Abstract
Context:
The concept of quality of life (QoL) is becoming an important measure of the impact of psychiatric disorders. It is natural that once patient achieves remission, QoL would improve, but very few studies are conducted under this phase. This study compares the differences in QoL in remitted patients with monotherapy and polypharmacy.
Aims:
The aim of this study is to compare the QoL between psychiatric patients in remission treated with monotherapy and polypharmacy.
Settings and Design:
It is a questionnaire based cross-sectional comparative study.
Materials and Methods:
This study included outpatients under remission who come for follow-up in psychiatric department. Semi-structured data collection form was used. Remission was confirmed using suitable scales, and QoL was assessed using the World Health Organization quality of life-Brief (WHOQOL-BREF) scale. Clinical Global Impression (CGI) and Global Assessment of Functioning (GAF) were applied to understand the overall improvement and functioning levels.
Results:
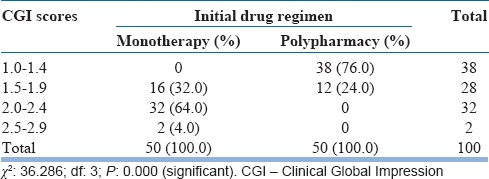
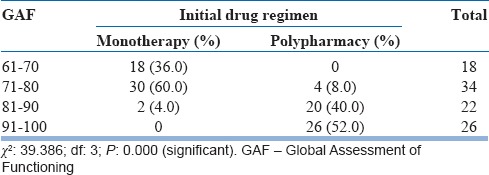
Out of the total 100 patients enrolled in the study, fifty patients were on monotherapy and fifty patients on polypharmacy. The cost of medication was comparatively high for polypharmacy (Rs. 3568.92 [±348.54]) than monotherapy (Rs. 1936.56 [±252.07]). The QoL in physical, psychological, and social domains was significantly high in patients on polypharmacy rather than monotherapy when assessed using the WHOQOL-BREF scale. Ninety-six percent of monotherapy patients had CGI scores between 1.5 and 2.4 while 74% of polypharmacy patients had scores between 1.0 and 1.5. Ninety-six percent of monotherapy patients had <80 GAF scores while 92% of polypharmacy patients had >80.
Conclusions:
Patients treated with polypharmacy had better QoL and also clinical improvement and functioning levels were superior.
Key words: Monotherapy, polypharmacy, psychiatry, quality of life, remission
INTRODUCTION
The concept of quality of life (QoL) is becoming an increasingly important measure of the impact of psychiatric disorders and is now recognized as useful in the health-care evaluation of patients with psychiatric disorders.[1] The concept of QoL has progressively shifted from a strictly sociological and objective prospective to a psychosocial prospective in which the individual's sense of well-being becomes a primary dimension of QoL.[2]
Psychotropic treatment regimens are generally divided into two broad categories: (1) single drug regimen, known as monotherapy (2) multiple drug regimens, known as polypharmacy. Monotherapy is the use of only one drug of a particular class consistently for achieving remission in a psychiatric disorder.
Polypharmacy is the use of two or more drugs of the same chemical class or with the same or similar pharmacologic actions for achieving remission.[3] Recent surveys have repeatedly documented the high frequency of polypharmacy in the treatment of seriously ill psychiatric patients.[4,5]
Most experts are in favor of psychopharmacological monotherapy[6] owing to its lesser adverse effects, reduced burden on patients in terms of cost,[7] drug load and better compliance, etc., even though it may cause an incomplete remission,[8] increased time duration, and tolerability problems.
Polypharmacy, on the other hand, has high efficacy and remission rates but causes lot of adverse effects[9] and increases the burden on patient. Remission is the elimination of ill symptoms and a return to premorbid levels of functioning.[10] It is well known with the support of many literatures that the QoL in symptomatic psychiatric patients is very low.[11,12] However, very few studies are conducted in patients under remission phase. It is natural that once patient achieves remission, his QoL would improve.[13] However, this study aims at comparing the differences in QoL in remitted patients with monotherapy and polypharmacy. It also aims at determining the cost associated with both the treatment regimens.
MATERIALS AND METHODS
Study design
The study involves the collection of data prospectively in psychiatry department of a tertiary care hospital. This is a questionnaire-based cross-sectional comparative study.
Study period
The study was conducted for a period of 6 months from November 2014 to April 2015.
Study subjects
The study includes hospital outpatients treated in psychiatry department. Patients who met the following criteria were enrolled in the study.
Study criteria
Inclusion criteria
All outpatients in psychiatric department who come for follow-up and under remission for not less than a period of 1 month and not more than a period of 6 months
Patients of age 18–60 years were included in the study.
Exclusion criteria
Patients with already established physical or intellectual impairments and disabilities
Patients with poor compliance and drug defaulters even though they are in remission
Patients with chronic morbidities or conditions which can independently alter QoL
Patients who have switched the treatment regimen from one to another were excluded from the study.
Study materials
Patient data collection form: It includes demographic details of the patients such as other people number, age, gender, diagnosis, and treatment chart
QoL assessment scales.
The World Health Organization Quality of Life-Brief scale
It comprises 26 items, which measure the following broad domains: physical health, psychological health, social relationships, and environment. The World Health Organization quality of life-Brief (WHOQOL-BREF) scale is a shorter version of the original instrument that may be more convenient for use in large research studies or clinical trials.[14]
Global Assessment of Functioning scale
The three areas examined by the Global Assessment of Functioning (GAF) are:
Psychological – obsessions, panic attacks, etc.
Social and interpersonal – maintaining friendships, personal hygiene, etc.
Occupational – work attendance, ability to follow directions, etc.
The GAF scoring system works on a numeric scale from 0 to 100, broken down into groups of ten. The higher the score, the better is functioning level. The most recent revision of the GAF scale as they appear in Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (text revision), released in 2000.[15]
Clinical Global Impression
The Clinical Global Impression (CGI) rating scales are widely used tool in psychiatry that measures of symptom severity, therapeutic response, and the efficacy of treatments. The CGI-improvement (CGI-I) scale is a seven-point scale used by a clinician to evaluate how much the patient's illness has improved or worsened relative to a baseline state at the beginning of the intervention and rated as: (1) very much improved; (2) much improved; (3) minimally improved; (4) no change; (5) minimally worse; (6) much worse; or (7) very much worse.[16]
Study procedure
Patients who satisfy above study criteria were included in the study. The signed informed consent form by the patient or by their representatives was taken. Annexure-VII
Patient's demographic details, medication history, therapeutic category, and socioeconomic status were collected and were documented in a suitably designed data collection form
-
Remission was ascertained under the guidance of psychiatrist by employing following scales:
The QoL was assessed by the WHO-BREF scale
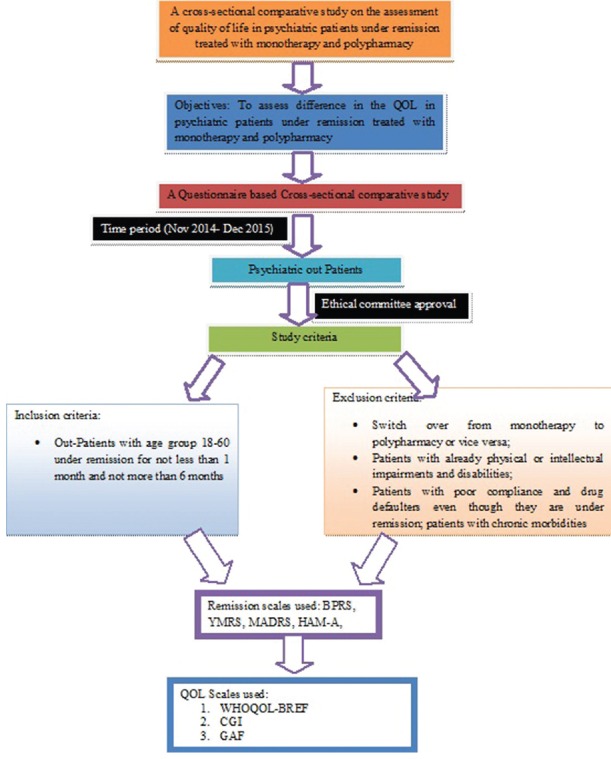
CGI and GAF were applied on the patient. Figure 1 summarizes methodological aspects of the study.
Figure 1.
Methodology flowchart
Statistical analysis
The data were entered and the results were analyzed using Statistical Package for Social Services 19.0 (IBM Corporation – http://www.spss.com/). Descriptive methods were applied to obtain the frequency. Kolmogorov–Smirnov test was applied to test the type of distribution of data. Independent samples t-test and Chi-square tests were applied to determine any significant difference between quantitative variables; Pearson correlation was applied between the scales to correlate them.
Sources of data
Medical records of the patients
Through direct interviewing of psychiatric patients
Opinion of the psychiatrist regarding the remission status of the patient.
RESULTS
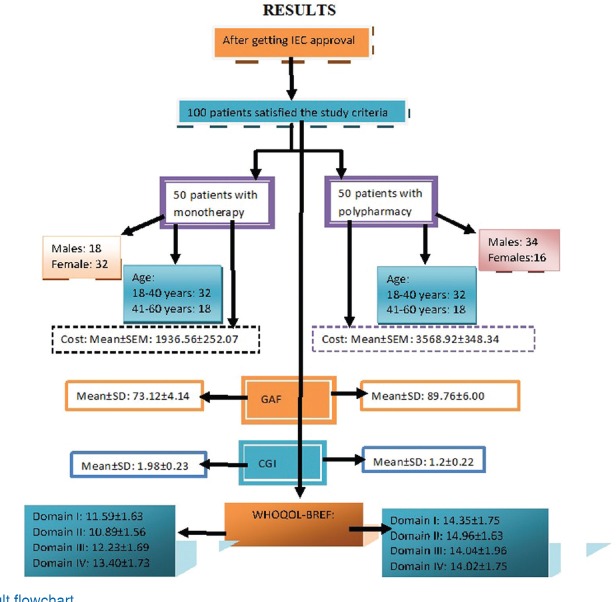
The data collected during the study period were analyzed for various parameters such as age, gender distribution of patients, marital status, socioeconomic status, diagnosis, and treatment given to patients. Figure 2 summarizes the results graphically. The information regarding the follow-up of the patients were obtained from the medication records, and QoL of these patients was assessed using the WHOQOL-BREF scale, GAF scale, and CGI scale. A total of 100 adult patients visited to psychiatric outpatient department (OPD) were enrolled for the study, among which 50 were on monotherapy and the other 50 were on polypharmacy.
Figure 2.
Result flowchart
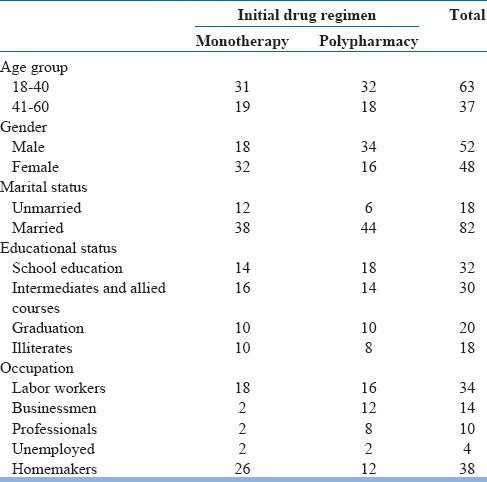
Demographic distribution of patients
The total patients were categorized into two groups based on the treatment as monotherapy and polypharmacy groups. Table 1 describes the sociodemographic profile of the study patients.
Table 1.
Distribution based on sociodemographic profile of the study patients
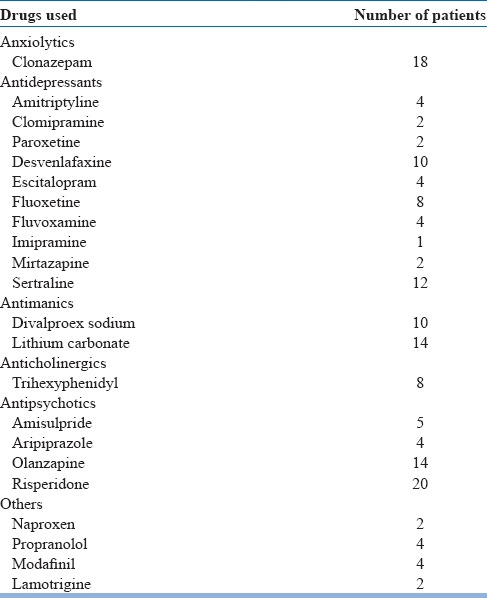
Distribution based on the treatment
The medications prescribed for monotherapy and polypharmacy patients on the sixth follow-up were taken into consideration for assessing the drug use. The medications prescribed among monotherapy and polypharmacy patients are described as below in Tables 2 and 3, respectively.
Table 2.
Distribution based on the medications prescribed for monotherapy

Table 3.
Distribution based on the medications prescribed for polypharmacy
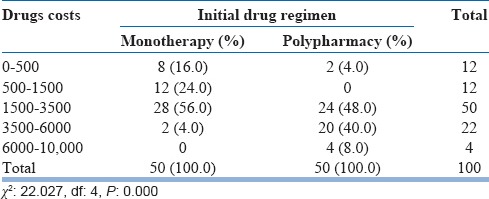
Distribution according to cost of medication
The cost of the medication was assessed for six follow-ups of the study period. Out of 50 patients on monotherapy, 28 patients have spent between Rs. 1500 and Rs. 3500, and 2 patients have spent between Rs. 3500 and Rs. 6000. Among 50 patients on polypharmacy, 24 patients have spent between Rs. 1500 and Rs. 3500, 20 patients have spent between Rs. 3500 and Rs. 6000, and 4 patients have spent above Rs. 6000. The mean ± standard error of the mean costs of the monotherapy patients was 1936.56 ± 252.07 and polypharmacy patients was 3568.92 ± 348.54. Chi-Square test reveals the significant relation between drug regimen and cost of the drugs. The detailed expenditure on medication is depicted in Table 4.
Table 4.
Distribution according to cost of medication
Assessment of quality of life based on the World Health Organization Quality of Life-Brief scale
The WHOQOL-BREF scale comprises 26 questions which measures the following broad domains: physical health, psychological health, social relationship, and environmental. By comparing the scores of monotherapy and polypharmacy, it was revealed that the mean ± standard deviation scores of physical, psychological, social, and environmental domains for monotherapy are 11.59 ± 1.63, 10.89 ± 1.56, 12.23 ± 1.69, and 13.40 ± 1.73, respectively, and for polypharmacy are 14.35 ± 1.75, 14.96 ± 1.63, 14.04 ± 1.96, and 14.02 ± 1.75, respectively, which reveals that the patients with polypharmacy are having good QoL when compared to patients with monotherapy. Independent t-test reveals that there is significant change between the QoL of monotherapy and polypharmacy patients. Comparisons of the WHOQOL-BREF SCALE mean scores of each domain for monotherapy and polypharmacy patients are given in Table 5 and are graphically depicted in Figure 3.
Table 5.
Mean values of the World Health Organization Quality of Life domain scores of monotherapy versus polypharmacy
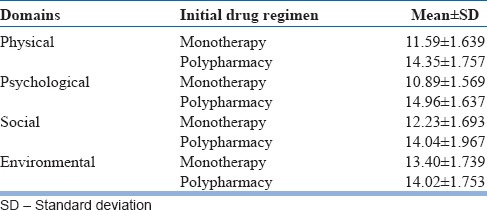
Figure 3.
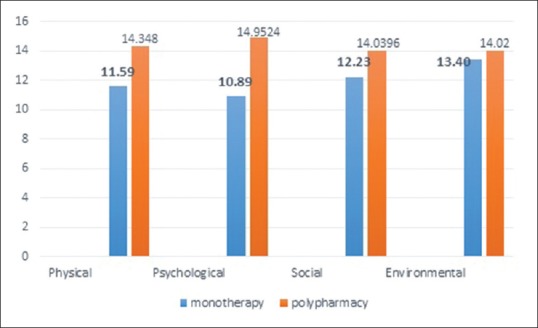
Comparison of mean values of the World Health Organization-quality of life domain scores of monotherapy versus polypharmacy
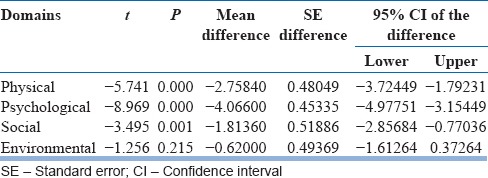
After determining parametric distribution of the sample using tests for normality, Independent t-test was used to assess whether there is a statistically significant difference between the means of above two groups. A significant difference was found in three domains, namely, physical, psychological, and social of polypharmacy group when compared with monotherapy. Independent t-test values are depicted in Table 6.
Table 6.
Independent t-test values of the World Health Organization Quality of Life domain scores of monotherapy versus polypharmacy
Assessment based on Clinical Global Impression
Among fifty patients of monotherapy, 16 patients scored between 1.5 and 1.9, 32 patients scored between 2.0 and 2.4 range, and 2 patients scored between 2.5 and 2.9.
Among fifty patients of polypharmacy, 38 patients scored between 1.0 and 1.4 and 12 patients scored between 1.5 and 1.9. The questionnaire concludes that patients on polypharmacy have better improvement in clinical status since the beginning of treatment. The results are shown in Table 7.
Table 7.
Clinical Global Impression scores of monotherapy versus polypharmacy
Assessment based on Global Assessment of Functioning
Among 50 patients on monotherapy, 18 patients scored between 61 and 70, 30 patients scored between 71 and 80, and 2 patients scored between 81 and 90.
Among 50 patients on polypharmacy, 4 patients scored between 71 and 80, 20 patients scored between 81 and 90, and 26 patients scored between 91 and 100. Thus, the scale reveals that patients on polypharmacy have superior functioning level in a wide range of activities compared to patients on monotherapy. The results are shown in Table 8.
Table 8.
Global Assessment of Functioning scores of monotherapy versus polypharmacy
Correlation between Clinical Global Impression and Global Assessment of Functioning
By applying the Pearson's correlation test, it was revealed that there exists a negative correlation between CGI and GAF; this indicates that as there is an increase in clinical improvement (lower CGI scores), the functioning rate will increase (higher GAF scores).
DISCUSSION
Only recently, the interest in the QoL has gained prominence in mental health practice with respect to other medical disciplines, such as oncology or cardiology, perhaps because the QoL measures were considered as tautological and largely overlapping with measures of psychopathology. Moreover, most of the recognized components of QoL represent the main areas of psychiatric intervention.
In addition, measures of QoL in psychiatric patients may be biased by some aspects of the disease, including impaired evaluation capacity or decreased expectations. Nowadays, QoL issues in relation to mental health care are especially relevant with regard to part of evaluation of treatment outcomes.[2]
In our study, out of the total 230 patients under came to Psychiatric Department of BMCH and RC, only 100 patients could satisfy the inclusion criteria and were enrolled into the study. Out of 100, 64 patients were from 18 to 40 years (64%) and 36 patients were from 41 to 60 years (36%). A study conducted by Moore et al. reveals that 40.2% of patients belong to the age group of 20–39 years,[22] and Deshmukh and Ismail work on psychotropic drugs use pattern in psychiatric OPD also reveals that 248 patients belong to the age group of 21–35 years[23] even Kousalya et al. show that 68 patients and 58 patients belong to the age group of 21–30 years and 31–40 years, respectively.[24] The age group attains significance in terms of productivity. QoL often affects productivity, and hence, assessment of QoL would be prudent even in remission phase at these age groups. Selecting treatment modes early in the course of treatment aimed at improving QoL becomes important.
Very few studies have been conducted for assessing the QoL in psychiatric patients based on monotherapy and polypharmacy. According to several observational studies conducted by Barbui et al., Faries et al., Gilmer et al., and Joukamaa et al., antipsychotic polypharmacy was associated with higher rates of extrapyramidal side effects (EPS) than antipsychotic monotherapy.[25,26,27,28] Further, antipsychotic polypharmacy was also reported to decrease adherence to treatment and to increase relapse and mortality compared to antipsychotic monotherapy. A multicenter cohort study conducted by Millier et al. in France assessed the QoL of schizophrenic patients, and the GAF scores were higher for monotherapy than polypharmacy (P = 0.20).[29] However, in our study, the GAF scores were higher for those patients on polypharmacy than monotherapy (P = 0.000). This difference from our study might be attributed due to the reason that all the medications, not just antipsychotics, are taken into consideration and antipsychotics, especially conventional antipsychotics have considerable EPS. In fact, our study did not have any patient on conventional antipsychotics and hence lesser likelihood of EPS [Tables 2 and 3]. Many medications used in polypharmacy actually may alleviate the side effects of each other, for example, risperidone-induced parkinsonism is alleviated by trihexyphenidyl as well as clonazepam and valproate. A meta-analysis by Correll et al. found that antipsychotic polypharmacy might be superior to monotherapy with respect to general measures of efficacy in certain clinical situations.[30] This is probably because in polypharmacy, lesser doses of multiple drugs may be utilized, and side effects which are usually higher at higher doses may not be manifest. The shortcomings of one drug such as insomnia may be alleviated by addition of another drug which considerably improves QoL and faster return to functioning and remission.
At the bottom line, the QoL assessed using the WHOQOL-BREF scale was found higher for patients on polypharmacy than monotherapy in all four domains. The CGI scores also have shown better therapeutic improvement for polypharmacy. The GAF scores have shown superior functioning level in polypharmacy patients.
Limitations
Lesser size of the sample
As there are many exclusion criteria to improve biases concerned to QoL, the generalizability to natural setting may be affected.
CONCLUSIONS
Patients treated with polypharmacy had better QoL and also clinical improvement and functioning levels were superior. But further, studies are needed to emphasize the present results.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aloba O, Fatoye O, Mapayi B, Akinsulore S. A review of quality of life studies in Nigerian patients with psychiatric disorders. Afr J Psychiatry (Johannesbg) 2013;16:333–7. doi: 10.4314/ajpsy.v16i5.44. [DOI] [PubMed] [Google Scholar]
- 2.Gigantesco A, Giuliani M. Quality of life in mental health services with a focus on psychiatric rehabilitation practice. Ann Ist Super Sanita. 2011;47:363–72. doi: 10.4415/ANN_11_04_07. [DOI] [PubMed] [Google Scholar]
- 3.Kingsbury SJ, Yi D, Simpson GM. Psychopharmacology: Rational and irrational polypharmacy. Psychiatr Serv. 2001;52:1033–6. doi: 10.1176/appi.ps.52.8.1033. [DOI] [PubMed] [Google Scholar]
- 4.Williams CL, Johnstone BM, Kesterson JG, Javor KA, Schmetzer AD. Evaluation of antipsychotic and concomitant medication use patterns in patients with schizophrenia. Med Care. 1999;37(4 Suppl Lilly):AS81–6. doi: 10.1097/00005650-199904001-00011. [DOI] [PubMed] [Google Scholar]
- 5.Frye MA, Ketter TA, Leverich GS, Huggins T, Lantz C, Denicoff KD, et al. The increasing use of polypharmacotherapy for refractory mood disorders: 22 years of study. J Clin Psychiatry. 2000;61:9–15. doi: 10.4088/jcp.v61n0104. [DOI] [PubMed] [Google Scholar]
- 6.Rittmannsberger H, Meise U, Schauflinger K, Horvath E, Donat H, Hinterhuber H. Polypharmacy in psychiatric treatment. Patterns of psychotropic drug use in Austrian psychiatric clinics. Eur Psychiatry. 1999;14:33–40. doi: 10.1016/s0924-9338(99)80713-5. [DOI] [PubMed] [Google Scholar]
- 7.Velligan DI, Carroll C, Lage MJ, Fairman K. Outcomes of medicaid beneficiaries with schizophrenia receiving clozapine only or antipsychotic combinations. Psychiatr Serv. 2015;66:127–33. doi: 10.1176/appi.ps.201300085. [DOI] [PubMed] [Google Scholar]
- 8.Robert M. Monotherapy vs. polypharmacy. Medscape Psychiatry. 2009:9. [Google Scholar]
- 9.Trumic E, Pranjic N, Begic L, Becic F, Asceric M. Idiosyncratic adverse reactions of most frequent drug combinations longterm use among hospitalized patients with polypharmacy. Med Arch. 2012;66:243–8. doi: 10.5455/medarh.2012.66.243-248. [DOI] [PubMed] [Google Scholar]
- 10.Kennedy S. Full remission: A return to normal functioning. J Psychiatry Neurosci. 2002;27:233–4. [PMC free article] [PubMed] [Google Scholar]
- 11.Pawlowska B, Frock FP, Potembska E, Domanski M, Lewczuk E. Changes in psychosocial functioning in patients with schizophrenia falling psychiatric rehabilitation. Psychiatr Pol. 2015;49:1191–202. doi: 10.12740/PP/36019. [DOI] [PubMed] [Google Scholar]
- 12.González N, Padierna A, Quintana JM, Aróstegui I, Horcajo MJ. Quality of life in patients with eating disorders. Gac Sanit. 2001;15:18–24. doi: 10.1016/s0213-9111(01)71513-0. [DOI] [PubMed] [Google Scholar]
- 13.Helldin L. The Importance of Remission in Treatment of Patients with Schizophrenia Spectrum Syndromes-Clinical Long-Term Investigation of Psychosis in Swedan [Dissertation] Karlstad University Studies. 2009 [Google Scholar]
- 14.The World Health Organization Quality of Life (WHOQOL)-BREF. Geneva: World Health Organization; 2004. [Last accessed on 2016 Apr 04]. Available from: http://www.who.int/substance_abuse/research_tools/whoqolbref/en/ [Google Scholar]
- 15.Global Assessment of Functioning (GAF) Scale. (From DSM-IV-TR, p. 34) [Last accessed on 2016 Apr 04]. Available from: https://www.u.osu.edu/files/2009/04/GAF-scale.pdf .
- 16.Guy W. ECDEU Assessment Manual for Psychopharmacology. Rockville, USA: Health, Education, and Welfare, Public Health Service; 1976. [Last accessed on 2016 Apr 04]. Available from: http://www.ncbi.nlm.nih.gov>PMC2880930 . [Google Scholar]
- 17.Overall JE, Gorham DR. Brief Psychiatric Rating Scale (BPRS) Psychol Rep. 1962;10:799–812. [Google Scholar]
- 18.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 19.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton Anxiety Rating Scale (HAM-A) [Last accessed on 2016 Apr 04]. Available from: http://www.dcf.psychiatry.ufl.edu>files>2011/15 .
- 21.Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale. Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–11. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 22.Moore S, Jaime LK, Maharajh H, Ramtahal I, Reid S, Ramsewak FS, et al. The prescribing of psychotropic drugs in mental health services in Trinidad. Rev Panam Salud Publica. 2002;12:207–14. doi: 10.1590/s1020-49892002000900010. [DOI] [PubMed] [Google Scholar]
- 23.Deshmukh SA, Ismail TS. Evaluation of psychotropic drugs use pattern among out patients attending psychiatry department at government medical college and hospital, Nagpur: A cross sectional study. Int J Pharma Bio Sci. 2012;3:428–36. [Google Scholar]
- 24.Kousalya K, Vasantha J, Ponnudurai R, Sumitkumar G, Ramalakshmi S, Saranya P, et al. Study on non-adherence and the effect of counseling in the pharmacological management of psychiatric patients. Int J Pharma Bio Sci. 2012;3:102–9. [Google Scholar]
- 25.Barbui C, Signoretti A, Mulè S, Boso M, Cipriani A. Does the addition of a second antipsychotic drug improve clozapine treatment? Schizophr Bull. 2009;35:458–68. doi: 10.1093/schbul/sbn030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Faries D, Ascher-Svanum H, Zhu B, Correll C, Kane J. Antipsychotic monotherapy and polypharmacy in the naturalistic treatment of schizophrenia with atypical antipsychotics. BMC Psychiatry. 2005;5:26. doi: 10.1186/1471-244X-5-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gilmer TP, Dolder CR, Lacro JP, Folsom DP, Lindamer L, Garcia P, et al. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161:692–9. doi: 10.1176/appi.ajp.161.4.692. [DOI] [PubMed] [Google Scholar]
- 28.Joukamaa M, Heliövaara M, Knekt P, Aromaa A, Raitasalo R, Lehtinen V. Schizophrenia, neuroleptic medication and mortality. Br J Psychiatry. 2006;188:122–7. doi: 10.1192/bjp.188.2.122. [DOI] [PubMed] [Google Scholar]
- 29.Millier A, Sarlon E, Azorin JM, Boyer L, Aballea S, Auquier P, et al. Relapse according to antipsychotic treatment in schizophrenic patients: A propensity-adjusted analysis. BMC Psychiatry. 2011;11:24. doi: 10.1186/1471-244X-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Correll CU, Rummel-Kluge C, Corves C, Kane JM, Leucht S. Antipsychotic combinations vs. monotherapy in schizophrenia: A meta-analysis of randomized controlled trials. Schizophr Bull. 2009;35:443–57. doi: 10.1093/schbul/sbn018. [DOI] [PMC free article] [PubMed] [Google Scholar]