Abstract
Background
After steady decline since the 1990s, tuberculosis (TB) incidence in New York City (NYC) and the United States (US) has flattened. The reasons for this trend and the implications for the future trajectory of TB in the US remain unclear.
Methods
We developed a compartmental model of TB in NYC, parameterized with detailed epidemiological data. We ran the model under five alternative scenarios representing different explanations for recent declines in TB incidence. We evaluated each scenario’s relative likelihood by comparing its output to available data. We used the most likely scenarios to explore drivers of TB incidence and predict future trajectories of the TB epidemic in NYC.
Findings
Demographic changes and declining TB transmission alone were insufficient to explain recent trends in NYC TB incidence. Only scenarios that assumed contemporary changes in TB dynamics among the foreign-born – a declining rate of reactivation or a decrease in imported subclinical TB – could accurately describe the trajectory of TB incidence since 2007. In those scenarios, the projected decline in TB incidence from 2015 to 2025 varied from minimal [2·0%/year (95% credible interval 0·4–3·5%)] to similar to 2005 to 2009 trends [4·4%/year (2·5–6·4%)]. The primary factor differentiating optimistic from pessimistic projections was the degree to which improvements in TB dynamics among the foreign-born continued into the coming decade.
Interpretation
Further progress against TB in NYC requires additional focus on the foreign-born population. Absent additional intervention in this group, TB incidence may not decline further.
Keywords: Tuberculosis, Mathematical Model, Health Resources, United States, New York City, Humans
INTRODUCTION
After steadily declining since the 1990s, the incidence of tuberculosis (TB) in the United States (US) remained relatively flat from 2013 – 2015.1 This plateau was presaged by a slowing decline of TB incidence in New York City (NYC) since 2010.2 New York City has long been an important locus of TB in the US,3 and changes in NYC TB incidence often anticipate national trends.4 The reasons for the abrupt plateauing of TB incidence in NYC and the US more broadly and whether TB incidence can decline further in the future remain unclear.
As incidence has declined, TB budgets have contracted,5 and limited resources must be allocated efficiently to continue progress toward TB elimination. Declines in TB over the last half of the 20th century have been driven by antibiotic chemotherapy, decreasing TB transmission,6 lower prevalence of latent TB infection (LTBI) among younger generations,7 and an aggressive public health response since the 1980s surge of TB.4 If these are the key drivers of recent declines as well, then the downward trajectory of TB incidence might be expected to resume. If, however, the more recent declines in TB incidence reflect processes that will not inevitably continue, then additional steps, such as increased screening for and treatment of LTBI,8 may be necessary to resume seemingly stalled progress in the ongoing fight against TB.
Mathematical models can be useful for understanding the dynamics of infectious disease epidemics9, 10 and could be applied to forecast the trajectory of the TB epidemic in the US. There are relatively few models of TB in the US10 or other low-burden settings,11, 12 and the data informing these models to date have been insufficient to address detailed mechanistic questions. NYC collects detailed clinical and epidemiological data on TB dynamics (including LTBI prevalence estimates13 and routine genotyping14), demography, and immigration. The quality and breadth of this information offers a unique opportunity to examine in detail the effects on TB incidence of changing demographics and immigration. We therefore incorporated these data into a model designed to explore the major drivers of the recent flattening of TB incidence in NYC and to project the future trajectory of the TB epidemic in the absence of any additional intervention.
METHODS
Model Description
We developed a compartmental transmission model of TB in NYC stratified by age and nativity: US-born (born within the US or a US territory) or foreign-born (see Supplement Figure S1). Compartmental models are widely used in TB modeling as their computational efficiency allows for running many simulations; our model uses compartments similar to other studies10 and is stratified by age. Susceptible populations in our model become infected with TB at a rate proportional to the prevalence of active TB; upon infection, people are categorized as having ‘recently acquired’ LTBI and experience a specified rate of progression to active TB. As time passes since the initial infection, LTBI advances through stages of declining progression rates, but the rate of progression (“reactivation”) never falls to zero. Active TB is identified and treated at a given rate; people with active TB also experience competing rates of spontaneous resolution and death. Reinfection among people with LTBI or those who have completed treatment is allowed, but their rate of reinfection is reduced compared to never-infected individuals, reflecting partial immunity to reinfection. We chose our age strata to match strata for which mortality rates and TB incidence have been recorded by the NYC Department of Health and Mental Hygiene (DOHMH). We initiated the model in 1950 and ran simulations through 2025. We describe the full model in detail in the supplement.
Model Calibration
We sought to capture the state of TB in 2015 and the trends in TB incidence leading up to 2015. Because our model is only an approximation of reality and depends on a number of parameters that are not known exactly, we used a Bayesian approach (as in prior modeling studies) to handle uncertainty.15 In this approach, we ran 20,000 simulations, each with slightly different model parameters chosen from ranges of likely values. We then weighted the simulations according to how well they corresponded to TB incidence from 2010 to 2015 using a likelihood function. This calibration yielded estimates of future TB incidence and reductions in incidence with 95% credible intervals – intervals within which a prediction will fall with 95% certainty, assuming the model appropriately reflects TB transmission in NYC.
We estimated model parameters from three sources: (1) epidemiological data from the NYC DOHMH, (2) the scientific literature, and (3) exploratory simulations with the model (see Supplement). To reflect uncertainty in the model parameters that were not directly estimated from NYC data, for each simulation we sampled parameters from uniform distributions over the ranges of possible values given in Table S1 in the Supplement. For parameters with minimal supporting data available, we selected median values consistent with the published literature or based on initial simulations and sampled from a range of possible values around that median. We incorporated uncertainty about LTBI prevalence in incoming immigrants and in the NYC population in 1950 by allowing them to vary randomly from 0.5 to 1.5 times our estimated values.
We designed our likelihood function to match the case notification of TB among US-born and foreign-born NYC residents in both 2010 and 2015. The likelihood weighted each simulation according to a product binomial likelihood that multiplied the probability of observing the reported number of TB cases in 2010 and 2015 separately among US-born (all ages) and foreign-born (all ages) individuals, given the simulation results. Since LTBI prevalence reflects TB dynamics from the preceding 50–60 years, we excluded those simulations that projected a decline in overall TB incidence from 1950 to 1960 that was more than 50% above or below the estimated historical decline. Similarly, among simulations which sought to reproduce the increase in TB incidence in the 1980s–1990s (see ‘Scenarios’ below), we excluded those that projected an overall TB incidence in 1992 more than 50% above or below the observed TB incidence at that time; this ensured that simulations reflected the 1980s–1990s trend to an approximate (±50%) degree, since a simulation could match well in 2015 while matching poorly in 1992. We fit the model to TB notifications as a proxy for underlying incidence, as TB is a reportable disease, and it is widely felt that most epidemiologically relevant TB cases in the United States are notified.
Model Outcomes and Scenarios
Our research objectives were to explore potential mechanisms underlying the recent declines in TB in NYC and to describe the reasonable range of future epidemic trajectories. Our primary outcome was the projected rate of decline in TB incidence from 2015 to 2025.
To explore different possible mechanisms for recent TB trends in NYC, we generated simulations under five different sets of assumptions, detailed in Table 1. We evaluated whether trends in TB incidence in NYC from 2010 to 2015 could be replicated under each set of assumptions, and how each assumption affected projections of future TB incidence. These five scenarios differed in allowing rates of progression of LTBI to decline with time since infection (beyond five years), attempting to recapitulate the increase in TB incidence in the 1980s and 1990s, allowing rates of LTBI progression to differ between US-born and foreign-born populations, or allowing for a reduction in the amount of subclinical TB in incoming immigrants (subclinical TB refers to active TB after it can be transmitted and diagnosed microbiologically but before it would be diagnosed based on symptoms16). All five scenarios allowed transmission rates to fall over the 65-year period (see Supplement for details) and assumed that prevalence of LTBI among incoming immigrants is constant.
Table 1.
Five Scenarios under which simulations were run
| Scenario | Brief Description | Comments |
|---|---|---|
| Baseline | Demographic changes only | Constant rate of LTBI reactivation beyond five years after infection, no change in TB dynamics in 1980s – 1990s |
| Declining Progression | Allows declining rate of LTBI reactivation | As in Baseline, but allows for linear decline in the rate of LTBI reactivation with time since infection |
| 1980s Increase | Increased TB incidence from 1984 to 1992 | As in Declining Progression, but allows for higher rates of transmission and reactivation as observed from 1984 to 1992, without specifying a specific mechanism (e.g., HIV or worsening TB control infrastructure) |
| Differential Progression | Different reactivation rates in US-born versus foreign-born | As in 1980s Increase, but allows for different rates of progression from LTBI to active TB in US-born and foreign born individuals, as well as allowing the rate of progression in foreign-born individuals with LTBI to decline by 1·5 to 5·25% per year after 2007, without specifying a specific mechanism (e.g., due to improved nutritional/immune status).* |
| Reduced Importation | Reduced importation of subclinical TB from 2007 to 2012 | As in the 1980s Increase scenario, but models a decrease in imported subclinical TB without specifying a specific mechanism (e.g. changing patterns of immigration or use of TB culture rather than sputum smear microscopy to screen some foreign-born persons seeking permanent residence in the US prior to entry17). We represent this decrease as a linear reduction in the risk of incident active TB among immigrants in their first year after arrival; we assume that in 2007 immigrants have a normal risk, but by 2012 (and after) have that first-year risk cut in half. |
Rates of decline were selected based on preliminary simulations. Our primary analysis of this scenario assumed that LTBI progression rates among the foreign-born continued to decline through 2025. As it is not clear that such a decline would continue year after year, we conducted a secondary analysis which assumed LTBI progression rates did not decline further after 2015. Further details are provided in the Supplement.
We note that our scenarios (particularly the Differential Progression and Reduced Importation scenarios) are broad paradigms that highlight general mechanisms by which TB incidence may be changing.
Model Analyses and Sensitivity Analyses
We compared the five scenarios based on their fit to the observed trends qualitatively by plotting model projections and quantitatively using Bayes factors: the ratio of the overall likelihood of one model versus another – the greater the ratio, the more the data (TB incidence in 2010 and 2015) support one scenario over the other.18 In addition, we examined the ability of simulations in each scenario to recapitulate the age distribution in the population, fraction of incident TB due to recent (within 2 years) transmission (estimated using the proportion of cases clustered by IS6110 restriction fragment length polymorphism and spoligotyping14), age distribution of active cases, and age distribution of LTBI in both US-born and foreign-born populations.
We analyzed the sensitivity of our primary outcome to each individual parameter value, adjusting for all other parameters in the model, by calculating partial rank correlation coefficients (PRCCs) between the parameter value and the projected decline in TB from 2015 to 2025: the correlation between the ranked value of the outcome and the ranked value of each individual parameter, adjusted for all other parameters. We also compared the primary outcome in simulations with the parameter values in the highest quintile to the outcome in simulations with parameter values in the lowest quintile for each parameter. We conducted sensitivity analyses to determine how much the specification of the likelihood function and prior distributions for model parameters influenced our primary outcome.
Software
Simulations were run using the R language, version 3.3.1, and the deSolve package.
Role of the Funding Source
No external funding was used for this study. The corresponding author had full access to all of the data and the final responsibility to submit for publication.
RESULTS
Model Selection
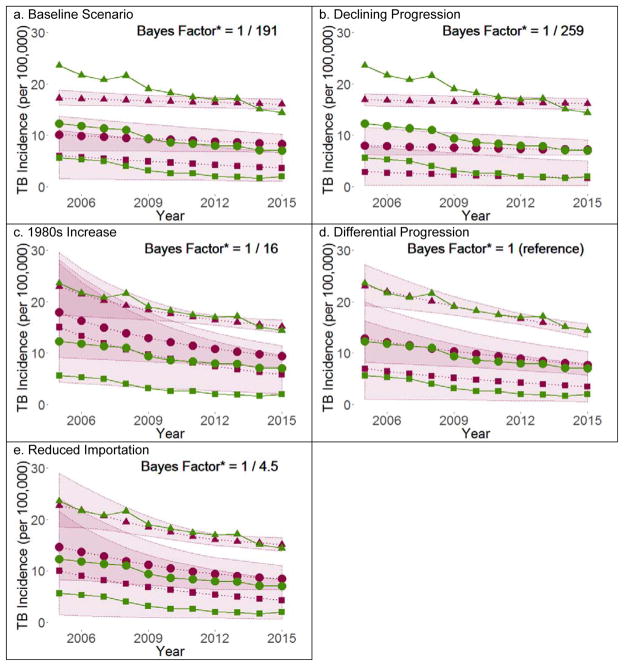
We determined which model assumptions were necessary to replicate recent trends in TB incidence. Scenarios resting on demographic changes and historical changes in transmission alone (the Baseline, Declining Progression, and 1980s Increase scenarios) fit the data poorly (Figure 1). To accurately replicate the recent decline in TB incidence in NYC, it was important to incorporate a more recent (since 2007) change in the dynamics of TB within the foreign-born population; examples of such changes included ongoing declines in LTBI progression among foreign-born individuals (the Differential Progression scenario) or more recent reductions in imported subclinical TB in this population (the Reduced Importation scenario). The data did not strongly support one or the other of these mechanisms; rather, a recent change in the dynamics of TB among the foreign-born was required to replicate the observed data, regardless of the mechanism of that change. Our subsequent analyses focus on the Differential Progression and Reduced Importation scenarios.
Figure 1.
Estimated versus Actual TB Incidence in US-born, Foreign-born, and Total NYC Population under Five Scenarios
Mean model estimates (points) of TB incidence with 95% credible intervals (ribbon) shown in purple, case notification rates (points) shown in green. Triangles denote the foreign-born, squares denote the US-born, and circles denote the total population. *Bayes Factors are with respect the Differential Progression scenario. A Bayes factor is the ratio of the overall likelihood of one scenario versus another – the greater the ratio, the more the data (TB incidence in 2010 and 2015) support one scenario over the other. A Bayes factor of 1/10 or less indicates strong evidence in favor of the Differential Progression scenario.18
Model Estimates and Projections
Both the Differential Progression and the Reduced Importation scenarios estimated that slight declines in the transmission rate (3·3% and 3·8% relative reduction per year, respectively) underpinned part of the recent decline in TB incidence for US- and foreign-born populations. The Differential Progression scenario suggested that, if the recent decline in TB incidence among the foreign-born was due to a decrease in foreign-born reactivation rates starting in 2007, the rate of that decline was 2·8% per year (95% credible interval 1·5–4·1% per year).
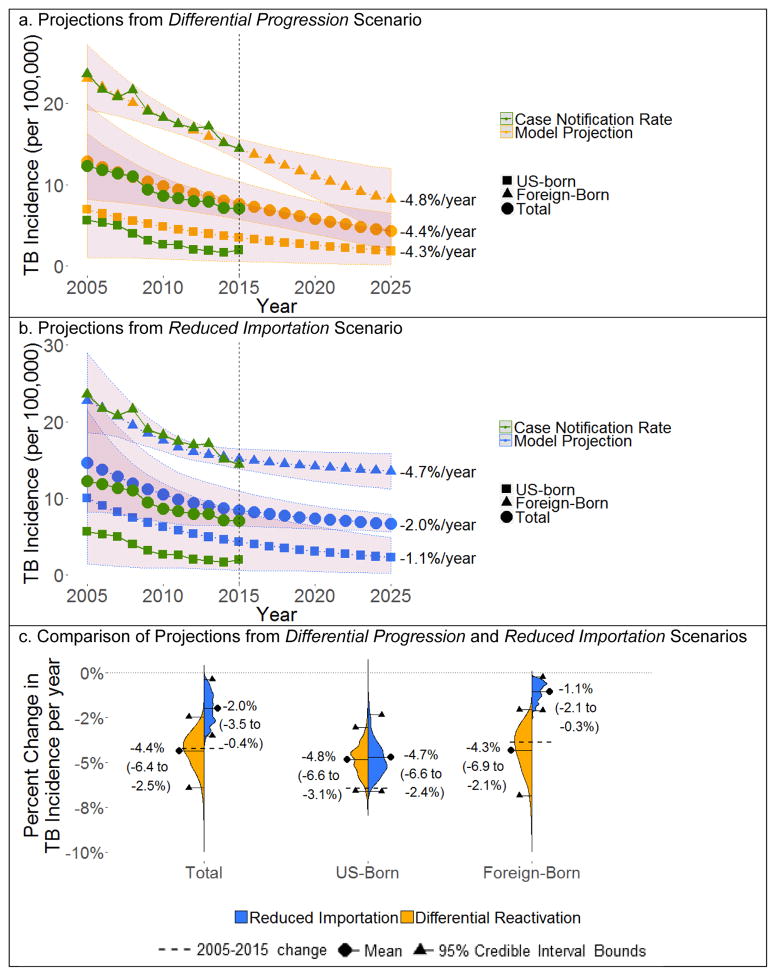
Although both of these scenarios fit historical data well and provided a mechanism for recent declines in incidence among the foreign-born population, the two scenarios differed markedly in projections of TB over the next decade due to their different assumptions about whether the modeled mechanisms can be maintained (Figure 2). The Reduced Importation scenario, in which imported subclinical TB was not reduced further after 2012, projected a flattening of TB incidence beyond 2015, with an estimated decline of only 2·0% per year from 2015 to 2025 (95% credible interval 0·4–3·5%). In contrast, the Differential Progression scenario, which assumed that LTBI progression rates among the foreign-born would continue to fall in the coming decade, projected ongoing declines in TB incidence similar to those over the last decade – 4·4% per year (95% credible interval 2·5–6·4%). When we instead assumed that rates of LTBI progression among the foreign-born remained constant beyond 2015, the decline in TB incidence over the coming decade flattened to 1·3% per year (95% credible interval 0·2–2·6%).
Figure 2.
Estimated Change in Total TB Incidence from 2015 to 2025
bProjected TB incidence for Total, US-born, and Foreign-born in NYC under the (a) Differential Progression and (b) Reduced Importation scenarios. (c) Violin plots comparing projected distributions of the yearly decline in TB incidence from 2015 to 2025 in total, US-born, and foreign-born populations. Circles denote mean estimates, triangles denote 95% credible intervals bounds. Dashed lines indicate corresponding change in case notification rate from 2005 to 2015.
Sensitivity Analyses
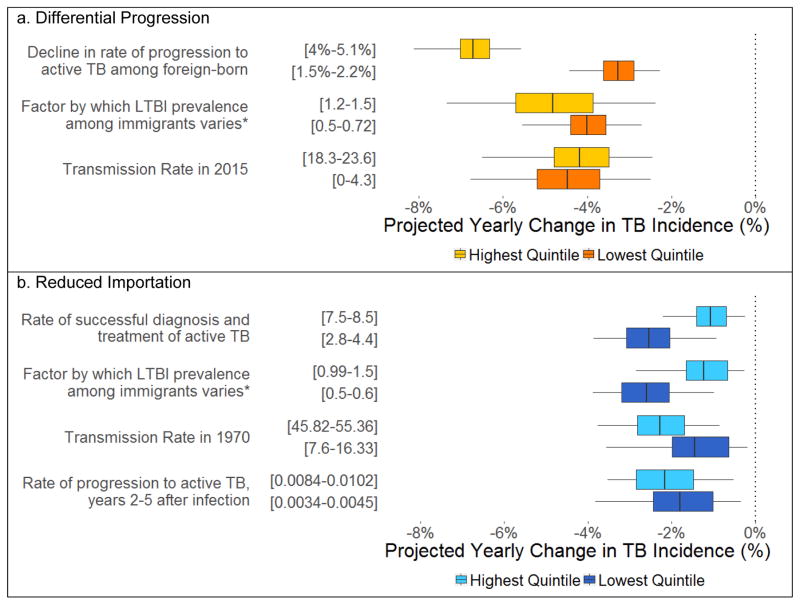
Sensitivity analyses demonstrated that the projected decline in incidence from 2015 to 2025 in the Differential Progression scenario was driven primarily by the rate of decline of LTBI progression in the foreign-born (PRCC = 0·95, indicating that the greatest estimated reductions in TB were strongly correlated with the highest rates of decline in LTBI progression in the foreign-born). The projected yearly decline in TB incidence from 2015 to 2025 was 3·4% greater (6·7% versus 3·3%) in the simulations assuming the highest quintile of values for the decline in LTBI progression compared to the lowest quintile (Figure 3). In contrast, under the Reduced Importation scenario, multiple parameters had mild effects on the primary outcome, but no parameter shifted the projected yearly decline in TB incidence by more than 1·5% when comparing simulations in the highest quintile to those in the lowest quintile of values for that parameter. Sensitivity analyses also demonstrated that our results changed little if we calibrated to years other than 2010 and 2015 or used non-uniform prior distributions for model parameters (see Supplement).
Figure 3.
Projected Annual Change in TB Incidence in Simulations with the Highest vs Lowest Quintiles of Selected Model Parameters
The relationship of projected yearly change in incidence to an individual model parameter is shown if the projections of yearly decline in TB incidence from 2015 to 2025 based on the highest quintile of the parameter (the highest 20% of sampled values for the parameter) differed by more than 0.3% per year in absolute terms from projections based on the lowest quintile of the parameter, in the (a) Differential Progression scenario or (b) Reduced Importation scenario. Vertical dark lines denote mean estimated yearly decline in TB incidence, shaded boxes denote interquartile range, error bars denote 95% credible interval. *The “Factor by which LTBI prevalence among immigrants varies” is a parameter that allows the LTBI prevalence among immigrants to vary up or down from estimates generated by prevalence surveys13 (a value of 1.0 represents no change from the baseline estimate).
DISCUSSION
Declines in TB since the 1990s, both in NYC and throughout the US, have been driven at least in part by decreasing transmission,6 the lower prevalence of latent TB infection (LTBI) among younger generations,7 and public health measures in place since the surge of TB in the 1980s.4 While budgetary considerations depend on multiple competing priorities, the implicit assumption that such factors are driving current trends and will continue to drive down TB incidence is reflected in cuts to TB control budgets. However, our results suggest that reduced transmission, changes in demography, and historical trends are not enough to explain the declines in TB incidence since 2005. In the context of our model, these declines can only be explained by assuming contemporary changes in TB epidemiology among the foreign-born population, such as a decrease in imported subclinical TB or declining risk of progression to active TB. To the extent that efforts are not undertaken to further reduce reactivation or importation of TB among the foreign-born in the next decade, the flattening of TB incidence observed over the last two years could easily continue into the next decade.
Our models suggest that existing data are consistent with either declining risk of reactivation or reduced importation as the dominant driver of recent TB trends; they do not elucidate a specific mechanism for either process. We also considered that decreasing prevalence of LTBI among incoming immigrants might partially explain the greater decline in TB incidence among the foreign-born, but LTBI notifications among legal immigrants have increased and serial surveys of LTBI in NYC clinics show that LTBI prevalence among the foreign-born rose from 2009 to 2011;13 while these observations were not taken on random population samples, they suggest that it is unlikely that LTBI prevalence among new immigrants is falling dramatically. Decreasing reactivation rates among the foreign-born could result from improved nutritional or socioeconomic status, better access to healthcare, or increasing treatment of LTBI. For example, after switching from tuberculin skin test to interferon-gamma release assays for LTBI testing in DOHMH chest clinics in 2006, patients with LTBI were more likely to complete treatment, particularly if foreign-born.19 Some degree of reduced importation of subclinical TB is suggested by internal data from the NYC DOHMH from 2007 to 2011 which show a slightly decreasing incidence of TB among immigrants during their first year after arrival, although there is substantial year-to-year variation. This could reflect improved global TB control efforts or enhanced screening of immigrants and refugees beyond US borders; following nation-wide augmentation of pre-immigration screening with TB culture in 2007, incident TB in the first 6 months after arrival fell from 4.2% to 1.5% among those eligible for screening in California.17 However, many immigrants are not covered by the extended screening, and it is unclear what the impact of this change has been for NYC. In actuality, a combination of factors likely underpins recent declines in TB, none of which are likely to fully account for trends on their own.
Regardless of the specific mechanisms, our study suggests that the future trajectory of TB incidence is linked strongly to the mix of underlying factors that have driven declines in TB incidence among the foreign-born since 2005, and the degree to which that mix changes in the future. To the extent that future dynamics are driven by mechanisms that can be further improved, sustained reductions in incidence may be feasible. This is consistent with other studies that have found rapidly decreasing incidence among the foreign born over the last decade20 and identified TB among the foreign-born population as a major driver of the overall epidemic,10, 12 and has several important implications. First, it suggests TB control programs should focus on surveillance data by country of origin and time since arrival to understand the primary underlying mechanisms underpinning incidence in the foreign-born population. Second, interventions that can sustain those declines should be a priority. To decrease progression from LTBI to active TB among the foreign-born, attention should focus on improving healthcare access for foreign-born populations or broadening testing and treatment of LTBI, as recently recommended by the US Preventive Services Task Force.8 In terms of reducing imported TB, a pilot of a pre-screening program for immigrants to the UK from high-burden countries that diagnosed immigrants in their country of origin highlights the role that innovations in screening of migrants can play.21 However, greater reductions in imported TB may be difficult to sustain unless patterns of immigration or the global burden of TB shift substantially. Consequently, our results argue for increased investment in TB control for countries from which large numbers of the foreign-born currently originate.
As with all models, we make a number of simplifying assumptions. First, we assume homogeneous respiratory mixing among all New Yorkers. This assumption is commonly made in compartmental models of TB given the airborne nature of transmission,15 and is likely to reflect the population-average transmission in our model. While there may be subpopulations with preferential mixing in NYC, it is unlikely that any single social or geographic group accounts for a large proportion of transmission; only 17% of TB cases with genotype data available from 2001 to 2015 were part of a cluster of 10 or more cases, and none of the 42 United Hospital Fund neighborhoods in NYC have an incidence more than 2.5 times the citywide average.2 Second, we treat the foreign-born as a homogenous population and do not consider migration internal to the US. This allowed us to use NYC-specific estimates of LTBI prevalence and age-stratified immigration patterns. As internal migration is not a strong driver of TB transmission, and countries of origin have not changed greatly among NYC immigrants from 2000 to 2011,22 our modeled population accurately reflects the population-average patterns (most TB cases in NYC come from China, Mexico, the Dominican Republic, and the Philippines2). However, our projections up to 2025 depend on the composition of incoming immigrants remaining broadly similar; future work could examine the effects if immigration patterns were to shift due to national policy or economic pressures. Third, we do not explicitly model HIV. While persons living with HIV are more susceptible to TB infection, studies suggest that they are no more likely to transmit TB infections;23 coupled with the low and decreasing prevalence of HIV coinfection (currently 6% of all TB cases in NYC2), this makes it unlikely that HIV would strongly influence current trends. Fourth, we assume that rates of diagnosis, treatment, and mortality are constant over time and we do not explicitly model drug resistance. As TB treatment outcomes, TB-specific mortality, and overall mortality have not changed appreciably from 2006 to 2015, and the prevalence of multidrug resistant TB was 2% in NYC in 2015, it is unlikely that any of these factors greatly affect current TB trends.2
In summary, our results highlight that demographic changes, decreasing transmission, and the robust public health measures in place since the 1990s are not enough to explain recent trends in NYC TB incidence. The declines in TB over the past decade likely reflect more recent changes in TB among the foreign-born population: a decrease in imported subclinical TB or ongoing declines in progression to active TB. Whether TB incidence continues to decline in the coming decade depends on our ability to sustain these mechanisms. In the absence of additional interventions, ongoing reductions in TB incidence are far from certain. Further study can help refine predictions and focus limited TB control resources; in the meantime, our model results argue for redoubled public health efforts and corresponding financial support if the successes against TB of the last decades are to be continued in the years to come.
Supplementary Material
RESEARCH IN CONTEXT.
Evidence before this study
We searched PubMed and Embase for articles published in any language from Jan 1, 1980 to Jan 1, 2017 with the term “tuberculosis” as well as any of the following: “New York City”, “United States”, or “low-burden”. Several studies note that after steady decline since the 1990s, the incidence of tuberculosis (TB) in New York City and the United States has remained relatively flat since 2013. While studies suggest that declines in TB incidence in the second half of the 20th century were driven by a variety of factors – antibiotic chemotherapy, decreasing TB transmission, lower prevalence of latent TB infection among younger generations, and an aggressive public health response since a surge of TB in the 1980s and 1990s – the reasons for more recent declines and for the current plateau in TB incidence remain unclear. Trends in TB among foreign-born residents have been identified in prior modeling studies as a major driver of TB in low-burden settings.
Added value of this study
This study uses rich epidemiological data on TB in New York City to inform a model of TB transmission and explore the drivers of recent trends in TB incidence. Our results suggest that recent declines in TB incidence cannot be explained by demographic trends alone and instead likely reflect contemporary changes in reactivation of latent TB among the foreign-born or a decreasing amount of imported TB. We provide numerical estimates of declines in TB incidence over the coming decade and demonstrate that, without additional efforts to further reduce TB in the foreign-born population, ongoing declines in TB incidence may not materialize.
Implications of all the available evidence
The primary determinant of future declines in TB incidence in settings like New York City is our ability to further reduce importation and reactivation of TB among foreign-born residents. Further study into the reasons for declining TB in this subpopulation can help to prioritize the allocation of limited TB control budgets. Without additional interventions, TB incidence in New York City may remain flat.
Footnotes
CONFLICTS OF INTEREST: None
AUTHOR CONTRIBUTIONS:
ATF, DWD, NLS, ASA, and SDA conceived the study.
All authors contributed to the study design.
ATF, NLS, and ASA developed the model.
NLS and SDA collected and synthesized data from New York City records.
ATF performed the data analysis and wrote the first draft of the manuscript.
All authors contributed to the data interpretation and critical review of the manuscript.
ROLE OF FUNDING SOURCE: None (there was no funding source)
Funding: None
References
- 1.Salinas JL, Mindra G, Haddad MB, Pratt R, Price SF, Langer AJ. Leveling of Tuberculosis Incidence - United States, 2013–2015. MMWR Morb Mortal Wkly Rep. 2016;65(11):273–8. doi: 10.15585/mmwr.mm6511a2. [DOI] [PubMed] [Google Scholar]
- 2.Shama Ahuja P, MPH, Knorr Jillian, MPH, Proops Douglas, MD, MPH, Silin Muriel, MPH, Shuster Yelena, BS, Stennis Natalie, MPH, Meissner Jeanne Sullivan, MPH, Trieu Lisa., MPH . Tuberculosis in New York City, 2015: New York City Bureau of Tuberculosis Control Annual Summary. 2016. [Google Scholar]
- 3.Frieden TR, Fujiwara PI, Washko RM, Hamburg MA. Tuberculosis in New York City--turning the tide. N Engl J Med. 1995;333(4):229–33. doi: 10.1056/NEJM199507273330406. [DOI] [PubMed] [Google Scholar]
- 4.Schneider E, Castro KG. Tuberculosis trends in the United States, 1992–2001. Tuberculosis (Edinb) 2003;83(1–3):21–9. doi: 10.1016/s1472-9792(02)00075-6. [DOI] [PubMed] [Google Scholar]
- 5.Committe NTCAS. NTCA Capacity Survey. 2013 [Google Scholar]
- 6.Vynnycky E, Fine PE. Interpreting the decline in tuberculosis: the role of secular trends in effective contact. Int J Epidemiol. 1999;28(2):327–34. doi: 10.1093/ije/28.2.327. [DOI] [PubMed] [Google Scholar]
- 7.Mori T, Leung CC. Tuberculosis in the global aging population. Infect Dis Clin North Am. 2010;24(3):751–68. doi: 10.1016/j.idc.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 8.Force USPST. Bibbins-Domingo K, Grossman DC, Curry SJ, Bauman L, Davidson KW, et al. Screening for Latent Tuberculosis Infection in Adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2016;316(9):962–9. doi: 10.1001/jama.2016.11046. [DOI] [PubMed] [Google Scholar]
- 9.Grassly NC, Fraser C. Mathematical models of infectious disease transmission. Nat Rev Microbiol. 2008;6(6):477–87. doi: 10.1038/nrmicro1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hill AN, Becerra J, Castro KG. Modelling tuberculosis trends in the USA. Epidemiol Infect. 2012;140(10):1862–72. doi: 10.1017/S095026881100286X. [DOI] [PubMed] [Google Scholar]
- 11.Wolleswinkel-van d B, Nagelkerke NJ, Broekmans JF, Borgdorff MW. The impact of immigration on the elimination of tuberculosis in The Netherlands: a model based approach. Int J Tuberc Lung Dis. 2002;6(2):130–6. [PubMed] [Google Scholar]
- 12.Jia ZW, Tang GY, Jin Z, Dye C, Vlas SJ, Li XW, et al. Modeling the impact of immigration on the epidemiology of tuberculosis. Theor Popul Biol. 2008;73(3):437–48. doi: 10.1016/j.tpb.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 13.Stennis NL, Trieu L, Ahuja SD, Harris TG. Estimated Prevalence of Tuberculosis Infection Among a New York City Clinic Population Using Interferon-gamma Release Assays. Open Forum Infect Dis. 2014;1(2):ofu047. doi: 10.1093/ofid/ofu047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clark CM, Driver CR, Munsiff SS, Driscoll JR, Kreiswirth BN, Zhao B, et al. Universal genotyping in tuberculosis control program, New York City, 2001–2003. Emerg Infect Dis. 2006;12(5):719–24. doi: 10.3201/eid1205.050446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Menzies NA, Cohen T, Lin HH, Murray M, Salomon JA. Population health impact and cost-effectiveness of tuberculosis diagnosis with Xpert MTB/RIF: a dynamic simulation and economic evaluation. PLoS Med. 2012;9(11):e1001347. doi: 10.1371/journal.pmed.1001347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dowdy DW, Basu S, Andrews JR. Is passive diagnosis enough? The impact of subclinical disease on diagnostic strategies for tuberculosis. Am J Respir Crit Care Med. 2013;187(5):543–51. doi: 10.1164/rccm.201207-1217OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lowenthal P, Westenhouse J, Moore M, Posey DL, Watt JP, Flood J. Reduced importation of tuberculosis after the implementation of an enhanced pre-immigration screening protocol. Int J Tuberc Lung Dis. 2011;15(6):761–6. doi: 10.5588/ijtld.10.0370. [DOI] [PubMed] [Google Scholar]
- 18.Kass RE, Raftery AE. Bayes Factors. Journal of the American Statistical Association. 1995;90(430):773. [Google Scholar]
- 19.Crossa A, Kessler J, Harris TG. Enhanced Tuberculosis Infection Treatment Outcomes after Implementation of QuantiFERON(R)-Gold Testing. PLoS One. 2015;10(9):e0138349. doi: 10.1371/journal.pone.0138349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker BJ, Winston CA, Liu Y, France AM, Cain KP. Abrupt Decline in Tuberculosis among Foreign-Born Persons in the United States. PLoS One. 2016;11(2):e0147353. doi: 10.1371/journal.pone.0147353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aldridge RW, Zenner D, White PJ, Williamson EJ, Muzyamba MC, Dhavan P, et al. Tuberculosis in migrants moving from high-incidence to low-incidence countries: a population-based cohort study of 519–955 migrants screened before entry to England, Wales, and Northern Ireland. The Lancet. 2016;388(10059):2510–8. doi: 10.1016/S0140-6736(16)31008-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lobo AP, Salvo JJ New York (N.Y.). Department of City Planning. Population Division. The newest New Yorkers : characteristics of the city’s foreign-born population. 2013. New York: City of New York, Department of City Planning, Office of Immigrant Affairs; 2013. p. x.p. 235.p. 1. [Google Scholar]
- 23.Cruciani M, Malena M, Bosco O, Gatti G, Serpelloni G. The Impact of Human Immunodeficiency Virus Type 1 on Infectiousness of Tuberculosis: A Meta-Analysis. Clinical Infectious Diseases. 2001;33(11):1922–30. doi: 10.1086/324352. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.