Abstract
Objective
To increase the diagnostic sensitivity of standard MAG3 diuretic renal scans for ureteropelvic junction obstruction (UPJO) by exploring the utility of an alternative measurement P40, the percentage of maximal tracer counts present at 40 minutes.
Methods
Patients with strong clinical and anatomic evidence for UPJO may have a normal T1/2, making definitive diagnosis difficult. We reviewed the charts of 142 consecutive patients who underwent successful laparoscopic or robotic-assisted laparoscopic pyeloplasty for UPJO between 2005 and 2015. Both pre- and post-operative renal scan images were available for 37 symptomatic patients with primary unilateral UPJO and two kidneys. We defined P40 as the percentage of maximal tracer counts present at 40 minutes. We identified the upper limit of normal (97.5th percentile, +2SD) for P40 using the pre-operative renal scans from the unaffected kidney. We compared the sensitivity of P40 to T1/2 to identify symptomatic UPJO.
Results
In our cohort, 51% of symptomatic patients (n=19) had a normal T1/2 (Median 8.9 min; IQR: 7.5 min) and 49% (n=18) had an abnormal T1/2 (Median: 40 min; IQR: 0 min). No patients had an abnormal P40 on their unaffected kidney. All patients with an abnormal T1/2 also had an abnormal P40. P40 increased the sensitivity of the renal scan from 49% (n=18/37) to 73% (n=27/37) when compared to T1/2. The majority of patients (95%) demonstrated an improvement in P40 after pyeloplasty.
Conclusion
P40 markedly increases the sensitivity of a renal scan for diagnosing symptomatic UPJO and may be another valuable marker in addition to T1/2 to document functional improvement in drainage after pyeloplasty.
Keywords: UPJ obstruction, renal scans, pyeloplasty, radiology, renogram, pyeloplasty
Introduction
The diagnosis of clinically significant ureteropelvic junction obstruction (UPJO) requires a comprehensive work-up including a history, physical examination, functional imaging and an endoscopic evaluation.1 Diuretic renography can provide functional evidence to help identify patients who may benefit from surgical intervention and is a mainstay of the preoperative work-up. The traditional interpretation of renal scans depends on the calculation of the time to 50% tracer clearance after diuretic administration (T1/2).2
The optimal approach for both the interpretation of excretory renogram curves (i.e. visual analysis versus a quantitative index) and the timing of diuretic administration with various protocols (F-15, F0, F+20) remains controversial. The Consensus Committee of the Society of Radionuclides in Nephrourology recommends the F+20 protocol that prescribes furosemide injection at 20 minutes following tracer administration.3 A T1/2 of > 20 min is strongly suggestive of obstruction. Improvement in T1/2 to ≤ 20 min following pyeloplasty is deemed evidence for resolution of obstruction.2 However, a significant number of patients present preoperatively with compelling clinical symptoms and anatomic evidence of UPJO but equivocal T1/2 (>10 but <20min) and many continue to show a delayed T1/2 despite complete resolution of symptoms postoperatively.4
The use of T1/2 to assess obstruction has significant limitations, as this value captures only a small subset of the information stored in a renal scan drainage curve. In many cases, the T1/2 conflicts with a patient's clinical status and can confuse diagnosis and counseling. A substantial number of patients who have compelling clinical histories of flank pain and anatomic imaging consistent with UPJO have “non-obstructed” renal scans by T1/2.4 How to use this information in both the pre and postoperative settings remains controversial.
The morphology of 99mTc-MAG3 diuretic renogram drainage curves can vary between patients. We hypothesized that T1/2 may not be adequately conveying the information needed to assess obstruction in some cases, and we hypothesized that a measurement that does not depend on the maximal tracer being present at furosemide administration (e.g. large collecting systems continue to fill after furosemide) would identify additional patients with clinically relevant UPJO. We defined a new measurement which is the percent of maximal tracer that is still present at 40 minutes (P40). P40 can be easily abstracted from a standard MAG3 renogram (Figure 1).
Figure 1.
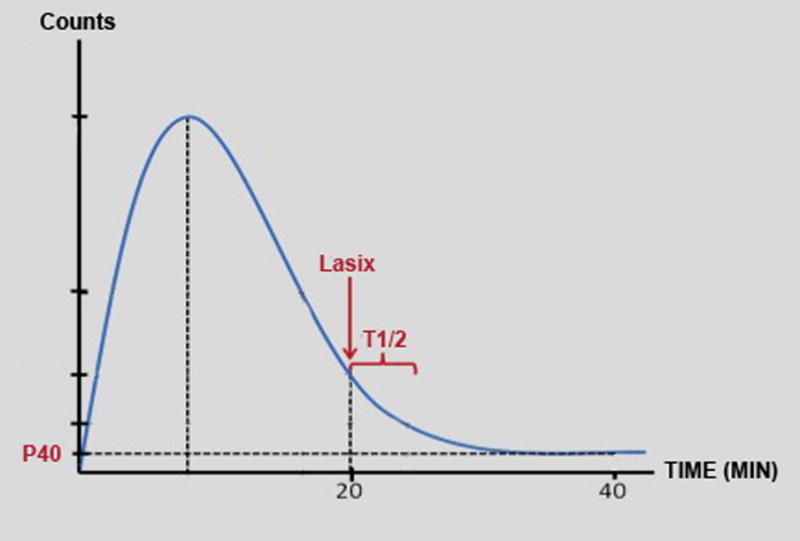
Representative renogram curve demonstrating the T1/2 and P40 value measurements.
Materials and Methods
Data collection and database use were approved by our institutional review board and compliant with the terms of the Health Insurance Portability and Accountability Act (HIPAA) with waiver of requirement for informed consent. We retrospectively reviewed records of 146 consecutive adult patients undergoing laparoscopic or robotic-assisted dismembered pyeloplasty for UPJO between 2005 and 2015 by one of two surgeons (REL and WAM).
Inclusion criteria were adult patients who had undergone successful pyeloplasty with two native kidneys and symptoms of unilateral obstruction who had undergone both pre-operative and post-operative 99mTc-MAG3 diuretic renography. Exclusion criteria included: (1) vesicoureteral reflux, (2) chronic kidney disease as defined by glomerular filtration rate (GFR) < 60 mL/min/1.73m2, (3) ectopic pelvic kidneys and (4) prior renal transplantation. Patients with secondary UPJO following previous endopyelotomy were not excluded from the analysis. In all cases, a standard 99mTc-MAG3 diuretic renal scan protocol was performed with recording for at least 40 minutes and IV furosemide (40 mg) was injected at the 20-minute time point in the majority of patients (78%, n=29). Patient demographics are listed in Table 1.
Table 1. Subject demographics.
| N = 37 | |
|---|---|
| Age (y) | 42 ± 16 |
| Gender | 12M/25F |
| Abnormal T1/2 | 18/37 (48.6%) |
| Abnormal P40 | 27/37 (73.0%) |
| Differential Renal Function <40% | 12/37 (32.4%) |
We identified two groups of patients who had undergone successful pyeloplasty for symptomatic UPJO and were followed with renal scans. Success in this setting was defined as (a) complete resolution of UPJO symptoms and (b) stable differential renal function on follow up renal scan. By comparing patients with preoperative T1/2 ≤ 20 min and > 20 min both before and after surgery, we sought to determine if P40 could identify more patients with clinically relevant UPJO than T1/2. We defined P40 as the percent of maximal tracer that is still present at 40 minutes (Figure 1).
We utilized the renogram data from the pre-operative contralateral unaffected kidney to determine an upper limit of normal for the P40 value (97.5th percentile, +2SD). We validated the reproducibility of this value by comparing the pre-surgical P40 values in the unaffected kidneys to the post-surgical P40 values in the unaffected kidneys. We compared the sensitivity of P40 to identify symptomatic UPJO to T1/2. We also investigated which patients had normalization of their abnormal P40 value after surgery. Statistical analysis utilizing paired t-test was performed with R version 3.2.3. P-values of <0.05 were considered statistically significant.
Results
Thirty-seven patients met inclusion criteria and were included for analysis (Table 1). 19 patients (51%) presented with a normal T1/2 (Median 8.9 min; IQR: 7.5 min) and 18 (49%) with an abnormal T1/2 (Median: 40 min; IQR: 0 min). Using data from the unaffected kidney, we determined that the upper-limit of normal (97.5th percentile) for P40 in our population was 0.244 (24.4%). We validated this range using values from the unaffected kidney on the post-operative renal scan and found that no unaffected kidneys had an abnormal P40 (Figure 2). Pre-operatively, 73% (n=27) of patients had an abnormal P40, whereas only 49% (n=18) had abnormal T1/2. All patients with an abnormal T1/2 also had an abnormal P40 (Figure 3).
Figure 2.
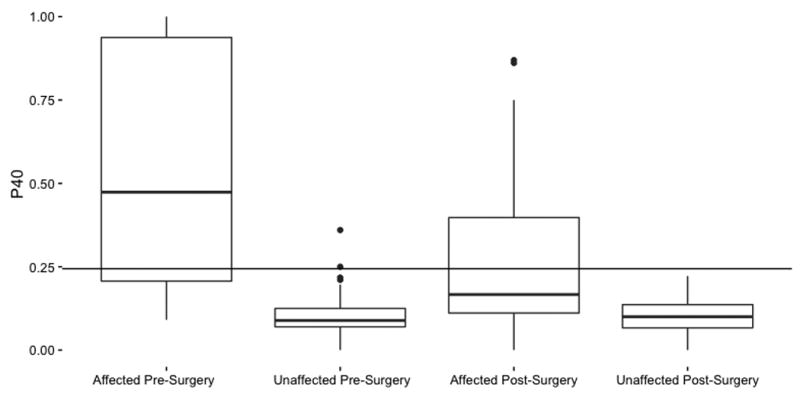
Pre- and post-surgical P40 values in the affected and unaffected kidneys. The horizontal line represents the upper limit of normal for P40 (97th percentile).
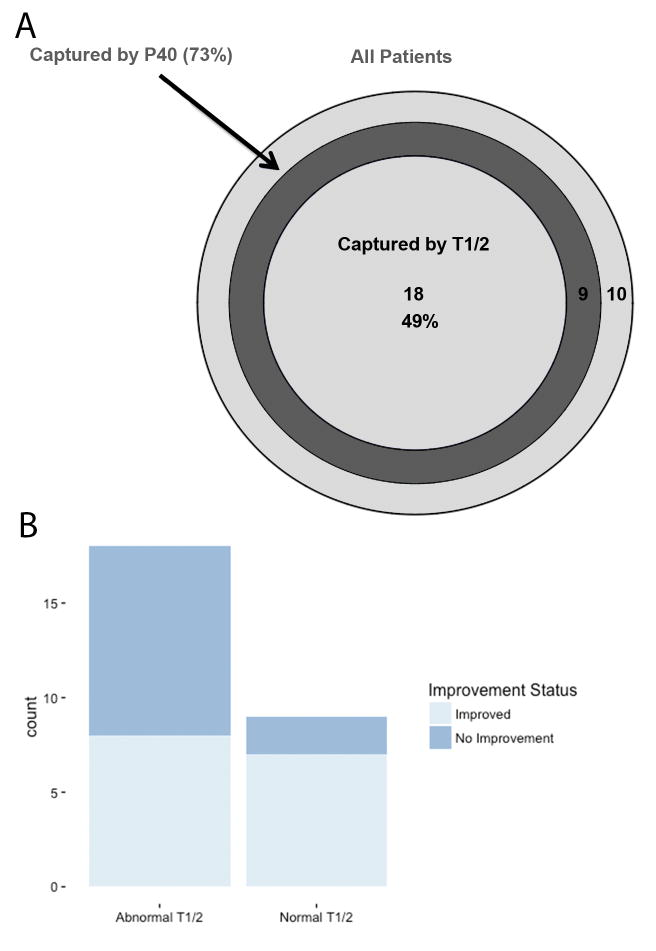
Figure 3.
(A) Euler diagram representing the patients that were identified as abnormal by T1/2 (innermost circle), patients that were abnormal by P40 (second circle, encompassing all abnormal T1/2 patients). The outer circle represents all patients included in the study, including those with normal P40 and T1/2 despite having clinically relevant UPJO. (B) The number of patients who had normalization of their P40 after surgery with a pre-operatively abnormal P40 and either a normal or abnormal T1/2.
In the diagnostically challenging subset of patients with symptomatic UPJO and a normal T1/2, P40 identified an additional 47% (n=9) of patients as abnormal, increasing the sensitivity of the renal scan from 49% to 73% (Figure 3; p = 0.032). All patients with an abnormal preoperative T1/2 showed an improvement in P40 after pyeloplasty (Median: 0.842 vs. 0.336, p<0.01). 84% (n=16) of patients with a normal preoperative T1/2 had a significantly lower P40 post-pyeloplasty (Median: 0.206 vs. 0.136, p<0.01) (Figure 2). Normalization of P40 occurred in 15 patients (56%) with a pre-operatively abnormal P40 value. Patients with a normal T1/2 and an abnormal P40 had a normalization rate of 78% (n=7/9; Figure 3). 12 (32%) patients had <40% differential renal function (DRF) in their affected kidney.
Comment
Here we demonstrate that P40 is a simple measurement requiring no additional testing that can substantially improve the sensitivity of a diuretic renogram to detect clinically significant renal obstruction even in the setting of a normal T1/2. The reduction in P40 following pyeloplasty with resolution of symptoms supports this measurement as an indicator of flow.
A renal scan is an important test to support surgical intervention in a suspected case of UPJO. While there are specific recommendations on how a renogram should be performed in suspected UPJO, we encountered significant institution-to-institution variation in practice.3, 5 Variation was frequently due to nonstandard performance of the test or inaccurate interpretation. Even when the renal scan is performed correctly, it may not indicate obstruction despite the presence of clinical symptoms and hydronephrosis on imaging. An equivocal renal scan in a patient with symptoms of UPJO presents the clinician with a dilemma regarding definitive management. There is conflicting data on patients with an equivocal renal scan.6 A recent study from Fontenot et al. reported less symptom relief in patients with a normal preoperative T1/2 but symptom relief was not recorded in a standardized manner. A second study from Ozayer et al. reported mutual symptom relief in patients after pyeloplasty regardless of any evidence of obstruction on the preoperative renal scan.7 In our cohort, a relatively high number of patients had a normal T1/2 that ultimately underwent pyeloplasty and achieved symptomatic relief. We confirmed the presence of UPJO with retrograde ureterograms for patients who had a compelling history for UPJO with a normal T1/2 hprior to pyeloplasty. In our own clinical practice, we consider relief of symptoms the single most important data point. While subjective improvement is difficult to capture numerically the patient's satisfaction will guide further management. Postoperative renal scans should also be utilized to document stable kidney function over time.
The F+20 diuretic protocol is the accepted initial technique of choice to differentiate between a non-obstructive dilatation and clinically relevant obstruction. The estimated reporting of ‘equivocal results’ in most series is 15%.7-9 In our series, 52% had equivocal T1/2 which may be attributed to testing at various independent radiological centers outside of our tertiary referral institution. We found a wide range of nonstandard protocols being used at these centers to perform MAG3 renal scans and great divergence in the interpretation of results on radiographic reports. For patients with an equivocal renal scan, the recourse may be to repeat the study with a standard diuretic protocol or to perform a Whitaker antegrade pressure flow study which requires more invasive intervention and is not readily available in all clinical settings.
Alternative renal scan measurements have been described such as the renal tissue tracer transit time (TTT) or the “single (or differential) kidney function <40%” in identifying kidneys that require surgical repair.10, 11 The TTT is conceptually somewhat similar to P40 and illustrates the tracer transit from parenchyma to the collecting system. TTT monitors kidneys with a large collecting system that show a delayed drainage pattern but no obstruction. Nevertheless it has the disadvantage of relying on a visual assessment of the actual scan images and appears to be less reproducible than the calculated tracer clearance and less objective than the quantifiable P40 clearance parameter. Our series did not identify differential renal function (DRF) to be indicative of outcome. While DRF did differ between the affected and control kidneys pre-operatively, it did not improve significantly following surgery. This pattern was consistent throughout both groups and may be related to irreversible kidney damage from long term UPJO.
P40 is a novel variable that can be easily extracted from the diuretic curve and is defined as the percent uptake of tracer at 40 minutes compared to maximum tracer uptake. On assessment of the renogram curves, there are several characteristics of P40 that lend credibility to its potential utility. The longer time interval provides a more accurate measurement of slower filling and draining collecting systems. By measuring tracer counts at 40 minutes, large collecting systems are given time to clear the tracer in the absence of an obstructive component. Furthermore, taking the value at maximum tracer uptake instead of tracer at time of furosemide exclusively covers the entire excretion phase, which is crucial for drainage assessment. To start at the time of furosemide injection may include the tail end of tracer uptake or miss the initial part of the excretion phase on the descending curve, which may not incorporate the true excretory urodynamics of the upper tracts.
The strength of P40 is that it identified all patients who would have been diagnosed with a significant obstruction by T1/2, and captures additional patients that T1/2 missed. Furthermore, the majority of patients with a normal T1/2 but an abnormal P40 had complete normalization of their P40 value after surgery, which strongly supports the capability of P40 to identify clinically relevant obstruction. Future prospective studies will be required to validate P40 for the diagnosis of UPJO and to determine if P40 should supplant T1/2 as the diagnostic measurement of choice or if it should be used as an adjunct in those patients with symptoms of UPJO and an equivocal T1/2.
There are several key strengths and weaknesses of our study that merit discussion. One of the strengths was our ability to make comparisons between pre and postoperative P40 and T1/2 values, and to compare these changes to an internal control, the unaffected contralateral kidney. In most published studies, the preoperative scans were used solely for deduction and analysis of diagnosis without taking into consideration postoperative outcomes. This is important as there are cases of persistently prolonged T1/2 on post-operative renal scans that could represent a ‘reservoir effect’ with increase pelvis capacity as compared to a true secondary UPJO. P40 may potentially address this. In this study, all included patients were determined to have clinically significant UPJO that resolved after surgery. The number of patients studied was limited by the availability of both pre and postsurgical renograms of suitable quality and standard protocol in the majority of patients screened. Our practice is a tertiary referral center for many secondary UPJO cases. Because of this, most preoperative imaging studies were done at outside institutions which often did not adhere to the standard renal scan protocol. Lastly, this study is retrospective in nature and as a result our findings will need to be validated in a prospective cohort.
Conclusions
P40 markedly increases the sensitivity of a renal scan for the diagnosis of a clinically significant UPJO and may be particularly useful in diagnosing the patient with symptoms of UPJO despite an equivocal T1/2.
Footnotes
The authors declare no conflict of interest
References
- 1.Khan F, Ahmed K, Lee N, Challacombe B, Khan MS, Dasgupta P. Management of ureteropelvic junction obstruction in adults. Nature reviews Urology. 2014;11:629–638. doi: 10.1038/nrurol.2014.240. [DOI] [PubMed] [Google Scholar]
- 2.O'Reilly PH, Lawson RS, Shields RA, Testa HJ. Idiopathic hydronephrosis--the diuresis renogram: a new non-invasive method of assessing equivocal pelvioureteral junction obstruction. The Journal of urology. 1979;121:153–155. doi: 10.1016/s0022-5347(17)56703-8. [DOI] [PubMed] [Google Scholar]
- 3.O'Reilly PH, Consensus Committee of the Society of Radionuclides in N Standardization of the renogram technique for investigating the dilated upper urinary tract and assessing the results of surgery. BJU international. 2003;91:239–243. doi: 10.1046/j.1464-410x.2003.04050.x. [DOI] [PubMed] [Google Scholar]
- 4.Lee D, Link RE. Recurrent symptoms following pyeloplasty with a normal endoscopic evaluation: assessment and outcomes of a challenging patient cohort. Urology. 2014;84:227–231. doi: 10.1016/j.urology.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 5.Cosgriff PS, Lawson RS, Nimmon CC. Towards standardization in gamma camera renography. Nuclear medicine communications. 1992;13:580–585. [PubMed] [Google Scholar]
- 6.Fontenot PA, Jr, Capoccia TR, Wilson B, Arthur A, Duchene DA. Robotic-assisted Laparoscopic Pyeloplasty: Analysis of Symptomatic Patients With Equivocal Renal Scans. Urology. 2016 doi: 10.1016/j.urology.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 7.Ozayar A, Friedlander JI, Shakir NA, Gahan JC, Cadeddu JA, Morgan MS. Equivocal ureteropelvic junction obstruction on diuretic renogram--should minimally invasive pyeloplasty be offered to symptomatic patients? The Journal of urology. 2015;193:1278–1282. doi: 10.1016/j.juro.2014.10.100. [DOI] [PubMed] [Google Scholar]
- 8.Hay AM, Norman WJ, Rice ML, Steventon RD. A comparison between diuresis renography and the Whitaker test in 64 kidneys. British journal of urology. 1984;56:561–564. doi: 10.1111/j.1464-410x.1984.tb06116.x. [DOI] [PubMed] [Google Scholar]
- 9.Koff SA, Thrall JH, Keyes JW., Jr Diuretic radionuclide urography: a non-invasive method for evaluating nephroureteral dilatation. The Journal of urology. 1979;122:451–454. doi: 10.1016/s0022-5347(17)56458-7. [DOI] [PubMed] [Google Scholar]
- 10.Schlotmann A, Clorius JH, Clorius SN. Diuretic renography in hydronephrosis: renal tissue tracer transit predicts functional course and thereby need for surgery. European journal of nuclear medicine and molecular imaging. 2009;36:1665–1673. doi: 10.1007/s00259-009-1138-5. [DOI] [PubMed] [Google Scholar]
- 11.Liu M, Fu Z, Li Q, et al. Delayed renal tissue tracer transit in Tc-99m-DTPA renography correlates with postoperative renal function improvement in UPJO patients. Nuclear medicine communications. 2015;36:833–838. doi: 10.1097/MNM.0000000000000332. [DOI] [PubMed] [Google Scholar]