptible animals in case of an unexpected RVF outbreak. Because the MP-12 vaccine lacks a DIVA marker, subunit vaccines or replicon or vector vaccines will be more useful than the MP-12 vaccine on the occasion when rapid protection is less important, and surveillance of viral spread is required.
11. Five-year view
Highly immunogenic RVF vaccines, such as ChAdOx1-GnGc, NSR-Gn, and subunit Gne/Gc, have been developed to replace traditional live-attenuated vaccines or formalin-inactivated RVF vaccines. It will be important to evaluate protective efficacy of new vaccines in pregnant ewes and cows for further demonstration of vaccine safety. If colostrum of vaccinated animals contains sufficient neutralizing antibodies to protect newborn animals, vaccination will effectively prevent the spread of RVFV by protecting highly susceptible newborn animals. The conditional license of MP-12 vaccine may be changed in the U.S. in future. This vaccine is attenuated in both animals and humans, and will be also useful for endemic countries if this vaccine becomes available outside the U.S. A new generation MP-12 vaccine, rMP12-ΔNSm21/384, will be less likely transmitted by mosquitoes and has a similar vaccine potency to that of the parental MP-12 vaccine. In the next five years, commercial development of novel RVF vaccines may be expected in endemic countries. Human RVF vaccination is also important for populations with high risk of RVFV exposure. Because the vaccine market may be small, the use of RVF vaccine such as MP-12 vaccine, evaluated both in animals and humans, will be an option without additional investment. The MP-12 vaccine has been shown to elicit long-term immunity in humans with a single dose, whereas further evaluation of vaccine safety in healthy or immunosuppressed individuals will be required. High risk personnel such as veterinarians or animal workers should be vaccinated with an appropriate RVF vaccine before handling infected animals during a RVF outbreak. For those who become infected and develop hemorrhagic fever or encephalitis, current medicine may not support prophylaxis. Post-exposure vaccination with rMP12-ΔNSs16/198 showed reduction of pathogenic RVFV replication in liver or spleen, and resulted in improved survival rate in highly susceptible mice and hamsters [96,97]. Future studies should also identify antivirals or other biologicals which can rapidly reduce viral replication and support recovery from late stages of infection.
Key issues.
RVFV is endemic to Africa and the Arabian Peninsula, and infected mosquitoes can transmit viruses to ruminants and humans.
RVFV is teratogenic in ruminants, such as sheep, cattle, and goats.
RVF vaccines for animals are available in endemic areas, yet the development of further safe and efficacious vaccines for pregnant animals remains important.
The live-attenuated MP-12 vaccine is attenuated and efficacious for both animals and humans, and is conditionally licensed for animal use in the U.S.
Effective control of a RVF outbreak should be considered using suitable RVF vaccines in different scenarios.
Acknowledgments
The author thanks Dr. J.C. Morrill for sharing the information of IND BB-4307, and Ms. H.J. Ly for proof-reading the manuscript.
Financial and competing interest disclosure
A MP-12 vaccine study using reverse genetics was supported by NIH grant R01 AI08764301-A1 and by the Sealy Center for Vaccine Development at the University of Texas Medical Branch at Galveston. T.I. claims intellectual property of reverse genetics for the MP-12 strain. This author has no financial conflict with any organization or entity in relation to the subject matter or materials discussed in this manuscript.
References
- 1.Daubney R, Hudson JR. Enzootic hepatitis or Rift Valley fever: An undescribed virus disease of sheep cattle and man from east Africa. J Path Bact. 1931;34:545–579. [Google Scholar]
- 2.Smithburn KC, Haddow AJ, Gillett JD. Rift Valley fever; isolation of the virus from wild mosquitoes. Br J Exp Pathol. 1948;29(2):107–121. [PMC free article] [PubMed] [Google Scholar]
- 3**.Swanepoel R, Coetzer JAW. Rift Valley fever. In: Coetzer JAW, Tustin RC, editors. Infectious diseases of livestock with special reference to southern Africa. 2. Cape Town, South Africa: Oxford University Press; 2004. pp. 1037–1070. A historical review of Rift Valley fever in Africa. [Google Scholar]
- 4.Ikegami T, Makino S. The Pathogenesis of Rift Valley Fever. Viruses. 2011;3(5):493–519. doi: 10.3390/v3050493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peters CJ, Meegan JM. Handbook Series of Zoonoses, Section B: Viral Zoonoses. Vol. 1. Boca Raton, FL: CRC Press; 1981. Rift Valley Fever; pp. 403–420. [Google Scholar]
- 6.Balkhy HH, Memish ZA. Rift Valley fever: an uninvited zoonosis in the Arabian peninsula. Int J Antimicrob Agents. 2003;21(2):153–157. doi: 10.1016/s0924-8579(02)00295-9. [DOI] [PubMed] [Google Scholar]
- 7.Nanyingi MO, Munyua P, Kiama SG, et al. A systematic review of Rift Valley Fever epidemiology 1931–2014. Infect Ecol Epidemiol. 2015;5:28024. doi: 10.3402/iee.v5.28024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu W, Sun FJ, Tong YG, Zhang SQ, Cao WC. Rift Valley fever virus imported into China from Angola. Lancet Infect Dis. 2016;16(11):1226. doi: 10.1016/S1473-3099(16)30401-7. [DOI] [PubMed] [Google Scholar]
- 9.Pepin M, Bouloy M, Bird BH, Kemp A, Paweska J. Rift Valley fever virus (Bunyaviridae: Phlebovirus): an update on pathogenesis, molecular epidemiology, vectors, diagnostics and prevention. Vet Res. 2010;41(6):61. doi: 10.1051/vetres/2010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smithburn KC. Rift Valley fever; the neurotropic adaptation of the virus and the experimental use of this modified virus as a vaccine. Br J Exp Pathol. 1949;30(1):1–16. [PMC free article] [PubMed] [Google Scholar]
- 11.Botros B, Omar A, Elian K, et al. Adverse response of non-indigenous cattle of European breeds to live attenuated Smithburn Rift Valley fever vaccine. J Med Virol. 2006;78(6):787–791. doi: 10.1002/jmv.20624. [DOI] [PubMed] [Google Scholar]
- 12*.Grobbelaar AA, Weyer J, Leman PA, Kemp A, Paweska JT, Swanepoel R. Molecular epidemiology of Rift Valley fever virus. Emerg Infect Dis. 2011;17(12):2270–2276. doi: 10.3201/eid1712.111035. Demonstration of a natural reassortant strain between Smithburn vaccine and pathogenic RVFV strain in Africa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yedloutschnig RJ, Dardiri AH, Mebus CA, Walker JS. Abortion in vaccinated sheep and cattle after challenge with Rift Valley fever virus. Vet Rec. 1981;109(17):383–384. doi: 10.1136/vr.109.17.383. [DOI] [PubMed] [Google Scholar]
- 14.Kortekaas J. One Health approach to Rift Valley fever vaccine development. Antiviral Res. 2014;106:24–32. doi: 10.1016/j.antiviral.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 15*.FAO. The last hurdles towards Rift Valley Fever control. FAO Animal Production and Health Report No. 9; Report on the Ad hoc workshop on the current state of Rift Valley fever vaccine and diagnostics development; Rome. 5–7 March 2014; Rome, Italy: 2015. Update of RVF vaccine development in 2015. [Google Scholar]
- 16.Indran SV, Ikegami T. Novel approaches to develop Rift Valley fever vaccines. Front Cell Infect Microbiol. 2012;2:131. doi: 10.3389/fcimb.2012.00131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ikegami T, Makino S. Rift valley fever vaccines. Vaccine. 2009;27(Suppl 4):D69–72. doi: 10.1016/j.vaccine.2009.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18*.Caplen H, Peters CJ, Bishop DH. Mutagen-directed attenuation of Rift Valley fever virus as a method for vaccine development. J Gen Virol. 1985;66(Pt 10):2271–2277. doi: 10.1099/0022-1317-66-10-2271. Original research paper describing the development of MP-12 strain. [DOI] [PubMed] [Google Scholar]
- 19.Lokugamage N, Freiberg AN, Morrill JC, Ikegami T. Genetic Subpopulations of Rift Valley Fever ZH548, MP-12 and Recombinant MP-12 Strains. J Virol. 2012;86:13566–13575. doi: 10.1128/JVI.02081-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20**.Morrill JC, Jennings GB, Caplen H, Turell MJ, Johnson AJ, Peters CJ. Pathogenicity and immunogenicity of a mutagen-attenuated Rift Valley fever virus immunogen in pregnant ewes. Am J Vet Res. 1987;48(7):1042–1047. Immunogenicity and safety of MP-12 vaccine have been analyzed in ewes. [PubMed] [Google Scholar]
- 21.Morrill JC, Carpenter L, Taylor D, Ramsburg HH, Quance J, Peters CJ. Further evaluation of a mutagen-attenuated Rift Valley fever vaccine in sheep. Vaccine. 1991;9(1):35–41. doi: 10.1016/0264-410x(91)90314-v. [DOI] [PubMed] [Google Scholar]
- 22.Morrill JC, Mebus CA, Peters CJ. Safety and efficacy of a mutagen-attenuated Rift Valley fever virus vaccine in cattle. Am J Vet Res. 1997;58(10):1104–1109. [PubMed] [Google Scholar]
- 23.Morrill JC, Mebus CA, Peters CJ. Safety of a mutagen-attenuated Rift Valley fever virus vaccine in fetal and neonatal bovids. Am J Vet Res. 1997;58(10):1110–1114. [PubMed] [Google Scholar]
- 24.Morrill JC, Laughlin RC, Lokugamage N, et al. Safety and immunogenicity of recombinant Rift Valley fever MP-12 vaccine candidates in sheep. Vaccine. 2013;31:559–565. doi: 10.1016/j.vaccine.2012.10.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hubbard KA, Baskerville A, Stephenson JR. Ability of a mutagenized virus variant to protect young lambs from Rift Valley fever. Am J Vet Res. 1991;52(1):50–55. [PubMed] [Google Scholar]
- 26.Baskerville A, Hubbard KA, Stephenson JR. Comparison of the pathogenicity for pregnant sheep of Rift Valley fever virus and a live attenuated vaccine. Res Vet Sci. 1992;52(3):307–311. doi: 10.1016/0034-5288(92)90029-2. [DOI] [PubMed] [Google Scholar]
- 27.Miller MM, Bennett KE, Drolet BS, et al. Evaluation of the efficacy, potential for vector transmission, and duration of immunity of MP-12, an attenuated Rift Valley fever virus vaccine candidate, in sheep. Clin Vaccine Immunol. 2015;22(8):930–937. doi: 10.1128/CVI.00114-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lihoradova O, Kalveram B, Indran SV, et al. The dominant-negative inhibition of double-stranded RNA-dependent protein kinase PKR increases the efficacy of Rift Valley fever virus MP-12 vaccine. J Virol. 2012;86(14):7650–7661. doi: 10.1128/JVI.00778-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lihoradova OA, Indran SV, Kalveram B, et al. Characterization of Rift Valley Fever Virus MP-12 Strain Encoding NSs of Punta Toro Virus or Sandfly Fever Sicilian Virus. PLoS Negl Trop Dis. 2013;7(4):e2181. doi: 10.1371/journal.pntd.0002181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morrill JC, Peters CJ. Mucosal Immunization of Rhesus Macaques With Rift Valley Fever MP-12 Vaccine. J Infect Dis. 2011;204(4):617–625. doi: 10.1093/infdis/jir354. [DOI] [PubMed] [Google Scholar]
- 31.Morrill JC, Peters CJ. Protection of MP-12-vaccinated rhesus macaques against parenteral and aerosol challenge with virulent rift valley fever virus. J Infect Dis. 2011;204(2):229–236. doi: 10.1093/infdis/jir249. [DOI] [PubMed] [Google Scholar]
- 32.Morrill JC, Peters CJ. Pathogenicity and neurovirulence of a mutagen-attenuated Rift Valley fever vaccine in rhesus monkeys. Vaccine. 2003;21(21–22):2994–3002. doi: 10.1016/s0264-410x(03)00131-2. [DOI] [PubMed] [Google Scholar]
- 33**.Pittman PR, McClain D, Quinn X, et al. Safety and immunogenicity of a mutagenized, live attenuated Rift Valley fever vaccine, MP-12, in a Phase 1 dose escalation and route comparison study in humans. Vaccine. 2016;34(4):424–429. doi: 10.1016/j.vaccine.2015.12.030. Clinical trial of MP-12 vaccine including the evaluation of adverse effects. [DOI] [PubMed] [Google Scholar]
- 34**.Pittman PR, Norris SL, Brown ES, et al. Rift Valley fever MP-12 vaccine Phase 2 clinical trial: Safety, immunogenicity, and genetic characterization of virus isolates. Vaccine. 2016;34(4):523–530. doi: 10.1016/j.vaccine.2015.11.078. Clinical trial of MP-12 vaccine including the analysis of MP-12 vaccine isolates from vaccinees. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hills RE. Notice no. 13–12. Center for Veterinary Biologics; Ames, IA: 2013. Issuance of a conditional license for Rift Valley fever vaccine, modified live virus. [Google Scholar]
- 36.Environmental Assessment - Rift Valley Fever Vaccine, Modified Live Virus (Unlicensed in Canada and USA) The Canadian Centre for Veterinary Biologics (CCVB) of the Canadian Food Inspection Agency (CFIA); 2013. http://www.inspection.gc.ca/animals/veterinary-biologics/licensed-products/environmental-assessments/rift-valley-fever-vaccine/eng/1393256796335/1393256857602. [Google Scholar]
- 37.Wilson WC, Bawa B, Drolet BS, et al. Evaluation of lamb and calf responses to Rift Valley fever MP-12 vaccination. Vet Microbiol. 2014;172(1–2):44–50. doi: 10.1016/j.vetmic.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 38.Rissmann M, Ulrich R, Schroder C, et al. Vaccination of alpacas against Rift Valley fever virus: Safety, immunogenicity and pathogenicity of MP-12 vaccine. Vaccine. 2017;35(4):655–662. doi: 10.1016/j.vaccine.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 39.Hunter P, Erasmus BJ, Vorster JH. Teratogenicity of a mutagenised Rift Valley fever virus (MVP 12) in sheep. Onderstepoort J Vet Res. 2002;69(1):95–98. [PubMed] [Google Scholar]
- 40.Antonis AF, Kortekaas J, Kant J, et al. Vertical transmission of rift valley fever virus without detectable maternal viremia. Vector Borne Zoonotic Dis. 13(8):601–606. doi: 10.1089/vbz.2012.1160. [DOI] [PubMed] [Google Scholar]
- 41.Coetzer JA, Barnard BJ. Hydrops amnii in sheep associated with hydranencephaly and arthrogryposis with wesselsbron disease and rift valley fever viruses as aetiological agents. Onderstepoort J Vet Res. 1977;44(2):119–126. [PubMed] [Google Scholar]
- 42.Kamal SA. Pathological studies on postvaccinal reactions of Rift Valley fever in goats. Virol J. 2009;6:94. doi: 10.1186/1743-422X-6-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Makoschey B, van Kilsdonk E, Hubers WR, et al. Rift Valley Fever Vaccine Virus Clone 13 Is Able to Cross the Ovine Placental Barrier Associated with Foetal Infections, Malformations, and Stillbirths. PLoS Negl Trop Dis. 2016;10(3):e0004550. doi: 10.1371/journal.pntd.0004550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lo MM, Mbao V, Sierra P, et al. Safety and immunogenicity of Onderstepoort Biological Products’ Rift Valley fever Clone 13 vaccine in sheep and goats under field conditions in Senegal. Onderstepoort J Vet Res. 2015;82(1):857. doi: 10.4102/ojvr.v82i1.857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Njenga MK, Njagi L, Thumbi SM, et al. Randomized controlled field trial to assess the immunogenicity and safety of rift valley fever clone 13 vaccine in livestock. PLoS Negl Trop Dis. 2015;9(3):e0003550. doi: 10.1371/journal.pntd.0003550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pittman PR, Liu CT, Cannon TL, et al. Immunogenicity of an inactivated Rift Valley fever vaccine in humans: a 12-year experience. Vaccine. 1999;18(1–2):181–189. doi: 10.1016/s0264-410x(99)00218-2. [DOI] [PubMed] [Google Scholar]
- 47.Rusnak JM, Gibbs P, Boudreau E, Clizbe DP, Pittman P. Immunogenicity and safety of an inactivated Rift Valley fever vaccine in a 19-year study. Vaccine. 2011;29(17):3222–3229. doi: 10.1016/j.vaccine.2011.02.037. [DOI] [PubMed] [Google Scholar]
- 48.U.S. Department of Health and Human Services FaDA. Guidance for industory: Toxicology grading scale for healthy adult and adolescent volunteers enrolled in preventive vaccine clinical trials. 2007 https://www.fda.gov/biologicsbloodvaccines/guidancecomplianceregulatoryinformation/guidances/vaccines/ucm074775.htm.
- 49.U.S. Department of Health and Human Services FaDA. Approval of Biological Products when Human Efficacy Studies Are Not Ethical or Feasible. Title 21 Code of Federal Regulations, Subpart H, Section 601.90.).
- 50.U.S. Department of Health and Human Services FaDA. Approval based on evidence of effectiveness from studies in animals. Title 21 Code of Federal Regulations, Subpart I, Section 314.610.).
- 51.Snoy PJ. Establishing efficacy of human products using animals: the US food and drug administration’s “animal rule”. Vet Pathol. 2010;47(5):774–778. doi: 10.1177/0300985810372506. [DOI] [PubMed] [Google Scholar]
- 52.Turell MJ, Rossi CA. Potential for mosquito transmission of attenuated strains of Rift Valley fever virus. Am J Trop Med Hyg. 1991;44(3):278–282. doi: 10.4269/ajtmh.1991.44.278. [DOI] [PubMed] [Google Scholar]
- 53.Turell MJ, Saluzzo JF, Tammariello RF, Smith JF. Generation and transmission of Rift Valley fever viral reassortants by the mosquito Culex pipiens. J Gen Virol. 1990;71( Pt 10):2307–2312. doi: 10.1099/0022-1317-71-10-2307. [DOI] [PubMed] [Google Scholar]
- 54.Briese T, Bird B, Kapoor V, Nichol ST, Lipkin WI. Batai and Ngari viruses: M segment reassortment and association with severe febrile disease outbreaks in East Africa. J Virol. 2006;80(11):5627–5630. doi: 10.1128/JVI.02448-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gerrard SR, Li L, Barrett AD, Nichol ST. Ngari virus is a Bunyamwera virus reassortant that can be associated with large outbreaks of hemorrhagic fever in Africa. J Virol. 2004;78(16):8922–8926. doi: 10.1128/JVI.78.16.8922-8926.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Briese T, Kapoor V, Lipkin WI. Natural M-segment reassortment in Potosi and Main Drain viruses: implications for the evolution of orthobunyaviruses. Arch Virol. 2007;152(12):2237–2247. doi: 10.1007/s00705-007-1069-z. [DOI] [PubMed] [Google Scholar]
- 57.Berthet N, Nakoune E, Gessain A, Manuguerra JC, Kazanji M. Complete Genome Characterization of the Arumowot Virus (Unclassified Phlebovirus) Isolated from Turdus libonyanus Birds in the Central African Republic. Vector Borne Zoonotic Dis. 2016;16(2):139–143. doi: 10.1089/vbz.2015.1830. [DOI] [PubMed] [Google Scholar]
- 58.Tesh RB. The genus Phlebovirus and its vectors. Annu Rev Entomol. 1988;33:169–181. doi: 10.1146/annurev.en.33.010188.001125. [DOI] [PubMed] [Google Scholar]
- 59.Traore-Lamizana M, Fontenille D, Diallo M, et al. Arbovirus surveillance from 1990 to 1995 in the Barkedji area (Ferlo) of Senegal, a possible natural focus of Rift Valley fever virus. J Med Entomol. 2001;38(4):480–492. doi: 10.1603/0022-2585-38.4.480. [DOI] [PubMed] [Google Scholar]
- 60.Kemp GE, Causey OR, Setzer HW, Moore DL. Isolation of viruses from wild mammals in West Africa, 1966–1970. J Wildl Dis. 1974;10(3):279–293. doi: 10.7589/0090-3558-10.3.279. [DOI] [PubMed] [Google Scholar]
- 61**.Ikegami T, Hill TE, Smith JK, et al. Rift Valley Fever Virus MP-12 Vaccine Is Fully Attenuated by a Combination of Partial Attenuations in the S, M, and L Segments. J Virol. 2015;89(14):7262–7276. doi: 10.1128/JVI.00135-15. Individual mutations of MP-12 strain was evaluated for attenuation in a mouse model. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Billecocq A, Gauliard N, Le May N, Elliott RM, Flick R, Bouloy M. RNA polymerase I-mediated expression of viral RNA for the rescue of infectious virulent and avirulent Rift Valley fever viruses. Virology. 2008;378(2):377–384. doi: 10.1016/j.virol.2008.05.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Saluzzo JF, Smith JF. Use of reassortant viruses to map attenuating and temperature-sensitive mutations of the Rift Valley fever virus MP-12 vaccine. Vaccine. 1990;8(4):369–375. doi: 10.1016/0264-410x(90)90096-5. [DOI] [PubMed] [Google Scholar]
- 64.Nishiyama S, Ikegami T. Temperature-sensitive mutations for live-attenuated Rift Valley fever vaccines: implications from other RNA viruses. Front Microbiol. 2015;6:787. doi: 10.3389/fmicb.2015.00787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ikegami T, Won S, Peters CJ, Makino S. Rescue of infectious rift valley fever virus entirely from cDNA, analysis of virus lacking the NSs gene, and expression of a foreign gene. J Virol. 2006;80(6):2933–2940. doi: 10.1128/JVI.80.6.2933-2940.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gerrard SR, Bird BH, Albarino CG, Nichol ST. The NSm proteins of Rift Valley fever virus are dispensable for maturation, replication and infection. Virology. 2007;359(2):459–465. doi: 10.1016/j.virol.2006.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Habjan M, Penski N, Spiegel M, Weber F. T7 RNA polymerase-dependent and -independent systems for cDNA-based rescue of Rift Valley fever virus. J Gen Virol. 2008;89(Pt 9):2157–2166. doi: 10.1099/vir.0.2008/002097-0. [DOI] [PubMed] [Google Scholar]
- 68.Won S, Ikegami T, Peters CJ, Makino S. NSm protein of Rift Valley fever virus suppresses virus-induced apoptosis. J Virol. 2007;81(24):13335–13345. doi: 10.1128/JVI.01238-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Crabtree MB, Kent Crockett RJ, Bird BH, et al. Infection and transmission of Rift Valley fever viruses lacking the NSs and/or NSm genes in mosquitoes: potential role for NSm in mosquito infection. PLoS Negl Trop Dis. 2012;6(5):e1639. doi: 10.1371/journal.pntd.0001639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kading RC, Crabtree MB, Bird BH, et al. Deletion of the NSm virulence gene of Rift Valley fever virus inhibits virus replication in and dissemination from the midgut of Aedes aegypti mosquitoes. PLoS Negl Trop Dis. 2014;8(2):e2670. doi: 10.1371/journal.pntd.0002670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kreher F, Tamietti C, Gommet C, et al. The Rift Valley fever accessory proteins NSm and P78/NSm-Gn are determinants of virus propagation in vertebrate and invertebrate hosts. Emerg Microbe Infect. 2014;3:e71. doi: 10.1038/emi.2014.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bird BH, Maartens LH, Campbell S, et al. Rift Valley Fever Virus Vaccine Lacking the NSs and NSm Genes Is Safe, Nonteratogenic, and Confers Protection from Viremia, Pyrexia, and Abortion following Challenge in Adult and Pregnant Sheep. J Virol. 2011;85(24):12901–12909. doi: 10.1128/JVI.06046-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Morrill JC, Laughlin RC, Lokugamage N, et al. Immunogenicity of a recombinant Rift Valley fever MP-12-NSm deletion vaccine candidate in calves. Vaccine. 2013;31(43):4988–4994. doi: 10.1016/j.vaccine.2013.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Weingartl HM, Nfon CK, Zhang S, et al. Efficacy of a recombinant Rift Valley fever virus MP-12 with NSm deletion as a vaccine candidate in sheep. Vaccine. 2014;32(20):2345–2349. doi: 10.1016/j.vaccine.2013.12.064. [DOI] [PubMed] [Google Scholar]
- 75.Nishiyama S, Slack OA, Lokugamage N, et al. Attenuation of pathogenic Rift Valley fever virus strain through the chimeric S-segment encoding sandfly fever phlebovirus NSs or a dominant-negative PKR. Virulence. 2016:1–11. doi: 10.1080/21505594.2016.1195528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bird BH, Albarino CG, Nichol ST. Rift Valley fever virus lacking NSm proteins retains high virulence in vivo and may provide a model of human delayed onset neurologic disease. Virology. 2007;362(1):10–15. doi: 10.1016/j.virol.2007.01.046. [DOI] [PubMed] [Google Scholar]
- 77.Lihoradova O, Ikegami T. Modifying the NSs gene to improve live-attenuated vaccine for Rift Valley fever. Expert Rev Vaccines. 2012;11(11):1283–1285. doi: 10.1586/erv.12.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ikegami T, Narayanan K, Won S, Kamitani W, Peters CJ, Makino S. Rift Valley fever virus NSs protein promotes post-transcriptional downregulation of protein kinase PKR and inhibits eIF2alpha phosphorylation. PLoS Pathog. 2009;5(2):e1000287. doi: 10.1371/journal.ppat.1000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Li S, Koromilas AE. Dominant negative function by an alternatively spliced form of the interferon-inducible protein kinase PKR. J Biol Chem. 2001;276(17):13881–13890. doi: 10.1074/jbc.M008140200. [DOI] [PubMed] [Google Scholar]
- 80.Indran SV, Lihoradova OA, Phoenix I, et al. Rift Valley fever virus MP-12 vaccine encoding Toscana virus NSs retains neuroinvasiveness in mice. J Gen Virol. 2013;94(Pt 7):1441–1450. doi: 10.1099/vir.0.051250-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Alhaj M. Safety and Efficacy Profile of Commercial Veterinary Vaccines against Rift Valley Fever: A Review Study. Journal of immunology research. 2016;2016:7346294. doi: 10.1155/2016/7346294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ahmed Kamal S. Observations on rift valley fever virus and vaccines in Egypt. Virol J. 2011;8:532. doi: 10.1186/1743-422X-8-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Barnard BJ, Botha MJ. An inactivated rift valley fever vaccine. J S Afr Vet Assoc. 1977;48(1):45–48. [PubMed] [Google Scholar]
- 84.Davies FG, Martin V. Recognizing Rift Valley fever. Food and Agriculture Organization of the United Nations; 2003. Prevention and control of Rift Valley fever; pp. 33–38. [Google Scholar]
- 85.Metras R, Baguelin M, Edmunds WJ, et al. Transmission potential of Rift Valley fever virus over the course of the 2010 epidemic in South Africa. Emerg Infect Dis. 19(6):916–924. doi: 10.3201/eid1906.121641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Al-Afaleq AI, Hussein MF. The status of Rift Valley fever in animals in Saudi Arabia: a mini review. Vector Borne Zoonotic Dis. 2011;11(12):1513–1520. doi: 10.1089/vbz.2010.0245. [DOI] [PubMed] [Google Scholar]
- 87.Kortekaas J, Oreshkova N, van Keulen L, et al. Comparative efficacy of two next-generation Rift Valley fever vaccines. Vaccine. 2014;32(39):4901–4908. doi: 10.1016/j.vaccine.2014.07.037. [DOI] [PubMed] [Google Scholar]
- 88.Kortekaas J, Oreshkova N, Cobos-Jimenez V, Vloet RP, Potgieter CA, Moormann RJ. Creation of a non-spreading Rift Valley fever virus. J Virol. 2011;85:12622–12630. doi: 10.1128/JVI.00841-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Warimwe GM, Gesharisha J, Carr BV, et al. Chimpanzee Adenovirus Vaccine Provides Multispecies Protection against Rift Valley Fever. Scientific reports. 2016;6:20617. doi: 10.1038/srep20617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Warimwe GM, Lorenzo G, Lopez-Gil E, et al. Immunogenicity and efficacy of a chimpanzee adenovirus-vectored Rift Valley fever vaccine in mice. Virol J. 2013;10:349. doi: 10.1186/1743-422X-10-349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dulal P, Wright D, Ashfield R, Hill AV, Charleston B, Warimwe GM. Potency of a thermostabilised chimpanzee adenovirus Rift Valley Fever vaccine in cattle. Vaccine. 2016;34(20):2296–2298. doi: 10.1016/j.vaccine.2016.03.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Faburay B, Lebedev M, McVey DS, et al. A glycoprotein subunit vaccine elicits a strong Rift Valley fever virus neutralizing antibody response in sheep. Vector Borne Zoonotic Dis. 2014;14(10):746–756. doi: 10.1089/vbz.2014.1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Faburay B, Wilson WC, Gaudreault NN, et al. A Recombinant Rift Valley Fever Virus Glycoprotein Subunit Vaccine Confers Full Protection against Rift Valley Fever Challenge in Sheep. Scientific reports. 2016;6:27719. doi: 10.1038/srep27719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Faburay B, Wilson W, McVey DS, et al. Rift valley Fever virus structural and nonstructural proteins: recombinant protein expression and immunoreactivity against antisera from sheep. Vector Borne Zoonotic Dis. 2013;13(9):619–629. doi: 10.1089/vbz.2012.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bird BH, Nichol ST. Breaking the chain: Rift Valley fever virus control via livestock vaccination. Curr Opin Virol. 2012;2(3):315–323. doi: 10.1016/j.coviro.2012.02.017. [DOI] [PubMed] [Google Scholar]
- 96.Gowen BB, Westover JB, Sefing EJ, et al. MP-12 virus containing the clone 13 deletion in the NSs gene prevents lethal disease when administered after Rift Valley fever virus infection in hamsters. Front Microbiol. 2015;6:651. doi: 10.3389/fmicb.2015.00651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gowen BB, Bailey KW, Scharton D, et al. Post-exposure vaccination with MP-12 lacking NSs protects mice against lethal Rift Valley fever virus challenge. Antiviral Res. 2013;98(2):135–143. doi: 10.1016/j.antiviral.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nishiyama S, Lokugamage N, Ikegami T. The L-, M- and S-segments of Rift Valley fever virus MP-12 vaccine independently contribute to a temperature-sensitive phenotype. J Virol. 2016;90(7):3735–37644. doi: 10.1128/JVI.02241-15. [DOI] [PMC free article] [PubMed] [Google Scholar]